Summary
Background
We assessed prevalence and resistance of uropathogens on antimicrobial agents (AA) from urine cultures (UC) in children hospitalized with urinary tract infections (UTI) at University Hospital in Split.
Material/Methods
During the 7-year period, children hospitalized only once with UTI alone were compared to those repeatedly hospitalized, and who received long-term antimicrobial prophylaxis (LTAP), as well as those with associated anomalies of the urinary system (US).
Results
E. coli was the most frequent isolate (67.7%) with resistance to ampicillin by 69.5%, amoxicillin/clavulonic acid by 3.5%, cephalexin by 6.6%, trimethoprim/sulfamethoxazole (TMP-SMX) by 27.5%, and nitrofurantoin by 0.4%. For other uropathogens, AA resistance rates were the following: 64.3%, 5.8%, 10.5%, 21.3%, and 7.9%. The high or increasing resistance to TMP-SMX is characterized by all uropathogens. Patients with anomalies of US showed a lower prevalence of E. coli and Enterococcus sp., but a higher prevalence of Pseudomonas sp., ESBL-producing E. coli and Klebsiella sp. than those without US anomalies. Repeatedly hospitalized patients showed a lower prevalence of E. coli, but a higher prevalence of Pseudomonas sp. and Klebsiella sp. than patients hospitalized only once. Both groups displayed significantly less resistance of Enterococcus sp. In patients receiving LTAP before hospitalization, E. coli was significantly more resistant to ampicillin, amoxicillin/clavulonic acid and TMP/SMX than in those without LTAP.
Conclusions
Based on our results, we recommend excluding ampicillin altogether, and reconsideration of further use of TMP-SMX, as well as use of nitrofurantoin, cephalexin and amoxicillin/clavulonic acid for LTAP in our region.
Keywords: children, urinary tract infection, antibiotics, resistance pattern
Background
Urinary tract infection (UTI) is a significant cause of morbiditiy among children, and may result in permanent parenchymal damage with the possible development of late complications such as arterial hypertension or chronic renal failure. The likelihood of developing these late complications in UTIs is the greatest in the first year of life, but gradually decreases in older children [1,2]. Following the treatment of a full dose of antibiotics for symptomatic UTI, long-term antibacterial prophylaxis (LTAP) is applied. The aim of LTAP is to prevent a recurring urinary infection and the potential for permanent tissue damage. Recurrent UTI with or without vesico ureteral reflux in children is the most frequent indication for LTAP [2,3]. The idea of LTAP is to provide small levels of antimicrobial agents (AA) in the urinary system, sufficient to prevent bacterial multiplication [4]. Aside from some controversies regarding the use of LTAP, widely accepted indications for LTAP are as follows: vesico ureteral reflux, recurrent UTI with or without associated anomalies, febrile UTI in the first year of life, prenatal hydronephrosis due to obstruction or vesico ureteral reflux, and UTI associated with voiding disturbances or the weakness of the immune system. LTAP is usually administered in a single daily dose equivalent to a quarter or half of the conventional therapeutic dose. The most commonly prescribed medication is nitrofurantoin in children after the first year of life and trimethoprim/sulfamethoxazole (TMP/SMX) in children older than 3 months. For newborns and infants less than 3 months of age, prescribed antibiotics for LTAP are amoxicillin/clavulonic acid and cephalosporins. However, quinolones are not regularly prescribed in children [3]. Limitations of LTAP include relative ineffectiveness, increasing microbial resistance rates that are proportionate to the duration of treatment, adverse effects, poor compliance and cost [3,5]. Some authors reported a growing bacterial resistance to common AAs used in LTAP [6–11]. Other authors have reported an increasing rate of bacterial resistance to AAs in patients who had anatomic or functional abnormalities of the US, as well as those patients who were repeatedly hospitalized for UTI [11,12]. Nowadays, various recommendations exist concerning indications for LTAP in comparison to previous guidelines. Some authors do not recommend prophylaxis after a single UTI in infancy [13–15], a surprising position in light of the fact that in the first year of life the frequency of febrile UTI is highest, as well as the susceptibility of permanent parenchymal damage [16]. In cases of prescribed LTAP, there is still no consensus about the duration of treatment. A variety of guidelines have been proposed regarding the age of patients, grade of vesico ureteral reflux, any co-existing anatomic anomalies of urinary tract, the frequency of UTI and size of renal scarring. Furthermore, careful monitoring of each patient is recommended in order to detect UTI as early as possible, as well as treating the patient with the proper antibiotic and changing the antibiotic in the case of a recurrent UTI [3,14]. Although prophylactic use of antibiotics in pediatric nephrology has been commonly accepted and used all over the world, some recent studies question the effectiveness of LTAP in the prevention of UTI and renal scarring, stressing the great need for new well-designed studies, whose results would give new insight in antibiotic use in LTAP [4,6,7,17,18]. The American Academy of Pediatrics (1999) and Matoo (2007) proposed several medications and their doses for LTAP [1,3]. We suspected that some of the proposed medications would have a high percentage of bacterial resistance in our local community; therefore we decided to undertake our own study in order to assess the situation regarding bacterial resistance in University Hospital in Split. We will also give some recommendations regarding the choice of drugs for LTAP in our region. In addition, we investigated the prevalence of uropathogens isolated from urine cultures in children hospitalized with UTI at the Department of Pediatrics during the 7-year study period.
