Abstract
Women exposed to more types of violence (e.g., emotional, physical, or sexual violence) – referred to here as cumulative violence exposure – are at risk for more severe mental health symptoms compared to women who are exposed to a single type of violence or no violence. Women exposed to violence may also experience greater emotional nonacceptance compared to women with no exposure to violence. Emotional nonacceptance refers to an unwillingness to experience emotional states, including cognitive and behavioral attempts to avoid experiences of emotion. Given the links between cumulative violence exposure, emotional nonacceptance, and mental health symptoms among female victims of violence, the current study tested victims’ emotional nonacceptance as a partial mediator between cumulative violence exposure and the severity of three types of symptoms central to complex trauma responses: depression, dissociation, and Posttraumatic stress disorder (PTSD) symptoms. A non-treatment seeking community sample of women (N = 89; Mage = 30.70 years) completed self-report questionnaires and interviews. Bootstrap procedures were then used to test three mediation models for the separate predictions of depression, dissociation, and PTSD symptoms. Results supported our hypotheses that emotional nonacceptance would mediate the relationship between women’s cumulative violence exposure and severity for all symptom types. The current findings highlight the role that emotional nonacceptance may play in the development of mental health symptoms for chronically victimized women and point to the need for longitudinal research in such populations.
Keywords: depression, dissociation, emotional nonacceptance, cumulative violence, Posttraumatic stress disorder (PTSD)
Violence against women is a social and public health problem that demands critical attention. A national survey estimated that approximately 30% of U.S. women are victims of physical, sexual, or emotional/psychological intimate partner violence (IPV; Coker et al., 2002). Women exposed to violence are at significantly greater risk than their non-exposed peers for mental health difficulties, including symptoms of depression (Calvete, Corral, & Estevez, 2007; Golding, 1999), dissociation (Neumann, Houskamp, Pollock, & Briere, 1996), and posttraumatic stress disorder (PTSD; e.g., Kessler, Sonnega, Bromet, & Hughes, 1995; Kilpatrick, Saunders, & Smith, 2003). Further, women exposed to more types of victimizations (e.g., emotional, physical, sexual violence) – referred to here as cumulative violence exposure – report more severe mental health symptoms as compared to women exposed to one or no victimizations (Follette, Polusny, Bechtle, & Naugle, 1996; Green et al., 2000).
In order to enhance the impact of prevention and intervention efforts for victims of violence, a critical goal of current research is to identify risk and resilience factors that contribute to the relationship between cumulative violence exposure and later mental health symptoms among victims. The current study pursues that goal through examining a mechanism that may link victims’ cumulative violence exposure to the severity of their mental health symptoms: emotional nonacceptance. As mental health outcomes of interest, we focused on symptoms of depression, dissociation, and PTSD due to the centrality of these symptoms to the phenomena of complex trauma among chronically victimized individuals (e.g., Cook et al., 2005; see Golding, 1999 for a review).
Cumulative Violence Exposure
While several studies now document associations between greater cumulative violence exposures and greater severity of mental health symptoms (e.g., Follette et al., 1996; Green et al., 2000), several methodological issues remain to be addressed within those studies connecting violence and mental health. The first methodological issue is one of generalizability. Previous studies of victims’ mental health following violence exposure have often relied on college samples of women (e.g., Messman-Moore, Long, & Siegfried, 2000; Sappington, Pharr, Tunstall, & Rickert, 1997). College samples typically include fewer women of lower socioeconomic status (SES) and racial/ethnic minority identification compared to the general population (see Messman-Moore & Long, 2003 for a review). Research demonstrates that women of racial/ ethnic minority and low SES are at particularly high risk for the experience of multiple violence exposures and severe mental health symptomatology (Crouch, Hanson, Saunders, Kilpatrick, & Resnick, 2000). Thus, findings from previous studies of college samples are likely limited in their generalizability to more typical populations of victimized women.
