Abstract
The magnitude of humeral torsion (HT) affects the internal and external rotation range of motion at the shoulder. Currently imaging is required to quantify the HT angle, however, factors such as cost and non-availability of imaging to musculoskeletal clinicians limits its use. The aim of this study was to examine the validity of palpation of the bicipital tuberosities as an alternative to imaging for quantifying HT angles. The bicipital-forearm angle, an indirect measure of HT, was measured using palpation and real-time ultrasound imaging in 25 subjects. The agreement among the two methods was excellent with the Intraclass Correlation Coefficient (3,k) = 0.92, and the mean difference between the two methods was −0.2° (SD 4.1°) with 95% limits of agreement of −8.3° to 7.9°. Pearson’s correlation coefficient (r) among the two methods was 0.85. In a clinical setting, palpation appears to be a practical alternative to US imaging for measuring HT.
INTRODUCTION
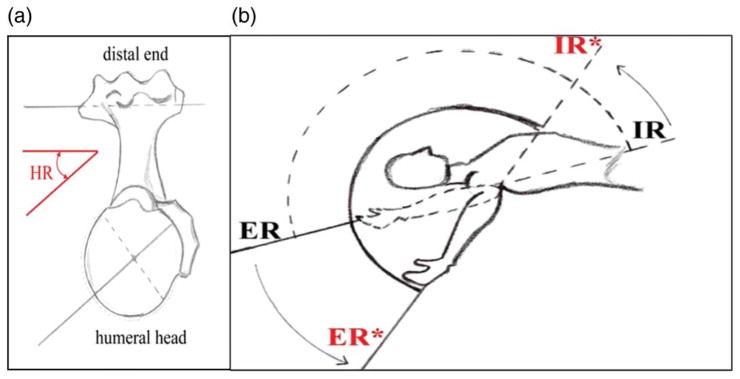
Increased external rotation (ER) and decreased internal rotation (IR) range of motion (ROM) is common in people who use their arms repeatedly in an over-head manner such as throwing athletes. This shift in ROM is associated with shoulder injuries (Shanley et al, 2011; Wilk et al, 2011), and restoration of normal ROM is associated with improvement in clinical symptoms (Burkhart, Morgan, and Kibler, 2003a; 2003b; Myers et al, 2006; Tyler et al, 2000; 2010). Anatomical structures are thought to be altered when increased ER and decreased IR ROM at the shoulder are apparent and include the posterior glenohumeral (GH) joint capsule, posterior shoulder muscles and humeral torsion (HT) (Myers et al, 2006; Tyler et al, 2000; 2010). The HT angle represents the degree of twist of the humerus along its longitudinal axis and is quantified as the acute angle formed medially and posteriorly between the trans-condylar axis (distal humerus) and the line bisecting the humeral head (proximal humerus) (Figure 1a). The more posteriorly oriented the humeral head is with respect to the epicondyles, the larger is the magnitude of HT. A larger HT angle is associated with decreased IR and increased ER ROM at the shoulder (Kronberg, Broström, and Söderlund, 1990)
FIGURE 1.
(a) Human retroversion (HR) angle. The angle sustained between the epicondylar axis (distal end) and a line bisecting the humeral head; b) posteriorly shifted arc of motion due to increased HR angle. Note the apparent reduction in the internal rotation (IR*) and increased external rotation (ER*)
The range of HT is reported to be −5° to 50° (Boileau et al, 2008; Robertson et al, 2000). HT angle also varies by: race (Edelson, 1999); age (Edelson, 2000); hand dominance (Doyle and Burks, 1998; Yamamoto et al, 2006); and the level and intensity of repeated overhead activity (Chant, Litchfield, Griffin, and Thain, 2007; Crockett et al, 2002; Makiuchi et al, 2004; Myers et al, 2009; Osbahr, Cannon, and Speer, 2002; Reagan et al, 2002; Schwab and Blanch, 2009; Tokish et al, 2008; Yamamoto et al, 2006). Due to the great variation in HT angle and its influence on shoulder ER and IR ROM, clinical measurement of HT should be an essential part of the shoulder examination. Conventionally, ER and IR ROM at the shoulder are quantified with the patient in supine, the shoulder abducted, and the elbow flexed to 90°, so that forearm is aligned with vertical (Figure 1b). From this starting position, he end ranges in passive IR and ER are measured. However, in these measurements, the influence of the HT angle on ROM is not considered, which may lead to incorrectly interpreting the cause of the apparent shift in ROM.
