Abstract
Background
This survey characterized the strategies used by general dentists to manage temporomandibular muscle joint disorders (TMJD) pain, and assessed the feasibility of doing a randomized clinical trial (RCT) of the effectiveness of these strategies.
Methods
Dentists from three Practice-Based Research Networks (PBRNs) specifically, DPBRN, PEARL, NWPRECEDENT) accepted to participate in this survey.
Results
Out of 862 dentists surveyed, 654 were general dentists who treat TMJD; among these, 80.3 percent stated they would participate in a RCT. Dentists treated an average of three pain-related TMJD patients per month. Splints (97.6 percent), self-care (85.9 percent) and over-the-counter or prescribed medications (84.6 percent) were the treatments most frequently used. The preferred treatments to compare in a RCT were splint therapy (35.8 percent), self-care (27.4 percent) and medications (16.9 percent).
Conclusions
Most general dentists treat TMJD pain, and reversible initial care is typically provided. Finally, it is feasible to conduct a RCT in the PBRNs to assess the effectiveness of splint therapy, medications and/or self-care, for the initial management of painful TMJD.
Clinical Implications
There is an opportunity to do a RCT in PBRNs leading to the development of evidence-based treatment guidelines for the initial treatment of pain-related TMJD by primary care dentists.
Keywords: Temporomandibular muscle joint disorders, survey, PBRN, splint, self-care, medications
INTRODUCTION
Temporomandibular muscle and joint disorders (TMJD) (a.k.a temporomandibular disorders [TMD]) are the second most commonly occurring musculoskeletal pain condition after chronic low back pain.1 Approximately 5 to 12 percent of the U.S. population are affected by TMJD, and around half to two-thirds will seek professional care, with an annual cost estimated at $4 billion dollars.1 General dentists often are the first health care professionals to diagnose and treat patients with pain-related TMJD.
As appropriate initial therapy for the management of patients with pain, the National Institute of Dental and Craniofacial Research (NIDCR) TMD 1996 Technology Assessment Conference Statement supported patient education with self-care, pharmacological pain control, physical therapy, and splint therapy.2 The Statement also called for randomized controlled clinical trials (RCTs) to assess the effectiveness of these treatment modalities. To date, there are no reported RCTs in the United States that compared the effectiveness of these recommended initial treatments in a primary care setting. In the UK, only one RCT has been done in a primary care setting to compare a splint to a non-occluding splint.3, 4 In this study, at 1-year follow-up, 81 percent of all subjects reported good to excellent reduction in pain with either treatment, and 14 percent were referred to a TMJD specialty clinic. These findings suggest that the majority of TMJD patients are treated successfully in the primary care setting by a general dentist.
Although RCTs have been conducted in tertiary care centers, it is not clear how the results would apply in the primary care setting. This circumstance suggests a compelling need to conduct a multi-site RCT in the primary care setting with adequate sample size (power) to establish evidence-based guidelines for the initial management of TMJD pain. In 2005, the NIDCR established three dental Practice-Based Research Networks (PBRNs): 1) Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (Northwest PRECEDENT), a consortium of practices in the northwest United States;5 2) The Dental Practice-Based Research Network (DPBRN), a consortium of practices in the United States and Scandinavia;6 and 3) the Practitioners Engaged in Applied Research and Learning (PEARL) network. A three-network entity called the Collaboration on Networked Dental and Oral Research (CONDOR) was also created. The intent of these PBRNs is to connect practitioners with experienced clinical investigators to enhance the movement of clinical research evidence into daily clinical practice. This survey characterized the strategies used by CONDOR primary care dentists to manage pain-related TMJD, and assessed the feasibility of doing a RCT of the effectiveness of these strategies.
METHODS
Study design and study population
All primary care dentists in the three PBRNs: DPBRN, PEARL, and PRECEDENT were invited to participate in this survey. The inclusion criteria were: 1) had participation in at least one PBRN study previously; and 2) be a dentist practitioner-investigator (i.e., not a dental hygienist practitioner-investigator). Furthermore, only active general dentist members who treat TMJD were included in this analysis. An effort was made to ensure that the number of participating active practices would comprise at least 80 percent of the active members. Participation was voluntary. All CONDOR Institutional Review Boards approved the study protocol. The recruitment at each PBRN is described below.