Second, many previous studies assess women’s history of exposure to violence in a fairly limited fashion. For instance, some studies ask women to report only certain types of violence (e.g., sexual abuse), but not other types of violence (e.g., physical abuse) (e.g., Marhoefer-Dvorak, Resick, Hutter, & Girelli, 1998; Murphy, Kilpatrick, Amick-McMullan, & Veronen, 1988). Other studies ask women to report upon violence that occurred only within limited stages of their development (e.g., childhood; Merrill, Thomsen, Sinclair, Gold, & Milner, 2001; adulthood; Gelles & Harrop, 1989). Finally, victims’ histories of violence are often dichotomized into either single-type or multi-type exposure (i.e. exposure to two or more types). Those rather time-limited or category-limited approaches to assessing women’s history of violence exposure then constrain the conclusions that researchers can draw about the effect of multiple types of exposure across women’s broader development. In order to address the limitations of previous work, the current study asked a diverse community sample of women about multiple types of violence exposures (e.g., physical abuse, sexual abuse, witnessing violence) across their entire lifetime.
Emotional Nonacceptance
The term emotional nonacceptance describes how people relate to their internal experiences of emotions. In particular, emotional nonacceptance reflects a general unwillingness to experience emotions (sometimes referred to experiential avoidance; Hayes et al., 2004), including efforts to avoid emotional states (e.g., efforts to avoid fear that may, in turn, increase fear) and the experience of secondary negative emotions in response to primary emotions (e.g., feeling ashamed about being upset; Gratz & Roemer, 2004). Though several studies document positive correlations between emotional nonacceptance and psychopathology (e.g., Soenke, Hahn, Tull, & Gratz, 2010; Vujanovic, Youngwirth, Johnson, & Zvolensky, 2009), emotional nonacceptance describes how people relate to their own internal experiences of emotions distinct from psychiatric symptoms per se (Hayes et al., 2004).
While the construct of emotional nonacceptance did not originate from studies of trauma-exposed individuals, recent research indicates that individuals exposed to traumatic events (including interpersonal violence) report higher levels of emotional nonacceptance than their non-exposed peers (Polusny, Rosenthal, Aban, & Follette, 2004; Tull, Barnett, McMillian, & Roemer, 2007). Well-known models for the treatment of interpersonal trauma (e.g., Herman, 1992; Linehan, 1993) suggest that emotional nonacceptance may be a learned response to the overwhelming stress and pain associated with chronic trauma or victimization. If so, more chronic or frequent experiences of violence (i.e. greater cumulative violence exposure) should be linked with greater emotional acceptance. To date, however, studies examining emotional nonacceptance among trauma-exposed individuals (e.g., Gratz, Bornovalova, Delany-Brumsey, Nick, & Lejuez, 2007; Tull et al., 2007; Valentiner, Foa, Riggs, & Gershuny, 1996) have not specifically tested whether greater cumulative trauma exposure does indeed predict greater emotional nonacceptance.
Though emotional nonacceptance may be adaptive under some conditions (e.g., for limited periods of time; while surviving a trauma), more chronic and cross-situational nonacceptance may be less helpful and perhaps even harmful in the long run (Gross & John, 2003; Herman, 1992; Linehan, 1993). For example, emotional nonacceptance used chronically and inflexibly may undermine a survivor’s ability to use emotions for a host of critical functions (e.g., communication). Past research has documented links between traumatic experiences, emotional nonacceptance, and trauma-related psychopathology, though this research has been largely limited to samples of college students (e.g., Jain et al., 2007; Polusny et al., 2004) or clinical (i.e. treatment-seeking) populations (e.g., Gratz et al., 2007; Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006). Thus, the current study aimed to extend previous work by testing emotional nonacceptance as a mediator of the link between cumulative violence exposure and mental health outcomes in a racially/ethnically heterogeneous and non-treatment seeking community sample of women.
Hypotheses and Planned Analyses
We hypothesized that women’s exposure to more types of violence – referred to here as cumulative violence exposure - would predict greater severity of depression, dissociation, and PTSD symptoms. Furthermore, we hypothesized that this relationship would be mediated by victims’ emotional nonacceptance. Figure 1 provides a collapsed representation of the three separate models that we tested for the prediction of depression, dissociation, and PTSD symptoms among victims. To estimate and test the significance of the mediation effect for each model, we used bootstrapping procedures outlined by Hayes (2009) and Preacher and Hayes (2008). Several recent simulation studies have demonstrated bootstrapping procedures to be one of the most valid and powerful methods for testing mediation effects (e.g., MacKinnon, Lockwood, & Williams, 2004; Williams & MacKinnon, 2008). Specifically, to test each mediation model, we ran the Preacher and Hayes (2008) macro within the Predictive Analytics SoftWare (PASW) – Version 19.0. Using a total of 5,000 bootstrapping samples, the macro estimated each path of the models, obtaining bias-corrected and accelerated confidence intervals that were set to 95% (BCa95%CIs).
