Abstract
Aims. Homonymous hemianopia (HH), a severe visual consequence of stroke, causes difficulties in detecting obstacles on the nonseeing (blind) side. We conducted a pilot study to evaluate the effects of oblique peripheral prisms, a novel development in optical treatments for HH, on detection of unexpected hazards when driving. Methods. Twelve people with complete HH (median 49 years, range 29–68) completed road tests with sham oblique prism glasses (SP) and real oblique prism glasses (RP). A masked evaluator rated driving performance along the 25 km routes on busy streets in Ghent, Belgium. Results. The proportion of satisfactory responses to unexpected hazards on the blind side was higher in the RP than the SP drive (80% versus 30%; P = 0.001), but similar for unexpected hazards on the seeing side. Conclusions. These pilot data suggest that oblique peripheral prisms may improve responses of people with HH to blindside hazards when driving and provide the basis for a future, larger-sample clinical trial. Testing responses to unexpected hazards in areas of heavy vehicle and pedestrian traffic appears promising as a real-world outcome measure for future evaluations of HH rehabilitation interventions aimed at improving detection when driving.
1. Introduction
Driving is the primary mode of transportation in the USA. Cessation of driving decreases independence and employment opportunities and increases the risk of depression [1, 2]. Thus, returning to driving following a stroke is an important rehabilitation goal. However, since stroke may cause a number of visual, perceptual, cognitive, and motor impairments that could adversely affect driving skills, poststroke driving rehabilitation is not straightforward [3–5]. In this paper we focus on rehabilitation of people with homonymous hemianopia (HH), the loss of the same half of the visual field in each eye due to postchiasmal lesions, a severe visual consequence of stroke. People with spatial neglect or other significant cognitive impairments were not included, as our goal was to address the effects of the sensory visual loss without other confounding perceptual or cognitive impairments.
In 2010, there were about 6.2 million stroke survivors in the USA [6] with at least 50% having partial or complete HH in the acute stage immediately following the stroke [7, 8]. Spontaneous recovery, either complete or partial, may occur within the first three months after the injury [8–11], but improvement after six months is rare [9]. About 30% of stroke patients still have chronic HH after nine months [12]. Chronic HH causes difficulties in detecting objects on the nonseeing (blind) side that may compromise safe walking (bumping into obstacles and falls [13, 14]), compromise safe driving (failure to see potential blindside hazards [15–17]), limit independence, and reduce quality of life [18–20].
In Europe [23], Australia [24], and 22 states of the USA [25], persons with HH do not meet the minimum visual field requirements for licensure (e.g., 120° horizontal field in Massachusetts). However, there are some states where they do meet the field requirements (e.g., New Hampshire has no field requirement) and may legally drive. Furthermore, in some countries (e.g., Belgium, Netherlands, Switzerland, UK, and Canada), persons with stable vision loss (but less than 120° horizontal field) may be licensed after taking a specialized on-road test [23, 26, 27]. Even when persons with HH are not legally permitted to drive, some do continue to drive to maintain independence and quality of life; 50% of participants with complete HH in a driving simulator study were still driving despite not meeting the 120° field requirement of the state in which the study was conducted [15]. Pass rates of drivers with HH in on-road studies have varied from 17% [28] to 73% [29], suggesting that some people with HH may be considered fit to drive [27, 30]. Nevertheless, there is a strong evidence that HH adversely affects both vehicle control (steering and lane position [28, 29, 31–33]) and detection of potential blindside hazards [15–17].
Prism glasses are a commonly-applied rehabilitation treatment for HH that optically shift images of objects located in the blind field into regions of the seeing field so that they can be seen [34]. Potentially they could be used to ameliorate blind-side deficits of HH drivers, but there are only very limited data addressing their effects on driving-related skills [35]. Here we report a pilot evaluation of the effects of a new type of prism glasses—oblique peripheral prisms—on detection of unexpected hazards while driving.
Peripheral prisms are a recent development in optical treatments for HH [36]. High-powered prism segments placed above and below the primary line of sight on the spectacle lens on the side of the field loss (Figure 1) provide visual field expansion (enlargement of the visual field; Figure 2), which is helpful for obstacle detection when walking [21, 36, 37]. When permanent peripheral prism glasses incorporating 57Δ embedded prism segments are worn (Figure 1(b)), the expansion can extend as much as 30° into the blind hemifield (equivalent to the width of about 6 to 7 lanes of traffic at 50 m). The latest innovation is the oblique design [38] that provides expansion in paracentral areas of the field, in regions used when looking through a car windshield [22] (Figure 2(b)). By comparison, the original “horizontal” design provided expansion only in areas outside the central regions of the field (Figure 2(c)). With the oblique design, although the expansion is in paracentral areas, the prism images fall on more peripheral retina; therefore, central diplopia (double vision) does not occur. Users are taught to always look through the central, prism-free area of the lens and to eye scan as they would do habitually; the visual field expansion is effective at all lateral positions of gaze.
Figure 1.
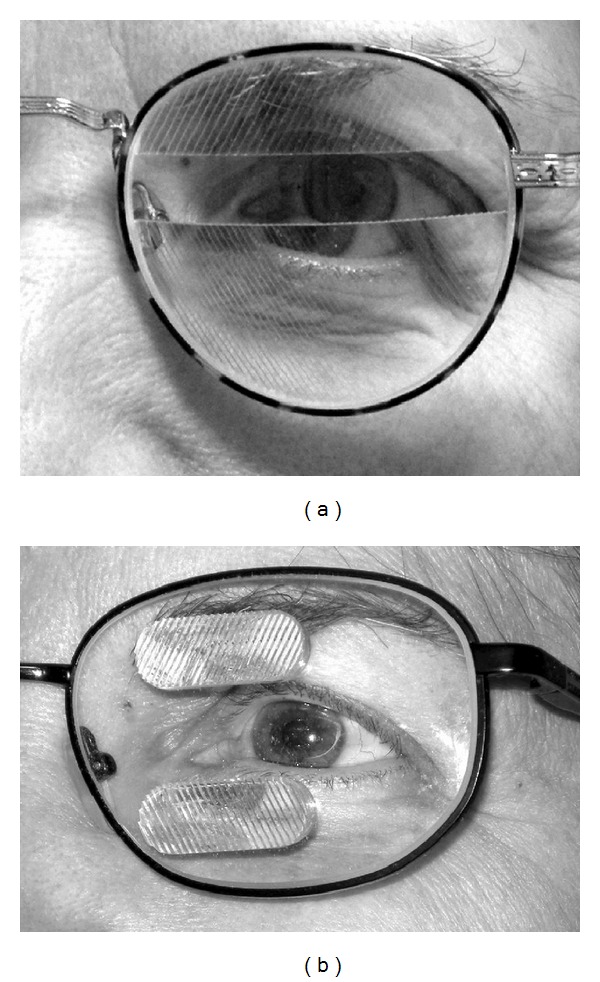
(a) Press-on 40Δ Fresnel peripheral prism segments in the oblique configuration on the left spectacle lens as fitted for the study to a patient with left HH. The upper prism is base out and base down, and the lower prism is base out and base up, shown with 9 mm interprism separation, providing expansion in the central area of the visual field used when driving (Figure 2(b)). The effect of the lower prism is notable by the apparent shift of the centrally located lower lid margin, iris, and sclera (imaged by the prism segment). The wearer has an uninterrupted binocular view through the central prism-free area of the lens. (b) Higher-power, 57Δ permanent prism glasses in the oblique configuration with 12 mm interprism separation (not used in this study, but now available from Chadwick Optical Inc., White River Junction, VT, USA).