The purpose of this study was to evaluate changes in bacterial resistance patterns among 3 specific patient populations: patients on/off LTAP, patients with multiple/single hospitalization and patients with/without functional or anatomic abnormalities of the urinary system. Finally, we compared our results with those from other studies and deduced our own recommendations for antibiotic use.
Material and methods
We retrospectively reviewed the charts of all 1158 patients hospitalized for UTI at University Hospital in Split between 2000 and 2007.
UTI was confirmed by a positive urine culture of 105 or more colony-forming units of a single organism per milliliter of urine. Isolates were initially recovered on blood agar plates from urine samples. The initial identification of a pure bacterial culture was made by using convential biochemical tests and was confirmed by Vitek 2 systems (bioMerieux, Marc Marcyl’Etoile, France). Routine susceptibility testing to antibiotics was made by disk-diffusion tests, according to CLSI recommendations.
We recorded the patient’s pertinent medical history, including the number of hospitalizations for UTI, possible treatment of LTAP in the last 6 months before hospitalization, the presence of acute or chronic infection, and the presence of any anatomic or functional anomalies of the urinary system such as vesico ureteral reflux, neurogenic bladder, or other anatomic abnormalities. In this study, acute UTI was defined as the patient’s first UTI with no signs of permanent damage of the urinary system. At the same time, chronic UTI was defined as permanent or recurrent UTI with definite damage to the urinary system. Functional anomaly of the urinary system was defined as a change in function of the lower urinary system, resulting in dysfunctional voiding.
Statistical analysis
In the statistical analysis of data we used a χ2 test with P<0.05 as a statistically significant value and Spearman’s correlation test.
Results
From the group of 1158 children with UTI, hospitalized at our Department, 1355 positive urine cultures were isolated.
E. coli was isolated in 917 cases (67.7%), Enterococcus in 164 isolates (12.1%), Klebsiella sp. in 110 isolates (8.1%), Proteus sp. in 67 isolates (4.9%), Pseudomonas sp. in 64 isolates (4.6%), and other bacteria were isolated in the remaining 33 cases (2.3%).
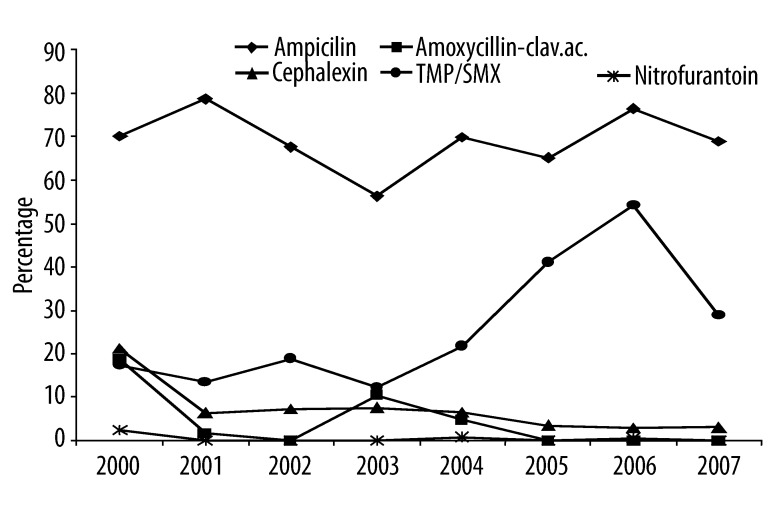
The mean resistance rates of the most prevalent E. coli were as follows: 69.5% to ampicillin, 3.5% to amoxicillin/clavulonic acid, 6.6% to cephalexin, 27.5% to TMP/SMX, and 0.4% to nitrofurantoin. During the study period, follow-up of the trends in resistance rates of E. coli to antimicrobial agents disclosed a statisticaly significant positive trend to TMP/SMX (ρ=0.762; P=0.028), a statisticaly significant negative trend to cephalexin (ρ=−0.786; P=0.021), while no significant trends were detected to ampicillin (ρ=−0.120; P=0.776) and nitrofurantoin (r=−0.192; p=0.648). We also proved 93% probability of a negative trend in the resistance rate of E. coli to amoxicillin/clavulonic acid (r=−0.66; P=0.075) during the study period (Figure 1).