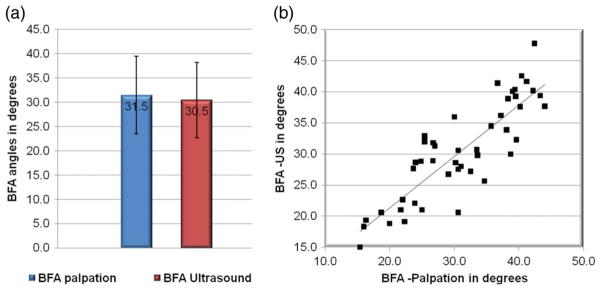
Plain radiographs (Osbahr, Cannon, and Speer, 2002; Reagan et al, 2002; Tokish et al, 2008); computed tomography (CT) (Chant, Litchfield, Griffin, and Thain, 2007; Crockett et al, 2002; Hernigou, Duparc, and Hernigou, 2002); and ultrasound (US) (Ito et al, 1995; Myers et al, 2009; Whiteley, Ginn, Nicholson, and Adams, 2006) are used to measure HT angle. US can measure HT quickly, is non-invasive (Myers et al, 2009; Whiteley, Ginn, Nicholson, and Adams, 2006), and allows assessment of HT angle without exposing the patients to radiation (Ito et al, 1995; Myers et al, 2009). Because it is not possible to visualize both ends of the humerus simultaneously using one US unit, a direct measurement of HT angle is impossible. To address this limitation, Ito et al (1995) quantified the angle between the forearm and vertical while using a real-time US image to orient the bicipital tuberosities, calling this measure the bicipital-forearm angle (BFA) (Figure 2). Because the ulna is essentially perpendicular to the epicondylar axis (line connecting medial and lateral epicondyle of humerus) when the elbow is flexed to 90°, the angle between the ulna and vertical can be used to quantify HT. The BFA and the HT angle are inversely related such that a smaller BFA indicates a greater amount of HT (Yamamoto et al, 2006).
FIGURE 2.
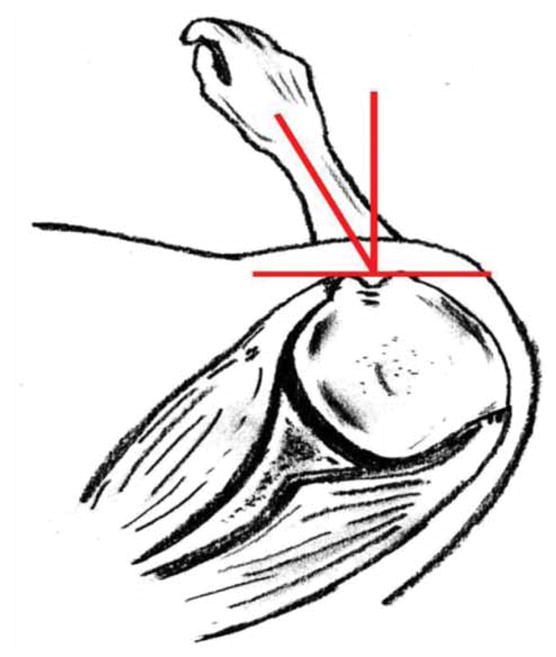
The bicipital - forearm angle: the angle between the epicondylar axis (distal humerus) and a line connecting the two tuberosities (proximal humerus) representa the torsion of the humerus. Because the ulna is perpendicular to the epicondylar axis, the angle between the ulna and vertical is a measure of humeral retroversion.
While US imaging has been used for quantifying HT angle (Ito et al, 1995; Myers et al, 2009; Whiteley, Ginn, Nicholson, and Adams, 2006; Yamamoto et al, 2006), its utility in many rehabilitation settings is limited (Myers et al, 2009). The cost incurred by patients is one factor limiting the use of US imaging to assess HT angle. Other limiting factors are the restricted availability of real-time US imaging units in rehabilitation settings, and lack of clinician training. On the other hand, clinicians regularly palpate various anatomical structures during physical assessment, and a method of quantifying HT using palpation will make the clinical measurement of HT angle a part of the regular physical examination. The purpose of this study was to examine the validity of measuring BFA by palpation of the bicipital tuberosities through comparison to BFA as measured by using US imaging to orient the bicipital tuberosities. Our hypothesis was that BFA measured using palpation of the bicipital tuberosities would be a valid alternative to measuring BFA with US.
