Abstract
The upward trend in obesity prevalence across regions and continents is a worldwide concern. Today a majority of the world’s population live in a country where being overweight or obese causes more deaths than being underweight. Only a portion of those qualifying for treatment will get the health care they need. Still, a minor weight loss of 5–10% seems to be sufficient to provide a clinically significant health benefit in terms of risk factors for cardiovascular disease and diabetes. Diet, exercise and behavior modifications remain the current cornerstones of obesity treatment. Weight-loss drugs play a minor role. Drugs which were available and reasonably effective have been withdrawn because of side effects. The fact that the ‘old’ well known, but pretty unexciting tools remain the basic armamentarium causes understandable concern and disappointment among both patients and therapists. Hence, bariatric surgery has increasingly been recognized and developed, as it offers substantial weight loss and prolonged weight control. The present review highlights the conventional tools to counter obesity, lifestyle modification, pharmacotherapy and bariatric surgery, including some of the barriers to successful weight loss: (1) unrealistic expectations of success; (2) high attrition rates; (3) cultural norms of self-acceptance in terms of weight and beliefs of fat being healthy; (4) neighborhood attributes such as a lack of well-stocked supermarkets and rather the presence of convenience stores with low-quality foods; and (5) the perception of the neighborhood as less safe and with low walkability. Prevention is the obvious key. Cost-effective societal interventions such as a tax on unhealthy food and beverages, front-of-pack traffic light nutrition labeling and prohibition of advertising of junk food and beverages to children are also discussed.
Keywords: bariatric surgery, drug therapy, health behavior, intervention studies, life style, obesity, overweight, primary prevention
Introduction
According to the World Health Organization, 65% of the world’s population live in a country where being overweight or obese causes more deaths than being underweight [World Health Organization, 2009]. Worldwide, more than 1 billion people are estimated to be overweight (body mass index [BMI] ≥25 kg/m2), and more than 300 million of these are considered obese (BMI ≥30 kg/m2), making obesity one of the greatest threats to public health today [World Health Organization, 2009]. In Western Australia, high BMI has even overtaken tobacco as the leading independent risk factor contributing to disease [Hoad et al. 2010]. If predictions become facts, the majority of the world’s adults will be overweight or obese by 2030 [Kelly et al. 2008].
During the last century, public health interventions have become success stories in reducing risk factors such as smoking, infectious disease, high cholesterol, hypertension and injuries. However, no country has yet curbed the obesity epidemic. A systematic review of studies from 25 countries, investigating the obesity trends since 1999, documents a continuous increase of obesity [Rokholm et al. 2010]. According to the review, this is especially seen in European countries (such as Austria, Denmark and Sweden) as well as Asian countries (such as India, Nepal, Bangladesh and Malaysia). In the American population, on the other hand, prevalence over time is linked to race and ethnicity. While obesity is increasing among non-Hispanic Blacks and in Mexican American women, it is starting to level off among other groups [Flegal et al. 2010].
In developing countries, the highest prevalence of overweight is still found in the highest wealth and education groups, according to a study of overweight trends in 39 low- and middle-income countries [Jones-Smith et al. 2011]. However, the overweight prevalence growth rate was found to be higher in lower wealth and less educated segments of the population in a number of countries. As a consequence, an unfavorable future social distribution of risk factors for chronic disease in lower-income countries may develop.
Although the obesity prevalence among adults continues to increase worldwide, there are indications of a decrease in children. A recent review with data on almost 500,000 children from 9 countries in Europe, North America, Asia and Oceania has indicated that childhood obesity and overweight prevalence have stabilized [Olds et al. 2011]. However, there is evidence from Europe, Australia and the US that the obesity trend commonly develops in a nonlinear fashion, with stepwise increases in prevalence [Rokholm et al. 2010]. Today’s plateau among children may be the result of successful public health campaigns. There is obviously no guarantee that the previous rising trend will not start again, given the prevailing obesogenic environment. Government leadership and regulations, investment in national intervention programs, trend monitoring, as well as funding of research [Swinburn et al. 2011] are urgently needed to reduce the pressure on scarce healthcare resources. Nonetheless, while some governments are searching for ways to reverse the obesity epidemic, the absence of political leadership for action is obvious in many countries [Gortmaker et al. 2011], leaving it up to the individual or to private enterprises to cope with the problem.
The pandemic pattern of obesity
The increase in obesity prevalence became evident in high-income countries during the 1980s, when eating habits and movement patterns changed dramatically [Flegal et al. 2010]. The availability of refined carbohydrates and fats increased during this time at a rapid pace. Energy dense, processed foods become cheaper and therefore available to most people [Swinburn et al. 2011]. Although physical activity energy expenditure may not have declined to the degree that it really fuels the obesity epidemic [Westerterp and Speakman, 2008], labor-intensive work, such as farming and lumberjacking, have become mechanized through improved technology, making workers less physically active. Even ordinary tasks in daily life have become easier to perform, requiring less physical effort. Elevators, remote controls, computers and increased transportation by various vehicles, even for shorter distances, contribute to decreased physical activity. For example, Canadian children of today only expend one quarter of the energy their counterparts did 40 years ago [Pipe, 2002].
There seems to be a predictable pattern in the spreading of obesity. Middle- and low-income countries are now going through the same rapid transition as industrialized countries already have done. Groups of high socioeconomic status in urban areas are the first to increase their obesity prevalence. Later, obesity is also spread to groups of lower socioeconomic status in suburban and rural areas. When gross domestic product (GDP) increases, there is also a faster increase in obesity prevalence among low-income groups [Jones-Smith et al. 2011].
