Summary
Background
The short stay unit (SSU) is a ward providing targeted care for patients requiring brief hospitalization and dischargeable as soon as clinical conditions are resolved. Therefore, SSU is an alternative to the ordinary ward (OW) for the treatment of selected patients. The SSU model has been tested in only a few hospitals, and the literature lacks systematic evaluation of the impact of SSU use. The aim of our study was to evaluate the use of SSUs in terms of length of hospital stay, mortality and readmission rate.
Material/Methods
A random effect meta-analysis was carried out by consulting electronic databases. Studies were selected that focused on comparison between use of SSUs and OWs. Mean difference of length of stay was calculated within 95% confidence intervals.
Results
Six articles were selected, for a total of 21 264 patients. The estimated mean difference was −3.06 days (95% CI −4.71, −1.40) in favor of the SSU. The selected articles did not show any differences in terms of mortality and readmission rate.
Conclusions
Use of SSUs could reduce patient length of stay in hospital, representing an alternative to the ordinary ward for selected patients. A shorter period of hospitalization could reduce the risk of hospital-acquired infections, increase patient satisfaction and yield more efficient use of hospital beds. Findings of this study are useful for institutional, managerial and clinical decision-makers regarding the implementation of the SSU in a hospital setting, and for better management of continuity of care.
Keywords: monday to friday clinic, monday to friday surgery ward, short stay hospitalization, alternative to conventional hospitalization, alternative admissions, new option for patient care, week hospital, short stay surgery, short stay surgical unit, short-stay unit, short stay hospital unit, short stay clinic, short stay medical unit, unitad medica de estancia corta, optimize hospital resource, cost effectiveness, safety, effectiveness and safety
Background
Appropriateness of care is a major issue in provision of modern health services, and a large portion of delivered health care services could be considered as inappropriate [1]. Appropriateness is related to the quality of service and to the setting where care is provided [2]. Appropriate services provide high quality care in a setting according to the patient’s clinical characteristics [2]. A setting is inappropriate when the patient’s admission in hospital is not necessary or when the length of stay is longer than needed [3].
Inappropriateness is associated with the challenges hospitals face in efficiently admitting patients from emergency services and from waiting lists [4–6].
Reduction in number of inappropriate admissions and length of stay requires new hospital organization as an alternative to the ordinary ward.
The Short Stay Unit (SSU) can be considered as an alternative to conventional hospitalization.
The Short Stay Unit (SSU) is a type of admission that can provide targeted care for patients requiring brief hospitalization (≤5 days), as well as patients ready to be discharged as soon as their clinical condition is resolved. Usually, the SSU is open from Monday to Friday, 24 hours a day, and provides the same level of medical care as an ordinary ward.
The SSU was first introduced in the 1970’s, and the earliest models were designed to meet the special needs of pediatric and surgical patients. Subsequent models targeted general medical patients and critically ill patients [8–15].
The organizational models of these units in different countries show significant differences, even if the more common model is designed for patients with exacerbated chronic pathologies, requiring continuous care for more than 2 and less than 5 days [12].
The SSU model has been tested in only a few hospitals, and a systematic evaluation of the impact of SSU use in a hospital setting is not yet available in the scientific literature.
The objective of our study was to assess the impact of use of SSUs in hospital settings, evaluating the effectiveness of SSUs in terms of length of stay, mortality and readmission rates.
Material and Methods
Search strategy
An extensive search of the scientific literature was carried out by querying electronic databases to identify relevant studies: Pubmed; Embase; Google Scholar; Dare; Cochrane Library; Sumsearch; Scirus (last consultation April 2009). Language limitations were not used in our search strategy. The keywords used to search articles were associated to typology of hospital admission, ward definition, and outcomes. The following search terms were used: Terms related to type of hospital admission: Monday to Friday clinic, Monday to Friday surgery ward, Short Stay Hospitalization, alternative to conventional hospitalization, alternative admissions, new option for patient care.
Terms associated with ward definition: Week Hospital, short stay surgery, Short stay surgical unit, Short-stay unit, Short Stay Hospital Unit, Short Stay Clinic, Short Stay Medical Unit, Unitad Medica de estancia corta.