Figure 1.
This figure shows that resistant rates of E. coli to various uroantiseptic drugs were the highest for ampicillin and TMP/SMX. During the period of observance E. coli’s resistance to TMP/SMX had significantly increasing trend, to cephalexin had significantly decreasing trend while to amoxicillin/clavulonic acid had 93% probability to have decreasing trend. Resistance rates of E. coli did not change significantly to ampicillin and to nitrofurantoin during the period of observance. Spearman’s correlation coefficient (ρ) and χ2 (p) were as follows: to ampicillin (ρ=−0.120; p=0.776), to TMP/SMX (ρ=0.762; p=0.028), to cephalexin (ρ=−0.786; p=0.021), amoxicillin/clavulonic acid (ρ=−0.66; p=0.075), and to nitrofurantoin (ρ=−0.192; p=0.648).
The mean resistance rates of all isolated uropathogens to common AAs were the following: 64.3% to ampicillin, 5.8% to amoxicillin/clavulonic acid, 10.5% to cephalexin, 21.3% to TMP/SMX, and 7.9% to nitrofurantoin.
Follow-up of the trends in resistence rates of all uropathogens to antimicrobial agents during the study period disclosed statisticaly significant negative trends to cephalexin (ρ=−0.934; P=0.001) and to amoxicillin/clavulonic acid (ρ=−0.802; P=0.017), while no significant trends were detected to ampicillin (ρ=0.143; P=0.736) and TMP/SMX (ρ=0.419; P=0.301). For nitrofurantoin, we found a 90% probability of a negative trend in resistance rates for all uropathogens during the study period (ρ=−0.618; P=0.102). However, resistance to TMP/SMX increased from 2004 to 2006, but not during the entire study period. Pseudomonas sp. and Enterococcus were not included in these results due to the fact that they have not been tested by all the AAs.
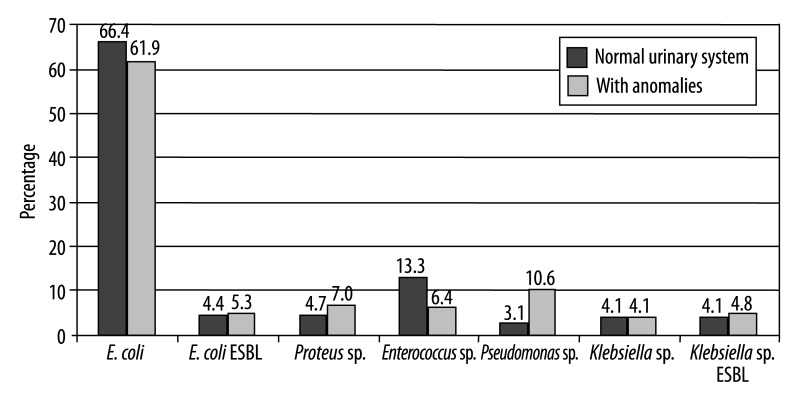
Among the group of 324 children with functional or anatomic abnormalities, there were 27 cases of functional anomalies of the lower urinary system, 47 cases of hydronephrosis, 35 cases of duplex collecting system, 11 cases of urolithiasis, 116 cases of vesico ureteral reflux, and 29 cases of other anatomic anomalies of the urinary system. Fifty-nine patients underwent surgery on the urinary system. Pseudomonas was 3 times more common while Enterococcus was 2 times less common in patients with functional or anatomic anomalies of the urinary system than in patients with normal urinary systems (Figure 2).
Figure 2.
This figure shows significantly higher prevalence of Pseudomonas sp. and significantly lower prevalence of Enterococcus sp. in patients with functional or anatomic anomalies of urinary system.