Thus, obesity is no longer a problem only in industrialized countries. It has now reached urban and rural areas in the poorest countries of sub-Saharan Africa and South Asia [Popkin et al. 2012]. Local traditions of foods with high fiber content have been exchanged for processed foods and sugar sweetened soft drinks as a sign of wealth. In fact, not only do many countries suffer from the double burden of both nutrient malnutrition and its related diseases, they also face the comorbidities associated with obesity and being overweight in parallel [Swinburn et al. 2011].
Although obesity is not an infectious disease, and consequently cannot correctly be entitled a pandemic, it is rapidly spreading across regions and continents, making it a worldwide concern. Perhaps it is time to question the definition of a pandemic, and upgrade the commonly called obesity epidemic to the new pandemic? By definition, a pandemic disease threatens the whole of society and, therefore, powerful measures have been taken on when a pandemic warning has been issued. Possibly, this upgrade could make politicians react and take command as promptly as they did with the outbreak of swine flu, H1N1. The goal was to nip it in the bud before the situation got worse.
Awareness about the obesity situation has improved, at least in terms of the number of policy programs, guidelines and strategic plans. However, translation into action has not followed. In 2010, the US Surgeon General pointed out that there is a need for dedicated and compassionate citizens involved in grass root efforts [U.S. Department of Health and Human Services, 2010]. These grass roots are thought to find their own creative ways to implement changes for healthier behaviors in their families and communities. Parents, child care professionals and teachers are encouraged to prevent and intervene even before a child enters the path to obesity. To resolve the obesity epidemic we also need concerted action involving not only the civil society, but also the private sector, professional networks, media and international organizations and last, but not least, the governments [Deitel, 2007].
Obesity is one of the most difficult conditions to overcome. The forces that make us enjoy energy-dense food and a sedentary lifestyle are strong. There is a general agreement that prevention of obesity, already from childhood, would be an optimal strategy. When prevention fails, there are in principle three tools to counter obesity: lifestyle modification, pharmacotherapy and bariatric surgery.
This nonsystematic, brief review addresses prevention, as well as current approaches to manage the rising tide of obesity, from patient-centered individual therapies to community-based interventions.
Policy programs: what works?
There is a growing demand that governments and international bodies such as the United Nations (UN) and World Health organization (WHO) take action to reduce the burden of obesity. Charters may be signed, but too often the resources needed to make a change are not set aside. Political commitment hopefully increases when interventions prove to give value for money. To facilitate political action, an Australian initiative, Assessing Cost-Effectiveness (ACE) in obesity [Vos et al. 2010], creates simulation models of the cost-effectiveness of obesity interventions. Interestingly, environmental interventions are rated as the most cost-effective. While the cost is fairly low, such activities have a moderate effect on the individual, but since they affect the entire population the overall impact makes a difference. For example, ACE recommends the following interventions: (1) a tax on unhealthy food and beverages; (2) front-of-pack traffic light nutrition labeling; and (3) reduction of advertising of junk food and beverages to children. Below are examples of how these interventions have successfully been implemented in some countries around the world.
Tax on unhealthy food and beverages
In 2010, the Danish government imposed a 25% increased tax on sweets, chocolate and ice cream with the aim of targeting the public health burden of obesity and heart disease. Next in line are soft drinks, tobacco and alcohol [Wilkins, 2010]. The Danes have a good track record. In 2003 they passed a law to ban the use of transfatty acids. Transfatty acids, known to increase the risk of coronary heart disease [Willett et al. 1993], are now completely removed from food products in Denmark. Instead, food producers have developed new production methods. Hence, the products in focus are still around, but with better fat quality [Leth et al. 2006]. Neighboring countries have emphasized voluntary agreements, but have not succeeded in completely ridding their populations of transfatty acid consumption.
Front-of-pack traffic light nutrition labeling
Front-of-pack signposting for informed and healthy shopping decisions has received increasing interest. Formats vary, from color coded with well-known symbols such as traffic lights, to healthy logos such as the New Zealand and Australian ‘Pick the Tick’ [Young and Swinburn, 2002] or in the form of guideline healthy amounts.
Recently, a randomized-controlled study conducted to evaluate different food label formats on consumers’ choices, demonstrated that traffic light labels had the most influence on consumers, compared with other formats [Borgmeier and Westenhoefer, 2009]. Even if the consumers are under time constraints, traffic light labels and logos have been proven to enhance the likelihood of healthy choices [Hebden et al. 2011]. Not surprisingly, unlabeled food is more difficult to classify as healthy or unhealthy [Borgmeier and Westenhoefer, 2009].
Consumers are constantly exposed to many information sources such as the media, advertisements and promotions. When comparing two products with comparable prices or when making first-time purchases, 58% of the consumers said that they used product labels [Wills et al. 2009]. Interestingly, Canadians claim product labels as their most important source for nutritional information. This source is then followed by printed media, friends and family, electronic media channels and lastly family physicians or other professionals [Wills et al. 2009]. It is noteworthy that the medical profession seems to play such a minor role in national information.
Potentially, with the right organization and presentation, signposts could be of high value and result in improved food choice patterns. To achieve implementation of successful nutrition labeling, engagement and regulation from the authorities are needed.
Reduction of advertising of junk food and beverages to children
Regulation has also been suggested for food and beverages advertised to children. Regulation could focus on the type of program (typically children’s programs), type of product (unhealthy foods), target audience (children), time of day (when many children are watching) and content of advertisements (persuasive intent with, for example, premiums) [Handsley et al. 2009].
In Sweden, Norway and Quebec the government has regulated television advertising to children. More specifically, the Swedish Radio and Television Act does not allow commercial television advertising intended to attract the attention of children below the age of 12. However, most countries do not regulate advertisements to children. A comparison of food advertising in 13 countries across 5 continents, found that a child who was watching television 2 hours per day would be exposed to between 28 and 84 food advertisements a week for food with high energy content and undesirable nutrients. Only television channel promotions were more frequently advertised than food. Fast food restaurant meals constituted every third advertisement in the US and every seventh advertisement in Australia [Kelly et al. 2010].