Figure 2.
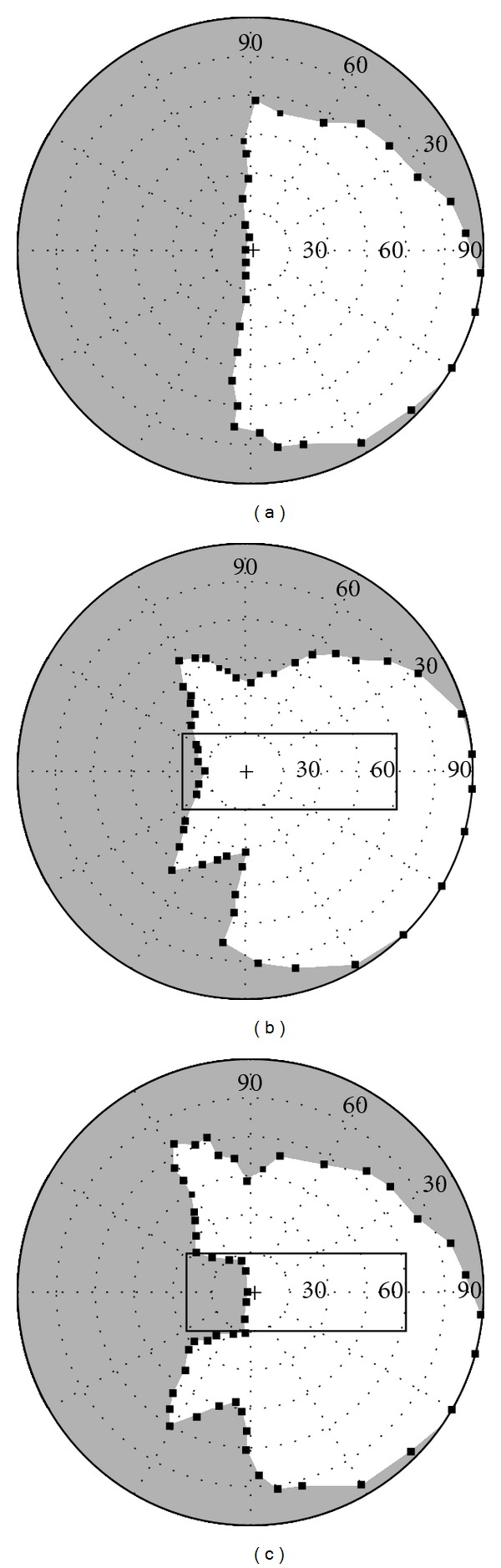
Binocular visual field (Goldmann V4e) of a patient with left HH (a) without peripheral prisms, (b) with 40Δ oblique peripheral prisms as fitted for this study with no vertical separation between the expansion areas (9 mm interprism separation and 30° angle of tilt), and (c) with the original horizontal design of 40Δ peripheral prisms for walking [21] (12 mm interprism separation). The oblique design provides about 20° of lateral expansion into central areas of the blind hemifield in the region used when looking through a car windshield (rectangle represents the field of view through a typical car windshield for driving on the right [22]); the horizontal design does not provide expansion within this area. Small black squares are the individual points mapped during the perimetry.
With the use of the oblique peripheral prisms, it is possible that people with HH could meet the visual field requirements for licensure in many states and countries (e.g., 90° horizontal visual field extent plus 20° to 30° field expansion, depending on the power and design of the prisms). Indeed, a few persons with HH have already been licensed to drive with these prisms in the USA and Canada. However, use of these prisms does not necessarily mean that the wearer would be safe to drive and, as yet, there had been no evaluation of their effects on detection performance when driving. We therefore conducted a pilot, open-road trial comparing driving performance when real and sham oblique peripheral prisms were worn. Response to unexpected blindside events was selected as the primary measure of the effects of the prism glasses for two reasons. Firstly, reactions to potential pedestrian hazards in driving simulator studies had proven to be a sensitive measure of the effects of a variety of types of visual field loss [15, 16, 39]. Secondly, data from two on-road studies of drivers with peripheral field loss due to glaucoma had demonstrated the possibility of using reactions to unexpected hazards as an outcome measure in open-road evaluations. In the first study [40], drivers with more restricted visual fields had poorer responses to unexpected events than drivers with less restricted fields, while in the second [41] drivers with glaucoma were 6 times more likely to have a critical intervention (driving examiner took control of the vehicle) than drivers with normal vision. Importantly, the critical interventions were primarily due to detection failures, mostly failing to notice pedestrians.
The main aim of the study was not to conduct fitness-to-drive tests in order to provide driving licenses for study participants. Rather, our goal was to conduct a pilot study to evaluate the effects of oblique peripheral prisms on detection of unexpected hazards when driving in order to acquire the necessary preliminary data to design a larger sample, future clinical trial of the device.
2. Methods
The study was conducted in accordance with the tenets of the Declaration of Helsinki and was approved by the Ethics Committees of the University Hospital of Ghent and Schepens Eye Research Institute. All participants gave their written consent before entering the study.
2.1. Participants
Four current and eight noncurrent HH drivers (with previous driving experience), representative of people with HH who might be driving or wish to resume driving, were recruited from individuals with visual field defects who had applied to CARA (a department of the Belgian Road Safety Institute) for a fitness-to-drive evaluation or annual reevaluation. Screening tests to determine eligibility were conducted by study investigators. The primary inclusion criteria were complete HH (no more than 5° of residual vision on the hemianopic side of the vertical meridian within 30° above and below fixation assessed with a Goldmann V4e target [37]), and no visual neglect (Bells test [42] and Schenkenberg Line Bisection test [43]). In addition, participants had visual acuity of 6/12 (20/40) or better in each eye with their habitual correction, and no significant cognitive decline (Minimental State Examination test, MMSE ≥ 24 [44]). Previous studies [15, 17] have reported no significant differences in blindside detection rates between right and left HH for participants without neglect; therefore, ensuring equal numbers of right HH and left HH was not a recruitment goal. Thus, our sample was homogeneous for visual and perceptual factors that might impact detection, but heterogeneous for other factors that normally vary within the HH population who are likely to want to apply for a driving license (Table 1).
