Summary
Background
Total body irradiation is a protocol used to treat acute lymphoblastic leukemia in patients prior to bone marrow transplant. It is involved in the treatment of the whole body using a large radiation field with extended source-skin distance. Therefore measuring and monitoring the skin dose during the treatment is important. Two kinds of metal oxide semiconductor field effect transistor (OneDose MOSFET and mobile MOSEFT) dosimeter are used during the treatment delivery to measure the skin dose to specific points and compare it with the target prescribed dose.
The objective of this study was to compare the variation of skin dose in patients with acute lymphatic leukemia (ALL) treated with total body irradiation (TBI) using OneDose MOSFET detectors and Mobile MOSFET, and then compare both results with the target prescribed dose.
Material/Methods
The measurements involved 32 patient’s (16 males, 16 females), aged between 14–30 years, with an average age of 22.41 years. One-Dose MOSFET and Mobile MOSFET dosimetry were performed at 10 different anatomical sites on every patient.
Results
The results showed there was no variation between skin dose measured with OneDose MOSFET and Mobile MOSFET in all patients. Furthermore, the results showed for every anatomical site selected there was no significant difference in the dose delivered using either OneDose MOSFET detector or Mobile MOSFET as compared to the prescribed dose.
Conclusions
The study concludes that One-Dose MOSFET detectors and Mobile MOSFET both give a direct read-out immediately after the treatment; therefore both detectors are suitable options when measuring skin dose for total body irradiation treatment.
Keywords: Skin Dose, Total Body Irradiation, MOSFET, acute lymphatic leukemia
Background
Acute lymphoblastic leukemia (ALL) accounts for 15% of acute leukemias [1,2]. Total body irradiation (TBI) for patients with acute lymphatic leukemia (ALL) is a vital technique used prior to bone marrow transplant [2]. TBI is used in the treatment of ALL to obliterate the malignant cells and in the mean time to support the immune system, to avoid rejection of the donor bone marrow transplant, thus to allow for successful bone marrow transplantation [2]. Since the treatment is delivered at an extended source skin distant (SSD) of 400 cm, it is important to monitor the skin dose to ensure the accuracy of the delivered dose to patients. For this procedure of extended distance, the treatment planning system (TPS) cannot perform the calculation for the dose, thus, the dose has to be calculated by a point-dose determination at the dose prescription point. The variation in the energy dependence for both MOSFETs detectors is beyond the scope of the present study. Metal oxide semiconductor field-effect transistors have 2 types of detectors, the OneDose MOSFET and the metal oxide semiconductor field-effect transistors Mobile MOSFET dose verification system dosimeter.
OneDose MOSFET detectors verification system (Figure 1) (Sicel Technologies, Inc., Morrisville, NC; distributed by Med Tec, Orange City, USA), which is a solid-state detector, now is used in radiotherapy treatment applications to measure the entrance and exit dose during the treatment [3]. The system is small (3 mm diameter, 25 mm length), factory calibrated, wireless, and easy to use. The accuracy of the detectors, as specified by the manufacturer, is ±1 cGy for a dose of less than 20 cGy and ±5% for a dose of 20 to 500 cGy (Sicel Technologies Inc). The detectors are factory calibrated with a Co-60 beam with full build-up conditions. They are normalized to a 6-MV photon beam [5], and each detector is valid for 1 use only [3].
Figure 1.
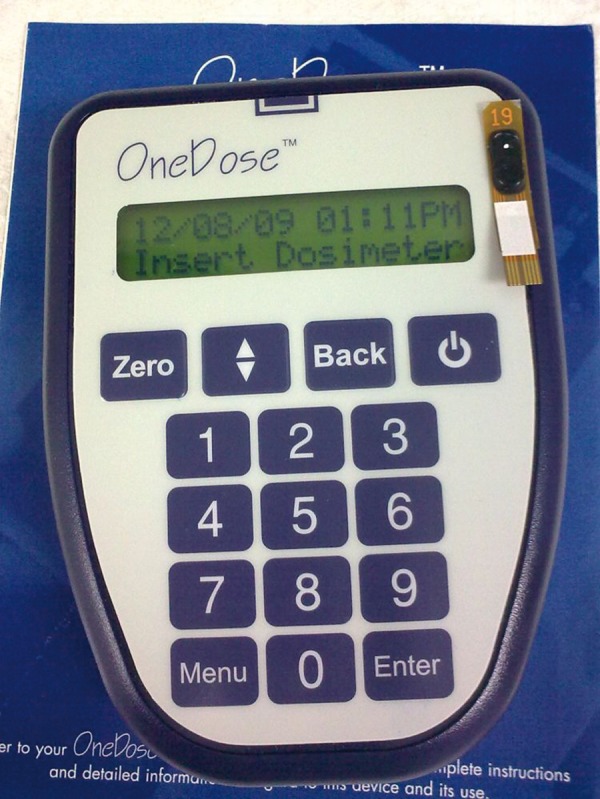
MOSEFT detectors reader.