In the group of children with normal urinary tracts, 113 cases of Enterococcus sp. were found to be resistant to 5 tested AAs (37%), but were susceptible in 196 cases (63%). While in the group of children who had abnormalities of the urinary tract, 20 isolated strains of Enterococcus sp. were found to be resistant to the 5 tested AAs (24%), but were susceptible in 63 cases (76%). This means that the isolated strains of Enterococcus sp. were 1.5 times more resistant to the tested AAs in the group of children who had normal urinary systems than the group of children who had anatomic or functional abnormalities of the urinary system (χ2=4.5; P=0.033).
In the group of patients with a normal urinary system, isolated strains of Klebsiella sp. were resistant to 45 of the tested AAs (29%) and were susceptible to 109 (71%), while in the group of patients who had abnormalities of urinary tract, isolated strains of Klebsiella sp. were resistant to 36 of the tested AAs (40%) and were susceptible to 53 of those AAs (60%). This means that the isolated strains of Klebsiella sp. were 1.4 times more resistant to AAs in patients with anatomical or functional anomalies of urinary system than in those with a normal urinary system (χ2=3.2; P=0.074).
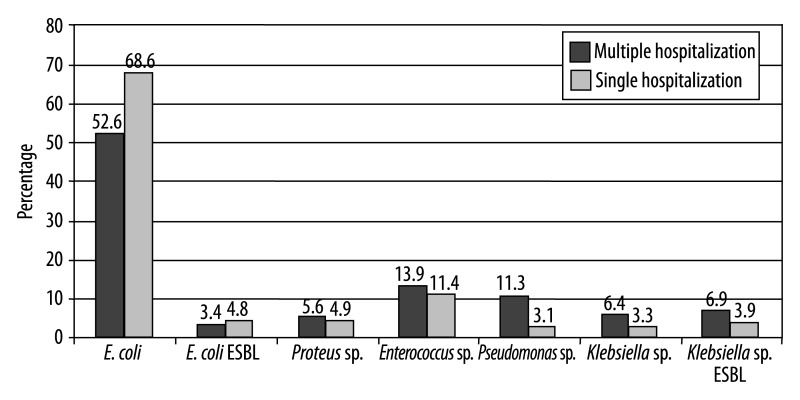
In this study the prevalence of uropathogens in terms of the number of hospitalizations showed that patients hospitalized more than once had a lower chance of having isolated E. coli. However, they had approximately a 3 times greater frequency of UTI caused by Pseudomonas sp. and a 2 times greater frequency of UTI caused by Klebsiella sp. than patients who were hospitalized only once (Figure 3).
Figure 3.
This figure shows significantly higher prevalence of Pseudomonas sp. and Klebsiella sp. in patients who were hospitalized for UTI more than once.
In the group of children who were hospitalized only once, isolated strains of Enterococcus sp. were resistant to 115 of 5 tested AAs (37%) and were susceptible to 193 of those AAs (63%), while in the group of patients who had multiple hospitalizations, the isolated strain of Enterococcus sp. was resistant to 18 of 5 tested AAs (21%) and were susceptible to 66 (79%). This means that isolated strains of Enterococcus sp. were 1.7 times more resistant to AAs in patients who were admitted to the hospital only once than in those who were hospitalized more than once (χ2=7.45; P=0.006).
As opposed to the results obtained in Enterococcus sp., the isolated strains of ESBL-producing Klebsiella sp. in children with multiple hospitalizations were 1.4 times more resistant to antibiotics than the strains isolated in the group of children who were admitted only once. The isolated strains of ESBL-producing Klebsiella sp. in the children upon their first hospitalization were resistant to 107 of the 5 tested AAs (53%) and were susceptible to 95 (47%), while in the group of children with repeated hospitalizations isolated ESBL-producing Klebsiella sp. were resistant to 61 of the 5 tested AAs (68%), and were susceptible to 28 (32%), χ2=6,14, P=0.013.
Out of all the patients who were admitted to the Pediatric Department for an UTI, a group of 175 children received various AAs for LTAP prior to hospitalization at the primary health care level (Table 1).
Table 1.
The distribution of the most frequently used AA for LTAP at the primary health care level among hospitalized patients during the period from 2000 to 2007.
| Medication | Number of patients (%) |
|---|---|
| TMP/SMX | 56 (32) |
| Nitrofurantoin | 34 (19.3) |
| TMP/SMX/nitrofurantoin | 14 (8) |
| Cephuroxime | 31 (17.7) |
| Amoxicillin | 12 (6.7) |
| Cephalexin | 14 (8.0) |
| Amoxicillin-clavulonic acid | 8 (4.5) |
| Other antimicrobial drugs* | 7 (4) |
| Total | 175 (100) |
Other antimicrobial drugs: cephtibuten, cephyxime, ampicillin.