DPBRN
An invitation letter was mailed to 707 DPBRN practitioner-investigators (P-Is) who met the eligibility criteria as of the date of first mailing on December 31, 2009. The letter invited practitioners to log onto a DPBRN Web site created to administer the questionnaire. The site had been tested for readability, feasibility, and internet browser compatibility by DPBRN investigators, staff, and at least one P-I in each of DPBRN’s five main regions. Of the 707 practitioners mailed an invitation letter, seven were subsequently determined to be ineligible because they were no longer in the active practice of dentistry. The DPBRN protocol allowed for up to three mailings at one-month intervals. Of these 700 P-Is, 504 (72 percent) completed the questionnaire. A total of 84 P-Is completed a paper version of the questionnaire instead of the online version. Of the 504 P-Is, 444 (95.7 percent) and 34 (85 percent) were general dentists from DPBRN US and Scandinavia, respectively. From these dentists, 363 (81.8 percent) and 31 (91.2 percent) dentists treat TMJD pain.
PEARL
practitioner investigator’s (P-I’s) were invited via email to participate in the TMJD study. The New York University School of Medicine IRB approved the TMJD survey prior to release. The email explained the nature of the study and included the Code of Federal Regulations (CFR) compliant components of the informed consent. A statement describing the process was included in the email that when activated, by a clickable link, indicated implied consent by the practitioner to participate in the survey through a web-based data entry system. The web site was open for a total of five months and a total of 130 practitioners responded to the survey. During the time the survey was open to the Network, emails and occasional telephone calls were utilized to remind the P-I’s of the opportunity to participate in the survey. There was a 62 percent response rate from the total practitioners of the PEARL Network. All responses were collected via direct remote data entry to the EMMES Corporation, the PEARL data coordinating center of Rockville, MD. The proprietary web-based data entry system of EMMES, Advantage EDC, is fully 21 CFR 11 compliant. Of the responses collected by PEARL, 105 (81 percent) of the respondents identified themselves as general dentists, 13 (10 percent) were specialists, while 12 (9 percent) did not report their type of practice. From these 105 dentists, 92 (87.6 percent) treat TMJD pain. Remuneration was provided to each P-I who completed the survey.
Northwest PRECEDENT
All general dentists from the five-state Northwest PRECEDENT region (Idaho, Montana, Oregon, Washington and Utah, n=198) and Friends of PRECEDENT (general dentists outside the 5-state region and specialists, n=67) were invited to participate, by means of a letter or an e-mail containing a brief explanation of the study and instructions about how to log on to the data-capture Web site. The Web site used to conduct the survey was open from August 20, 2009 through January 4, 2010, and attempts to increase the response rate by contacting the dentists via e-mail, letters and telephone calls were made during this period. Dentists who completed the survey received a monetary token of appreciation. The institutional review board at the University of Washington, Seattle, approved the study protocol and survey.Of the 265 dentists invited to participate in the survey, 228 (86 percent) responded. From these 228 dentists, 168 (73.7 percent) treat TMJD pain.
These dentists were distributed by their regions: Midwest (MW: Minnesota), South (SO), Scandinavia (Sc), Northeast (NE), and West. MW (n = 37) and Sc (n = 31) dentists were from DPBRN. SO dentists were from PRECEDENT (n = 4) and from DPBRN (n = 294). NE dentists were from PEARL (n = 92) and from DPBRN (n = 2). West included dentists from PRECEDENT(n = 164) and DPBRN (n = 30).
Data collection
A questionnaire was pre-tested in a survey in 2009 among CONDOR dentists. It quantifies how often dentists treat patients with TMJD pain; assesses methods used for TMJD diagnosis; evaluates the treatment modalities of TMJD pain treatment; estimates the potential number of CONDOR dentists who provide TMJD pain treatments and that would be interested in participating in a RCT; describes the study group that would be evaluated in a RCT; and documents the economic and business barriers to participation by these CONDOR dentists and patients in an eventual RCT. A copy of the full questionnaire is publicly available at http://www.dentalpbrn.org/users/publications/Supplement.aspx.
Statistical analysis
The questionnaire responses from CONDOR general dentists who treat TMJD pain were analyzed for demographics, TMJD pain diagnostics protocol, treatments and economic and business barriers. Multiple choice answers: 1) Never; 2) Sometimes; 3) Half of time; 4) Usually; and 5) Always, where merged in: 1) Never; 2) Sometimes-Half of time; and 3) Usually and always. The analyses were stratified by age (< 50 years old, ≥ 50 years old) and regions: MW, NE, SO, West, and Sc. These analyses were repeated for the subset of dentists interested in participating in a RCT. Analysis of variance and Chi-square were used to test statistical differences between dentists relative to age and regions. A P-value less than .05 was considered statistically significant (SAS 9.2, SAS Institute, Cary, N.C.).
RESULTS
Of the 654 general dentists who reported currently treating TMJD, 76.5 percent were male, 85.8 percent were white and their mean age was 50.5 (standard deviation = 10.7) years. More than 80 percent had practiced dentistry for more than 10 years, 85.2 percent reported that their practice sees more than 30 patients per month, and 154 (27.9 percent) were in private solo practices. Statistically significant differences were found on the demographic characteristics and clinical practice between dentists by region (Table 1).