METHODS
The Ohio State University Institutional Review Board approved this study and all volunteers provided informed consent prior to data collection. The study sample included 49 shoulders from 12 males and 13 females. Mean age was 26.2 years (SD 3.9) and mean body mass index (BMI) was 21.4 (2.4). All were right-hand dominant. Overhead athletes were not excluded; however, none of our subjects had a history of participating in overhead sports. No subject reported a prior fracture or surgery involving the shoulder or upper extremity.
Procedures
Shoulder IR and ER ROM were measured by the first examiner with the subject positioned supine with the shoulder abducted to 90° and the elbow flexed to 90°. The scapula was manually stabilized over the coracoid process by the second examiner during the IR measurement. The BFA was then measured using two methods of orienting the bicipital tuberosities, with palpation always performed first, followed by US imaging. Two examiners performed the measurements; Examiner 1 oriented the humeral head while rotating the forearm medially and laterally, while Examiner 2 quantified BFA using an inclinometer (Baseline Inclinometer, Fabrication Enterprise Inc., Irvington, NY, USA). Examiner 1 was allowed to rotate the humerus using the forearm to orient the tuberosities, but a curtain was used to blind him to the visual orientation of the forearm. With the exception of one subject, all measurements were repeated three times and taken on both shoulders.
Palpation
Volunteers were positioned supine, with arms at the side, elbow flexed to 90°, the forearm midway between supination and pronation with palm facing the subject. The clearance of the forearm in IR was increased by placing a pillow under the distal humerus. Examiner 1 began the trial by palpating the lateral tip of the acromion with his thumb, then glided the thumb inferiorly between the anterior and middle fibers of deltoid to the head of humerus. At times, it was helpful to ask the subject to isometrically contract the deltoid in order to detect the interval between the anterior and middle fibers. Next, Examiner 1 palpated the greater and lesser tuberosities of the humerus. At this point, the orientation of the palpating thumb was changed from the tip of the thumb facing inferior to the tip facing medial. The subject’s humerus was then rotated medially and laterally, and the humerus was considered in its desired orientation when the greater and lesser tuberosities were both felt under the thumb. If the lesser tuberosity was not felt under the thumb, as happened occasionally, the most prominent part of the greater tuberosity was used to orient the humerus.
Ultrasound
For the criterion-standard measurement, a Sonosite TITAN US machine (6 MHz transducer, 6 cm scan depth) was used to visualize the bicipital tuberosities in real time. Examiner 1 spent 3 months familiarizing himself with using US for identifying anatomical structures at the shoulder, including the rotator cuff, posterior capsule, and bicipital tuberosities. The technique used for this study was developed and refined during pilot testing of approximately 20 shoulders. During pilot testing, it was noted that slight changes in the US transducers orientation impacted the orientation of the tuberosities on the US image. To address this, two bubble levels were attached to the transducer to confirm the correct orientation of the transducer, which was then maintained using a test tube holder.
The US transducer was placed on the shoulder to display a transverse section of the proximal humerus. Similar to the palpation method, the humerus was rotated until the tuberosities were in the desired orientation. The orientation was defined by the following criteria: (1) the floor of the bicipital groove was horizontal; and (2) both the tuberosities were at the same level horizontally on the US image. A 0.5 cm2 grid printed on a transparency was attached to the screen of the US unit to ensure that these criteria were met consistently.
BFA measurement
Once the humerus was oriented, Examiner 2 quantified the BFA using an inclinometer with respect to the vertical. The inclinometer was placed flush with the distal forearm just proximal to the ulnar styloid process.