In contrast, the Mobile MOSFET system (TN-502RD MOSFET dosimeters, Thomson and Nielsen Electronics Ltd, Ottawa, Canada) (Figure 2), consists of 5 high-sensitivity dosimeters attached to a reader. The 5 supports on the MOSFETs probes permit measurements of 5 different locations [3,5]. The attached reader records a voltage difference in each of the dosimeters when exposed to radiation. The difference between the voltages is proportional to the total amount of radiation [3]. The Mobile MOSFET channels are used in the standard basic setting, giving a normal sensitivity of ~1 mV/cGy. The overall physical size of the sensors is 1.0×1.0×3.5 mm3, and the actual sensitive volume is 0.2×0.2 mm×0.5 μm. MOSFET calibrations were performed under full buildup conditions, which then produced a very small sensing volume and less than 2% isotropy under full build-up through 360 degrees rotation. A group of MOSFET detectors were exposed to 100 cGy dose using 6 MV from Varian Clinac 2300 EX accelerator at 10 cm water equivalent depth. Both MOSFETs detectors are characterized for energy response, [5,6]; however, the details of energy depend for MOSFET is out of the scope of the present study. All 5 channels of the mobile MOSFET are made for multiple uses and can accumulate a dose up to 7000 cGy before it needs to be replaced [7]. The system is controlled by remote dose-verification software running on a personal laptop. The present study aimed to compare the target prescribed dose to the dose that is the measured by OneDose MOSFET detector and Mobile MOSFET dosimetry in order to determine which system is superior in monitoring and measuring the TBI doses.
Figure 2.
Mobile MOSEFT system.
Material and Methods
Patient selection
Patients with ALL (n=32; 16 males, 16 females) receiving total body irradiation of 1200 cGy prior to bone marrow transplantation participated in this study. Patient characteristics are summarized in Table 1. All patients consented to their treatments and were selected randomly from our patients to measure their skin dose during the treatment of TBI using dosimetry detectors. The patients were divided into 2 groups, and each group had 16 patients. For measurements, the first group was measured using OneDose MOSFET detectors, and the second group was measured using Mobile MOSFET detectors. All the anatomical sites, patient’s position and the treatment protocol were the same in both groups. All patients were treated with TBI protocol as explained in the treatment session.
Table 1.
Patient characteristics.
| Gender | Mean ±SD |
|---|---|
| Male | 22.12±5.22 |
| Female | 21.11±5.81 |
Treatment’s protocol
Monitoring skin dose during treatment is considering an essential tool for quality assurance in radiation therapy. For a treatment such as TBI it is essential to monitor the dose that is actually delivered compared to the prescribed dose. The TBI technique used in the Department of Radiation Oncology, King Fasial Specialist Hospital and Research Center, Riyadh, Saudi Arabia takes into account recommendations of the AAPM Task Group 29 [8] based on delivering 2 opposed bilateral fields (right and left lateral), allowing for sufficient field size to cover the whole body during the treatment. The patient is supine and the radiation beam is directed horizontally across the treatment room directly on the patient. The treatment was delivered at an extended source-to-surface distance (SSD) of 400 cm, with radiation field size 40×40 cm2 at 1 meter and the collimator was rotated through 45° and gantry angle of 270°, using 18 MV X-ray beams generated by a Varian Clinac-2300 EX linear accelerator (Palo Alto, California, USA). The dose rate was 200 to 300 Mu/min, depending on the patient’s separation. A 1.5 cm thick Perspex™ beam spoiler was used in front of the patient to make the dose uniform, with a total dose of 1200 cGy delivered by a hyper-fractionated technique with 6 fractions of 200 cGy twice a day over 3 days [7]. The dose was prescribed to the patients’ midline depth. Rice bags and tissue-equivalent bolus were used to compensate for missing tissues to make the dose uniform around the patient’s body [9,11].