Terms related to outcomes: optimize hospital resource, cost effectiveness, safety, effectiveness and safety.
A further analysis of the grey literature was conducted in generic search engines, consulting ‘Google Scholar’ and looking for unpublished studies about Short Stay Unit.
Electronic searches were combined with hand searching, manually checking the reference lists of relevant articles and contacting experts working in the field to identify further studies.
Inclusion criteria
Studies comparing SSUs with ordinary wards were included. Studies focusing on SSUs used for clinical or post-operative stay were chosen.
Articles with patients requiring a brief hospitalization (≤3 days) and ready to be discharged within a maximum of 5 days were included. Included studies had to measure at least 1 of the following outcomes: length of stay, mortality rate or readmission rate.
Data extraction and data analysis
Data were extracted using a standardized form including information on: authors, year of publication, patient selection criteria, length of stay, mortality and readmission rates.
The mean difference of length of stay was estimated, within 95% confidence intervals, applying a random effects model. A sensitivity analysis was carried out to assess the robustness of our study.
Quality assessment
The methodology of each study was assessed independently by 2 authors (L.P. and V.V.), according to a score based on 5 potential sources of bias [16,17]. Disagreements were resolved by a third epidemiologist (G. D.) or by consensus.
Our study considered the method of allocation to study groups (random, 2; vs. quasi-random, 1; vs. selected concurrent controls, 0), data analysis and presentation of results (appropriate statistical analysis and clear presentation of results, 2; inappropriate statistical analysis or unclear presentation of results, 1; inappropriate statistical analysis and unclear presentation of results, 0), the presence of baseline differences between the groups that were potentially linked to study outcomes (of particular importance for observational studies; no baseline differences present or appropriate statistical adjustments made for differences, 2; vs. baseline differences present and no statistical adjustments made, 1; vs. baseline characteristics not reported, 0), the objectivity of the outcome (objective outcomes or subjective outcomes with blinded assessment, 2; vs. subjective outcomes with no blinding but clearly defined assessment criteria, 1; vs. subjective outcomes with no blinding and poorly defined, 0), and the completeness of followup for the appropriate unit of analysis (90%, 2; vs. 80–90%, 1; vs. 80% or not described, 0).
The cut-off value for including an article in our revision was 6/10.
Results
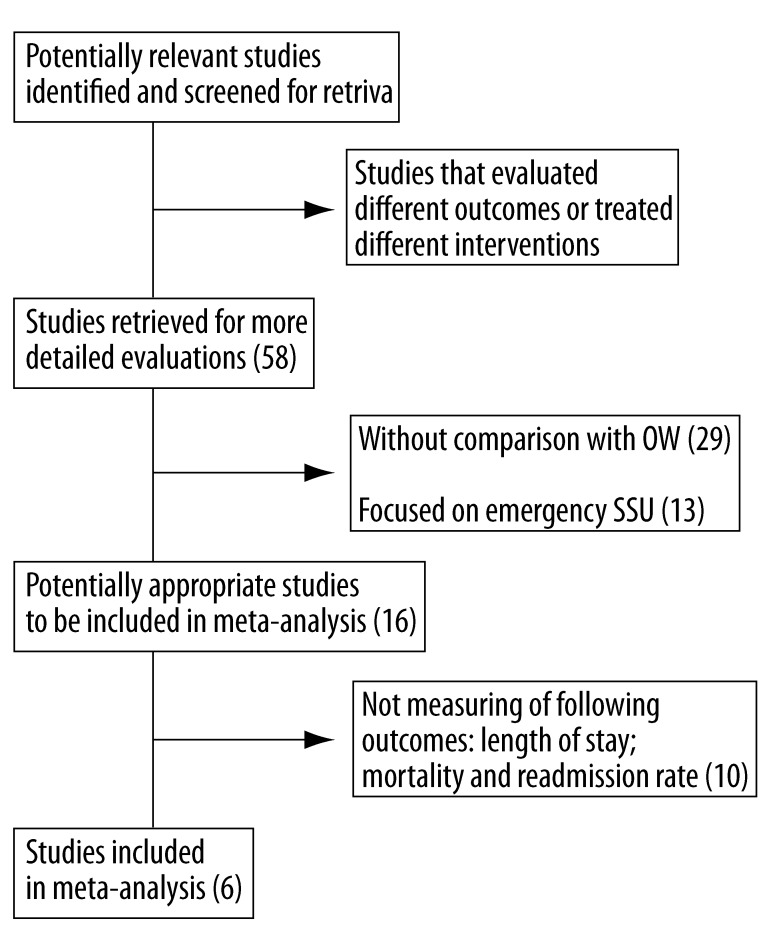
After searching electronic databases, 58 potentially relevant studies were identified by abstract and title; 29 articles were excluded because they evaluated SSU without a quantitative comparison with OW; 13 articles were not included because they were focused on emergency SSU (Figure 1); 6 articles (Table 1), dated from 1995 to 2008, met the selection criteria and were included in the revision.