Data analysis
A repeated measure ANOVA was used to compare BFA detected by palpation and US methods, with BFA the dependent variable and the two measurement methods the repeated within-subject factor. An Intraclass Correlation Coefficient (ICC(3, 2)) between the palpation and US methods was calculated to assess the validity. ICC values above 0.75 conventionally indicate good reliability between two methods. Pearson’s correlation coefficient (r) was used to determine the relationship among BFA values detected by palpation and US. Bland–Altman plots were used to calculate the mean difference and evaluate the 95% limits of agreement between the two methods. For statistical analysis, NCSS 2001 and a significance level set at p < 0.05 were used.
RESULTS
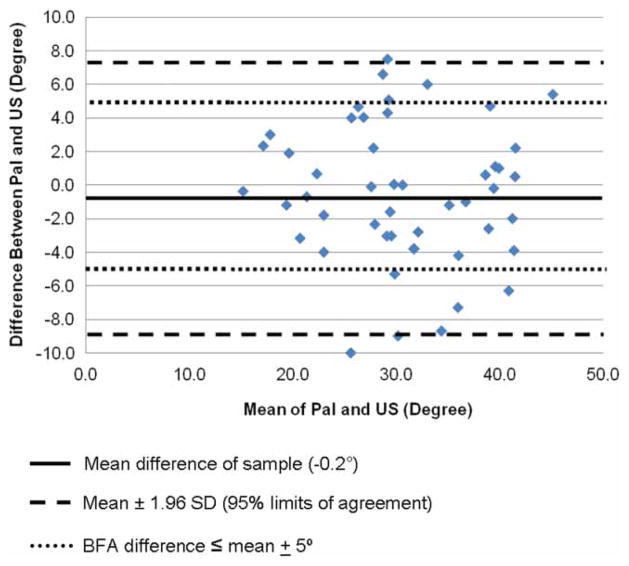
The mean BFA measured with US and palpation were 31.5° (SD 7.5°) and 30.5° (SD 7.9°) respectively, which were not statistically different (F = 0.0; p = 0.99) (Figure 3a). The correlation and agreement among the two methods were excellent with the ICC = 0.92 (95% CI 0.86–0.95), and r calculated to be 0.85 (95% CI 0.69–0.93) (Figure 3b). The mean difference between the two methods was −0.2° (SD 4.1°). The 95% limits of agreement were −8.3° to 7.9°, and 79.6% of the difference values were within ±5° of the mean difference (Figure 4).
FIGURE 3.
(a) Mean BFA detected by palpation and US; (b) Correlation among the BFA detected by palpation (x-axis) and US (y-axis).
FIGURE 4.
Difference between BFA measurements by palpation and US plotted against the mean value of BFA for each subject—Mean difference of sample (−0.2°)–Mean±1.96 SD (95% limits of agreement)……BFA differences ≤ mean±5°
DISCUSSION
We quantified the BFA using palpation of the bicipital tuberosities to orient the humeral head and compared it to the BFA quantified using real-time US images. Our results suggest that palpation of bicipital tuberosities is a valid clinical alternative for measuring the BFA. A comparison of mean values of BFA measured using palpation and US suggest no significant difference between the two measurement methods. The correlation coefficient (r = 0.85) suggests high covariance among the two methods (Figure 3a and b). Comparison of means and the correlation coefficient, however, do not reflect the extent of agreement among the two methods (Portney and Watkins, 2009). We used the ICC to assess agreement among the two methods, which was noted to be excellent at 0.92.
Bland–Altman plots were used to further compare the ability of palpation to measure BFA as a clinical substitute for US. Bland–Altman plots graphically quantify the variation in “between-method” differences for every subject. The true value of the phenomenon being measured is estimated in Bland–Altman analysis as the overall mean difference of the mean values obtained by the each method separately. The difference between the values obtained by two methods for each subject are then plotted against the overall mean difference to provide information about the discrepancy between the two methods relative to the estimate of the true value. The 95% limits of agreement provide a visual estimate of the agreement between the two methods, with smaller the range of the limits of agreement, the stronger the agreement between methods.