One-Dose MOSFET Detectors were used with the first group of patients (n=16). The detectors were first zeroed by the handheld reader and then were placed at 10 selective anatomical points for every patient. The total 10 points selected in the patients to measure the skin dose were the neck (right and left), lungs (right and left), midline point of the patient (between the legs), abdominal area (right and left), right eye, umbilicus level and right knee, and the last point was the ionization chamber point which was used at the groin for absolute dose verification placed between the thighs in the mid-perineal region to monitor the dose during treatment. After the treatment the detectors were collected and then 2 minutes later each detector was placed in the handheld reader and the resulting doses were recorded.
For the second group of patients (n=16), 2 sets of Mobile MOSFET were used. One was to cover the superior part of the body and the second was to cover the inferior part of the body. The 10 individual dose points recorded by the 2 MOSFET systems were placed in the same selected 10 points as the One-Dose MOSFET. All dose measurements were carried out with the flat side of the MOSFET placed to face the beam.
Statistical analysis
Data from each sample were run in duplicate and expressed as means ±SD (cGy, n=32 patients). The results were compared using one-way ANOVA analysis followed by Tukey’s test for multiple comparison tests. Means were considered significant if P<0.05. Statistical analysis was performed by means of GraphPad Prism™ package for personal computers (GraphPad Software, Inc., San Diego, USA) and figures was performed by means of GraFit™ package for personal computers (Erithacus Software Limited, Surrey, UK).
Results
Both MOSFETs detectors show accurate and reproducible measurements. Table 1 summarizes the patients’ characteristic that been chosen for the present study. Table 2 shows the means ±SD of the measured skin doses for the selected 10 anatomical sites in each patient. The result showed that there was no significant difference between the 2 systems (One-Dose MOSFET dosimetry and the Mobile MOSFET) measurements of skin dose at the treatment of TBI as compared to the prescribed dose.
Table 2.
Measured skin doses (means ±SD, n=32 patients) for selected points in patients with One-Dose MOSFET (n=16) and Mobile MOSFET (n=16) during TBI treatment with Linac 2300 EX. The skin dose was measured for a single fraction from parallel opposed field for each patient.
| Selected points | Prescribed dose | One-Dos MOSFET | Mobile MOSFET |
|---|---|---|---|
| Right neck | 200.02±1.22 | 194.03±4.46ns | 198.02±1.82ns |
| Left neck | 199.51±0.55 | 193.02±7.98ns | 198.10±3.60ns |
| Right lung | 200.02±2.20 | 197.21±3.21ns | 198.12±3.95ns |
| Left lung | 199.92±1.42 | 195.83±5.56ns | 196.11±2.50ns |
| Chamber | 200.02±2.12 | 201.01±2.31ns | 196.01±2.21ns |
| Right abdomen | 198.88±1.11 | 195.03±5.05ns | 196.10±3.36ns |
| Left abdomen | 198.92±2.62 | 198.02±2.56ns | 193.12±3.41ns |
| Umbilicus | 200.02±2.02 | 195.05±4.19ns | 195.21±2.55ns |
| Right knee | 200.12±0.12 | 194.01±7.65ns | 196.11±2.35ns |
| Right eye | 200.10±0.10 | 194.92±4.37ns | 196.11±2.35ns |
Data are expressed as means ±SD;
– not significantly different as compared to the prescribed dose.
Discussion
Early treatment of acute lymphoblastic leukemia (ALL) with chemotherapy and radiation therapy showed a good response [11,14]. TBI is a protocol treatment for ALL during radiotherapy treatment. TBI is used in cases of ALL to demolish the cancer cells and to suppress the immune system to allow for bone marrow transplantation. TBI is considered as an essential technique used prior to bone marrow transplantation [1]. During the treatment it is important to measure and monitor the skin dose using patient dosimetry such as MOSFET or thermo-luminescent dosimetry (TLD) [15]. The present results of our study suggest that if there is any major difference between the outcome of using One-Dose MOSFET dosimeter and Mobile MOSFET in the treatment of TBI, to monitor the skin dose. It is a very important point because clinical decisions are currently made with respect to skin dose. It is necessary to monitor the skin dose and in the meantime to ensure accurate dose delivery to patients, determined by using selected points in the patient’s body for verifying the accuracy in delivering of the prescribe dose [14,18].