The Australian fast-food industry has agreed on a self-regulation to decrease fast-food advertisement to children. Despite this, exposure is unchanged according to Australian researchers requesting policy framework for regulation of advertising to children [Hebden et al. 2011].
Commonly, but not unexpectedly, recommended food policies and regulations are opposed by the powerful food industry. Other types of interventions, such as physical activity interventions, and different types of school and community actions may be easier to implement, but may also be less beneficial ways to fight obesity.
Lifestyle interventions for weight reduction: successful examples
There is general agreement that weight loss will follow a negative energy balance, independently of how that is achieved. It is important to distinguish between weight loss (reasonably easy to achieve) and weight-loss maintenance (considerably more difficult to achieve). Weight loss can be accomplished in numerous ways.
Bariatric surgery has proven to be more effective than conventional weight-loss management for morbid obesity, in a Cochrane database systematic review [Colquitt et al. 2005]. Still, lifestyle interventions will be the most realistic treatment option for the vast majority of obese children, adolescents and adults. Leblanc and colleagues [Leblanc et al. 2011] recently made a systematic review, summarizing the effectiveness of lifestyle weight-loss interventions. The authors concluded that behavior-based treatment programs are safe and effective.
As long as 20 years ago the Diabetes Prevention Study (DPS) randomized Finish middle-aged, overweight men and women with impaired glucose tolerance into either intensive lifestyle intervention or to a control group receiving usual care. After 3 years, weight reductions were 3.5 kg in the intervention group and 0.9 kg in the control group, respectively. In total, 9% in the intervention group and 20% in the control group developed diabetes. In addition, favorable changes were seen in terms of measures of lipemia [Lindstrom et al. 2003].
Later the Diabetes Prevention Program (DPP) enrolled more than 3000 subjects at high risk for diabetes type 2. Patients were randomized to one of three arms: lifestyle intervention with a weight-loss goal of 7% and at least 150 minutes of moderate physical activity of similar intensity to brisk walking a week, metformin (850 mg twice daily) or placebo. The average follow-up time was 2.8 years. Lifestyle intervention turned out to be the most successful method. Losing weight and increasing physical activity resulted in a 58% reduction in diabetes incidence rate compared with placebo. Presented as numbers needed to treat (NNT), 6.9 subjects needed to take part in the lifestyle intervention program, compared with 13.9 receiving metformin to prevent one case of diabetes, during a 3-year period [Knowler et al. 2002].
The DPP study was soon followed by another large, still ongoing intervention study: the Look AHEAD trial. It aimed to investigate the long-term effects of lifestyle intervention (diet modification and increased physical activity with a gradual progression; the goal was set as 175 minutes of moderate intensity a week) in 5000 overweight and obese subjects with type 2 diabetes. Participants randomized to the intervention arm lost on average 8.6% of their initial body weight during the first year of the intervention, while those assigned to the education and diabetes support group lost 0.7% of their weight. HbA1c, urine albumin-to-creatinine ratio and risk factors for cardiovascular disease such as high systolic and diastolic blood pressure, triglycerides and high-density lipoprotein (HDL) cholesterol all improved significantly more in the intervention group compared with the control group [Pi-Sunyer et al. 2007].
Barriers to success
A minor weight loss seems to be sufficient to provide a clinically significant health benefit in terms of risk factors for cardiovascular disease and diabetes. These, and similar findings [Van Gaal et al. 2005; Tuomilehto et al. 2001], have made up the base for current health recommendations.
However, there is a striking difference between professional recommendations of sustained minor weight loss and patients’ unrealistic expectations of success. This was illustrated in a study by Foster and colleagues, where 60 obese women (mean BMI 36.3 kg/m2) were asked about their weight goal prior treatment. The goal was on average to reach a 32% reduction in body weight. A weight loss of 17 kg (a 17% reduction in body weight for the average participant) was regarded as ‘not successful in any way’ and disappointing. A 25 kg weight loss would be acceptable, but ‘not one that I would be particularly happy with’. After almost a year of treatment, the average weight loss was an impressive 16.3 kg: a weight loss which was considered disappointing at the start of the program [Foster et al. 1997].
Similar findings were reported by Linné and colleagues [Linné et al. 2002]. In a severely obese group with an average BMI of 40.7 kg/m2, a sex difference was noted. Men hoped for a 29% reduction in body weight and women aimed for an even higher weight loss, 42%, at the start of the program. It is conceivable that poor compliance could be due to unrealistic expectations from the start.
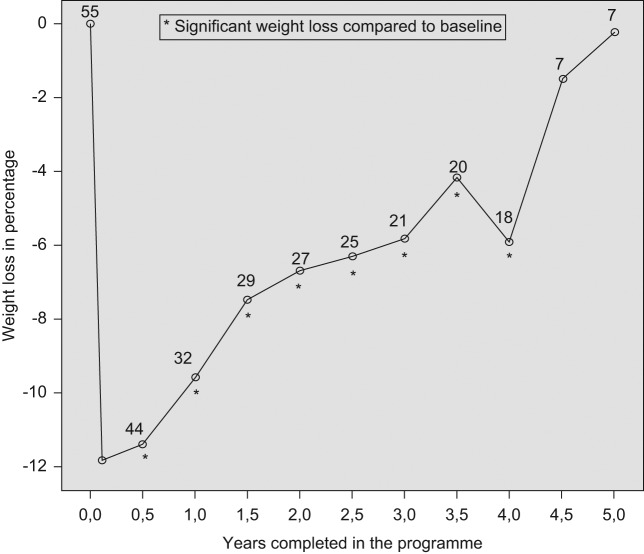
A concern in lifestyle interventions is participant attrition. Across 80 intervention trials, the average attrition rate was 29% at 1-year follow up [Franz et al. 2007]. The typical story of success with initial weight loss and the sad story of attrition and subsequent weight gain is shown in Figure 1. A group of 55 Swedish obese men (average BMI 39 kg/m2) took part in monthly group sessions at a Swedish hospital for 4 years. A total drop-out rate of 67% was observed, of which more than 40% dropped out from the program during the first year. A total of 7/55 men kept the group sessions rolling for a fifth year. Despite this initiative, their weight had returned to baseline weight at the end of the program.
