Summary
Background
One of the complications of total knee arthroplasty (TKA) which has not yet been directly addressed is pseudo-patella baja (PPB). True patella baja (PB) is present when the length of the patellar tendon becomes shorter. PPB is present when the patella tendon is not shortened, but the level of the joint line is elevated. This study was conducted to assess PPB in TKA.
Material/Methods
Sixty patients who had had a primary TKA at our center between 1995 and 2005 were included. The average follow-up was 27.5 months. The Knee Society Scoring (KSS), lateral knee x-rays and the Blackburne-Peel index were used for assessments.
Results
Out of the 60 patients, 43 (72%) demonstrated no joint line elevation or patellar tendon shortening (group A). Fifteen patients (25%) had joint line elevation (group B), and both PB and PPB were present in 2 (3%) patients (group C). KSS was lower in groups B and C compared with group A, but this difference was not statistically significant. The average range of motion (ROM) in group A was significantly higher compared with either group B or C, and patients in groups B and C showed significantly more severe pain compared with group A (P<0.001).
Conclusions
PPB is not an uncommon finding after TKA and is associated with a statistically significant decrease in ROM and an increase in pain. Furthermore, KSS in the PPB group was less than in patients without PPB, although the difference was not statistically meaningful.
Keywords: Patella Baja, Pseudo Patella Baja, total knee arthroplasty, complication
Background
Total knee arthroplasty (TKA) is a rather common operation. Although clearly beneficial to the well-being of the patient, it may cause biomechanical changes in the knee joint and complications in the patellofemoral joint such as stiffness, instability, patellar fracture, rupture of the patellar or the quadriceps tendon and subsequent fibrosis behind the patellar tendon, patellar tendon shortening and the patellar clunk syndrome. One of the relatively infrequently reported problems is the change in the position of the patella and the tibiofemoral joint, which gives rise to 2 distinct complications; patella baja (PB) and pseudo-patella baja (PPB). Patella baja is when the patella is placed too distally relative to the femoral trochlea. True PB is present when the length of the patellar tendon becomes shorter than normal. This may happen as a result of trauma to the tendon, for example during high tibial osteotomy, ACL reconstruction or simply after TKA, distal positioning of the patella relative to the femoral trochlea, or scarring and adhesion of the patellar tendon to the anterior aspect of the tibia as a result of trauma or surgery [1–6].
On the other hand, there is a similar complication, PPB, in which the patella is abnormally positioned and the patellar tendon is of normal length. When the patella tendon is not shortened but the level of the joint line is elevated, PPB is present. This may be caused by a higher than usual femoral cut made during the operation, tibial under-resection (when the prosthetic tibial component is thicker than the section of upper tibia that has been resected) or excessive soft tissue release necessitating elevation of the tibiofemoral joint line to provide stability [2].
Few studies have focused on PB complicating TKA [7–10]. The incidence of patella baja after TKA has been reported as 34%, 37% and 65% in different studies [8,9,11]. This complication may result in decreased extensor mechanism power, anterior knee pain due to patellar impingement on the tibial polyethylene insert, and limitation of knee flexion as a result of tightening of the collateral ligaments of the knee and diminished femoral rollback [7–11].
To the best of our knowledge no study considered pseudo-patella baja and its implications on outcome of TKA. Some studies have revealed the importance of joint line balance in TKA [12,13], but PPB has not yet been directly addressed. PB and PPB each involve differing management; additionally, treatment of the complications first depends on determining the cause and distinguishing between patella baja and pseudo-patella baja. Thus, our study aimed to assess the incidence and outcome of pseudo-patella baja after standard TKA.
Material and Methods
Sixty patients who had had a primary TKA at our center between 1995 and 2005 were invited for the study. All the participants consented to take part in the study; 11 (18.3%) were men and 49 were women (81.7%), and the average age was 65.2 years with a range of 40 to over 70 years. The average follow-up was 27.5 months, with the minimum follow up of 24 months (Table 1). All of the subjects showed 10–15 degrees of flexion contracture of the knees.
Table 1.