Table 1.
Characteristics of the participants with HH.
| All participants (n = 12) | Current drivers (n = 4) | Noncurrent drivers (n = 8) | |
|---|---|---|---|
| Male, n (%) | 9 (75) | 3 (75) | 6 (75) |
| Age, years | 49 | 44 | 53 |
| Median, range | 29 to 68 | 29 to 60 | 43 to 68 |
| Binocular VA | 6/6 | 6/6 | 6/6 |
| Median, range | 6/4.5 to 6/7.5 | 6/4.5 to 6/6 | 6/5 to 6/7.5 |
| Left hemianopia, n (%) | 8 (67) | 2 (50) | 6 (75) |
| Time since onset HH, years | 2.3 | 6.1 | 0.8 |
| Median, range | 0.3 to 11.3 | 1.9 to 11.3 | 0.3 to 10.3 |
| Stroke caused HH, n (%) | 8 (67) | 3 (75) | 5 (63) |
| Hemiplegia, n (%) | 3 (25) | 1 (25) | 2 (25) |
| MMSE score | 28 | 28 | 29 |
| Median, range | 26 to 29 | 26 to 29 | 27 to 29 |
Eleven participants had driven for at least 15 years before the onset of the HH, including eight who had not driven since the onset (range 0.3–11.3 years; Table 1), and three who were currently active licensed drivers and were applying for reevaluation. The twelfth was in the process of obtaining a driving license but had been driving vehicles on private land for many years and had completed 10 hours of driving lessons prior to enrolment. Current drivers (n = 4) tended to be younger and to have had HH for longer than noncurrent drivers (Table 1; P = 0.13). For noncurrent drivers (n = 8), the etiologies were stroke (5), tumors (2), and traumatic brain injury (1). For current drivers the etiologies were stroke (3) and brain surgery for epilepsy (1). None of the participants had motor impairments that affected their ability to operate a car. For the three participants with hemiplegia (Table 1), the test vehicle was adapted to their needs, including selecting automatic gearshift and attaching steering knobs. There was no evidence that the hemiplegia adversely affected their driving performance.
2.2. Peripheral Prisms
An orthoptist at the University Hospital of Ghent, Belgium, (Universitair Ziekenhuis Gent) fitted and trained participants in the use of the prism glasses following procedures based on those successfully implemented in previous studies in which the prisms were evaluated for walking [21, 37]. The only difference was that the “oblique” prism configuration was used [38]. Upper and lower 40Δ press-on Fresnel prism segments (3M Health Care, St Paul, MN, USA) were fitted to the back surface of one lens (on the side of the field loss) of participants' spectacles primarily used for distance vision. The upper prism was placed base out and base down and the lower prism was placed base out and base up, with the base-apex line at an angle of tilt of 30° to the horizontal (Figure 1(a)). The interprism separation was adjusted so that there was little (2-3°) or no vertical separation between the visual field expansion areas (mapped with V4e target in a Goldmann perimeter), ensuring that the expansion covered as much as possible of the central visual field likely to be used when driving (Figure 2(b)). Participants were taught to always look through the central, prism-free area of the lens and were told to eye scan as they would do habitually.
2.3. Supervised Driving with Prisms
After four weeks of using the prism glasses for walking and as a front-seat car passenger (but not driving), all participants drove for two hours in locations of their choice, wearing and using their prisms under the supervision of a CARA driving evaluator. The primary role of the evaluator was to ensure safety; no scoring was conducted. The supervised practice ensured that all participants had some experience of using the prisms while driving before undertaking the driving evaluation with the prism glasses.
2.4. Driving Evaluations with Real and Sham Prisms
About two weeks after the supervised driving practice with the prisms, participants completed two test drives. In one, the participant was fitted with the prescribed 40Δ prisms (real prisms; RP). In the other, the participant also wore press-on Fresnel prisms, but of a very low power (5Δ; sham prisms; SP), which provided no useful field expansion (2°), essentially equivalent to not wearing prisms. The prisms were fitted and changed in between test drives by a third person (a clinician at the hospital). To the evaluators conducting the test drives, the RP and SP glasses appeared identical (both were of the oblique design). Thus the evaluators were masked as to whether the participant was wearing real or sham prisms. However, the participants and clinicians were not masked. The two test drives were conducted on the same day by the same evaluators with an hour break in between; the order of the RP and SP drives was counterbalanced across participants.
2.5. Route and Evaluation Procedures
To ensure that route familiarity did not affect driving performance, different routes of comparable difficulty (each about 25 km in the city of Ghent, Belgium) were used for the RP and SP drives. The route used for each drive was counterbalanced across participants. The route designs were based on those implemented in a previous on-road study [40] and were representative of routes used in standard fitness-to-drive evaluations conducted by CARA. Each route included a similar number of maneuvers and road types (residential and nonresidential, city center, and highway (120 km/h) or expressway (divided road at 90 or 120 km/h)). The traffic was dense, especially in the city and residential areas, including many pedestrians, bicycles, trams, and other vehicles. The high traffic density (including pedestrians and bicyclists) provided ideal conditions for evaluating the impact of the prisms on detection of potential blindside hazards.
The driving evaluations were conducted by CARA evaluators in dual-control cars. The procedures were similar to standard CARA practice for official fitness-to-drive tests, differing only in the scoring system employed and the use of predetermined routes. The CARA evaluator sat in the front seat and had access to the dual controls. The driving evaluations were scheduled as part of the daily CARA routine; therefore, based on their availability, four experienced CARA evaluators participated. Their role was to ensure safety and provide navigational instructions. Detailed scoring [40] of driving was conducted by a rater in the back seat; it was the same rater for all participants (a specialist in fitness-to-drive evaluations of visually impaired people).
At the start of the driving evaluation, a number of basic maneuvers were performed in a parking lot to familiarize the participant with the car and its controls. All driving tests took place in the prevailing weather conditions (unless unsafe because of snow) and between 8:30 AM and 3:00 PM to avoid rush hour traffic in the city. Each test drive took about 40 minutes.
2.6. Driving Measures
Two main aspects of driving were evaluated: responses to unexpected hazards and driving skills (including vehicle control) for specific maneuvers. We evaluated these skills to ensure that there were no negative effects of using the prism glasses (e.g., lane position might be affected by areas of the blind hemifield being made visible by the visual field expansion).