Figure 1.
Weight-loss pattern and program participation in a group of 55 Swedish obese men.
Among other barriers to successful weight loss is family eating habits (eating out, unhealthy cooking and lack of healthy food in the home) [Porter et al. 2010]. Family and social pressure to consume large amounts of food, including high-fat foods, have been described in focus groups as a barrier to weight loss [Blixen et al. 2006]. Culture and ethnicity are other aspects of importance. Several studies on African American women have pointed out the cultural norm of self-acceptance in terms of weight, the family members’ satisfaction with their weight and thus the lack of necessary social support to lose weight [Baturka et al. 2000; Blixen et al. 2006; Thomas et al. 2008]. Likewise, in a focus group study among Latinos in South Carolina, USA, both males and females expressed a preference for a heavier body type. Their perception of fat being healthy was in direct conflict with medical advice [Diaz et al. 2007].
Attributes of the neighborhood have also been reported to be associated with BMI. In a study of almost 11,000 participants in four US states, the presence of supermarkets in the neighborhood was associated with a lower prevalence of obesity and overweight, while the presence of convenience stores was associated with a higher prevalence of obesity and being overweight [Morland et al. 2006]. Similarly, a high concentration of local restaurants was associated with a higher BMI in a study by Inagami and colleagues [Inagami et al. 2009].
Perceived neighborhood safety is another mechanism through which the neighborhood may have an impact on obesity. Those that perceive their neighborhoods as less than extremely safe were more than twice as likely to have no leisure-time physical activity in a Texas study [Centers of Disease Control and Prevention, 2005]. Individuals who perceived their neighborhoods as unsafe had a BMI that was 2.81 kg/m2 higher than those who perceived their neighborhood as safe, according to another US study among adults [Fish et al. 2010]. Adjustment for depressive symptoms did not alter this finding. Similar findings have been reported among children growing up in neighborhoods perceived as less safe; the parental perception of the neighborhood as less safe was independently associated with an increased risk of overweight at the age of seven [Lumeng et al. 2006].
Neighborhood walkability has also been examined in some studies. Hardly surprisingly, lower neighborhood walkability was associated with more driving time, but also with more self-reported TV viewing [Kozo et al. 2012]. The latter has been shown in an Australian study as well; walkability was negatively associated with TV viewing (in women, but not in men) [Sugiyama et al. 2007], suggesting that environmental characteristics may contribute to sedentary behavior and an increased BMI.
Lifestyle interventions: now with modern technology
The primary focus in self-care interventions is the encouragement of the participant’s behavior change. The basis is increased knowledge of his or her condition, and the goal is to modify eating, activity and other aspects such as thinking habits that can contribute to the patient’s weight problem [Wadden et al. 2005]. While this can be done with pamphlets, books and other paper-based material, the rapid increase in availability and access to modern technology enables innovative ways of delivering, for example, weight-loss programs.
Today, the Internet has more than 2.2 billion users worldwide. Almost a third, 32.7%, of the world’s population uses its services [Internet World Stats, 2012]. The potential reach of health information through the Internet is enormous. Health information found is also in general trusted: the majority of healthcare seekers do not check the source and the date of the information they discover [Bennett and Glasgow, 2009].
Internet has increasingly been used for delivery of health interventions. At least theoretically, the Internet has the potential to overcome many of the limitations traditional weight-loss interventions are facing. Internet health applications, accessible at any time and independent of geography, could be a way to minimize the high attrition rates in obesity weight-loss programs. The programs can be reached with convenient tools, which are in place when the patient has the time and motivation to access them, 24 hours a day. A high number of participants may be targeted at a low cost when face-to-face programs are remodeled and become more accessible via new technology. Furthermore, healthcare professionals have the opportunity to maintain long-term contact with a large number of obese and overweight patients in a cost-effective way using the Internet.
New motivation and action support systems facilitate the process of tailoring programs to the precise needs of the participants. New technology may serve as a facilitator to acquire behavioral change. Even age groups, not growing up with new advanced technology such as computers, do well in Internet-based behavioral weight-loss programs. A study examining the effectiveness of an Internet-based program among those above the age of 65 concluded that they performed equally well or even better than younger participants. Older participants were more likely to be active, to log in and record their diet and current weight more frequently. Among women, those older than 65 had on average the highest percentage of weight loss, 6.8% in 6 months [Van Der Mark et al. 2009].
Weight Watchers is another example of a weight-loss program using the Internet [Weight Watchers, 2012]. It is an enterprise offering regular group meetings. With new technology, such as a smartphone application, the participants can choose whether they would like to attend the meetings online or in person, making the program available also for those who cannot, or are not interested in, attending meetings.
Despite more and more intervention studies using the Internet and the increasing number of commercial Web-based weight-loss programs, further evidence is required to assess the effectiveness. Systematic reviews on Internet-based behavioral interventions for obesity have identified the lack of well-designed efficacy trials. The heterogeneity of designs and low generalization of findings make effectiveness difficult to assess [Tsai and Wadden, 2005; Manzoni et al. 2011]. It is also still unclear which intervention components, for example support forums, coaching messages and BMI calculators, produce weight loss, either in isolation or collectively [Bennett and Glasgow, 2009]. Furthermore, participant attrition is high, sometimes up to 70% after a year [Neve et al. 2010].