Table 1.
Characteristics of 654 CONDOR general dentists who treat TMJD pain, by region.†
| CHARACTERISTIC | MIDWEST (MW) |
NORTHEAST (NE) |
WEST | SOUTH (SO) |
SCANDINAVIA (Sc) |
P-value |
|---|---|---|---|---|---|---|
|
| ||||||
|
| ||||||
| n = 37 (5.7%) |
n = 94 (14.4%) |
n = 194 (29.7%) |
n = 298 (45.6%) |
n = 31 (4.7%) |
||
|
More than 30
patients/week, no. (%) |
27 (79.4) | 89 (95.7) | 134 (87.0) | 190 (79.5) | 26 (96.3) | .001 |
|
Practicing > 10 years,
no. (%) |
29 (78.4) | 86 (91.5) | 137 (72.9) | 264 (88.9) | 25 (80.7) | <.0001 |
| Male, no. (%) | 24 (64.9) | 69 (73.4) | 147 (78.6) | 241 (80.9) | 14 (45.2) | <.0001 |
| Mean age (SD‡) | 49.6 (11.1) | 52.5 (9.5) | 46.6 (13.0) | 51.7 (10.8) | 49.7 (9.9) | <.0001 |
| Caucasian, no. (%) | 35 (94.6) | 76 (80.9) | 147 (75.8) | 273 (91.6) | 30 (96.8) | <.0001 |
Percentage of missing data < 1%; because of rounding, percentages may not add up to 100%.
SD: Standard deviation.
TMJD diagnostic protocol
Dentists treated an average of three pain-related TMJD patients per month (95 percent confidence interval [CI], 2.7-3.3) with no significant difference across regions (P = .87) or dentists’ age (P = .95). The most common symptoms recalled by the dentistwere that their patients usually or always reported jaw pain (76.0 percent), headache (51.2 percent) and facial pain (50.8 percent).
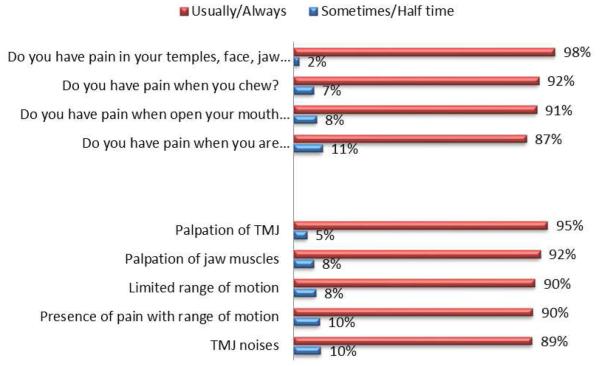
To diagnose pain-related TMJD, 93.9 percent dentists used both a history and exam protocol; the frequency of the specific questions and exam items used are shown in Figure 1. The diagnostic protocol was not significantly different between dentists’ age (P = .31), but WEST dentists use the physical exam less frequently (85.6 percent) than dentists from other regions (96-100 percent).
Figure 1. Frequency of the specific questions and exam items used to diagnose TMJD.
Note: The sum of percentages may be less than 100% because the answer “Never” is not presented.
Treatments provided for pain-related TMJD
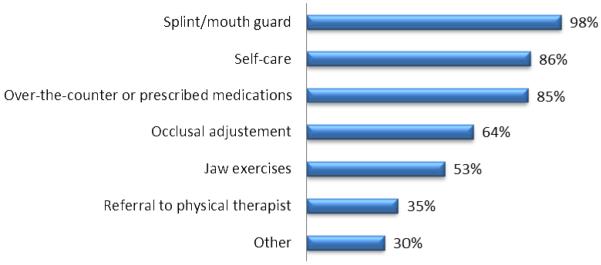
The most common treatments were splints (97.6 percent), self-care (85.9 percent) and over-the-counter or prescription medications (84.6 percent). Other treatments used are described in Figure 2.
Figure 2. Most frequently used treatments for pain-related TMJD.
Note: Dentists could select more than one treatment.
Splint therapy was the most frequently used treatment in all regions (P = .71). Dentists < 50 years old (100 percent) and dentists > 50 years old (96.6 percent; P = .001) use splints frequently. Hard acrylic custom stabilization splint was the most commonly used splint (n = 390, 60.1 percent), followed by the soft custom splint (n = 85, 13.3 percent). Soft over-the-counter mouth guards (n = 16, 2.5 percent), anterior repositioning splint (n = 25, 4.0 percent), and nociceptive trigeminal inhibition splint (n = 48, 7.5 percent) were rarely used.