Whenever an unexpected hazard occurred, the backseat rater scored the response of the driver as either satisfactory (safe) or unsatisfactory (unsafe; either without or with an intervention by the CARA evaluator). He also noted details of the hazard, including what the hazard was and whether it was on the left or the right of the car (subsequently recoded into the blind or seeing side for analyses). Interventions were made whenever the CARA evaluator judged that driving was becoming dangerous and there was no option other than to intervene to prevent accidents or collisions. Steering corrections were easily seen from the back seat, while use of the second brake or gas pedal was accompanied by a mechanical sound as well as a light to indicate their use to the backseat rater. Interventions are a direct measure of driving safety, while responses to unexpected hazards that did not require an intervention represent a proxy measure of driving safety.
Detailed scoring [40] of driving skills (lane position, steering, speed, gap judgment, and scanning) was conducted for a range of maneuvers (turning and crossing at intersections, curve taking, merging, changing lanes, and overtaking) by the backseat rater at predetermined locations along the route. Skills were scored as either satisfactory (safe), inadequate (but not unsafe), or unsatisfactory (unsafe; either without or with an intervention). For each driving skill, the proportion of satisfactory scores was computed for each participant as the number of satisfactory scores divided by the total number of times that a skill was assessed (including data from all maneuvers in which the skill was scored).
2.7. Data Analyses
The effect of the prisms was tested by comparing performance in the RP and SP drives. For measures with sufficient data, the effect of driving status (current or noncurrent driver) was also examined. Primary measures included the proportion of satisfactory responses to unexpected hazards on the blind and seeing sides, and the proportion of satisfactory scores for each driving skill.
3. Results
3.1. Responses to Unexpected Hazards
During the 24 drives, there were 80 unexpected hazards. Ten participants had unexpected hazards in both RP and SP drives; two had unexpected hazards in only one of the drives. Unexpected hazards were mainly pedestrians, vehicles, and bicycles at intersections. Responses were rated as unsatisfactory for 41 events (29 with an intervention and 12 without an intervention) and satisfactory for the remaining 39.
Braking was the most common intervention (Table 2) and was primarily due to failures to notice a traffic event (vehicles, pedestrians, traffic lights). By comparison, steering interventions were less common (Table 2) and were mainly a result of taking a lane position too far to the right or the left, or weaving; only 1 of 8 was a result of failing to notice a traffic event. For noncurrent drivers, there were significantly fewer interventions in the RP than the SP drives (Wilcoxon signed ranks test, z = 2.22, P = 0.01; Table 2 and Figure 3), and they had significantly more interventions than current drivers in the SP, but not the RP drives (Mann-Whitney U test, z = 1.84, P = 0.04 and z = 0.51, P = 0.34, resp.; Figure 3).
Table 2.
Summary of interventions that occurred in each condition and on each side for current (n = 4) and noncurrent (n = 8) drivers.
| Condition | |||||
|---|---|---|---|---|---|
| Intervention | SP drive | RP drive | Total for each intervention | ||
| Current | Noncurrent | Current | Noncurrent | ||
| Brake | 1 (0; 1 ; 0)† | 9 (3; 5; 1) | 0 | 5 (3; 2; 0) | 15 |
| Steering correction | 0 | 6 (1; 0; 5) | 1 (0; 0; 1) | 1 (0; 0; 1) | 8 |
| Verbal advice | 1 (0; 1; 0) | 4 (2; 0; 2) | 0 | 0 | 5 |
| Accelerator | 0 | 1 (0; 0 ; 1) | 0 | 0 | 1 |
| Total for each drive | 2 (0; 2; 0) | 20 (6; 5; 9) | 1 (0; 0; 1) | 6 (3; 2; 1) | |
|
| |||||
| Overall total | 22 (6; 7; 9) | 7 (3; 2; 2) | 29 | ||
†Numbers in brackets provide the breakdown of interventions by side (seeing side; blind side; no side). Cells with italics are significantly different, as are cells with bold (see Figure 3).
Figure 3.
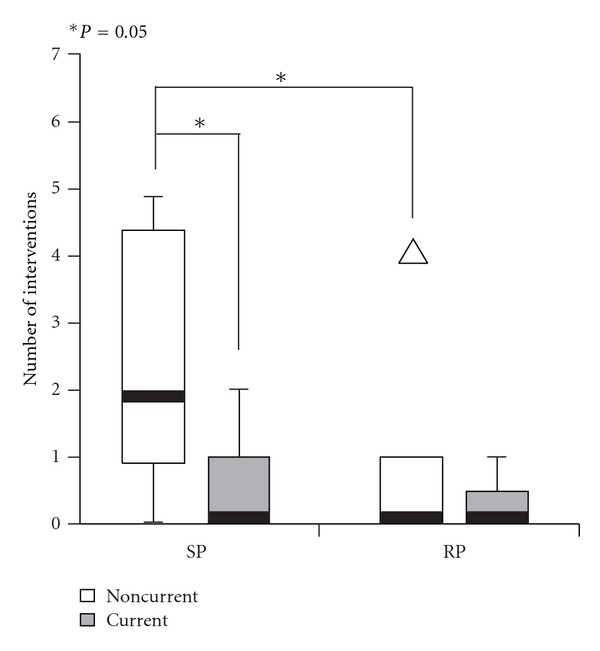
Number (median and interquartile range) of interventions in each drive for individual participants. Noncurrent drivers had fewer interventions in the real prism (RP) than the sham prism (SP) drives, and more interventions than current drivers in the SP but not the RP drives. The thick horizontal line within each box is the median; the vertical extent of the box is the interquartile range (IQR); vertical lines at box ends represent the largest nonoutlier data points within 1.5x IQR. Open triangle is a far outlier (>3x IQR).
Of the 80 unexpected hazards, 68 could be attributed to an event on either the blind (9 with and 34 without an intervention) or seeing side (9 with and 16 without an intervention). On the blind side, although the total number of events was similar for the RP and SP drives, the proportion of satisfactory responses was significantly higher in the RP drive (80% versus 30%; z = 3.25, P = 0.001; Figure 4); the same was true when only the participants with stroke were included (93% versus 32%; z = 3.52, P < 0.001). These analyses were for data pooled across participants, irrespective of whether or not there was an unexpected hazardous event on the blind side in both the RP and SP drives. When data for only those participants with blindside events in both the SP and RP drives (n = 8) were considered, the proportion of satisfactory responses for data pooled across participants was still significantly higher in the RP drive (78% versus 32%; z = 2.90, P = 0.002) and the proportion of satisfactory responses per participant was also significantly higher in the RP drive (Wilcoxon signed ranks test, z = 1.88, P = 0.03; Figure 5). Taken together, these results indicate a beneficial effect of the RP glasses on detection of blindside hazards. By comparison, on the seeing side, there were no significant differences in the proportion of satisfactory responses for the RP and SP drives (64% and 57%, resp.; data pooled across all participants; z = 0.33, P = 0.371; Figure 4).