Figure 1.
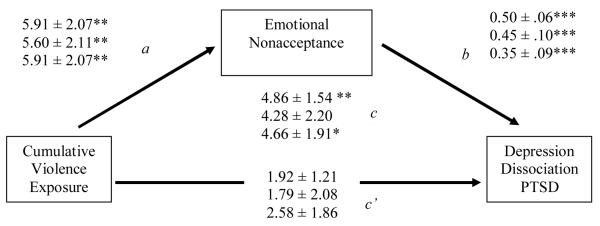
Collapsed results of three separate models to test mediation. Separate models were tested for each symptom outcome: 1) Depression, 2) Dissociation, and 3) PTSD. Values on paths represent unstandardized beta coefficients +/− the standard error of the coefficient. c = total effect (cumulative violence exposure affects symptom severity); ab = total indirect effect (cumulative violence exposure affects symptom severity through emotional nonacceptance); c’ = direct effect (cumulative violence exposure affects symptom severity after accounting for the indirect effect through emotional nonacceptance). Adapted from Preacher and Hayes (2008).
† p < .10*, p <.05; **, p < .01; ***, p < .001.
Method
Participants
Participants (N = 93) included women recruited as part of a larger “Violence Against Women” study. Participants were recruited from the following places: 53% responded to flyers at community agencies (e.g., mental health clinics, police departments, public housing shelters, social service agencies); 37% responded to web-based postings; and 10% received information from friends or family members. To be included in the larger study, a participant had to report at least one childhood violence exposure, in the form of physical and/or sexual abuse before age 14, or a recent exposure in adulthood to interpersonal violence. Exclusion criteria for the larger study included suicide attempts and/or hospitalizations for psychiatric reasons within the six months previous to the assessment.
Measures
Cumulative Violence Exposure
Cumulative violence exposure was assessed via a two-stage interview strategy adopted from the National Crime Victims Survey (see Fisher & Cullen, 2000). First, interviewers asked basic screening questions about women’s lifetime exposures to interpersonal violence, including physical abuse, sexual abuse, verbal abuse, and witnessing domestic violence. Second, interviewers asked more detailed questions about any endorsed exposures to violence. Women’s responses were then coded into four basic types of interpersonal victimization: verbal abuse including emotional and psychological violence, physical abuse/assault, sexual abuse/assault, and witnessing domestic violence. A Cumulative Violence Exposure variable was created to represent the sum of types of exposures that women had experienced.
Emotional Nonacceptance
The 16-item version of the self-report questionnaire, the Acceptance and Action Questionnaire (AAQ; Hayes et al., 2004), assessed emotional nonacceptance. Example items include: “It’s OK to feel depressed or anxious” (reverse scored), “I’m not afraid of my feelings” (reverse scored), “Anxiety is bad”, and “I try hard to avoid feeling depressed or anxious”. Participants responded to all items along a Likert-type scale of “1 = Never True” to “7 = Always True”. Higher scores indicated greater emotional nonacceptance. The 16-item version of the AAQ has demonstrated reliability and validity across a variety of samples (Bond & Bunce, 2003; Hayes et al., 2004). Cronbach’s alpha for the AAQ in the current sample was adequate (αAAQ= .77).
Symptom Severity
All symptoms were assessed via self-report questionnaires. Depression symptoms were assessed with the 21-item Beck Depression Inventory – Second Edition (BDI-II; Beck, Steer, & Brown, 1996). Women rated their experience of depression symptoms (0 = Low Severity to 3 = High severity) in the two weeks immediately prior to the assessment. The BDI-II has demonstrated excellent reliability and validity across a variety of samples (e.g., Beck, Steer, & Brown, 1996; Grothe et al., 2005). Cronbach’s alpha for the BDI-II was excellent in the current sample (αBDI = .90). Dissociation symptoms were assessed with a widely used 28-item questionnaire that has demonstrated reliability and validity, the Dissociative Experiences Scale (DES; Bernstein & Putnam, 1986). Women rated their experience of dissociation symptoms (0 = Low Severity to 100 = High Severity. Cronbach’s alpha for the DES was excellent in the current sample (αDES = .93). Finally, PTSD symptoms were assessed with the 49-item Post-traumatic Stress Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997).The PDS was designed to assess for PTSD as the disorder is defined by the criteria listed within the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev; DSM-IV-TR; American Psychiatric Association, 2000). Cronbach’s alpha for the PDS was excellent within the current sample (αPDS = .93).