Our results (Table 2) show that for One-Dose MOSFETs measured dose as compared to the prescribed dose for right and left neck decreased by 3%. The percentage mean difference in the lung site (right and left) decreased by 1% and 2%, respectively. The percentage mean difference in midline point using the ionization chamber increased by 0.5%. For the abdominal area (right and left) percentage mean difference decreased by 2% and 0.5%, respectively. Umbilicus region percentage means difference decreased by 2% and at the right knee site the percentage mean difference decreased by, for the right eye the percentage means difference decrease by 3%. However, for the Mobile MOSFET measurement of the 10 selected anatomical sites, the percentage mean difference between the measured dose and the prescribed dose for the neck area (right and left) decreased by 1% and 0.7%, respectively. In the lung area (right and left) the percentage mean difference between the measured dose and the prescribed dose decreased by 1% and 2%, respectively. The midline ionization chamber dose using Mobile MOSFET gave a decreased percentage mean difference of 2% as compared with the midline prescribed dose. For the abdominal area, in both right and left, the percentage mean difference between the measured and prescribed doses decreased by 1% and decreased by 3%, respectively. The umbilicus percentage mean difference decreased by 2%, the percentage mean different right knee decreased by 2%, and for the right eye the percentage means difference decrease by 2%. For the midline, which is the point of the ionization chamber, it was proven that the dose delivered matched the prescribed dose with upper and lower dose limits, decreased by only 0.5% of the prescribed dose. However, our data showed that there is no significant difference between the measured dose by using any MOSFETs system and the prescribed dose as shown in Table 2.
It is possible that the small and insignificant differences in the results for the both MOSFETs and prescribed dose could be the results of the additional buildup from the rice bag and/or the bolus that was placed on the patient’s anatomical sites. Because of the use of a 1.5-cm acrylic spoiler plate, the bolus, and the large field size, should have been in a relatively flat dose region close to the depth of the maximum dose [14,15]. Furthermore, although the MOSFET has an inherent buildup of 0.88 mm, we had expected that the dose absorbed by both of the MOSFET detectors should have been nearly the same at most of the selected points. The addition of the rice bag (with an approximate thickness of 2 cm) put those detectors beyond the depth of the maximum dose, where the additional inherent buildup of the MOSFETs should have led to a negligible decrease in the percent difference by 3% as compared with the measurements close to depth of the maximum dose. Finally, our study is limited by inadequate treatment plans and dose calculation procedure, such as wrong inverse square law corrections or errors due to limitations of the two-dimensional treatment planning system used. Our results are consistent with previous studies [17–22] in finding no variation between the measured doses using any MOSFETs system as compared to the prescribed dose.
Conclusions
The results show accurate and reproducible measurements with both MOSFETs dosimeters. Both the One-Dose MOSFET and the Mobile MOSFET are suitable options for measuring skin dose for total body irradiation treatment. Both systems can provide valuable skin dose information in areas where the treatment planning system may not be accomplished, such as for TBI.
Acknowledgments
The authors would like to express their gratitude to all of our patients who participated in this study and without who the study could not have been completed. In addition, the authors would like to extend their thanks to King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia and to Radiological Sciences Dept, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia for their continuous support.
Footnotes
Source of support: Departmental sources
References
- 1.Foa R, Vitale A. Towards an integrated classification of adult acute lymphoblastic leukemia. Rev Clin Exp Hematol. 2002;6:181–99. doi: 10.1046/j.1468-0734.2002.00070.x. [DOI] [PubMed] [Google Scholar]
- 2.Urasinski T, Urasinska E, Grabarek J, et al. Good early treatment response in childhood acute lymphoblastic leukemia is associated with Bax nuclear accumulation and PARP cleavage. Med Sci Monit. 2009;15(6):CR294–301. [PubMed] [Google Scholar]