The resistance rates of E. coli to some AAs were significantly different between the groups of children who received LTAP and those who did not receive LTAP. That difference was most significant in the administering of TMP/SMX. We found an approximately 2 times greater resistance rate in patients who received LTAP prior to hospitalization than in those who did not receive LTAP at all. Moreover, resistance to nitrofurantoin in both groups was very low (Table 2). The probability that E. coli would be more resistant in patients who had previously undergone LTAP than in those who did not was proven significant for ampicillin (χ2=3.83; P=0.05), for amoxicillin/clavulonic acid (χ2=4.29; P=0.038) and to TMP/SMX (χ2=23.4; P<0.01).
Table 2.
Comparison of resistance rates of E. coli isolates to AA between the groups of children who received LTAP previously and those who were not treated by LTAP.
| Antibacterial agent | Group: No LTAP (n=801) | Group: LTAP (n=114) |
|---|---|---|
| Resistance rate n (%) | Resistance rate n (%) | |
| Ampicillin | 548 (68.40%) | 89 (78.10%) |
| Amoxycillin-clavulanic ac. | 25 (3.10%) | 8 (7.00%) |
| Cephalexin | 54 (6.70%) | 7 (6.10%) |
| TMP/SMX | 202 (25.20%) | 53 (46.50%) |
| Nitrofurantoin | 3 (0.40%) | 1 (0.90%) |
Discussion
E. coli was generally found to be the most frequent cause of UTI in hospitalized (40–90%), as well as in non-hospitalized (63–78%) children [8–10,12,19–21]. The mean prevalence of isolated E. coli in our study during the observed period (2000–2007) was 67.5%; the highest being in year 2002 (73.7%), but the lowest in year 2007 (60.4%).
As also reported in previous studies that the incidence of E. coli was lower in the cases of multiple hospitalizations, in patients previously treated with LTAP, as well as in cases with coexisting urinary tract anomalies that allowed the increasing growth of some less common uropathogens [8,12].
Incidence of uropathogens in children with urinary tract anomalies and multiple hospitalizations
In our study the incidence of E.coli was slightly less in patients with urinary tract anomalies (61.9%) (Figure 2), as well as in patients with multiple hospitalizations (52.6%) (Figure 3), as opposed to patients with normal urinary tracts and those who were hospitalized only once for UTI.
The incidence of Enterococcus also decreased in patients with urinary tract anomalies. On the contrary, throughout the entire study period, the incidence of Pseudomonas sp. was 3 times greater in children with urinary tract anomalies as well as in those with multiple hospitalizations. In addition, isolated Klebsiella sp. were 2 times more frequent in the group of patients with multiple hospitalizations than in patients hospitalized only once (Figure 3).
Resistance rates of uropathogens to antimicrobial agents
In the American study by Lutter et al. (2005), performed during 1997–2001, the resistance rates of all isolates ranged from 48% to ampicillin, 17% to TMP/SMX and 7% to nitrofurantoin. In Taiwan, Tseng et al. (2008) reported 77.4% resistance to ampicillin, 44.6% to TMP/SMX, 27.2% to cephalotin, and 8.4% to nitrofurantoin, with growing resistance rates to ampicillin, TMP/SMX, and cephalosporins in the first generation during the 14-year study period [8,20].
In accordance with the above-mentioned studies, our results showed a similarly high resistance rate to ampicillin (45–62%), and a growing resistance to TMP/SMX (from 15% in 2000 to 35% in 2006). During the same period, the resistance of all uropathogens to nitrofurantoin remained low, while the resistance of E. coli to nitrofurantoin was even lower (Figure 1). Besides the relatively high resistance rate to ampicillin and TMP/SMX, resistance rates of all isolates, except Pseudomonas sp. and Enterococcus sp., showed a decreasing trend in first-generation cephalosporins (cephalexin) and amoxicilin-clavulonic acid. These changes in resistance could be explained by the extensive consumption of antibiotics, especially azitromicyn and third-generation cephalosporins, which were over the previous years widely prescribed for various indications in our region locally as well as in the entire country [1–3].