Procedure
A university-based Institutional Review Board reviewed and approved all study procedures. Potential participants contacted the researchers and responded to screener questions via phone to assess inclusion/exclusion criteria. Women who met criteria for the study were invited to an in-person testing session conducted by a graduate student in a university lab setting. Consent information was provided in writing and verbally; participant understanding of consent information was assessed with a quiz. Following consent procedures, participants completed both written and verbally administered self-report questionnaires as well as several behavioral tasks that were part of the larger study. At assessment completion, participants were debriefed and compensated monetarily for their time.
Results
The mean age of participants was 30.70 years (SD = 6.18). Of the eighty-three participants who reported racial or ethnic group identification, 63% were White, 19% were Hispanic/Latina, 16% were Black, 10% were “Other”, 3% were Asian/ Asian-American, and 1% were Native American/ Alaska Native. In terms of highest level of education, 18.0% of participants had completed some grade school up to part of high school, 15.7% obtained a high school diploma, 42.7% completed partial college or specialized training, 13.5% obtained a college degree, and 10.1% had some graduate or professional training. Finally, participants provided the following income information: 40.7% <$10,000; 12.3% $10,000-$20,000; 14.8% $20,000-$30,000; 9.9% $30,000-$40,000; 6.2% $40,000-$50,000; 16.0% >$50,000.
Four of the ninety-three participants (4.3%) did not complete the measures. Thus, the data that we present in the current study is collected from a sample of eighty-nine participants. Further, analyses involving Dissociation only included eighty-seven participants due to incomplete data on the DES for two participants. All variables were examined for violations of statistical assumptions underlying the proposed analyses. Two participants’ scores on the DES were outliers, which were defined as greater or less than three standard deviations above the mean for the Dissociation variable. However, correction of outliers was deemed inappropriate given that the variable did not display significant non-normality and the outlying values appeared to represent accurate reporting.1 Participants reported lifetime exposures to violence in the range of 1 to 4 exposures (M(SD) = 2.06 (0.65)). Descriptive statistics for emotional nonacceptance and symptoms of depression, dissociation, and PTSD were as follows: M (SD) = 65.97 (13.05) (AAQ); 14.71 (9.82) (BDI-II), 18.30 (13.38) (DES), and 19.61(11.91) (PDS).
Table 1 displays Pearson zero-order correlation coefficients for all bivariate relationships between the variables used in the bootstrapping procedures. All results are based on two-tailed tests of significance. Finally, both Table 2 and Figure 1 display the results of bootstrapping procedures used to test our primary hypotheses that emotional nonacceptance would mediate the relationship between cumulative violence exposures and severity of depression, dissociation, and PTSD symptoms. As indicated in Table 2, all models of symptom severity (Depression, Dissociation, and PTSD) were statistically significant. Table 2 also displays the bias-corrected and accelerated 95% confidence intervals (BCa(95%CIs)) that were estimated for the ab pathways (i.e. indirect pathways) of all models. Consistent with mediation by Emotional Nonacceptance for all models, no BCa(95%CI) crossed zero. A BCa(95%CI) that does not cross zero indicates that the difference between the c pathway (i.e. the total direct effect) and the c’ pathway (i.e. the total indirect effect) in each model was statistically different from zero.
Table 1.
Pearson Correlation Coefficients Between All Variables Used in Bootstrapping Procedures
| Cumulative Violence Exposure |
Emotional Nonacceptance |
Depression | Dissociation | PTSD | |
|---|---|---|---|---|---|
| Cumulative Violence Exposure |
-- | .29*** | .32** | .21† | .25* |
| Emotional Nonacceptance |
-- | .70*** | .46** | .43*** | |
| Depression | -- | .54*** | .53*** | ||
| Dissociation | -- | .52*** | |||
| PTSD | -- |
p < .10
p < .05
p < .01
p < .001
Table 2.