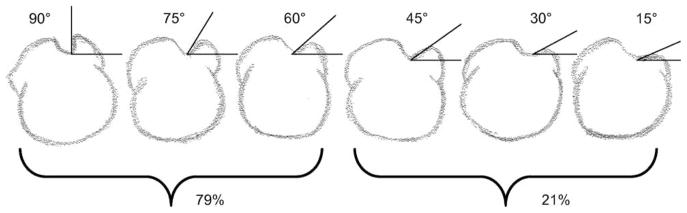
The overall mean difference (BFAUS–BFApalpation) between the two methods was −0.2° (SD 4.1°), implying that on average the difference between the two methods is small and definitely within an acceptable range of clinical error (Portney and Watkins, 2009). The 95% limits of agreement (−8.3° to 7.9°) define the range within which most differences between palpation and US measurement of BFA lie (Figure 4). This means that at its least accurate, the palpation method can either overestimate the BFA by 8.1° or underestimate by 8.1°. However, the majority of the difference values (79.6%) fall within a range of ±5° of the overall mean value. We propose that the values with greater error may be related to the anatomy of the lesser tuberosity. According to Rock-wood, Matsen, Lippitt, and Wirth (2009), 79% of the population have lesser tuberosities where the angle relative to the bicipital groove is between 60° and 90°, and the remaining 21% have angles between 15° and 45°. To meet our US orientation criteria, a humerus with lower angles of the lesser tuberosity will require greater ER of the shoulder to make the tuberosities level on the image. If palpation is not as sensitive to these lower angles, it would result in a larger difference in how the tuberosities are oriented and larger differences between the two methods.
To examine the clinical applicability of the palpation method in the context of shoulder pathology, consider that a loss in IR ROM of 25°–35° is associated with shoulder injuries (Myers et al, 2006; Tokish et al, 2008; Tyler et al, 2000; 2010). Even with a maximum overestimation of HT of 8.1°, the remaining 17° to 27° of motion loss in a patient requiring intervention can be attributed to soft tissue, which should only minimally affect clinical decision making regarding treatment. In addition, the overall distribution of difference values was well under 25°, supporting the clinical utility of using this measure to make decisions about patients with shoulder pathology and clinically meaningful IR ROM loss. Because there are no clearly established criteria for determining acceptable degrees of difference when comparing an old measurement method with a new one, the decision to accept a new method becomes a matter of judgment and examination of prior precedent. This study demonstrates, through limits of agreement that are comparable to the limits reported for other measures of joint motion, that using palpation to measure HT appears to be valid (de Winter et al, 2004; Tveitå, Ekeberg, Juel, and Bautz-Holter, 2008).
To further evaluate the clinical utility of the palpation method, we also calculated the standard error of measurement (SEM), which was 3.1°, and the minimal detectable change (MDC), which was 6.1°. Although the SEM and MDC statistics are most meaningful for evaluating the reliability of a measurement, they do give an estimate of the accuracy of a repeated measurement using the palpation method. The SEM suggests that there is a 95% chance that the true value of BFA for this sample lies between 24.4° and 36.6°. The MDC suggests that a change in the BFA measurement must be at least 6.1° to be confident that the change is not just measurement error. When considered relative to the 25° to 35° loss of IR ROM that is associated with shoulder pathology (Myers et al, 2009; Tyler et al, 2010), these statistics support the use of the palpation measurement to evaluate HT. One could potentially use MDC to evaluate change in HT in throwing athletes over time, or to verify that no change in HT has occurred when an intervention to stretch posterior shoulder tissues is given to skeletally mature individuals.
In a similar study, Whiteley, Ginn, Nicholson, and Adams (2006) compared the inter-tester reliability of palpation and US imaging methods for measuring BFA. They reported excellent inter-tester reliability for the US method (ICC = 0.98), but poor inter-tester reliability for palpation (ICC = 0.51). However, the Whiteley, Ginn, Nicholson, and Adams (2006) study did not make a direct comparison of BFA values measured by the palpation method to those measured by the US method. The focus of our study was to examine the agreement between BFA angle measured by palpation and US, and the comparison resulted in a high ICC (0.92) between the two methods. With evidence of validity, it is now necessary to examine the inter-tester reliability of using palpation to measure BFA among multiple clinicians.