Figure 4.
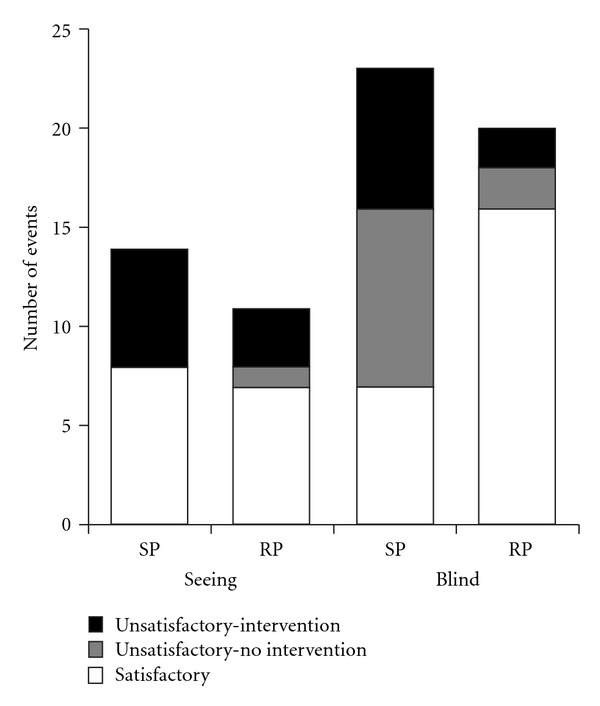
Total numbers of unsatisfactory and satisfactory responses to hazardous events on the seeing and blind sides for the 12 participants. The proportion of satisfactory responses to blindside hazards was significantly higher with real prisms (RP) than sham prisms (SP).
Figure 5.
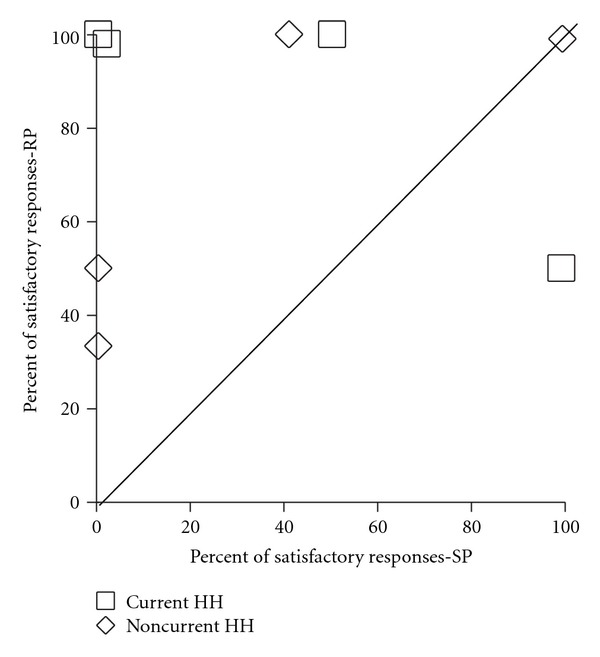
Percent of satisfactory responses to unexpected hazardous events on the blind side in the sham prism (SP) and real prism (RP) drives for the eight participants with blindside events in both drives. The diagonal line represents identical performance in the two drives. Six drivers (three current and three noncurrent) had a higher proportion of satisfactory responses in the RP than the SP drive (data points above the diagonal; P = 0.03).
There were enough blindside hazards (but not seeing-side hazards) to evaluate prism effects separately for current and noncurrent drivers. For these analyses, data were pooled across all participants within each group. The proportion of satisfactory responses to blindside hazards was significantly higher in the RP than the SP drives for both current and noncurrent drivers, again indicating a beneficial effect of the RP glasses (z = 2.49, P = 0.006; z = 2.26, P = 0.012, resp.; Figure 6).
Figure 6.
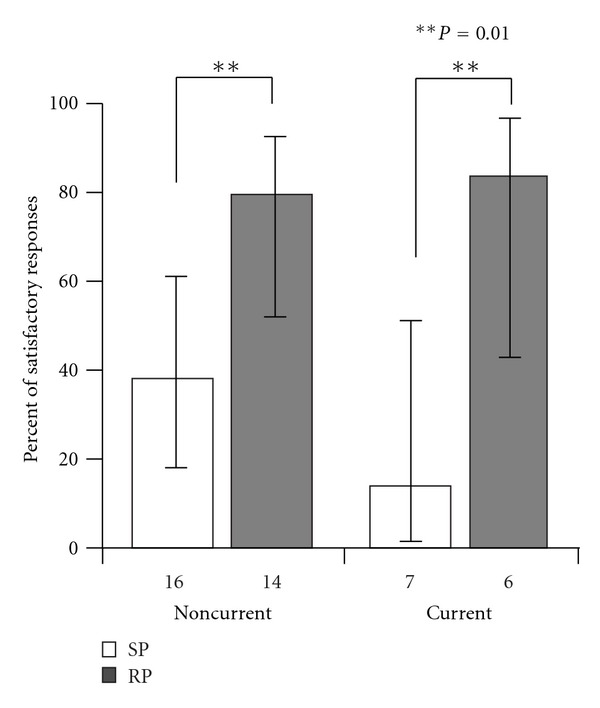
Percent of satisfactory responses to unexpected blindside hazards for current and noncurrent drivers. Both current and noncurrent drivers had better responses in the real prism (RP) than the sham prism (SP) condition, suggesting that the use of the peripheral prisms improved detection of blindside hazards for current drivers as well as noncurrent drivers. Numbers under each bar are the total number of hazards in each condition. Error bars represent 95% confidence limits.
3.2. Ratings of Skills during Specific Maneuvers
The majority of ratings for skills during specific maneuvers were satisfactory (Table 3). There were no significant differences (Wilcoxon signed ranks test, P > 0.1) in the proportion of satisfactory scores between the SP and RP drives for any of the skills, suggesting no adverse effects of the RP glasses. The few ratings that were not satisfactory were mainly inadequate, but not unsafe; only 4 out of a total of 3232 ratings (data pooled across all skills and maneuvers) were considered unsafe but did not require an intervention. Inadequate scores were mostly for driving too slowly, taking a path that was either too wide or too tight on left turns, unstable steering, and poor gap judgment (hesitating) at intersections (Table 3).
Table 3.