Bennett and Glasgow [Bennett and Glasgow, 2009] point out the need to attract, retain and engage intervention participants to prevent attrition. The trend on the Internet is a progression away from Web sites towards Web services, allowing users to have a high degree of control over their own data. They can store, view and share personal data in sophisticated ways. This set of design principles, called Web 2.0, is used by for example by Facebook and YouTube. A creative Internet service implementation of research sites for weight loss may be an attractive way to self-monitor weight and other health behaviors.
Today, the only limiting factor to health professionals and researchers is creativity. With an expanding field of new possibilities it is time to ask questions such as the following. How can behavioral weight-loss strategies effectively be taught online? Which features (self-monitoring, chat rooms, food diaries etc.) are associated with the most weight loss? How can motivation be maintained throughout a long treatment program using new technology? How can new technology overcome the boredom and fatigue associated with previous failures? How can different types of technology interact to offer enhanced support for individuals trying to lose weight? How can we integrate Web service principles into research Web sites? How can healthcare facilities utilize modern technology to target new groups of patients?
Obesity pharmacotherapy: a sad story
Appetite regulation has been a matter of survival for thousands of years. The neurobiology of hunger, appetite and eating is intricate, with many pathways not yet fully disentangled. Its complexity is a challenge, particularly in the development of a drug aimed at targeting one or several of these specific pathways.
The amount of weight loss has differed between different drugs. Even so, effect sizes are moderate. Haddock and colleagues [Haddock et al. 2002] reported that weight losses as a result of obesity medication never reached more than 4 kg, in their meta-analysis of 108 randomized clinical trials with durations between 7 and 47 weeks. However, in combination with lifestyle interventions, drugs have been shown to improve weight-loss maintenance [Franz et al. 2007].
Further, the pharmacological industry has invested enormous resources trying to find a unique drug to boost weight loss. Despite this, patients and health professionals face the bitter fact that, at present, only one obesity medication (with modest effect) is available on the market. The rise and fall of anti-obesity drugs is listed in Table 1 [Bray, 2007].
Table 1.
Anti-obesity drugs, their year of introduction, withdrawal and serious adverse events.
| Year of introduction and withdrawal | Anti-obesity drug | Serious adverse effect |
|---|---|---|
| 1893/1949 | Thyroxine | Thyrotoxicosis |
| 1933/1935 | Dinitrophenol | Cataracts and hyperthermia |
| 1937/1971 | Amphetamine and derivatives | Tolerance and psychosis |
| 1960/2000 | Phenylpropanolamine (norephedrine and norpseudoephedrine) | Hemorrhagic stroke |
| 1965/1972 | Aminorex | Pulmonary hypertension |
| 1973/1997 | Fenfluramine + phentermine (fen-phen) | Pulmonary hypertension and heart valve problems |
| 1997/2010 | Sibutramine | Myocardial infarction and stroke |
| 2006/2009 | Rimonabant | Suicidality and depression |
Recently, the market went through the introduction and the withdrawal of sibutramine (an antidepressant, which was a centrally acting monoamine-reuptake inhibitor increasing satiety) [Padwal and Majumdar, 2007]. When it was later reported that subjects with cardiovascular disease had an increased risk of nonfatal myocardial infarction and nonfatal stroke during long-term treatment with sibutramine [James et al. 2010], it was withdrawn. Rimonabant (a cannabinoid receptor blocker, initially intended as an anti-obesity and smoking-cessation dual-purpose drug) [Padwal and Majumdar, 2007] was never introduced in the US, but was available on the market in Europe and other parts of the world. It was also withdrawn a few years ago. The main reason for withdrawal was psychiatric side effects. However, even though the product information was continuously updated and strengthened to include further contraindications, it was later concluded that the benefits no longer outweighed the risks [The European Medicines Agency, 2008]. Only orlistat (a gastric and pancreatic lipase inhibitor reducing dietary fat absorption) [Hauptman et al. 1992] is still available on the market.
After these failures, few promising novel drugs have entered the market. Potentially the increased knowledge around the gastrointestinal peptide hormones affected by obesity surgery could lead to new insights, hopefully giving rise to new drugs in the field of obesity. There is an urgent need for safe and effective anti-obesity drugs to complement lifestyle changes. Table 2 lists some peptides, affected by bariatric surgery, that may hold key information about weight regulation and thus hold the potential to be developed into new drugs [Shukla and Rubino, 2011].
Table 2.
Origin, effects, and altered levels of some gastrointestinal hormones after bariatric surgery.
| Gastrointestinal hormones | Origin | Hunger and food intake | Other effects | After surgery |
|---|---|---|---|---|
| Glucagon-like pepitide-1 (GLP-1) | Ileum and colon | Decreased | Enhanced glucose-dependent insulin secretion, suppressed glucagon secretion, increased beta-cell mass, inhibited gastric emptying | Rise in GLP-1 occurs as early as 2 days after surgery |
| Gastric inhibitory peptide (GIP) | Duodenum and jejunum | Unknown | Enhanced triglyceride accumulation, fat deposition, beta-cell proliferation and bone formation | A reduction or no change |
| Grehlin | Stomach | Stimulated | Stimulated insulin counterregulatory hormones, suppressed adiponectin, blocked hepatic insulin signaling and inhibited insulin secretion | Unclear |
| Peptide YY (PYY) | Ileum and colon | Decreased | Decreased gastrointestinal motility, gastric acid secretion, pancreatic and intestinal secretion | Increased |
Surgery: an emerging strategy
Since the long lasting depressing story of pharmacotherapy of obesity has shown little success, it is no surprise that bariatric surgery has developed rapidly. It has increasingly been recognized as an effective option in obesity management. It offers substantial weight loss and prolonged weight control. Sjöström and colleagues reported that bariatric surgery was not only associated with positive effects on diabetes, cardiovascular risk factors and lifestyle [Sjöström et al. 2004], but also with cardiovascular events, cardiovascular mortality [Sjöström et al. 2012] and total mortality [Sjöström et al. 2007]. After almost 11 years of follow up with a follow-up rate of 99.9%, the total mortality was 24% lower in the surgery group when compared with the control group receiving conventional treatment. After controlling for confounders (age, gender and other risk factors) the difference was even higher (41%, p = 0.01). These results have also been confirmed by others [Adams et al. 2007]. Adams and colleagues have also reported a 46% lower total cancer mortality in the surgical group compared with controls, when following almost 6600 gastric bypass patients and their severely obese controls for a 24-year period [Adams et al. 2009].