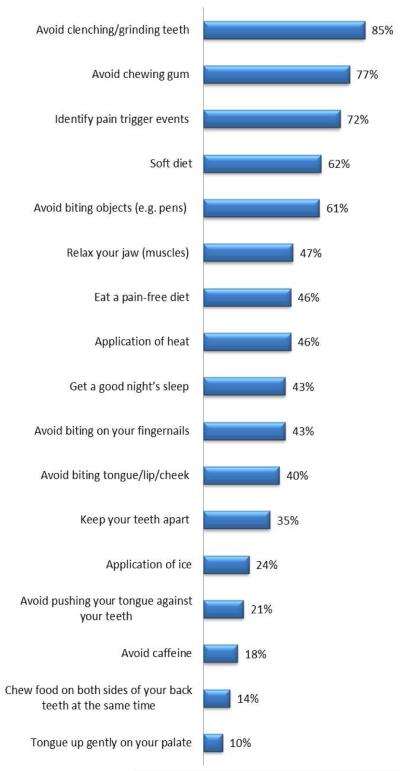
Dentists frequently use over-the-counter and prescription medications or self-care, independent of dentists’ age (Pmedication = .07 and Pself-care = .25). Over-the-counter ibuprofen was the medication most frequently used (Table 2). Figure 3 shows the use of specific self-care strategies. Significant differences were noted on the use of medications and self-care between regions (Table 3).
Table 2.
Medications recommended or prescribed for treating pain-related temporomandibular muscle joint disorders (TMJD).*†
| MEDICATIONS | NEVER | SOMETIMES | USUALLY OR ALWAYS |
|---|---|---|---|
| No. (%) | No. (%) | No. (%) | |
| Acetaminophen † | 287 (44.7) | 319 (49.7) | 36 (5.6) |
| Aspirin † | 452 (70.9) | 171 (26.8) | 15 (2.3) |
| Ibuprofen † | 28 (4.3) | 257 (39.7) | 363 (56.0) |
| Naprosyn † | 237 (36.9) | 305 (47.4) | 101 (15.7) |
| Prescription aspirin | 588 (92.5) | 44 (6.9) | 4 (0.6) |
|
Prescription
ibuprofen |
299 (46.6) | 241 (37.5) | 102 (15.9) |
|
Prescription
naprosyn |
444 (69.5) | 164 (25.6) | 31 (4.9) |
|
Low dose tricyclic
antidepressants |
576 (89.6) | 66 (10.3) | 1 (0.2) |
| Muscle relaxants | 186 (28.6) | 394 (60.6) | 70 (10.8) |
| Opioid-Tram | 510 (79.6) | 130 (20.3) | 1 (0.1) |
| Other opioid | 493 (76.9) | 145 (22.6) | 3 (0.5) |
Percentage of missing data < 2%
because of rounding, percentages may not add up to 100%.
Over-the-counter.
Figure 3. Components of self-care usually or always recommended for patients with pain-related TMJD.
Note: Percentage of missing data < 2%.
Table 3.
Used treatment for TMJD pain: Distribution by region.†
| MIDWEST (MW) |
NORTHEAST (NE) |
WEST | SOUTH (SO) |
SCANDINAVIA (Sc) |
P-value | |
|---|---|---|---|---|---|---|
| Splint, no. (%) | 37 (100) | 93 (98.9) | 188 (96.9) | 290 (97.3) | 30 (96.8) | 0.71 |
|
Over-the-counter
medication, no.(%) |
27 (73.0) | 88 (93.6) | 165 (85.1) | 256 (85.9) | 17 (54.8) | <.0001 |
| Self-care, no. (%) | 34 (91.9) | 91 (96.8) | 170 (87.6) | 252 (84.6) | 15 (48.4) | <.0001 |
|
Occlusal
treatment, no. (%) |
18 (48.7) | 64 (68.1) | 102 (52.6) | 214 (71.8) | 18 (58.1) | <.0001 |
Percentage of missing data < 1%.
Occlusal adjustment was another option frequently reported for the treatment of pain-related TMJD (63.6 percent), with dentists ≥ 50 years old (67.1 percent) using it more than dentists < 50 years old (59.9 percent; P = .06). Significant differences were noted on the use of medications and self-care between regions (Table 3). Most of these dentists also use splint (98.8%), self-care (65.0%) or over-the-counter or prescription medications (64.4%).
Responses of dentists willing to participate in a randomized controlled trial
Most of 654 dentists (80.3 percent) treating TMJD were willing to participate in a RCT to assess the best initial treatment for pain-related TMJD. These dentists were mostly males and white, although differences were found between those willing to participate (Males = 78.8 percent; White = 87.2 percent) and those who would not (Males = 66.9 percent; P = .005; White = 79.8 percent; P = .03). No significant differences were found between the age (P = .88), practice size (P = .97), years of practice (P = .82) or region (P = .19) of those willing to participate and those who would not.