Regarding resistance of E. coli, our study showed that the resistance rate to ampicillin was continuously high (a mean of 69.5%), with the highest rate being in year 2001 (78.6%). During the same period of time, resistance rates to amoxicilin-clavulonic acid and cephalexin decreased, similar to the trends observed in all the other isolates. However, the increasing resistance rate of E. coli to TMP/SMX was higher than the resistance to all other isolated uropathogens, first showing increasing trends until year 2004, but later showing a decrease in year 2007 (Figure 1). This increasing resistance rate might be explained by the widespread prescription of TMP/SMX for treatment of UTI and providing LTAP in Croatia. Increasing resistance rates to TMP/SMX was not uncommon in other countries all over the world [1–3]. On the contrary, permanently low resistance rates to nitrofurantoin, with an average value of 0.4%, could be associated with the infrequent prescription of this drug. Our results show a decreasing trend of resistance of E. coli to amoxicillin/clavulonic acid and cephalexin, but a low resistance to nitrofurantoin, in accordance with trends in other parts of Croatia, as reported by the Committee for Monitoring Bacterial Resistance Rates of the Croatian Academy of Medical Sciences [19]. Similar results of antibiotic resistance were reported in Canada and Brazil [11,22].
Permanently high resistance to antibiotics with increasing resistance rates of E. coli to ampicillin and TMP/SMX were shown in studies from the UK, Austria, Spain and Brasil [9,11,12,19 23]. Because of that, some authors concluded that ampicillin, trimetoprim, and TMP/SMX were insufficient for the monotherapy of UTI, as recommended by Wolff et al (2007) [9,24]. Furthermore, Cheng CH et al. (2008) warned that the use of cephalosporins in LTAP could increase the number of UTIs caused by ESBL-producing bacteria or multidrug-resistant uropathogens other than E. coli, therefore they suggested keeping TMP/SMX for use in LTAP [25].
Resistance to antimicrobial therapy in children with abnormalities of the urinary tract
In children with functional or anatomic urinary tract abnormalities, we expected to find more resistant pathogens, presuming that they probably had frequent exacerbations of UTI and received long and frequent antibiotic treatment. Our study fulfilled these expectations partly for Klebsiella sp. (probability of 97% to be more resistant to AAs), while Enterococcus showed that patients had significantly more resistant strains of that uropathogen than if they had normal urinary systems. However, other isolated uropathogens in that group of patients were not significantly more resistant to AAs as compared to patients with normal urinary systems. In contrast to our results, Ladhani and Grandsen (2003) found higher resistance rates of E. coli to ampicillin, amoxicillin/clavulonic acid, nitrofurantoin, and TMP/SMX in the group of patients with underlying renal problems compared to patients with normal urinary systems [12]. A study made by Allen et al. (1999) proved that children with urinary abnormalities had a 2.4 times higher chance of acquiring a UTI caused by E. coli that was resistant to TMP/SMX (11).
Resistance to antimicrobial therapy in repeatedly hospitalized children
Although we expected that some uropathogens from our study would disclose higher resistance rates to AAs in patients who were repeatedly hospitalized for UTI than those hospitalized only once, we confirmed those expectations in ESBL-producing Klebsiella sp. alone. Our results contradicted Allen’s study, claiming that children with 2 or more hospital admissions were 4 times more likely to have a resistant isolate of E.coli than those who had no admissions in the previous year [11]. Moreover, we found that Enterococcus was 1.7 times more resistant to tested AAs in patients who were admitted to the hospital only once.
Resistance to antimicrobial therapy in children receiving LTAP
Our study also showed that resistance rates of E. coli to AAs could be altered if patients had been receiving LTAP for up to 4 weeks within the last 6 months prior to hospitalization. The resistance rates of E. coli to TMP/SMX, ampicillin and amoxicillin/clavulonic acid were significantly higher in the group of children in this study who had received LTAP compared to those who had not. This is in accordance with Allen’s study (1999) showing a 23 times greater chance of getting a UTI caused by E. coli resistant to TMP/SMX. These patients received LTAP prior to hospitalization. Lutter’s study (2005) showed the same result in patients affected by all kinds of uropathogens [8,11]. Contrary to those results, resistance to nitrofurantoin in both groups from our study retained very low levels. Unexpectedly, the resistance rate of E. coli to cephalexin in children who received LTAP was even lower (4.9%) than in children who did not receive LTAP (6.8%). Some studies claimed that LTAP with TMP/SMX and ampicillin was ineffective in the prevention of UTI and kidney damage, as well as its connection to the increased risk of UTIs caused by resistant uropathogens in some categories of patients [6,7,9,10].