As a treatment option, surgery has gained increasing attention for subgroups such as diabetics, obese adolescents and children. A case report describing a vertical sleeve gastrectomy (VSG) for the treatment of a 6-year-old girl with morbid obesity was published in 2010 [Dan et al. 2010]. Technically, bariatric surgery can thus be performed in young children. Obviously, however, the long-term risks with bariatric surgery in children are still largely unknown.
Further research is needed, before we widen the eligibility criteria in terms of which patients are suitable for undergoing bariatric surgery. Questions for the future include: should there be age limits, both for young and old obese subjects? Are refinements of definitions of eligible patients needed? Shall we keep excluding psychiatric patients, drug users, alcoholics and patients with eating disorders? Are mechanical weight-related problems an additional indication even at lower BMI levels? Should we base criteria on other factors than age and BMI, for example the EOSS criteria [Padwal et al. 2011], which focus on obesity consequences rather than relative body weight?
Summary
Diet, exercise and behavior modifications will remain the cornerstones of obesity treatment for the foreseeable future. Drugs play a minor role and will perhaps continue to do so for a long period of time. The absence of powerful tools has led to an explosion in bariatric surgery, today acknowledged to be the only method resulting in significant weight-loss maintenance and overall risk reduction. In many countries, the standard cutoff value of BMI >35 kg/m2 for surgery nevertheless indicate that a large proportion of the obese population will technically qualify for surgery.
In the struggle to improve public health, it should be remembered that few people want to be obese. Obesity is not a surprising end result in our obesogenic environment, so maybe it should even be seen as a normal reaction. It has been said that to ask why obesity has become so prevalent is to ask the wrong question. Rather, the question should be: why are there any lean people around at all?
The global availability of cheap, highly promoted, energy-dense, tasty and processed foods has increased rapidly, whereas the need for physical activity has decreased in work and transportation as a result of modernization. Hence, physical activity has developed only into a voluntary undertaking in leisure time.
The implication of these dramatic shifts in energy intake and energy expenditure has vast consequences not only for the individual, but also in terms of societal healthcare costs and productivity. In reality, only a tiny proportion of the obese qualifying for treatment will get the healthcare attention they need and deserve, whether it is lifestyle changes, bariatric surgery or pharmacotherapy they need in their struggle to lose weight. Although the upward trend in the prevalence of obesity was noticed 30 years ago, it is not until recently that obesity and its consequences have become fully acknowledged as a worldwide burden. With political leadership we can declare a ‘war’ on obesity, nevertheless we have to remember that obese individuals are not ‘domestic terrorists’ [Rail et al. 2010].
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: Professor Stephan Rössner has received travel support from VIVUS Inc, USA.
Contributor Information
Ylva Trolle Lagerros, Unit of Clinical Epidemiology, Karolinska Institutet, T2, SE17176, Stockholm, Sweden.
Stephan Rössner, Department of Medicine, Karolinska University Hospital, Stockholm, Sweden.
References
- Adams T., Gress R., Smith S., Halverson R., Simper S., Rosamond W., et al. (2007) Long-term mortality after gastric bypass surgery. N Engl J Med 357: 753–761 [DOI] [PubMed] [Google Scholar]
- Adams T., Stroup A., Gress R., Adams K., Calle E., Smith S., et al. (2009) Cancer incidence and mortality after gastric bypass surgery. Obesity (Silver Spring) 17: 796–802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baturka N., Hornsby P., Schorling J. (2000) Clinical implications of body image among rural African-American women. J Gen Intern Med 15: 235–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett G., Glasgow R. (2009) The delivery of public health interventions via the internet: actualizing their potential. Annu Rev Public Health 30: 273–292 [DOI] [PubMed] [Google Scholar]
- Blixen C., Singh A., Thacker H. (2006) Values and beliefs about obesity and weight reduction among African American and Caucasian women. J Transcult Nurs 17: 290–297 [DOI] [PubMed] [Google Scholar]
- Borgmeier I., Westenhoefer J. (2009) Impact of different food label formats on healthiness evaluation and food choice of consumers: a randomized-controlled study. BMC Public Health 9: 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray G. (2007) The Battle of the Bulge. A History of Obesity Research. Pittsburgh, PA: Dorrance Publishing Co [Google Scholar]
- Centers of Disease Control and Prevention (2005) Perceptions of neighborhood characteristics and leisure-time physical inactivity - Austin/Travis County, Texas, 2004. MMWR Morb Mortal Wkly Rep 54: 926–928 [PubMed] [Google Scholar]
- Colquitt J., Clegg A., Loveman E., Royle P., Sidhu M. (2005) Surgery for morbid obesity. Cochrane Database Syst Rev: CD003641 [DOI] [PubMed] [Google Scholar]
- Dan D., Harnanan D., Seetahal S., Naraynsingh V., Teelucksingh S. (2010) Bariatric surgery in the management of childhood obesity: should there be an age limit? Obes Surg 20: 114–117 [DOI] [PubMed] [Google Scholar]
- Deitel M. (2007) The European charter on counteracting obesity. Obes Surg 17: 143–144 [DOI] [PubMed] [Google Scholar]