Percent (median and range) of satisfactory scores for ratings of skills during specific maneuvers.
| Skill | SP drive | RP drive |
|---|---|---|
| Speed | 98 | 100 |
| 77 to 100 | 88 to 100 |
|
| Path | 96 | 100 |
| 83 to 100 | 91 to 100 |
|
| Steering steadiness | 100 | 100 |
| 90 to 100 | 88 to 100 |
|
| Gap judgment | 100 | 100 |
| 89 to 100 | 88 to 100 |
|
| Lane position | 100 | 100 |
| 90 to 100 | 98 to 100 | |
| Scanning | 100 | 100 |
| 95 to 100 | 93 to 100 |
3.3. Participants' Experiences of Using the Prism Glasses
The majority (75%) of participants reported that the RP glasses were helpful when driving, in particular, for providing warning and seeing traffic on the blind side (Table 4). A minority (25%) reported initial difficulties in learning how to interpret the prism images of traffic (Table 4). At the end of the study, the clinical decision for 10 of the 12 participants (including seven with stroke) was to continue using the RP glasses for walking and driving (Table 4).
Table 4.
Participants' experiences of using real prism glasses and clinical decision.
| Hours per day, median (range) | 4.5 (1–12) |
| Moderately or very helpful for obstacle avoidance when walking, % (n) |
58 (7/12) |
| Moderately or very helpful for driving, % (n) | 75 (9/12) |
| Main ways in which helpful when driving, % (n)† | |
| Seeing blindside traffic | 30 (8/27) |
| Provided warning | 22 (6/27) |
| Merging/intersections | 15 (4/27) |
| More confident | 7 (2/27) |
| Other | 19 (5/27) |
| Unable to explain | 7 (2/27) |
| Difficulties using prisms when driving, % (n) | |
| None | 50 (6/12) |
| Initially (learn to use and interpret images) | 25 (3/12) |
| Busy places, rotaries | 17 (2/12) |
| No response | 8 (1/12) |
| Clinical decision % (n) | |
| Continue walking and driving | 83 (10/12) |
| Continue walking only | 8 (1/12) |
| Discontinue use | 8 (1/12) |
† n > 12 as participants made more than one response (open-ended question).
4. Discussion
In this study, the majority (62%) of interventions occurred as a result of a failure to notice a traffic event, suggesting that many participants (all with complete HH and without neglect) had significant detection deficits. If the examiner had not intervened, a collision would most likely have happened. These real-world data are in agreement with recent reports of detection deficits of people with HH in virtual driving and walking tasks [15–17, 45] and are consistent with the report of critical interventions for detection failures by drivers with restricted peripheral fields in another on-road study [41].
Nevertheless, our findings may seem at odds with some on-road studies of drivers with HH in which there were no reports of interventions for detection failures and the main problems were with lane position and steering control [28, 29]. It is possible that the routes in these studies did not include sufficient density of traffic and pedestrians (and bicycles, a feature of city-driving in Ghent, Belgium) to provide enough opportunities for evaluating responses to potentially hazardous events. It is worth noting that our cohort of HH drivers did have problems with steering: 24% of interventions were steering corrections (not in response to detection failures).
Not everybody with HH has poor detection. A common characteristic of prior studies [15, 17, 45] has been the wide between-subject variation in detection performance. Thus some patients with HH may compensate effectively using head and/or eye scanning, while others do not, and may need rehabilitation interventions such as prism glasses or scanning training. In order to evaluate the effects of such interventions, it is important to measure detection performance using tasks representative of real-world situations [46]. The results of this exploratory study suggest that responses to naturally-occurring blindside hazards in an open-road driving course has potential as an outcome measure for future studies of interventions aimed at improving detection while driving, provided they are conducted in an environment rich with potential hazards. In particular, despite a small sample size, we were able to measure differences in performance between drives with sham prism (SP) and real prism (RP) glasses. The data suggest that the RP glasses improved responses to blindside hazards for both current and noncurrent drivers as the proportion of satisfactory (safe) responses was higher with the RP than the SP glasses.
While responses to naturally occurring blindside hazards provide an outcome measure with maximum “real-world” validity, there are a number of challenges and limitations that have to be considered, not least the lack of control over whether or when an unexpected hazard might occur. Our approach was to select routes with a relatively high density of pedestrians, bicycles, and vehicular traffic, which were nevertheless representative of the test routes used in standard fitness-to-drive evaluations conducted by the Belgian Road Safety Institute. A standardized test in a driving simulator including detection of potential approaching hazards [16, 39] may be a useful adjunct, providing controlled, repeatable conditions with many opportunities to evaluate blind and seeing side detection performance. If detection performance in such a test could be validated against responses to unexpected hazards during a road test, it could be used as a replacement for the more dangerous and less well controlled road test.
In addition to prism glasses, compensatory strategies such as eye/head scanning [28, 47, 48] may ameliorate blindside detection deficits. In a recent on-road study, HH drivers rated as safe made more head movements into their blind field than HH drivers rated as unsafe [33]. Unlike explorative scanning, where the driver with HH has to remember to scan to the blind side, the peripheral prism visual field expansion is always present at all lateral gaze positions and provides a constant stimulus (as does normal peripheral vision) to initiate eye and/or head movements to the blind side to foveate potential hazards. However, the oblique prism glasses do not provide a total solution to the visual difficulties experienced by drivers with HH (they only ameliorate the detection problem) and do not address other driving deficits (such as poor steering control or driving too slowly).
Our sample was heterogeneous with respect to the etiology of the HH, which could be seen as a limitation of the study; however, we suggest otherwise. The main analyses were within-subjects comparisons of performance with RP and SP glasses; therefore, any effects of between-subject variability on performance (e.g., due to differences in etiology) were minimized. Furthermore, our primary interest was in the effect of HH, a sensory visual loss, on detection of hazards when driving and whether peripheral prism glasses could improve performance. Thus our participants were screened to ensure they did not have other comorbidities commonly associated with stroke including major cognitive deficits (MMSE scores ≥ 26; Table 1), spatial neglect (a perceptual impairment) and motor impairments that would have prevented them from operating a car (even with modifications such as a steering knob). The main findings were unchanged when only participants with stroke were included in analyses.
Our results add to the growing body of evidence that some people with HH following a stroke (or other forms of brain injury) are fit to drive, while others are not. There is no scientific evidence for the minimum field extent requirements for driving that automatically preclude people with HH from driving in many jurisdictions and countries [49]. Furthermore, conventional methods of assessing visual fields (in which eye movements are not permitted) do not provide any assessment of the ability of the person with HH to compensate by scanning. Thus, we suggest that it seems only fair to permit people with HH following a stroke an opportunity to demonstrate their competency to drive and compensate for their hemifield loss, for example, in a specialized road test [23, 26, 27]. A recent report suggests that this approach works well in Quebec, Canada [27]. However, there is generally a need for the development of standardized evaluation protocols and poststroke driving rehabilitation programs [3].