This study also differed from that of Whiteley, Ginn, Nicholson, and Adams (2006) in how subjects were positioned during the measurements. In the Whiteley, Ginn, Nicholson, and Adams (2006) study, subjects were positioned supine with the shoulder abducted to 90° and elbow flexed to 90°. In this position, the bicipital tuberosities are covered by the anterior fibers of the deltoid, making palpation of the tuberosities more difficult. In our study, subjects were supine but did not abduct the arm, which may have allowed improved palpation of the tuberosities between the anterior and middle fibers of the deltoid. We also observed a learning effect in palpating and orienting the bicipital tuberosities. In the first five subjects, the average difference of the BFA values between the two methods was 5.5°, as opposed to an average difference of 1.4° for the final five subjects tested. This suggests that with practice, an examiner will get closer to the criterion-standard US BFA values.
In a clinical setting, palpation is a practical alternative to US imaging for assessing HT. US imaging units are not widely available in outpatient clinics, especially in less developed parts of the world. In addition, most musculoskeletal clinicians lack the training necessary to use US as an imaging modality. Finally, because practice acts may not permit musculoskeletal clinicians to perform or prescribe imaging, referral of patients to another provider skilled in imaging may delay assessment and treatment. Palpation, however, is a common skill taught to all musculoskeletal clinicians, who use palpation regularly during patient assessment and treatment. The skills needed to perform the HT measurement can be learned with little practice and knowledge of shoulder anatomy.
A potential source of error of the palpation measurement is the amount of subcutaneous tissue through which the bicipital tuberosities must be felt. This source of error may be increased in more muscular individuals, and in individuals with higher BMI. The mean BMI of our sample was 21.4, however, in two subjects with BMI > 25 the difference between the two methods was greater than 5°. This suggests that the palpation method may be less accurate for measuring HT in overweight individuals, although a study to confirm this is needed. Another source of error is variation in the shape of the bicipital tuberosities. Bicipital tuberosities are classified on the basis of the angle the lesser tuberosity makes with the horizontal, (Figure 5) and vary between 15° and 90° (Rockwood, Matsen, Lippitt, and Wirth, 2009). A lesser tuberosity with a higher angle is more easily visualized using US, requires less humerus rotation to orient the tuberosities for the measurement, and may be easier to palpate. Unfortunately, we did not record US images of the bicipital tuberosities, so we do not know if or how this variable impacted the two measurements. According to Rockwood, Matsen, Lippitt, and Wirth (2009), 79% of the population have a lesser tuberosity with an angle between 60° and 90°, and the remaining 21% have an angle between 15° and 45°. Interestingly, these percentages are almost perfectly reflective of the percentage of subjects, in this study, whose BFA varied ≤5° between measurement methods (79.6%) and those whose BFA varied >5° (20.4%).
FIGURE 5.
Variation in the bicipital tuberosities. Adapted from Rockwood and Masten. Shoulder 4thedition. Saunders Elsevier.
While Examiner 1 was blinded to the visual orientation of the forearm, it was not possible to eliminate the kinesthetic feedback he received while orienting the forearm during the measurements. It is possible that kinesthetic memory of forearm position from the first method could have biased the forearm position during the second method. Kinesthetic feedback is an inevitable and essential part of a clinical physical assessment, and therefore constitutes one facet of the measurement that contributes to the validity of a clinical test. However, to control this potential bias, we measured BFA using the palpation method first. Because the criteria for orienting the tuberosities on the US image was objective and predefined, the US measure did not depend on the position of the forearm, negating the potential impact of kinesthetic memory.
A potential limitation of measuring BFA is that the measured angle may be influenced by the carrying angle of the elbow. However, the carrying angle reduces as the elbow flexes, minimizing its influence on BFA. For this study, in particular, any influence of the carrying angle on BFA is equally present in both measurement methods as long as elbow flexion angle is maintained at 90° for both. This limitation may be more of an issue when comparing BFA between subjects.
Myers, Oyama, and Clarke (2012) recently compared HT values measured using US against values measured using CT, the current gold standard, and concluded that US is a valid and reliable alternative to CT for measuring HT. Furthermore, the BFA angles previously reported by Myers et al (2009) and Whiteley, Ginn, Nicholson, and Adams (2006) using US are similar to angles reported in studies that have measured HT using radiographic methods (Crockett et al, 2002; Reagan et al, 2002). Collectively, these comparisons establish the validity of using US for measuring BFA (Myers et al, 2009; Myers, Oyama, and Clarke, 2012).