These 525 dentists preferred to randomly assign patients to different treatments (87.6 percent) than to a placebo (53.9 percent) or to no-treatment (49.9 percent) groups (this sum is higher than 100 percent because dentists could assign patients to multiple groups). The preference to assign patients to different treatments (P = .63) or to placebo (P = .09) was not significantly different across dentists’ age; however, dentists below 50 years old preferred to assign patients to no treatment (n = 115; 55.6 percent) more often than dentists > 50 years old (n = 140; 45.9 percent; P = .03). Significant differences were noted between regions (Table 4).
Table 4.
Planning for a randomized clinical trial (RCT): Distribution by region for preferred comparison groups and initial treatment for patients with pain-related temporomandibular muscle joint disorders (TMJD).†
| MIDWEST (MW) |
NORTHEAST (NE) |
WEST | SOUTH (SO) |
SCANDINAVIA (Sc) |
P- value |
|
|---|---|---|---|---|---|---|
|
| ||||||
| n = 27 (73%) |
n = 81 (86.2%) |
n = 148 (76.3%) |
n = 245 (82.2%) |
n = 24 (77.4%) |
||
| Preferred study design for a RCT | ||||||
|
| ||||||
|
Comparison of
different treatments, no. (%) |
24 (88.9) | 77 (95.1) | 135 (91.8) | 203 (82.9) | 20 (83.3) | 0.02 |
|
Include placebo
group, no. (%) |
12 (44.0) | 50 (61.7) | 98 (68.1) | 110 (44.9) | 11 (45.8) | 0.0001 |
|
Include “no
treatment” group, no. (%) |
12 (44.4) | 41 (50.6) | 87 (60.4) | 109 (44.5) | 11 (45.8) | 0.045 |
|
| ||||||
| Preferred initial treatment for TMJD pain | ||||||
|
| ||||||
| Splint, no. (%) | 10 (37.0) | 63 (77.8) | 110 (74.3) | 165 (67.4) | 17 (70.8) | 0.001 |
|
Over-the-counter
medication, no. (%) |
20 (74.1) | 73 (90.1) | 106 (71.6) | 154 (62.9) | 5 (20.8) | <.0001 |
| Self-care, no. (%) | 25 (92.6) | 73 (90.1) | 126 (85.1) | 188 (76.7) | 14 (58.3) | 0.0007 |
Percentage of missing data < 1%.
In addition, a significant difference was noted on the methods of diagnosing TMJD pain between dentists willing to participate in a RCT and those unwilling (P = .03). The physical exam is used more often by the willing dentists (95.1 percent) than those unwilling to participate (89.9 percent).
The majority of the 525 dentists currently use splint therapy (98.1 percent), over-the-counter medication (86.1 percent) and self-care (87.8 percent) for the treatment of pain-related TMJD.
Preferred treatments for the initial treatment of painful TMJD were splint therapy (69.5 percent), over-the-counter medication (68.2 percent) and self-care (81.4 percent), followed by jaw massage (38.9 percent), jaw exercises (36.0 percent), prescription medication (33.9 percent), or no preference (1.4 percent). No significant difference was noted on the preferred initial treatment across dentists’ age (P > .05). As shown in Table 4, dentists from all regions frequently preferred splint therapy, other than MW. Self-care or over-the-counter medications were also preferred treatments in all USA regions, but not in Scandinavia.
When asked which treatments the 525 dentists would like to compare in a RCT, splint (35.8 percent), self-care (27.4 percent), medications (17.0 percent) and exercises (15.1 percent) were the most selected. The preferred pairs of treatments out of 21 possible pairs from seven treatments were: splint and medication (n = 140; 26.7 percent), splint and jaw exercises (n = 99; 18.9 percent); splint and self-care (n = 97; 18.5 percent); and self-care and medication (n = 59; 11.2 percent). The frequencies of all other combinations were below 8 percent.