Figure 1.
Article eelection.
Table 1.
Selected articles.
| Authors | Country | Year | Type of ward | Typology of comparison | Quality scores |
|---|---|---|---|---|---|
| Hedenbro JL | Sweden | 1995 | Post operative | Ordinary ward | 10/10 |
| Downing H | England | 2004 | Acute illness | Ordinary ward | 8/10 |
| Broquetas JM | Spain | 2008 | Asthma, pneumonia or suspected lung cancer | Period before SSU implementation | 8/10 |
| Guirao Martinez R | Spain | 2008 | Acute illness | Ordinary ward | 8/10 |
| Puig J | Spain | 2007 | Diabetic patients | Period before SSU implementation | 7/10 |
| Schmidt C | Germany | 2006 | Post operative | Ordinary ward | 6/10 |
The final analysis considered a total of 21,264 patients (3463 admitted in SSU and 21,264 in OW). The agreement on selection of relevant articles was 100%.
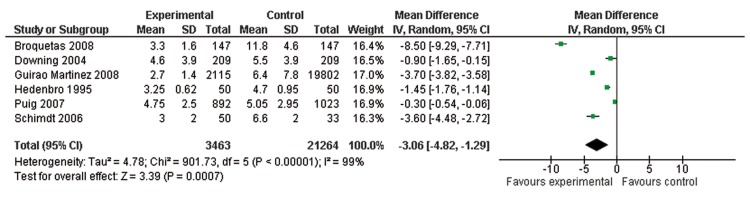
The estimated mean difference was −3.06 days (95% CI − 4.82, −1.29) in favor of SSU (Figure 2). Sensitivity analysis confirmed the robustness of the results.
Figure 2.
Forest plot of length of stay.
The χ2 test analysis showed the presence of heterogeneity among studies (χ2=901.73; p=0.007).
The number of selected studies evaluating mortality and readmission rate was not sufficient to perform a pooled estimate.
The selected articles did not show any differences between SSU and OW in terms of mortality (Table 2) and readmission rates (Table 3).
Table 2.
Death rate.
| Authors | Number of patients | Mortality |
|---|---|---|
| Broquetas JM | 147 vs. 147 | Unchanged |
| Puig J | 1023 vs. 892 (223 vs. 212) | No significant difference |
Table 3.
Readmission rate.
| Authors | Number of patients | Readmission |
|---|---|---|
| Downing H | 209 vs. 209 | Unchanged |
| Broquetas JM | 147 vs. 147 | 15% vs. 21% |
| Puig J | 1023 vs. 892 (223 vs. 212) | No significant difference |
Discussion
The results of our revision emphasize that use of the SSU could reduce length of stay compared with an ordinary ward. Despite the lack of a quantitative pooled estimate for mortality and readmission rates, the selected articles showed no differences for these outcomes. According to the scientific evidence [13], our results suggest that SSU patients can be safely and effectively treated without any increase in mortality and readmission rates. SSU patients could be discharged to home sooner, increasing the ward efficiency without compromising the effectiveness of care [14].