The use of low-dose prophylactic antibiotics to prevent recurrent UTI and kidney damage has been the standard care for many children with urinary tract anomalies, especially VUR [4]. In the last few years, some studies have expressed serious doubts concerning the efficiency of LTAP, but without providing convincing evidence against LTAP so far. Therefore, LTAP is still recommended [6,13,14,26] with customarily prescribed TMP/SMX, nitrofurantoin, cephalexin, ampicillin, and amoxicillin [1–3,6]. In our study, approximately 40% of the children received TMP/SMX for LTAP for different causes, alone or with other AAs. This percentage is lower in comparison to some other studies that used TMP/SMX – 61–100% of cases [7,10,12,17]. Apart from TMP/SMX, our patients received nitrofurantoin in 27.3% of cases and cephalosporins in 25% alone or alternating with another AA (Table 1). In comparison to other studies, nitrofurantoin was used in only 0–18%, and cephalosporins in 0–3% of cases receiving LTAP [7,10,12,17].
Conclusions
We believe that, based on our own data regarding resistance patterns of uropathogens in our local community, we should influence primary care doctors by encouraging them to prescribe more effective drugs in order to achieve better effects of LTAP. In cases where LTAP is undoubtedly prescribed, it should be administered according to the resistance patterns on a local level. This is the best way to choose optimal LTAP. Nevertheless, local studies on resistance patterns of uropathogens should be encouraged in the future. We believe that there is still room for conducting efficient LTAP if we change AAs according to the local results of resistant patterns, otherwise we are forced to follow the general recommendations for LTAP, which are not always appropriate and effective in specific local communities [1,2,13]. In that sense, our recommendation is to exclude ampicillin from further LTAP and reconsider the use of TMP/SMX. In addition, we recommend the use of amoxicillin/clavulonic acid and/or cephalexin in the first 3 months of life, and nitrofurantoin after the first year of life, whenever possible. The duration of LTAP is another not yet resolved issue. In conclusion, we are strongly convinced that if doctors at the primary medical care level were encouraged to carry out our recommendations, results of LTAP at the local level would greatly improve.
Footnotes
Source of support: Departmental sources
References
- 1.American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Urinary Tract Infection. The diagnosis, treatment and evaluation of the initial urinary tract infection in febrile infants and young children. Pediatrics. 1999;103:843–52. doi: 10.1542/peds.103.4.843. [DOI] [PubMed] [Google Scholar]
- 2.Šubat-Dežulović M. New guidelines for antibiotic prophylaxis in children with reccurent urinary tract infections. Pediatr Croat. 2008;52(Supl.1):56–59. [Google Scholar]
- 3.Mattoo TK. Medical management of vesicoureteral reflux. Pediatr Nephrol. 2007;22:1113–20. doi: 10.1007/s00467-007-0485-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le Saux N, Pham B, Moher D. Evaluating the benefits of antimicrobial prophylaxis to prevent urinary tract infections in children: a systematic review. CMAJ. 2000;163:523–29. [PMC free article] [PubMed] [Google Scholar]
- 5.Karpman E, Kurzrock EA. Adverse reactions of nitrofurantoin, trimethoprim and sulfamethoxazole in children. J Urol. 2004;172:448–53. doi: 10.1097/01.ju.0000130653.74548.d6. [DOI] [PubMed] [Google Scholar]
- 6.Williams GJ, Wei L, Lee A, Craig JC. Long-term antibiotics for preventing recurrent urinary tract infection in children. Cochrane Database Of Systematic Reviews. 2006;(3):Art. No.: CD001534. doi: 10.1002/14651858.CD001534.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Roussey-Kesler G, Gadjos V, Idres N, et al. Antibiotic prophylaxis for prevention of recurrent urinary tract infection in children with low grade vesicoureteral reflux: results from a prospective randomized study. J Urol. 2008;179(2):674–79. doi: 10.1016/j.juro.2007.09.090. [DOI] [PubMed] [Google Scholar]
- 8.Lutter SA, Currie ML, Mitz LB, Greenbaum LA. Antibiotic resistance pateterns in children hospitalized for urinary tract infections. Arch Pediatr Adolesc Med. 2005;159:924–28. doi: 10.1001/archpedi.159.10.924. [DOI] [PubMed] [Google Scholar]