5. Conclusions
The results of this exploratory study suggest that oblique peripheral prism glasses may improve responses to blindside hazards for drivers with HH (due to stroke or other conditions) while not adversely impacting other aspects of driving (such as vehicle control). These preliminary data represent a first step in addressing the paucity of evidence about the efficacy of prismatic interventions for patients with visual field defects following stroke [46, 50] and provide the basis for a future, larger-sample clinical trial that is needed before firm conclusions can be drawn. Furthermore, our findings suggest that responses to naturally occurring, unexpected hazards may provide a useful real-world outcome measure for future evaluations of rehabilitation interventions that aim to improve detection performance of drivers with HH.
Conflict of Interests
E. Peli has a financial interest in a patent related to the oblique peripheral prism glasses (assigned to Schepens Eye Research Institute). A. R. Bowers and M. Tant have no conflict of interests.
Acknowledgments
The authors thank Ann Vandesteene and Nancy La Grange, Universitair Ziekenhuis Gent, for conducting the clinical aspects of the project. This paper was supported in part by National Institutes for Health (NIH) grants EY12890 (E. Peli) and EY018680 (A. R. Bowers). The NIH had no role in study design, data collection, data analysis, or report writing.
References
- 1.Ragland DR, Satariano WA, MacLeod KE. Driving cessation and increased depressive symptoms. The Journals of Gerontology A. 2005;60(3):399–403. doi: 10.1093/gerona/60.3.399. [DOI] [PubMed] [Google Scholar]
- 2.Marottoli RA, Mendes de Leon CF, Glass TA, Williams CS, Cooney LM, Berkman LF. Consequences of driving cessation: decreased out-of-home activity levels. The Journals of Gerontology B. 2000;55(6):S334–340. doi: 10.1093/geronb/55.6.s334. [DOI] [PubMed] [Google Scholar]
- 3.Akinwuntan AE, Wachtel J, Rosen PN. Driving simulation for evaluation and rehabilitation of driving after stroke. Journal of Stroke & Cerebrovascular Diseases. 2012;21(6):478–486. doi: 10.1016/j.jstrokecerebrovasdis.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 4.Marshall SC, Molnar F, Man-Son-Hing M, et al. Predictors of driving ability following stroke: a systematic review. Topics in Stroke Rehabilitation. 2007;14(1):98–114. doi: 10.1310/tsr1401-98. [DOI] [PubMed] [Google Scholar]
- 5.Ponsford AS, Viitanen M, Lundberg C, Johansson K. Assessment of driving after stroke—a pluridisciplinary task. Accident Analysis and Prevention. 2008;40(2):452–460. doi: 10.1016/j.aap.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Schiller JS, Lucas JW, Ward BW, et al. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2010. National Center for Health Statistics, 2012. [PubMed]
- 7.Rowe F, Brand D, Jackson CA, et al. Visual impairment following stroke: do stroke patients require vision assessment? Age and Ageing. 2009;38(2):188–193. doi: 10.1093/ageing/afn230. [DOI] [PubMed] [Google Scholar]
- 8.Gray CS, French JM, Bates D, Cartlidge NEF, Venables GS, James OFW. Recovery of visual fields in acute stroke: homonymous hemianopia associated with adverse prognosis. Age and Ageing. 1989;18(6):419–421. doi: 10.1093/ageing/18.6.419. [DOI] [PubMed] [Google Scholar]
- 9.Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V. Natural history of homonymous hemianopia. Neurology. 2006;66(6):901–905. doi: 10.1212/01.wnl.0000203338.54323.22. [DOI] [PubMed] [Google Scholar]
- 10.Çelebisoy M, Çelebisoy N, Bayam E, Köse T. Recovery of visual-field defects after occipital lobe infarction: a perimetric study. Journal of Neurology, Neurosurgery and Psychiatry. 2011;82(6):695–702. doi: 10.1136/jnnp.2010.214387. [DOI] [PubMed] [Google Scholar]
- 11.Tiel K, Kolmel HW. Patterns of recovery from homonymous hemianopia subsequent to infarction in the distribution of the posterior cerebral artery. Neuro-Ophthalmology. 1991;11(1):33–39. [Google Scholar]
- 12.Townend BS, Sturm JW, Petsoglou C, O’Leary B, Whyte S, Crimmins D. Perimetric homonymous visual field loss post-stroke. Journal of Clinical Neuroscience. 2007;14(8):754–756. doi: 10.1016/j.jocn.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 13.Yates JS, Lai SM, Duncan PW, Studenski S. Falls in community-dwelling stroke survivors: an accumulated impairments model. Journal of Rehabilitation Research and Development. 2002;39(3):385–394. [PubMed] [Google Scholar]
- 14.Warren M. Pilot study on activities of daily living limitations in adults with hemianopsia. American Journal of Occupational Therapy. 2009;63(5):626–633. doi: 10.5014/ajot.63.5.626. [DOI] [PubMed] [Google Scholar]
- 15.Bowers AR, Mandel AJ, Goldstein RB, Peli E. Driving with hemianopia, I: detection performance in a driving simulator. Investigative Ophthalmology & Visual Science. 2009;50(11):5137–5147. doi: 10.1167/iovs.09-3799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bronstad PM, Bowers AR, Albu A, et al. Hazard detection by drivers with paracentral homonymous field loss: a small case series. Journal of Clinical & Experimental Ophthalmology. 2011;5:p. 1. [PMC free article] [PubMed] [Google Scholar]
- 17.Papageorgiou E, Hardiess G, Ackermann H, et al. Collision avoidance in persons with homonymous visual field defects under virtual reality conditions. Vision Research. 2012;52(1):20–30. doi: 10.1016/j.visres.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 18.Papageorgiou E, Hardiess G, Schaeffel F, et al. Assessment of vision-related quality of life in patients with homonymous visual field defects. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2007;245(12):1749–1758. doi: 10.1007/s00417-007-0644-z. [DOI] [PubMed] [Google Scholar]
- 19.O’Neill EC, Connell PP, O’Connor JC, Brady J, Reid I, Logan P. Prism therapy and visual rehabilitation in homonymous visual field loss. Optometry and Vision Science. 2011;88(2):263–268. doi: 10.1097/OPX.0b013e318205a3b8. [DOI] [PubMed] [Google Scholar]
- 20.Chen CS, Lee AW, Clarke G, et al. Vision-related quality of life in patients with complete homonymous hemianopia post stroke. Topics in Stroke Rehabilitation. 2009;16(6):445–453. doi: 10.1310/tsr1606-445. [DOI] [PubMed] [Google Scholar]
- 21.Bowers AR, Keeney K, Peli E. Community-based trial of a peripheral prism visual field expansion device for hemianopia. Archives of Ophthalmology. 2008;126(5):657–664. doi: 10.1001/archopht.126.5.657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vargas-Martín F, García-Pérez MA. Visual fields at the wheel. Optometry and Vision Science. 2005;82(8):675–681. doi: 10.1097/01.opx.0000175624.34252.73. [DOI] [PubMed] [Google Scholar]
- 23. DVLA Drivers Medical Group: For medical practitioners. At a glance guide to the current medical standards of fitness to drive. Swansea, UK, Driver Vehicle Licensing Authority, 2011.