Use of SSUs might reduce the risk of nosocomial illnesses related to prolonged hospitalization, as well as retaining better patient psychological condition and quality of life.
The use of SSUs also positively affects hospital organization through improved use of resources related to an expanded bed pool and increased hospital turnover. The reduced use of hospital beds and optimization of the turnover rate of hospital staff could minimize economic losses, and reduce hospital costs and waste of personnel time [11,15,20].
The organizational change related to the introduction of SSU use in a hospital does not require additional personnel or hospital beds, allowing a rational use of limited resources coupled with measurable benefits for the patients [13].
Furthermore, reorganizing patient admission protocols could help hospitals to much better satisfy the needs of a considerable proportion of patients [15].
The use of SSUs supports the admission and discharge planning for selected patients, and might facilitate the management of continuity of care among different providers [18].
In particular, use of SSUs could facilitate the bridging of pre-hospitalization phase and post-hospitalization phases, allowing the design of a single managed care plan covering the entire continuum of care for some chronic diseases.
Our study is limited by the presence of heterogeneity among studies, attributable to differences in selected groups of patients. However, random effects analysis performed on selected studies incorporate the heterogeneity in the pooled estimate, assuming that the effects in the different studies follow some distribution and are not identical, and considering the differences as if they were random [21]. Furthermore, the mean difference of length of stay is in favor of SSU for all selected studies.
Another limitation of our study is its lack of studies investigating mortality and readmission rate; for this reason our results cannot confirm the impact of SSUs on these outcomes.
Conclusions
Our findings show some potential benefits of SSUs and support the implementation of this organizational model in hospital settings.
Further studies should focus on accurate definition of criteria for identifying patients suitable for SSU admission, as well as evaluating cost effectiveness of the implementation of SSU use.
The SSU should be considered as a potentially efficient alternative to the ordinary ward, without any impact on the safety of selected patients. Findings of this study are useful for institutional, managerial and clinical decision-makers for implementation of the SSU in a hospital setting, and for better management of continuity of care.
Footnotes
Source of support: Self financing
References
- 1.Hammond CL, Phillips MF, Pinnington LL, et al. Appropriateness of acute admissions and last in-patient day for patients with long term neurological conditions. BMC Health Serv Res. 2009;27:9–40. doi: 10.1186/1472-6963-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lavis JN, Anderson GM. Appropriateness in health care delivery: definitions, measurement and policy implications. CMAJ. 1996;154(3):321–28. [PMC free article] [PubMed] [Google Scholar]
- 3.Hammond CL, Pinnington LL, Phillips MF. A qualitative examination of inappropriate hospital admissions and lengths of stay. BMC Health Serv Res. 2009;5:9–44. doi: 10.1186/1472-6963-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Restuccia JD, Payane SM, Lenhart G, et al. Assessing the appropriateness of hospital utilization to improve efficiency and competitive position. Health Care Manage Rev. 1987;12(3):17–27. doi: 10.1097/00004010-198701230-00006. [DOI] [PubMed] [Google Scholar]