- 9.Prelog M, Schiefecker D, Fille M, et al. Febrile urinary tract infection in children: ampicilin and trimetoprim insufficient as empirical mono-therapy. Pediatr Nephrol. 2008;23:145–52. doi: 10.1007/s00467-007-0701-1. [DOI] [PubMed] [Google Scholar]
- 10.Conway PH, Cnaan A, Zaoutis T, et al. Recurrent urinary tract infections in children – risk factors and association with prophylactic antimicrobials. JAMA. 2007;298:179–86. doi: 10.1001/jama.298.2.179. [DOI] [PubMed] [Google Scholar]
- 11.Allen UD, MacDonald N, Fuite L, et al. Risk factors for resistance to first-line antimicrobials among urinary tract isolates of Escherichia coli in children. CMAJ. 1999;160:1436–40. [PMC free article] [PubMed] [Google Scholar]
- 12.Ladhani S, Gransden W. Increasing antibiotic resistance among urinary tract isolates. Arch Dis Child. 2003;88:444–45. doi: 10.1136/adc.88.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institute for Health and Clinical Excellence (NICE) Urinary tract infection in children. 2007. http://guidelance.nice.org.uk/CG054. [DOI] [PubMed]
- 14.Montini G, Hewitt I. Urinary tract infections: to prophylaxis or not to prophylayxis? Pediatr Nephrol. 2009;24:1605–9. doi: 10.1007/s00467-009-1213-y. [DOI] [PubMed] [Google Scholar]
- 15.Beetz R. May we go on with antibacterial prophylaxis for urinary tract infections? Pediatr Nephrol. 2006;21:5–13. doi: 10.1007/s00467-005-2083-6. [DOI] [PubMed] [Google Scholar]
- 16.Bensman A, Dunand O, Ulinski T. Urinary tract infection. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N, editors. Pediatric Nephrology. 6th ed. Berlin Heidelberg: Springer-Verlag; 2009. pp. 1299–310. [Google Scholar]
- 17.Pennesi M, Travan L, Peratoner L, et al. Is antibiotic prophylaxis in children with vesicoureteral reflux effective in preventing pyelonephritis and renal scars? A randomized, controlled trial. Pediatrics. 2008;121(6):e1489–94. doi: 10.1542/peds.2007-2652. [DOI] [PubMed] [Google Scholar]
- 18.Montini G, Rigon L, Zucchetta P, et al. IRIS Group. Prophylaxis after first febrile urinary tract infection in children? A multicenter, randomized, controlled, noninferiority trial. Pediatrics. 2008;122(5):1064–71. doi: 10.1542/peds.2007-3770. [DOI] [PubMed] [Google Scholar]
- 19.Guidon EBM, Berezin EN, Nigro S, et al. Antibiotic resistance patterns of pediatric community acquired urinary infections. Braz J Infect Dis. 2008;12(4) doi: 10.1590/S1413-86702008000400013. [DOI] [PubMed] [Google Scholar]
- 20.Tseng MH, Lo WT, Lin WJ, et al. Changing trend in antimicrobial resistance of pediatric uropathogens in Taiwan. Pediatr Int. 2008;50(6):797–800. doi: 10.1111/j.1442-200X.2008.02738.x. [DOI] [PubMed] [Google Scholar]
- 21.Kurtaran B, Candevir A, Tasova Y, et al. Antibiotic resistance in comunity-acquired urinary tract infections: Prevalence and risk factors. Med Sci Monit. 2010;16(5):246–51. [PubMed] [Google Scholar]
- 22.Osjetljivost i rezistencija bakterija na antibiotike u Republici Hrvatskoj 2000,, 2001., 2002., 2003., 2004., 2005. i 2006. god. [Date of access to data: July 2008]. Available on: URL: http://www.amzh.hr/cro/index-cro.htm.
- 23.Eiros Bouza JM, Ochoa Sangrador C. Etiological profile of urinary tract infections and antimicrobial susceptibility of urinary pathogens. An Pediatr. 2007;67(5):461–68. doi: 10.1016/s1695-4033(07)70713-0. [DOI] [PubMed] [Google Scholar]
- 24.Wolff O, MacLennan C. Evidence behind the WHO Guidelines: hospital care for children: what is the appropriate empiric antibiotic therapy in uncomplicated urinary tract infections in children in developing countries? J Trop Pediatr. 2007;53:150–52. doi: 10.1093/tropej/fmm030. [DOI] [PubMed] [Google Scholar]
- 25.Cheng CH, Tsai MH, Huang YC, et al. Antibiotic resistance patterns of community-acqiured urinary tract infections in children with vesicoureteral reflux receiving prophylactic antibiotic therapy. Pediatrics. 2008;122(6):1212–17. doi: 10.1542/peds.2007-2926. [DOI] [PubMed] [Google Scholar]
- 26.Shakil A, Reed L. Do antibiotics prevent recurrent UTI in children with anatomic abnormalities ? Clinical Inquiries. 2004;53:67–72. [PubMed] [Google Scholar]