- 24.Silveira S, Jolly N, Heard R, Clunas NJ, Kay L. Current licensing authority standards for peripheral visual field and safe on-road senior aged automobile driving performance. Clinical & Experimental Ophthalmology. 2007;35(7):612–620. doi: 10.1111/j.1442-9071.2007.01544.x. [DOI] [PubMed] [Google Scholar]
- 25.Peli E. Low vision driving in the USA: who, where, when and why. CE Optometry. 2002;5(2):54–58. [Google Scholar]
- 26.Yazdan-Ashoori P, ten Hove M. Vision and driving: Canada. Journal of Neuro-Ophthalmology. 2010;30(2):177–185. doi: 10.1097/WNO.0b013e3181dfa982. [DOI] [PubMed] [Google Scholar]
- 27.Dow J. Visual field defects may not affect safe driving. Traffic Injury Prevention. 2011;12(5):483–490. doi: 10.1080/15389588.2011.582906. [DOI] [PubMed] [Google Scholar]
- 28.Tant MLM, Brouwer WH, Cornelissen FW, et al. Driving and visuospatial performance in people with hemianopia. Neuropsychological Rehabilitation. 2002;12(5):419–437. [Google Scholar]
- 29.Wood JM, McGwin G, Jr., Elgin J, et al. On-road driving performance by persons with hemianopia and quadrantanopia. Investigative Ophthalmology & Visual Science. 2009;50(2):577–585. doi: 10.1167/iovs.08-2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Racette L, Casson EJ. The impact of visual field loss on driving performance: evidence from on-road driving assessments. Optometry and Vision Science. 2005;82(8):668–674. doi: 10.1097/01.opx.0000174719.25799.37. [DOI] [PubMed] [Google Scholar]
- 31.Szlyk JP, Brigell M, Seiple W. Effects of age and hemianopic visual field loss on driving. Optometry and Vision Science. 1993;70(12):1031–1037. doi: 10.1097/00006324-199312000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Bowers AR, Mandel AJ, Goldstein RB, Peli E. Driving with hemianopia, II: lane position and steering in a driving simulator. Investigative Ophthalmology & Visual Science. 2010;51(12):6605–6613. doi: 10.1167/iovs.10-5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wood JM, McGwin G, Elgin J, et al. Hemianopic and quadrantanopic field loss, eye and head movements, and driving. Investigative Ophthalmology & Visual Science. 2011;52(3):1220–1225. doi: 10.1167/iovs.10-6296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen JM. An overview of enhancement techniques for peripheral field loss. Journal of the American Optometric Association. 1993;64(1):60–70. [PubMed] [Google Scholar]
- 35.Szlyk JP, Seiple W, Stelmack J, McMahon T. Use of prisms for navigation and driving in hemianopic patients. Ophthalmic and Physiological Optics. 2005;25(2):128–135. doi: 10.1111/j.1475-1313.2004.00265.x. [DOI] [PubMed] [Google Scholar]
- 36.Peli E. Field expansion for homonymous hemianopia by optically induced peripheral exotropia. Optometry and Vision Science. 2000;77(9):453–464. doi: 10.1097/00006324-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Giorgi RG, Woods RL, Peli E. Clinical and laboratory evaluation of peripheral prism glasses for hemianopia. Optometry and Vision Science. 2009;86(5):492–502. doi: 10.1097/OPX.0b013e31819f9e4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peli E. Peripheral field expansion device. United States patent US 7, 374, 284 B2. 2008.
- 39.Bronstad PM, Bowers AR, Albu A, et al. Driving with central visual field loss I: impact of central scotoma on response to hazards. doi: 10.1001/jamaophthalmol.2013.1443. JAMA Ophthalmology. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bowers A, Peli E, Elgin J, McGwin G, Owsley C. On-road driving with moderate visual field loss. Optometry and Vision Science. 2005;82(8):657–667. doi: 10.1097/01.opx.0000175558.33268.b5. [DOI] [PubMed] [Google Scholar]
- 41.Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Glaucoma and on-road driving performance. Investigative Ophthalmology & Visual Science. 2008;49(7):3035–3041. doi: 10.1167/iovs.07-1609. [DOI] [PubMed] [Google Scholar]
- 42.Vanier M, Gauthier L, Lambert J, et al. Evaluation of left visuospatial neglect: norms and discrimination power of two tests. Neuropsychology. 1990;4(2):87–96. [Google Scholar]
- 43.Schenkenberg T, Bradford DC, Ajax ET. Line bisection and unilateral visual neglect in patients with neurologic impairment. Neurology. 1980;30(5):509–517. doi: 10.1212/wnl.30.5.509. [DOI] [PubMed] [Google Scholar]
- 44.Folstein MF, Folstein SE, McHugh PR. ‘Mini-mental state’: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 45.Iorizzo DB, Riley ME, Hayhoe M, Huxlin KR. Differential impact of partial cortical blindness on gaze strategies when sitting and walking—an immersive virtual reality study. Vision Research. 2011;51(10):1173–1184. doi: 10.1016/j.visres.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lane AR, Smith DT, Schenk T. Clinical treatment options for patients with homonymous visual field defects. Clinical Ophthalmology. 2008;2(1):93–102. doi: 10.2147/opth.s2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pambakian ALM, Mannan SK, Hodgson TL, Kennard C. Saccadic visual search training: a treatment for patients with homonymous hemianopia. Journal of Neurology, Neurosurgery and Psychiatry. 2004;75(10):1443–1448. doi: 10.1136/jnnp.2003.025957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roth T, Sokolov AN, Messias A, Roth P, Weller M, Trauzettel-Klosinski S. Comparing explorative saccade and flicker training in hemianopia: a randomized controlled study. Neurology. 2009;72(4):324–331. doi: 10.1212/01.wnl.0000341276.65721.f2. [DOI] [PubMed] [Google Scholar]
- 49.Owsley C, McGwin G. Vision and driving. Vision Research. 2010;50(23):2348–2361. doi: 10.1016/j.visres.2010.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pollock A, Hazelton C, Henderson CA, et al. Interventions for visual field defects in patients with stroke. Cochrane Database of Systematic Reviews. 2011;(10) doi: 10.1002/14651858.CD008388.pub2.CD008388 [DOI] [PubMed] [Google Scholar]