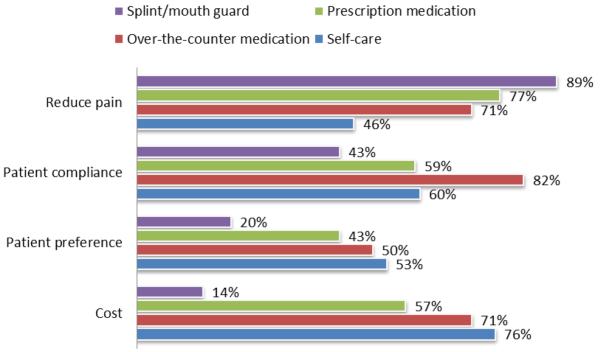
When asked why dentists had selected the specific treatments above, they indicated that splints were the best treatment to reduce pain (Figure 4), but were costly (n = 103; 56.6 percent) and time consuming to implement (n = 26; 14.3 percent). Self-care and medications were associated with greater patient compliance, preference, and lower costs than splints (Figure 4). Barriers to the use of self-care were the lack of experience/knowledge (n = 12; 9.0 percent), time consuming (n = 13; 9.8 percent) and short-term efficacy (n = 25; 18.8 percent). The most commonly reported difficulty for prescription medications (n = 18; 36.0 percent) and over-the-counter (n = 8; 24.2 percent) was the short-term efficacy.
Figure 4. Reasons dentists recommend a specific treatment for including in a RCT.
DISCUSSION
The results of this survey indicate that the majority of CONDOR general dentists treat TMJD pain, independent of their region and age. This survey also demonstrates that the majority of these dentists use a similar diagnostic protocol, including questionnaires and exams for the diagnosis of TMJD pain, and that the most-used treatments were splints, self-care and over-the-counter analgesic medications.
The current initial reversible treatments for pain-related TMJD used and preferred by CONDOR general dentists are consistent with the NIDCR’s TMD Technology Assessment Conference Statement, which supports patient education with self-care, pharmacological pain control, physical therapy and splint therapy as appropriate initial therapeutic interventions for the management of patients with pain.2 The Statement goes on to note that occlusal therapy is irreversible and should only be used to “… identify and eliminate gross occlusal discrepancies such as those that may inadvertently occur as a result of restorative procedures.” Although 63.6 percent of the CONDOR general dentists use occlusal adjustments for pain-related TMJD, it is not clear if this is primarily used for the NIDCR indications (i.e., elimination of gross occlusal discrepancies such as may inadvertently occur as a result of restorative procedures)2 or as an initial treatment for pain-related TMJD. A previous survey completed by U.S. and Canadian dental faculty responsible for teaching predoctoral TMJD found that “… occlusal adjustments was endorsed by 23 percent of respondents, and 11 percent reported teaching full-mouth occlusal equilibration as a TMD treatment modality.” 7 Therefore, if occlusal interventions are still being taught in dental schools as a TMJD treatment, it is not surprising that general dentists are using occlusal adjustments as treatment for pain-related TMJD.
Three results of this survey support the feasibility of conducting a RCT: 1) 80.3 percent of dentists who treat pain-related TMJD are willing to participate in a RCT, 2) 93.9 percent use both questionnaires and physical examinations to diagnosis pain-related TMJD and 3) most of the dentists want to compare reversible treatments: splint, self-care and medication. They prefer to randomly assign patients to different treatments and not to a placebo or to no-treatment group. Given that previous RCT8-19 and systematic reviews20-24 have demonstrated the effectiveness of diverse TMJD treatments in tertiary care centers, a RCT including a placebo group could raise bioethical concerns.25-27 Since self-care is a simple, inexpensive, reversible and effective treatment for pain-related TMJD, using it as a standard treatment to compare the effectiveness of other treatment options seems to be a pragmatic option in a future RCT.
In a future pragmatic28-31 RCT, a reliable and valid diagnosis of the pain-related TMJD will be obtained using the TMD Pain Screener questionnaire32 which includes assessment of whether this pain is changed with jaw movement, function (i.e., eating) and/or parafunction. Although this screener does not differentiate jaw-joint and jaw-muscle pain, when using validated diagnostic criteria, the majority of TMJD patients have both myofascial pain and arthralgia.33 Regardless, to render valid diagnoses of myofascial pain and arthralgia, the general dentists will use this validated protocol with replication and localization of the patient’s pain-related TMJD complaint in the jaw-joint and/or jaw-muscle with mandibular range of motion and/or palpation33 – simple examination tests already used by the vast majority of CONDOR general dentists. To improve the reliability of this examination protocol, the dentists will be provided a reference manual with specific operational procedures to standardize their diagnostic protocol. In addition, exclusion criteria will eliminate most clinically significant intra-articular disorders by eliminating patients with a history of intermittent locking closed (i.e., catching) and/or limited mouth opening upon examination.