- 5.Siu AL, Manning WG, Benjamin B. Patient, provider and hospital characteristics associated with inappropriate hospitalization. Am J Public Health. 1990;80(10):1253–56. doi: 10.2105/ajph.80.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rasmussen L, Münter D, Bøttcher C, et al. Appropriate use of hospital days in medical wards. Ugeskr Laeger. 2006;168(1):25–29. [PubMed] [Google Scholar]
- 7.Juan A, Salazar A, Alvarez A, et al. Effectiveness and safety of an emergency department short-stay unit as an alternative to standard inpatient hospitalisation. Emerg Med J. 2006;23(11):833–37. doi: 10.1136/emj.2005.033647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cerce JD, Reiss JB. Short stay unit servess overnight medical and surgical patients. Hospitals. 1981;16:141–43. [PubMed] [Google Scholar]
- 9.Laskin DM. The short-stay surgical facility: something-old something-new. J Oral Surg. 1972;30:394. [PubMed] [Google Scholar]
- 10.Barbado JM, Jimeno A, Ostolaza JM, Molinero J. Unidades de estancia corta dependientes de Medicina Interna. An Med Interna. 1999;16:504–10. [PubMed] [Google Scholar]
- 11.Gaspoz J, Lee T, Weistern M, et al. Cost-effectiveness of a new short stay unit to “rule out” acute myocardial infarction in a low risk patients. J Am Coll Cardiol. 1994;24:1249–59. doi: 10.1016/0735-1097(94)90106-6. [DOI] [PubMed] [Google Scholar]
- 12.Puig J, Supervía A, Márquez MA, et al. Diabetes team consultation: Impact on length of stay of diabetic patients admitted to a short-stay unit. Diabetes Res Clin Pract. 2007;78(2):211–16. doi: 10.1016/j.diabres.2007.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Downing H, Scott C, Kelly C. Evaluation of a dedicated short-stay unit for acute medical admissions. Clinical Medicine. 2008;8(1):18–20. doi: 10.7861/clinmedicine.8-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noval J, Campoamor MT, Avanzas E, et al. Are short stay medical units an appropriate place to manage community-acquired pneumonia? An Med Interna. 2006;23:416–19. doi: 10.4321/s0212-71992006000900004. [DOI] [PubMed] [Google Scholar]
- 15.Broquetas JM, Pedreny R, Martínez-Llorens JM, et al. Short-stay respiratory unit: A new option for inpatient care. Archivos de Bronconeumologia. 2008;44(5):252–56. doi: 10.1016/s1579-2129(08)60040-3. [DOI] [PubMed] [Google Scholar]
- 16.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of computer-based clinical decision support systems on physicians performance and patient outcomes. J Am Med Assoc. 1998;280:1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 17.Damiani G, Pinnarelli L, Sammarco A, et al. Postoperative pulmonary function in open versus laparoscopic cholecystectomy: a meta-analysis of the Tiffenau index. Dig Surg. 2008;25(1):1–7. doi: 10.1159/000114193. [DOI] [PubMed] [Google Scholar]
- 18.Haggerty JL, Reid RJ, Freeman GK, et al. Continuity of care: a multidisciplinary review. BMJ. 2003;327:1219–21. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hedenbro JL, Frederiksen SG, Lundgren PO. Patients Accept a Shorter Hospital Time for Vertical Banded Gastroplasty in a Short Stay Unit: a Randomized Study. Obesity Surgery. 1995;5(1):34–37. doi: 10.1381/096089295765558123. [DOI] [PubMed] [Google Scholar]
- 20.Guirao Martinez R, Sempere Selva MT, López Aguilera I, et al. Short-stay Medical Unit, an alternative to conventional hospitalization. Revista Clinica Espanola. 2008;208(5):216–21. doi: 10.1157/13119913. [DOI] [PubMed] [Google Scholar]
- 21.Higgins JPT, Green S, editors. The Cochrane Collaboration. 2009. Cochrane Handbook for Systematic Reviews of Interventions Version 502 [updated September 2009] [Google Scholar]
- 22.Hadden DS, Dearden CH, Rocke LG. Short stay observation patients: general wards are inappropriate. J Accid Emerg Med. 1996;13:163–65. doi: 10.1136/emj.13.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt C, Reibe F, Sellschopp C, et al. Risk Scores and Outcomes after Cholecystectomy: A comparison between a University Hospital and a Short-Stay Clinic. Anales de Medicina Interna. 2006;133(5):498–503. doi: 10.1055/s-2008-1076886. [DOI] [PubMed] [Google Scholar]