Bias Corrected and Accelerated 95% Confidence Intervals (BCa 95% CIs) for the Total Indirect Effect (ab) of Each Model
| Depression (n = 89) | Dissociation (n = 87) | PTSD (n = 89) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| BCa 95% CI | BCa 95% CI | BCa 95% CI | |||||||
|
| |||||||||
| Effect | Point Estimate |
Lower | Upper | Point Estimate |
Lower | Upper | Point Estimate |
Lower | Upper |
| ab | 2.94 | .76 | 5.02 | 2.49 | .77 | 4.82 | 2.08 | .04 | 1.03 |
Figure 1 also displays additional results of the bootstrapping procedures: the estimates of unstandardized beta coefficients and standard error (b ± (SE(b)) for each pathway (a, b, c, and c’). As Figure 1 indicates, regression coefficients for the a pathways (from Cumulative Violence Exposure to Emotional Nonacceptance), the b pathways (from Emotional Nonacceptance to Depression, Dissociation, or PTSD), and the c pathways (from Cumulative Violence Exposure to Depression, Dissociation, or PTSD) were significant and in the expected positive direction for all models. Also consistent with mediation by Emotional nonacceptance, the regression coefficients for the c’ pathways (from Cumulative Violence Exposure to Depression, Dissociation, or PTSD, after specifically accounting for Emotional Nonacceptance) were nonsignificant.
Discussion
The current study examined relationships between cumulative violence exposure, emotional nonacceptance, and three types of symptoms (depression, dissociation, PTSD) in a community sample of women. Consistent with past research on the deleterious effects of cumulative victimization (e.g., Follette et al., 1996; Green et al., 2000), greater cumulative violence exposure predicted greater mental health symptom severity across symptoms of depression, dissociation, and PTSD. Also, consistent with past research from acceptance-based models of psychopathology (e.g., Hayes et al., 2004; Vujanovic et al., 2009), higher levels of emotional nonacceptance among victims predicted greater symptom severity across all symptoms. Finally, consistent with the current study’s hypotheses and suggestions from the trauma treatment literature (e.g., Herman, 1992), greater cumulative violence exposure predicted greater emotional nonacceptance.
The particular symptoms that we examined within the current study, depression, dissociation, and PTSD, are central to the phenomena of complex trauma among chronically victimized individuals (e.g., Cook et al., 2005; DePrince, Chu, & Pineda, 2011). Results of bootstrapping procedures supported emotional nonacceptance as a mediator of the relationships between cumulative violence exposure and symptom severity for all symptoms. Thus, the current results also point to the need for continued research regarding the role that emotional nonacceptance plays in either the development and/or maintenance of complex trauma responses. Within the current study, and consistent with Hayes and colleagues (2004), we viewed emotional nonacceptance as a description of how people relate to their own internal experiences of emotions distinct from psychiatric symptoms per se. Future research, utilizing longitudinal assessment of those constructs, will be critical in continuing to establish how emotional nonacceptance is best characterized in relation to psychopathology.
Though these cross-sectional data prohibit establishing temporal precedence and inferring causality, previous theory (e.g., Linehan, 1993) and empirical evidence (e.g., Gratz et al., 2007; Segal, Williams, & Teasdale, 2001) informed our a priori hypotheses of mediation. Results are consistent with those hypotheses: greater cumulative violence exposure leads to increased emotional nonacceptance, which in turn contributes to more severe mental health symptoms among victims. Nevertheless, future longitudinal studies should attempt to replicate these findings in order to provide more direct support for our particular model and to rule-out alternative models. For instance, increased symptom severity also increases risk for future victimization (e.g., Cloitre, 1998), and that path was not represented in the models of symptoms that we tested. While highly complex and transactional relationships among variables are often difficult to establish statistically, research designs that are prospective, longitudinal, and can manipulate a variable of interest (e.g., training in psychotherapies that emphasize emotional acceptance) will be a critical next step in understanding women’s responses to cumulative violence exposure.
The results of this study should be interpreted in light of two additional limitations. First, the current study relied exclusively on self-report measures. Due to shared method variance, results may overestimate relationships between variables. The correlation between depression and emotional nonacceptance was strong, and consistent with results of other studies relating several versions of the AAQ to the BDI (e.g., Bond et al., 2011; Bond & Bunce, 2000). Previous studies also provide ample evidence that the constructs of emotional nonacceptance and depression, as measured respectively by various versions of the AAQ and BDI, display substantive (versus merely tautological) associations (Bond et al., 2011; Forsyth, Parker, & Finlay, 2003). Future research should strive for a multi-method approach, especially when assessing constructs that may demonstrate fairly high overlap such as emotional nonacceptance and trauma-related symptoms. Second, all participants in the study were adult women. Future research should explore whether this study’s results generalize to different populations of individuals (e.g., males, children, or adolescents). Some research has suggested that male and female victims of interpersonal violence differ in terms of the mental health outcomes they experience (e.g., see Putnam, 2003 for a review of gender differences in sexual abuse survivors), but other research finds little evidence for those gender differences (e.g., Dube et al., 2005).