Demographics of the TKA patients between 1995 and 2005.
| Number of patients | 60 |
| Male | 11 |
| Female | 49 |
| Age range | 40 to over 70 |
| 40–50 | 2 (3.3%) |
| 50–60 | 11 (18.3%) |
| 60–70 | 32 (50.3%) |
| >70 | 15 (25.0%) |
| Average age | 65.2 |
| Average follow-up | 27.5 months |
In all patients with or without a retained posterior cruciate ligament (PCL), deep dish PCL retaining prosthetic knees (Rotaglide®, Corin Group, UK) were used. The routine procedure was a standard operation with midline skin incision followed by a medial parapatellar arthrotomy and routine patellar eversion without resurfacing.
Patients with patella baja before their arthroplasty and patients with rheumatoid arthritis were excluded from the study. The patients’ knee scores and functional scores, based on the Knee Society Scoring (KSS) system, were recorded. This score takes note of pain, range of motion, stability, malalignment, extension lag, and walking and stair climbing ability [14], with a maximum of 200 for the knee and functional scores. X-rays were taken, including lateral knee projections in 30° of flexion.
In this study we chose to use the Insall Salvati ratio (ISR) for the diagnosis of patella baja. The basic pathology in patella baja is a shortened infra-patellar tendon; therefore, we devised a ratio that takes the length of this tendon into account, enabling us to differentiate between a normally placed patella and one that is inferiorly placed (patella baja). This is the ratio of the patellar tendon length to the length of the patella as judged on the lateral X-ray taken in 30° of flexion (patellar tendon length/patellar length) (Figure 1). ISR <0.8 was defined as PB (the normal ISR is 1±0.2) [2,15].
Figure 1.
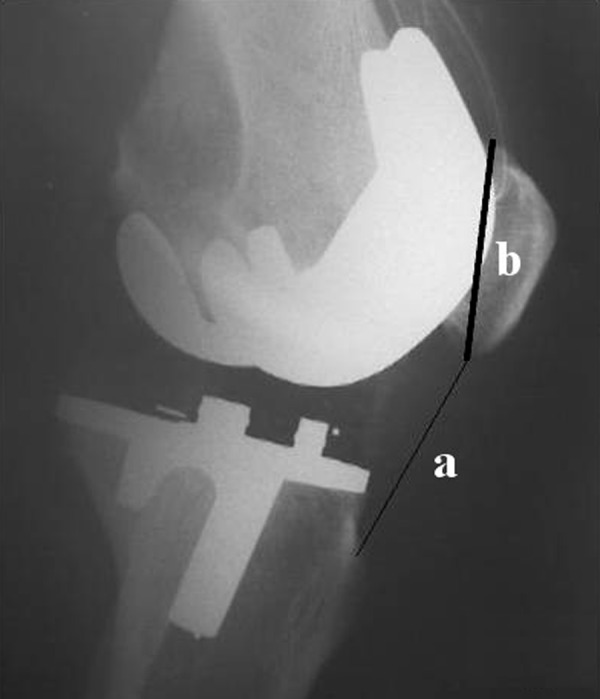
Insall-Salvati index, the ratio of the length of patellar tendon (a) to the longest (diagonal) length of patella (b).
As the length of the patellar tendon is normal in PPB, the use of the Insall Salvati ratio will not be appropriate; instead a different ratio that focuses on the joint line level must be considered. Therefore to look for PPB, we preferred the Blackburne-Peel index (BPI <0.54 defined PPB). The Blackburne-Peel ratio is the ratio of the distance between the inferior border of the patellar articular surface and the tibiofemoral joint line to the length of the patellar articular surface (Figure 2). The ratio becomes smaller as the joint line is raised. As the length of the patellar tendon is normal in PPB, this index, which takes the position of the joint line into account, is more appropriate [16].
Figure 2.
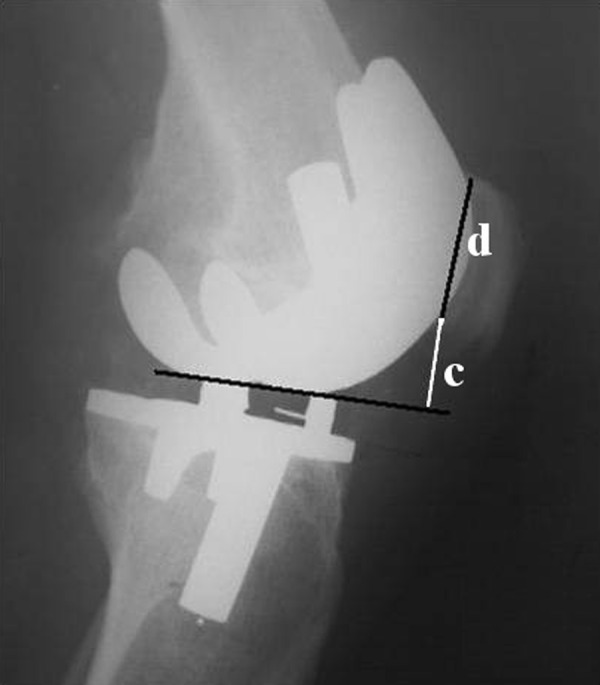
Blackburne-Peel index, the distance from the inferior border of the patellar articular surface to the tibiofemoral joint line (c) divided by the length of patellar articular surface (d).