- 24.Kubo G, Bucholz W, Utech J. Monday to Friday-clinic. Zentralblatt fur Chirurgie. 1978;3(6):358–63. [PubMed] [Google Scholar]
- 25.Raeder J. Bariatric procedures as day/short stay surgery: is it possible and reasonable? Current Opinion in Anesthesiology. 2007;20(6):508–12. doi: 10.1097/ACO.0b013e3282f09443. [DOI] [PubMed] [Google Scholar]
- 26.Mirnezami R, Sahai A, Symes A, Jeddy T. Day-case and short-stay surgery: the future for thyroidectomy? Int J Clin Pract. 2007;61(7):1216–22. doi: 10.1111/j.1742-1241.2006.01234.x. [DOI] [PubMed] [Google Scholar]
- 27.March S, Swart E, Robra B. Patient satisfaction with outpatient/short stay operations in a practice clinic. Gesundheitswesen. 2006;68(6):376–82. doi: 10.1055/s-2006-926868. [DOI] [PubMed] [Google Scholar]
- 28.Bitzer EM, Nickel S, Lorenz C, et al. Patient reported process and outcome indicators for clinical audit in short-stay surgery. Z Arztl Fortbild Qualitatssich. 2006;100(3):189–95. [PubMed] [Google Scholar]
- 29.Susilahti H, Suominen T, Leino-Kilpi H. Recovery of Finnish short-stay surgery patients. Medical-Surgical Nurses. 2004;13(5):326–35. [PubMed] [Google Scholar]
- 30.Kroovand RL, Perlmutter AD. Short stay surgery in pediatric urology. J Urol. 1978;120(4):483–84. doi: 10.1016/s0022-5347(17)57237-7. [DOI] [PubMed] [Google Scholar]
- 31.Noval Menéndez J, Campoamor Serrano MT, Avanzas González E, et al. Are short stay medical units an appropriate place to manage community-acquired pneumonia? Revista Clinica Española. 2008;23(9):416–19. doi: 10.4321/s0212-71992006000900004. [DOI] [PubMed] [Google Scholar]
- 32.Villalta J, Sisó A, Cereijo AC, et al. Appropriateness of hospitalization in a short stay unit of a teaching hospital. A controlled study. Medicina Clinica Spagna. 2004;122(12):454–56. doi: 10.1016/s0025-7753(04)74270-0. [DOI] [PubMed] [Google Scholar]
- 33.Abenhaim HA, Kahn SR, Raffoul J, Becker MR. Program description: A hospitalist-run, medical short-stay unit in a teaching hospital. CMAJ. 2000;163(11):1477–80. [PMC free article] [PubMed] [Google Scholar]
- 34.Rückert K, Nahrstedt U. Experiences with short-stay-surgery. Zentralblatt fur Chirurgie. 2001;126(5):353–56. doi: 10.1055/s-2001-14759. [DOI] [PubMed] [Google Scholar]
- 35.Andreu-Ballester JC, Almela-Quilis A, Ballester F, et al. Social and health characteristics of elderly patients with chronic and/or terminal diseases (PALET profile) attended in a short stay medical unit. Revista Española de Geriatria y Gerontologia. 2006;41(6):327–33. [Google Scholar]
- 36.Arendts G, MacKenzie J, Lee JK. Discharge planning and patient satisfaction in an emergency short-stay unit. EMA – Emergency Medicine Australasia. 2006;18(1):7–14. doi: 10.1111/j.1742-6723.2006.00798.x. [DOI] [PubMed] [Google Scholar]
- 37.Pascual A. Psiquis. 1995. Clinical and demographic characteristics of patients with repeated admissions in a short stay unit. [Google Scholar]
- 38.Vazquez-Noguerol Mendes R. Revista de Psicogeriatria. 2002. Characteristics of the elderly persons admitted to an adults short term hospitalization unit. [Google Scholar]
- 39.Márquez MA, Gutiérrez J, Supervía A, et al. Unidad de estancia corta: una forma de optimizar recursos hospitalarios. Calidad Asistencial. 2003;18(5) [Google Scholar]
- 40.Dallos V, Mouzas GL. An evaluation of the functions of the short-stay observation ward in the accident and emergency department. BMJ. 1981;282(6257):37–40. doi: 10.1136/bmj.282.6257.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hutchings P. Advances in anaesthesia. Some recent developments in techniques for short stay surgery. 1995;5(1):13–15. [PubMed] [Google Scholar]
- 42.Llewellyn JG. Short stay surgery. Present practices, future trends. AORN Journal. 1991;53(5):1179–91. doi: 10.1016/s0001-2092(07)69254-0. [DOI] [PubMed] [Google Scholar]