Despite the limitations of the current study, findings highlight the need for future longitudinal research projects that can test causal relationships between the experiences of cumulative violence, emotional nonacceptance, and mental health outcomes. To the extent that emotional nonacceptance is indeed a mechanism through which cumulative violence influences the development of mental health symptoms, avenues for intervention can be explored. Current psychotherapies that train individuals in improving their capacity for emotional acceptance, such as mindfulness- and acceptance-based psychotherapies (e.g., Kabat-Zinn, 2003) have already shown success in reducing a host of psychological symptoms, including anxiety (Kabat-Zinn, Massion, Kristeller, & Peterson, 1992), depression (e.g., Forman, Herbert, Moitra, Yeomans, & Geller, 2007), dissociation (e.g., Kimbrough Magyari, Langenberg, Chesney, & Berman, 2011), and PTSD (e.g., Nakamura, Lipschitz, Landward, Kuhn, & West, 2011; Orsillo & Batten, 2005).
Acceptance-based therapies, and the accompanying improvements in capacity to tolerate and engage (rather than avoid, which might increase) painful emotional experiences, might be especially relevant for victims of chronic exposure to violence. However, acceptance-based therapies have been explored to a relatively less thorough degree among such populations given the real challenges and barriers to treatment that victims of ongoing interpersonal violence may initially face. For example, victims may still be experiencing chronic stressors within their environment that require attention first or may need to utilize emotional nonacceptance as part of their survival in the context of ongoing threats. As has long been observed in the trauma treatment literature, addressing safety should precede other psychological interventions (Herman, 1992). Once safety is established, efforts to address emotional nonacceptance should include talking with clients about emotional nonacceptance as an understandable attempt to protect oneself from overwhelming and painful emotions. Clients should not be blamed for the actions of perpetrators or the use of cognitive and emotional strategies, such as emotional nonacceptance, to navigate abuse relationships. In the presence of safety and the absence of victim blaming, we see addressing and working to enhance emotional acceptance among victims of chronic violence as a potential path towards increasing tools for client empowerment and mental health.
Acknowledgments
Thanks to current and former members of the Traumatic Stress Studies Group at the University of Denver. This research was supported by the National Institute of Mental Health grant MH079769, the International Society for Traumatic Stress Studies Student Research Grant, the International Society for the Study of Trauma and Dissociation David Caul Graduate Research Award to Ann T. Chu, and the University of Denver Professional Opportunities for Faculty to Anne P. DePrince.
Footnotes
To ensure the accuracy of the decision to not correct outliers, we performed comparisons of results with and without the outliers for all analyses involving Dissociation. Results were nearly identical, with all pathways estimated as very similar numerical values and signs and with no changes in statistical significance of findings.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. The Journal of Nervous and Mental Disease. 1986;174(12):727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Devins G. Mindfulness: A proposed operational definition. Clinical Psychology: Science And Practice. 2004;11(3):230–241. [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Bond FW, Bunce D. The role of acceptance and job control in mental health, job satisfaction, and work performance. Journal of Applied Psychology. 2003;88(6):1057–1067. doi: 10.1037/0021-9010.88.6.1057. [DOI] [PubMed] [Google Scholar]
- Bond FW, Bunce D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. Journal of Occupational Health Psychology. 2000;5:156–163. doi: 10.1037//1076-8998.5.1.156. [DOI] [PubMed] [Google Scholar]
- Calvete E, Corral S, Estevez A. Cognitive and coping mechanisms in the interplay between intimate partner violence and depression. Anxiety, Stress, and Coping. 2007;20(4):369–382. doi: 10.1080/10615800701628850. [DOI] [PubMed] [Google Scholar]
- Cloitre M. Sexual revictimization: Risk factors and prevention. In: Follette VM, Ruzek JI, Abueg FR, Follette VM, Ruzek JI, Abueg FR, editors. Cognitive-behavioral therapies for trauma. Guilford Press; New York, NY US: 1998. pp. 278–304. [Google Scholar]
- Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH. Physical and mental health effects of intimate partner violence for men and women. American Journal of Preventive Medicine. 2002;23(4):260–268. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- Cook A, Spinazzola J, Ford J, Lanktree C, Blaustein M, Cloitre M, van der Kolk B. Complex trauma in children and adolescents. Psychiatric Annals. 2005;35(5):390–398. [Google Scholar]
- Crouch JL, Hanson RF, Saunders BE, Kilpatrick DG, Resnick HS. Income, race/ethnicity, and exposure to violence in youth: Results from the national survey of adolescents. Journal of Community Psychology. 2000;28(6):625–641. [Google Scholar]
- DePrince AP, Chu AT, Pineda AS. Links between specific posttrauma appraisals and three forms of trauma-related distress. Psychological Trauma: Theory, Research, Practice, and Policy. 2011 May 2; Advance online publication. doi: 10.1037/a0021576. [Google Scholar]
- Dube SR, Anda RF, Whitfield CL, Brown DW, Felitti VJ, Dong M, Giles WH. Long-term consequences of childhood sexual abuse by gender of victim. American Journal of Preventive Medicine. 2005;28(5):430–438. doi: 10.1016/j.amepre.2005.01.015. [DOI] [PubMed] [Google Scholar]
- Fisher BS, Cullen FT. Measuring the sexual victimization of women: Evolution, current controversies, and future research. Criminal Justice. 2000;4:317–390. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9(4):445–451. [Google Scholar]
- Follette VM, Polusny MA, Bechtle AE, Naugle AE. Cumulative trauma: The impact of child sexual abuse, adult sexual assault, and spouse abuse. Journal of Traumatic Stress. 1996;9(1):25–35. doi: 10.1007/BF02116831. [DOI] [PubMed] [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31(6):772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Forsyth JP, Parker JD, Finlay CG. Anxiety sensitivity, controllability and experiential avoidance and their relation to drug of choice and addiction severity in a residential sample of substance-abusing veterans. Addictive Behaviors. 2003;28(5):851–870. doi: 10.1016/s0306-4603(02)00216-2. [DOI] [PubMed] [Google Scholar]
- Gelles RJ, Harrop JW. Violence, battering, and psychological distress among women. Journal of Interpersonal Violence. 1989;4(4):400–420. [Google Scholar]
- Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14(2):99–132. [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, Lejuez CW. A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behavior Therapy. 2007;38(3):256–268. doi: 10.1016/j.beth.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology & Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Gratz KL, Rosenthal M, Tull MT, Lejuez CW, Gunderson JG. An experimental investigation of emotion dysregulation in borderline personality disorder. Journal Of Abnormal Psychology. 2006;115(4):850–855. doi: 10.1037/0021-843X.115.4.850. [DOI] [PubMed] [Google Scholar]
- Green BL, Goodman LA, Krupnick JL, Corcoran CB, Petty RM, Stockton P, Stern NM. Outcomes of single versus multiple trauma exposure in a screening sample. Journal Of Traumatic Stress. 2000;13(2):271–286. doi: 10.1023/A:1007758711939. [DOI] [PubMed] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal Of Personality And Social Psychology. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Grothe KB, Dutton GR, Jones GN, Bodenlos J, Ancona M, Brantley PJ. Validation of the Beck Depression Inventory-ii in a low-income African American sample of medical outpatients. Psychological Assessment. 2005;17(1):110–114. doi: 10.1037/1040-3590.17.1.110. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, McCurry SM. Measuring experiential avoidance: a preliminary test of a working model. The Psychological Record. 2004;54(4):553–578. [Google Scholar]
- Herman J. Trauma and recovery. Basic Books; New York, NY US: 1992. [Google Scholar]
- Jain S, Shapiro SL, Swanick S, Roesch SC, Mills PJ, Bell I, Schwartz GR. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Annals of Behavioral Medicine. 2007;33(1):11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice. 2003;10:144–156. [Google Scholar]
- Kabat-Zinn J, Massion AO, Kristeller J, Peterson LG. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. The American Journal of Psychiatry. 1992;149(7):936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Saunders BE, Smith DW. Youth victimization: Prevalence and implications: Findings from the National Survey of Adolescents. U.S. Department of Justice; Washington, DC: 2003. [Google Scholar]