This survey has several strengths. First, a large number of dentists across different regions were recruited for this study. Second, the participation rate across all PBRNs was higher than 80 percent. Third, dentists were recruited independent of their practice treating TMJD pain. Our study has a number of limitations. As the results of this survey were based on the self-reported questionnaire, information bias needs to be considered. It is possible that dentists over-reported the number of TMJD pain patients they treat or their willingness to participate in a RCT. In addition, this survey suggests that splint, self-care and over-the-counter medication were the most frequently used and preferred treatment for TMJD pain, but these choices vary by dentists’ regions. We cannot determine if this difference is a consequence of over-reporting any specific treatment by dentists from the USA, an underestimation by dentists from Scandinavia or a difference in practice between these countries. Data related to the frequency of patients’ symptoms were based on the dentists’ reports and may be biased by their memory. Finally, although studies comparing the demographics of the dentists in the dental PBRNs with national estimates have shown similar dentist and practice characteristics,5, 6 generalizability of results of that survey to all general dentists in the USA and Scandinavia should be done with caution.
CONCLUSION
Most general dentists treat TMJD pain patients. Reversible initial care is typically provided for TMJD pain. The results suggest that it would be feasible to conduct a pragmatic RCT in the PBRNs for assessing the effectiveness of self-care, splint therapy and/or medications for the initial management of pain-related TMJD.
Acknowledgements
This study was funded by grants U01-DE-16746, U01-DE-16747, U01-DE-16750, U01-DE-16752, U01-DE-16754 and U01-DE-16755 from the National Institutes of Health. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health.
Footnotes
Disclosure
The authors do not have any conflicts of interests associated with this manuscript.
REFERENCES
- 1.National Institute of Dental and Craniofacial Research Facial Pain. Available at: “ http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/FacialPain.
- 2.National Institutes of Health Technology Assessment Conference Statement Management of Temporomandibular Disorders Management of temporomandibular disorders. J Am Dent Assoc. 1996;127:1595–603. [PubMed] [Google Scholar]
- 3.Wassell RW, Adams N, Kelly PJ. The treatment of temporomandibular disorders with stabilizing splints in general dental practice: one-year follow-up. J Am Dent Assoc. 2006;137(8):1089–98. doi: 10.14219/jada.archive.2006.0347. [DOI] [PubMed] [Google Scholar]
- 4.Wassell RWAN, Kelly PJ. Treatment of temporomandibular disorders by stabilizing splints in general dental practice: Results after initial treatment. Br Dental J. 2004;197(1):35–41. [Google Scholar]
- 5.DeRouen TA, Cunha-Cruz J, Hilton TJ, Ferracane J, Berg J, Zhou L, et al. What’s in a dental practice-based research network? Characteristics of Northwest PRECEDENT dentists, their patients and office visits. J Am Dent Assoc. 2010;141(7):889–99. doi: 10.14219/jada.archive.2010.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ. Dentists in practice-based research networks have much in common with dentists at large: evidence from the Dental Practice-Based Research Network. Gen Dent. 2009;57(3):270–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Klasser GD, Greene CS. Predoctoral teaching of temporomandibular disorders: a survey of U.S. and Canadian dental schools. J Am Dent Assoc. 2007;138(2):231–7. doi: 10.14219/jada.archive.2007.0142. [DOI] [PubMed] [Google Scholar]
- 8.Herman CR, Schiffman EL, Look JO, Rindal DB. The effectiveness of adding pharmacologic treatment with clonazepam or cyclobenzaprine to patient education and self-care for the treatment of jaw pain upon awakening: a randomized clinical trial. J Orofac Pain. 2002;16(1):64–70. [PubMed] [Google Scholar]
- 9.Mulet M, Decker KL, Look JO, Lenton PA, Schiffman EL. A randomized clinical trial assessing the efficacy of adding 6 × 6 exercises to self-care for the treatment of masticatory myofascial pain. J Orofac Pain. 2007;21(4):318–28. [PubMed] [Google Scholar]
- 10.Wright EF, Domenech MA, Fischer JR., Jr. Usefulness of posture training for patients with temporomandibular disorders. J Am Dent Assoc. 2000;131(2):202–10. doi: 10.14219/jada.archive.2000.0148. [DOI] [PubMed] [Google Scholar]
- 11.Wright E, Anderson G, Schulte J. A randomized clinical trial of intraoral soft splints and palliative treatment for masticatory muscle pain. J Orofac Pain. 1995;9(2):192–9. [PubMed] [Google Scholar]