- Diaz V., Mainous A., III, Pope C. (2007) Cultural conflicts in the weight loss experience of overweight Latinos. Int J Obes (Lond) 31: 328–333 [DOI] [PubMed] [Google Scholar]
- Fish J., Ettner S., Ang A., Brown A. (2010) Association of perceived neighborhood safety with [corrected] body mass index. Am J Public Health 100: 2296–2303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K., Carroll M., Ogden C., Curtin L. (2010) Prevalence and trends in obesity among US adults, 1999–2008. JAMA 303: 235–241 [DOI] [PubMed] [Google Scholar]
- Foster G., Wadden T., Vogt R., Brewer G. (1997) What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. J Consult Clin Psychol 65: 79–85 [DOI] [PubMed] [Google Scholar]
- Franz M., Vanwormer J., Crain A., Boucher J., Histon T., Caplan W., et al. (2007) Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc 107: 1755–1767 [DOI] [PubMed] [Google Scholar]
- Gortmaker S., Swinburn B., Levy D., Carter R., Mabry P., Finegood D., et al. (2011) Changing the future of obesity: science, policy, and action. Lancet 378: 838–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddock C., Poston W., Dill P., Foreyt J., Ericsson M. (2002) Pharmacotherapy for obesity: a quantitative analysis of four decades of published randomized clinical trials. Int J Obes Relat Metab Disord 26: 262–273 [DOI] [PubMed] [Google Scholar]
- Handsley E., Mehta K., Coveney J., Nehmy C. (2009) Regulatory axes on food advertising to children on television. Aust N Z Health Policy 6: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauptman J., Jeunet F., Hartmann D. (1992) Initial studies in humans with the novel gastrointestinal lipase inhibitor Ro 18–0647 (tetrahydrolipstatin). Am J Clin Nutr 55: 309S-313S [DOI] [PubMed] [Google Scholar]
- Hebden L., King L., Grunseit A., Kelly B., Chapman K. (2011) Advertising of fast food to children on Australian television: the impact of industry self-regulation. Med J Aust 195: 20–24 [DOI] [PubMed] [Google Scholar]
- Hoad V., Somerford P., Katzenellenbogen J. (2010) High body mass index overtakes tobacco as the leading independent risk factor contributing to disease burden in Western Australia. Aust N Z J Public Health 34: 214–215 [DOI] [PubMed] [Google Scholar]
- Inagami S., Cohen D., Brown A., Asch S. (2009) Body mass index, neighborhood fast food and restaurant concentration, and car ownership. J Urban Health 86: 683–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Internet World Stats (2012) http://internetworldstats.com/stats.htm (accessed 25 June 2012).
- James W., Caterson I., Coutinho W., Finer N., Van Gaal L., Maggioni A., et al. (2010) Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med 363: 905–917 [DOI] [PubMed] [Google Scholar]
- Jones-Smith J., Gordon-Larsen P., Siddiqi A., Popkin B. (2011) Is the burden of overweight shifting to the poor across the globe? Time trends among women in 39 low- and middle-income countries (1991–2008). Int J Obes (Lond), in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly B., Halford J., Boyland E., Chapman K., Bautista-Castano I., Berg C., et al. (2010) Television food advertising to children: a global perspective. Am J Public Health 100: 1730–1736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly T., Yang W., Chen C., Reynolds K., He J. (2008) Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 32: 1431–1437 [DOI] [PubMed] [Google Scholar]
- Knowler W., Barrett-Connor E., Fowler S., Hamman R., Lachin J., Walker E., et al. (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346: 393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozo J., Sallis J., Conway T., Kerr J., Cain K., Saelens B., et al. (2012) Sedentary behaviors of adults in relation to neighborhood walkability and income. Health Psychol, in press [DOI] [PubMed] [Google Scholar]
- Leblanc E., O’Connor E., Whitlock E., Patnode C., Kapka T. (2011) Effectiveness of primary care-relevant treatments for obesity in adults: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med 155: 434–447 [DOI] [PubMed] [Google Scholar]
- Leth T., Jensen H., Mikkelsen A., Bysted A. (2006) The effect of the regulation on trans fatty acid content in Danish food. Atheroscler Suppl 7: 53–56 [DOI] [PubMed] [Google Scholar]
- Lindstrom J., Louheranta A., Mannelin M., Rastas M., Salminen V., Eriksson J., et al. (2003) The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 26: 3230–3236 [DOI] [PubMed] [Google Scholar]
- Linné Y., Hemmingsson E., Adolfsson B., Ramsten J., Rossner S. (2002) Patient expectations of obesity treatment-the experience from a day-care unit. Int J Obes Relat Metab Disord 26: 739–741 [DOI] [PubMed] [Google Scholar]
- Lumeng J., Appugliese D., Cabral H., Bradley R., Zuckerman B. (2006) Neighborhood safety and overweight status in children. Arch Pediatr Adolesc Med 160: 25–31 [DOI] [PubMed] [Google Scholar]
- Manzoni G., Pagnini F., Corti S., Molinari E., Castelnuovo G. (2011) Internet-based behavioral interventions for obesity: an updated systematic review. Clin Pract Epidemiol Ment Health 7: 19–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K., Diez Roux A., Wing S. (2006) Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med 30: 333–339 [DOI] [PubMed] [Google Scholar]
- Neve M., Collins C., Morgan P. (2010) Dropout, nonusage attrition, and pretreatment predictors of nonusage attrition in a commercial web-based weight loss program. J Med Internet Res 12: e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds T., Maher C., Zumin S., Peneau S., Lioret S., Castetbon K., et al. (2011) Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 6: 342–360 [DOI] [PubMed] [Google Scholar]