- 3.Diana G, Connolly B, Gordon C. Entrance skin dose measured with MOSFETs in children undergoing interventional radiology procedures. Pediatr Radiol. 2008;38:1180–87. doi: 10.1007/s00247-008-0966-y. [DOI] [PubMed] [Google Scholar]
- 4.Bilsk P. Response of various life thermoluminescent detectors to high energy ions results of the ICCHIBAN experiment. Nucl Instr Meth Phys Res B. 2009;251:121–26. [Google Scholar]
- 5.Lavallée M, Gingras L, Beaulieu C. Energy and integrated dose dependence of MOSFET dosimeter sensitivity for irradiation energies between 30 kV and 60Co. Med Phys. 2006;33(10):3683–89. doi: 10.1118/1.2349301. [DOI] [PubMed] [Google Scholar]
- 6.Soubra M, Cygler J, Mackay G. Evaluation of a dual bias dual metal oxide-silicon semiconductor field effect transistor detector as radiation dosimeter. Med Phys. 1994;21(4):567–72. doi: 10.1118/1.597314. [DOI] [PubMed] [Google Scholar]
- 7.AAPM Task Group 29. American association of physicists in medicine. 1986. The physical aspects of total and half body photon irradiation radiation therapy. [Google Scholar]
- 8.Panettieri V, Duch M, et al. Monte Carlo simulation of MOSFET detectors for high-energy photon beams using the PENELOPE code. Phy Med Biol. 2007;52:303–16. doi: 10.1088/0031-9155/52/1/020. [DOI] [PubMed] [Google Scholar]
- 9.Bufacchi A, Carosi A, Adorante N, et al. In vivo EBT radiochromic film dosimetry of electron beam for total skin electron therapy (TSET) Physica Medica. 2007;23(2):67–72. doi: 10.1016/j.ejmp.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 10.Sjögren R, Karlsson M, Karlsson M, Sevennon H. Depth for dose calibration in high energy photon beams. Radiother Oncol. 1997;43(3):311–13. doi: 10.1016/s0167-8140(97)00062-5. [DOI] [PubMed] [Google Scholar]
- 11.Lin M, Toncheva G, Nguyen G, et al. Application of MOSFET detectors for dosimetry in small animal radiography using short exposure times. Radiat Res. 2008;170(2):260–63. doi: 10.1667/RR1328.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cannizzo E, Carulli E, Buda G, et al. Meningeal relapse in a case of B acute lymphoblastic leukemia: The role of CD56 expression. Med Sci Monit. 2009;15(2):CS27–29. [PubMed] [Google Scholar]
- 13.Jornet N, Carrasco P, Jurado D, et al. Comparison study of MOSFET detectors and diodes for entrance in vivo dosimetry in 18 MV x-ray beams. Med Phys. 2004;31:2534–42. doi: 10.1118/1.1785452. [DOI] [PubMed] [Google Scholar]
- 14.Best Medical Canada. Thomson Nielsen mobile MOSFET operator’s manual. Best Medical Canada; Ottawa, Canada: 2008. [Google Scholar]
- 15.Kortov V. Materials for the thermoluminescent dosimetry: Current status and future trends. Radiat Meas. 2007;42:576–81. [Google Scholar]
- 16.Palmans H, Nafaa L, Patoul N, et al. A dosimetry study comparing NCS report-5, IAEA TRS-381, AAPM TG-51 and IAEA TRS-398. Phys Med Biol. 2003;48:1091–107. doi: 10.1088/0031-9155/48/9/301. [DOI] [PubMed] [Google Scholar]
- 17.Gurp E, Mijnheer B, Verschueren T, et al. Total body irradiation, toward optimal individual delivery: dose evaluation with metal oxide field effect transistors, thermoluminescence detectors, and a treatment planning system. Int J Radiat Oncol Biol Phys. 2007;69(4):1297–304. doi: 10.1016/j.ijrobp.2007.07.2334. [DOI] [PubMed] [Google Scholar]
- 18.Mukundan S, Inman P, Frush D, et al. MOSFET dosimetry for radiation dose assessment of bismuth shielding of the eye in children. Am J Roentgenol. 2007;188:1648–50. doi: 10.2214/AJR.06.1146. [DOI] [PubMed] [Google Scholar]
- 19.Kinhikar RA, Murthy V, Goel V, et al. Skin dose measurements using MOSFET and TLD for head and neck patients treated with tomotherapy. Appl Radiat Isot. 2009;67(9):1683–85. doi: 10.1016/j.apradiso.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 20.Best S, Ralston A, Suchowerska N. Clinical application of the OneDose™ patient dosimetry system for total body irradiation. Phys Med Biol. 2005;50:5909–19. doi: 10.1088/0031-9155/50/24/010. [DOI] [PubMed] [Google Scholar]
- 21.Ramani R, Russell S, O’Brien P. Clinical dosimetry using MOSFETs. Int J Radiat Oncol Biol Phys. 1997;37:959–64. doi: 10.1016/s0360-3016(96)00600-1. [DOI] [PubMed] [Google Scholar]
- 22.Al-Mohammed H, Mahyoub F, Moftah B. Comparative study on skin dose measurement using MOSFET and TLD for pediatric patients with acute lymphatic leukemia. Med Sci Monit. 2010;16(7):CR325–29. [PubMed] [Google Scholar]