- Kimbrough E, Magyari T, Langenberg P, Chesney M, Berman B. Mindfulness intervention for child abuse survivors. Journal Of Clinical Psychology. 2010;66(1):17–33. doi: 10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive - behavioral treatment of borderline personality disorder. Guilford Press; New York: 1993. [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marhoefer-Dvorak S, Resick PA, Hutter CK, Girelli SA. Single-versus multiple-incident rape victims: A comparison of psychological reactions to rape. Journal of Interpersonal Violence. 1988;3(2):145–160. [Google Scholar]
- Merrill LL, Thomsen CJ, Sinclair BB, Gold SR, Milner JS. Predicting the impact of child sexual abuse on women: The role of abuse severity, parental support, and coping strategies. Journal of Consulting and Clinical Psychology. 2001;69(6):992–1006. doi: 10.1037//0022-006x.69.6.992. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ. The role of childhood sexual abuse sequelae in the sexual revictimization of women: An empirical review and theoretical reformulation. Clinical Psychology Review. 2003;23(4):537–571. doi: 10.1016/s0272-7358(02)00203-9. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ, Siegfried NJ. The revictimization of child sexual abuse survivors: An examination of the adjustment of college women with child sexual abuse, adult sexual assault, and adult physical abuse. Child Maltreatment. 2000;5(1):18–27. doi: 10.1177/1077559500005001003. [DOI] [PubMed] [Google Scholar]
- Murphy SM, Kilpatrick DG, Amick-McMullan A, Veronen LJ. Current psychological functioning of child sexual assault survivors: A community study. Journal of Interpersonal Violence. 1988;3(1):55–79. [Google Scholar]
- Nakamura Y, Lipschitz DL, Landward R, Kuhn R, West G. Two sessions of sleep-focused mind–body bridging improve self-reported symptoms of sleep and PTSD in veterans: A pilot randomized controlled trial. Journal of Psychosomatic Research. 2011;70(4):335–345. doi: 10.1016/j.jpsychores.2010.09.007. [DOI] [PubMed] [Google Scholar]
- Neumann DA, Houskamp BM, Pollock VE, Briere J. The long-term sequelae of childhood sexual abuse in women: A meta-analytic review. Child Maltreatment. 1996;1(1):6–16. [Google Scholar]
- Orsillo SM, Batten SV. Acceptance and Commitment Therapy in the treatment of Posttraumatic stress disorder. Behavior Modification. 2005;29:95–129. doi: 10.1177/0145445504270876. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Rosenthal M, Aban I, Follette VM. Experiential avoidance as a mediator of the effects of adolescent sexual victimization on negative adult outcomes. Violence and Victims. 2004;19(1):109–120. doi: 10.1891/vivi.19.1.109.33238. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Putnam FW. Ten-year research update review: Child sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(3):269–278. doi: 10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- Sappington A, Pharr R, Tunstall A, Rickert E. Relationships Among Child Abuse, Date Abuse, and Psychological Problems. Journal of Clinical Psychology. 1997;53(4):319–329. doi: 10.1002/(sici)1097-4679(199706)53:4<319::aid-jclp4>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Segal Z, Teasdale JD, Williams JG. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. Guilford Press; United States: 2001. [Google Scholar]
- Soenke M, Hahn KS, Tull MT, Gratz KL. Exploring the relationship between child abuse and analogue generalized anxiety disorder: The mediating role of emotion dysregulation. Cognitive Therapy and Research. 2010;34(5):401–412. [Google Scholar]
- Tull MT, Barnett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Valentiner DP, Foa EB, Riggs DS, Gershuny BA. Coping strategies and posttraumatic stress disorder in female victims of sexual and nonsexual assault. Journal of Abnormal Psychology. 1996;105:455–458. doi: 10.1037//0021-843x.105.3.455. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Youngwirth NE, Johnson KA, Zvolensky MJ. Mindfulness-based acceptance and posttraumatic stress symptoms among trauma-exposed adults without axis I psychopathology. Journal of Anxiety Disorders. 2009;23:297–303. doi: 10.1016/j.janxdis.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J, MacKinnon DP. Resampling and distribution of the product methods for testing indirect effects in complex models. Structural Equation Modeling. 2008;15:23–51. doi: 10.1080/10705510701758166. [DOI] [PMC free article] [PubMed] [Google Scholar]