- Padwal R., Majumdar S. (2007) Drug treatments for obesity: orlistat, sibutramine, and rimonabant. Lancet 369: 71–77 [DOI] [PubMed] [Google Scholar]
- Padwal R., Pajewski N., Allison D., Sharma A. (2011) Using the Edmonton obesity staging system to predict mortality in a population-representative cohort of people with overweight and obesity. CMAJ 183: E1059–1066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pi-Sunyer X., Blackburn G., Brancati F., Bray G., Bright R., Clark J., et al. (2007) Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care 30: 1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pipe A. (2002) Get active about physical activity. Ask, advise, assist: get your patients moving. Can Fam Physician 48: 13–14, 21–23 [PMC free article] [PubMed] [Google Scholar]
- Popkin B., Adair L., Ng S. (2012) Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 70: 3–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter J., Bean M., Gerke C., Stern M. (2010) Psychosocial factors and perspectives on weight gain and barriers to weight loss among adolescents enrolled in obesity treatment. J Clin Psychol Med Settings 17: 98–102 [DOI] [PubMed] [Google Scholar]
- Rail G., Holmes D., Murray S. (2010) The politics of evidence on ‘domestic terrorists’: obesity discourses and their effects. Social Theory Health 8: 259–279 [Google Scholar]
- Rokholm B., Baker J., Sorensen T. (2010) The levelling off of the obesity epidemic since the year 1999 - a review of evidence and perspectives. Obes Rev 11: 835–846 [DOI] [PubMed] [Google Scholar]
- Shukla A., Rubino F. (2011) Secretion and function of gastrointestinal hormones after bariatric surgery: their role in type 2 diabetes. Can J Diabetes 35: 115–122 [Google Scholar]
- Sjöström L., Lindroos A., Peltonen M., Torgerson J., Bouchard C., Carlsson B., et al. (2004) Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 351: 2683–2693 [DOI] [PubMed] [Google Scholar]
- Sjöström L., Narbro K., Sjöström C., Karason K., Larsson B., Wedel H., et al. (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357: 741–752 [DOI] [PubMed] [Google Scholar]
- Sjöström L., Peltonen M., Jacobson P., Sjöström C., Karason K., Wedel H., et al. (2012) Bariatric surgery and long-term cardiovascular events. JAMA 307: 56–65 [DOI] [PubMed] [Google Scholar]
- Sugiyama T., Salmon J., Dunstan D., Bauman A., Owen N. (2007) Neighborhood walkability and TV viewing time among Australian adults. Am J Prev Med 33: 444–449 [DOI] [PubMed] [Google Scholar]
- Swinburn B., Sacks G., Hall K., McPherson K., Finegood D., Moodie M., et al. (2011) The Global obesity pandemic: shaped by global drivers and local environments. Lancet 378: 804–814 [DOI] [PubMed] [Google Scholar]
- The European Medicines Agency (2008) The European Medicines Agency Recommends Suspension of the Marketing Authorisation of Acomplia, http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2009/11/news_detail_000244.jsp&mid=WC0b01ac058004d5c1&jsenabled=true (accessed 15 February 2012).
- Thomas A., Moseley G., Stallings R., Nichols-English G., Wagner P. (2008) Perceptions of obesity: Black and White differences. J Cult Divers 15: 174–180 [PubMed] [Google Scholar]
- Tsai A., Wadden T. (2005) Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 142: 56–66 [DOI] [PubMed] [Google Scholar]
- Tuomilehto J., Lindstrom J., Eriksson J., Valle T., Hamalainen H., Ilanne-Parikka P., et al. (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344: 1343–1350 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2010) The Surgeon General’s Vision for a Healthy and Fit Nation. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General; [PubMed] [Google Scholar]
- Van Der Mark M., Jonasson J., Svensson M., Linneb Y., Rossner S., Lagerros Y. (2009) Older members perform better in an internet-based behavioral weight loss program compared to younger members. Obes Facts 2: 74–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gaal L., Mertens I., Ballaux D. (2005) What is the relationship between risk factor reduction and degree of weight loss? Eur Heart J 7: L21–L26 [Google Scholar]
- Vos T., Carter R., Barendregt J., Mihalopoulos C., Veerman J., Magnus A., et al. (2010) Assessing Cost-Effectiveness in Prevention (Ace–Prevention): Final Report. Brisbane: University of Queensland/ Melbourne: Deakin University [Google Scholar]
- Wadden T., Crerand C., Brock J. (2005) Behavioral treatment of obesity. Psychiatr Clin North Am 28: 151–170, ix [DOI] [PubMed] [Google Scholar]
- Weight Watchers (2012) http://www.weightwatchers.com/index.aspx (accessed 15 February 2012).
- Westerterp K., Speakman J. (2008) Physical activity energy expenditure has not declined since the 1980s and matches energy expenditures of wild mammals. Int J Obes (Lond) 32: 1256–1263 [DOI] [PubMed] [Google Scholar]
- Wilkins R. (2010) Danes impose 25% tax increases on ice cream, chocolate, and sweets to curb disease. BMJ 341: c3592. [DOI] [PubMed] [Google Scholar]
- Willett W., Stampfer M., Manson J., Colditz G., Speizer F., Rosner B., et al. (1993) Intake of trans fatty acids and risk of coronary heart disease among women. Lancet 341: 581–585 [DOI] [PubMed] [Google Scholar]
- Wills J., Schmidt D., Pillo-Blocka F., Cairns G. (2009) Exploring global consumer attitudes toward nutrition information on food labels. Nutr Rev 67(Suppl. 1): S102–S106 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2009) Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva: World Health Organization [Google Scholar]
- Young L., Swinburn B. (2002) Impact of the Pick the Tick food information programme on the salt content of food in New Zealand. Health Promot Int 17: 13–19 [DOI] [PubMed] [Google Scholar]