- 12.Singer E, Dionne R. A controlled evaluation of ibuprofen and diazepam for chronic orofacial muscle pain. J Orofac Pain. 1997;11(2):139–46. [PubMed] [Google Scholar]
- 13.Carlson CR, Okeson JP, Falace DA, Nitz AJ, Anderson D. Stretch-based relaxation and the reduction of EMG activity among masticatory muscle pain patients. J Orofac Pain. 5(3):205–12. [PubMed] [Google Scholar]
- 14.Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R. The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. J Orofac Pain. 2004;18(2):114–25. [PubMed] [Google Scholar]
- 15.Truelove E, Huggins KH, Mancl L, Dworkin SF. The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. J Am Dent Assoc. 2006;137(8):1099–107. doi: 10.14219/jada.archive.2006.0348. quiz 169. [DOI] [PubMed] [Google Scholar]
- 16.Turner JA, Mancl L, Aaron LA. Brief cognitive-behavioral therapy for temporomandibular disorder pain: effects on daily electronic outcome and process measures. Pain. 2005;117(3):377–87. doi: 10.1016/j.pain.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 17.Turner JA, Mancl L, Aaron LA. Short- and long-term efficacy of brief cognitive-behavioral therapy for patients with chronic temporomandibular disorder pain: a randomized, controlled trial. Pain. 2006;121(3):181–94. doi: 10.1016/j.pain.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 18.Dworkin SF, Huggins KH, Wilson L, Mancl L, Turner J, Massoth D, et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders-axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofac Pain. 2002;16(1):48–63. [PubMed] [Google Scholar]
- 19.Ekberg EC, Kopp S, Akerman S. Diclofenac sodium as an alternative treatment of temporomandibular joint pain. Acta odontologica Scandinavica. 1996;54(3):154–9. doi: 10.3109/00016359609003516. [DOI] [PubMed] [Google Scholar]
- 20.List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. J Oral Rehabil. 2010;37(6):430–51. doi: 10.1111/j.1365-2842.2010.02089.x. [DOI] [PubMed] [Google Scholar]
- 21.List T, Axelsson S, Leijon G. Pharmacologic interventions in the treatment of temporomandibular disorders, atypical facial pain, and burning mouth syndrome. A qualitative systematic review. J Orofac Pain. 2003;17(4):301–10. [PubMed] [Google Scholar]
- 22.Forssell H, Kalso E. Application of principles of evidence-based medicine to occlusal treatment for temporomandibular disorders: are there lessons to be learned? J Orofac Pain. 2004;18(1):9–22. discussion 23-32. [PubMed] [Google Scholar]
- 23.Forssell H, Kalso E, Koskela P, Vehmanen R, Puukka P, Alanen P. Occlusal treatments in temporomandibular disorders: a qualitative systematic review of randomized controlled trials. Pain. 1999;83(3):549–60. doi: 10.1016/S0304-3959(99)00160-8. [DOI] [PubMed] [Google Scholar]
- 24.Fricton J, Look JO, Wright E, Alencar FG, Jr., Chen H, Lang M, et al. Systematic review and meta-analysis of randomized controlled trials evaluating intraoral orthopedic appliances for temporomandibular disorders. J Orofac Pain. 2010;24(3):237–54. [PubMed] [Google Scholar]
- 25.Levine RJ. The need to revise the Declaration of Helsinki. N Engl J Med. 1999;341(7):531–4. doi: 10.1056/NEJM199908123410713. [DOI] [PubMed] [Google Scholar]
- 26.Freedman B. Equipoise and the ethics of clinical research. N Engl J Med. 1987;317(3):141–5. doi: 10.1056/NEJM198707163170304. [DOI] [PubMed] [Google Scholar]
- 27.O’Leary KD, Borkovec TD. Conceptual, methodological, and ethical problems of placebo groups in psychotherapy research. Am Psychol. 1978;33(9):821–30. doi: 10.1037//0003-066x.33.9.821. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. J Chronic Dis. 1967;20(8):637–48. doi: 10.1016/0021-9681(67)90041-0. [DOI] [PubMed] [Google Scholar]
- 29.Sackett DL, Gent M. Controversy in counting and attributing events in clinical trials. The N Engl J Med. 1979;301(26):1410–2. doi: 10.1056/NEJM197912273012602. [DOI] [PubMed] [Google Scholar]
- 30.Brass EP. The gap between clinical trials and clinical practice: the use of pragmatic clinical trials to inform regulatory decision making. J Clin Pharm Ther. 2010;87(3):351–5. doi: 10.1038/clpt.2009.218. [DOI] [PubMed] [Google Scholar]
- 31.Macpherson H. Pragmatic clinical trials. Complement Ther Med. 2004;12(2-3):136–40. doi: 10.1016/j.ctim.2004.07.043. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez YM, Schiffman E, Gordon SM, Seago B, Truelove EL, Slade G, et al. Development of a brief and effective temporomandibular disorder pain screening questionnaire: Reliability and validity. J Am Dent Assoc. 2011;142(10):1183–91. doi: 10.14219/jada.archive.2011.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schiffman EL, Ohrbach R, Truelove EL, Tai F, Anderson GC, Pan W, et al. The Research Diagnostic Criteria for Temporomandibular Disorders. V: methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain. 2010;24(1):63–78. [PMC free article] [PubMed] [Google Scholar]