CONCLUSION
Measurement of HT should be a part of ROM assessment at shoulder joint. This study demonstrates that using palpation to orient the bicipital tuberosities is a valid method of measuring BFA and assessing HT. Clinicians trained in palpation should be able to easily learn and use this palpation measurement of HT. As this study examined only validity, the reliability of this palpation measurement method remains unknown.
Acknowledgments
The authors thank Dr Deborah Givens for the ultrasound unit and Mr Oren Costantini for helping with data collection. Dr Borstad receives funding from the National Institute of Child Health and Human Development; Award no. K01HD052797.
Footnotes
Declaration of interest: The authors report no declaration of interest.
References
- Boileau P, Bicknell RT, Mazzoleni N, Walch G, Urien JP. CT scan method accurately assesses humeral head retroversion. Clinical Orthopaedics and Related Research. 2008;466:661–669. doi: 10.1007/s11999-007-0089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology Part I: Pathoanatomy and biomechanics. Arthroscopy. 2003a;19:404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: Spectrum of pathology. Part II: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy. 2003b;19:531–539. doi: 10.1053/jars.2003.50139. [DOI] [PubMed] [Google Scholar]
- Chant CB, Litchfield R, Griffin S, Thain LM. Humeral head retroversion in competitive baseball players and its relationship to glenohumeral rotation range of motion. Journal of Orthopaedic Sports Physical Therapy. 2007;37:514–520. doi: 10.2519/jospt.2007.2449. [DOI] [PubMed] [Google Scholar]
- Crockett HC, Gross LB, Wilk KE, Schwartz ML, Reed J, O’Mara J, Reilly MT, Dugas JR, Meister K, Lyman S, Andrews JR. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. American Journal of Sports Medicine. 2002;30:20–26. doi: 10.1177/03635465020300011701. [DOI] [PubMed] [Google Scholar]
- de Winter A, Heemskerk M, Terwee C, Jans M, Devillé W, Van Schaardenburg DJ, Scholten R, Bouter L. Inter-observer reproducibility of measurements of range of motion in patients with shoulder pain using a digital inclinometer. BMC Musculoskeletal Disorders. 2004;5:18–25. doi: 10.1186/1471-2474-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle AJ, Burks RT. Comparison of humeral head retroversion with the humeral axis/biceps groove relationship: A study in live subjects and cadavers. Journal of Shoulder and Elbow Surgery. 1998;7:453–457. doi: 10.1016/s1058-2746(98)90193-8. [DOI] [PubMed] [Google Scholar]
- Edelson G. Variations in the retroversion of the humeral head. Journal of Shoulder and Elbow Surgery. 1999;8:142–145. doi: 10.1016/s1058-2746(99)90007-1. [DOI] [PubMed] [Google Scholar]
- Edelson G. The development of humeral head retroversion. Journal of Shoulder and Elbow Surgery. 2000;9:316–318. doi: 10.1067/mse.2000.106085. [DOI] [PubMed] [Google Scholar]
- Hernigou P, Duparc F, Hernigou A. Determining humeral retroversion with computed tomography. Journal of Bone and Joint Surgery Am. 2002;84:1753–1762. doi: 10.2106/00004623-200210000-00003. [DOI] [PubMed] [Google Scholar]
- Ito N, Eto M, Maeda K, Rabbi ME, Iwasaki K. Ultrasonographic measurement of humeral torsion. Journal of Shoulder and Elbow Surgery. 1995;4:157–161. doi: 10.1016/s1058-2746(05)80045-x. [DOI] [PubMed] [Google Scholar]
- Kronberg M, Broström LA, Söderlund V. Retroversion of the humeral head in the normal shoulder and its relationship to the normal range of motion. Clinical Orthopaedics and Related Research. 1990;253:113–117. [PubMed] [Google Scholar]
- Makiuchi D, Tsutsui H, Mihara K, Hokari S, Suzuki K, Ota K, Matsuhisa T, Nishinaka N, Yamaguchi K. The humeral retroversion in baseball players with an internal impingement. Shoulder Joint. 2004;28:339–341. [Google Scholar]
- Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. American Journal of Sports Medicine. 2006;34:385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- Myers JB, Oyama S, Clarke JP. Ultrasonogrpahic assessment of humeral retrotorsion in baseball players: A validation study. American Journal of Sports Medicine. 2012 Mar 1; doi: 10.1177/0363546512436801. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Myers JB, Oyama S, Goerger BM, Rucinski TJ, Blackburn JT, Creighton RA. Influence of humeral torsion on interpretation of posterior shoulder tightness measures in overhead athletes. Clinical Journal of Sport Medicine. 2009;19:366–371. doi: 10.1097/JSM.0b013e3181b544f6. [DOI] [PubMed] [Google Scholar]
- Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. American Journal of Sports Medicine. 2002;30:347–353. doi: 10.1177/03635465020300030801. [DOI] [PubMed] [Google Scholar]
- Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Upper Saddle River, NJ: Pearson/Prentice-Hall; 2009. [Google Scholar]
- Reagan KM, Meister K, Horodyski MB, Werner DW, Carruthers C, Wilk K. Humeral retroversion and its relationship to glenohumeral rotation in the shoulder of college baseball players. American Journal of Sports Medicine. 2002;30:354–360. doi: 10.1177/03635465020300030901. [DOI] [PubMed] [Google Scholar]
- Robertson DD, Yuan J, Bigliani LU, Flatow EL, Yamaguchi K. Three-dimensional analysis of the proximal part of the humerus: Relevance to arthroplasty. Journal of Bone and Joint Surgery Am. 2000;82:1594–1602. doi: 10.2106/00004623-200011000-00013. [DOI] [PubMed] [Google Scholar]
- Rockwood CA, Matsen FA, Lippitt SB, Wirth MA. The Shoulder. Philadelphia: WB Saunders Co; 2009. [Google Scholar]
- Schwab LM, Blanch P. Humeral torsion and passive shoulder range in elite volleyball players. Physical Therapy in Sport. 2009;10:51–56. doi: 10.1016/j.ptsp.2008.11.006. [DOI] [PubMed] [Google Scholar]
- Shanley E, Rauh MJ, Michener LA, Ellenbecker TS, Garrison JC, Thigpen CA. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. American Journal of Sports Medicine. 2011;39:1997–2006. doi: 10.1177/0363546511408876. [DOI] [PubMed] [Google Scholar]
- Tokish JM, Curtin MS, Kim YK, Hawkins RJ, Torry MR. Glenohumeral internal rotation deficit in the asymptomatic professional pitcher and its relationship to humeral retroversion. Journal of Sports Science and Medicine. 2008;7:78–83. [PMC free article] [PubMed] [Google Scholar]
- Tveitå E, Ekeberg O, Juel N, Bautz-Holter E. Range of shoulder motion in patients with adhesive capsulitis: Intra-tester reproducibility is acceptable for group comparisons. BMC Musculoskeletal Disorders. 2008;9:49–57. doi: 10.1186/1471-2474-9-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler TF, Nicholas SJ, Lee SJ, Mullaney M, McHugh MP. Correction of posterior shoulder tightness is associated with symptom resolution in patients with internal impingement. American Journal of Sports Medicine. 2010;38:114–119. doi: 10.1177/0363546509346050. [DOI] [PubMed] [Google Scholar]
- Tyler TF, Nicholas SJ, Roy T, Gleim GW. Quantification of posterior capsule tightness and motion loss in patients with shoulder impingement. American Journal of Sports Medicine. 2000;28:668–673. doi: 10.1177/03635465000280050801. [DOI] [PubMed] [Google Scholar]
- Whiteley R, Ginn K, Nicholson L, Adams R. Indirect ultrasound measurement of humeral torsion in adolescent baseball players and non-athletic adults: Reliability and significance. Journal of Science and Medicine in Sport. 2006;9:310–318. doi: 10.1016/j.jsams.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson CD, Harker P, Paparesta N, Andrews JR. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. American Journal of Sports Medicine. 2011;39:329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]
- Yamamoto N, Itoi E, Minagawa H, Urayama M, Saito H, Seki N, Iwase T, Kashiwaguchi S, Matsuura T. Why is the humeral retroversion of throwing athletes greater in dominant shoulders than in nondominant shoulders? Journal of Shoulder and Elbow Surgery. 2006;15:571–575. doi: 10.1016/j.jse.2005.06.009. [DOI] [PubMed] [Google Scholar]