After collecting all data and making comparisons, the patients were placed into 3 groups: group A patients were without PB or PPB after arthroplasty of the knee, group B patients had only PPB, and group C patients had both PB and PPB/PB.
Statistical analysis was performed with SPSS statistical software (version 15.0; SPSS, Chicago, Illinois). Paired Student t-tests were utilized to compare variables between the 2 study groups. P-value <0.05 was considered significant.
Results
Out of the 60 patients entered into the study, 43 (72%) demonstrated no joint line elevation or patellar tendon shortening (group A); 15 patients (25%) had joint line elevation (group B); and both PB and PPB (PPB/PB) were present in 2 (3%) patients (group C) (Table 2).
Table 2.
Incidence of PB (patella baja) and PPB (pseudo-patella baja) in the three study groups.
| Group | Number |
|---|---|
| A (no PB or PPB) | 43(72%) |
| B (PPB) | 15(25%) |
| C (PB and PPB) | 2(3%) |
The average KSS was 141.2 in group A, and 137.7 and 132 in groups B and C, respectively. Although KSS was lower in patients with PPB and PPB/PB (Table 3), there was no significant relationship between group A and either group B or C. Therefore, we believe PPB/PB did not severely affect the knee score. However, the average range of motion (ROM) in uncomplicated subjects (group A) measured 98.7°, while the average ROM in groups B and C were 90.66° and 92.5°, respectively (Table 3). There was a meaningful relationship between ROM in group A and group B or and C, but in order to prove that PPB or PPB/PB actually reduce the ROM, it is necessary to have case and control groups that are matched for other causes of reduced range of motion. As for the knee pain according to KSS, patients in groups B and C showed significantly more severe pain compared with group A (P value <0.001) (Table 4).
Table 3.
Preoperative and postoperative range of motion and Knee society score in the three groups of patients.
| Group A N=43 |
Group B N=15 |
Group C N=2 |
||||
|---|---|---|---|---|---|---|
| Preop | Postop | Preop | Postop | Preop | Postop | |
| ROM | 96 | 98.7 | 102 | 90.66 | 104 | 92.5 |
| KSS | 91 | 141.2 | 92 | 137.7 | 94 | 132 |
Group A – without patella baja and/or pseudopatella baja; group B – with pseudopatella baja; group C – with pseudo-patella baja and patella baja; Preop – preoperative; Postop – postoperative; ROM – range of motion; KSS – knee society score.
Table 4.
Postoperative pain in three groups of patients based on KSS grading.
| No pain | Mild occasional | Mild stairs only | Mild walking & stairs | Moderate | Severe | Total | |
|---|---|---|---|---|---|---|---|
| Group A | 4 (9.3%) | 13 (30.2%) | 9 (21%) | 11 (25.5%) | 6 (14%) | 43 | |
| Group B | 1 (6.6%) | 1 (6.6%) | 5 (33.4%) | 4 (26.7%) | 4 (26.7%) | 15 | |
| Group C | 1 | 1 | 2 |
Discussion
Our results showed that in the 60 patients who underwent TKA, PPB and PPB/PB developed in 25% and 28% of the patients, respectively, and it had adversely affected some outcomes of the surgery. Occurrence of this complication was associated with a statistically significant decrease in the range of motion and an increase in pain. KSS in the PPB group was less than in patients without PPB, although the difference was not statistically meaningful.
According to our results, PPB and PPB/PB were associated with pain, decreased range of motion and a statistically insignificant decrease in KSS. Thus, it can be concluded that in addition to shortening of the patellar tendon, which can reduce knee function and increase knee pain following TKA, a change in the position of the joint line of the prosthetic knee in the absence of patellar tendon shortening can lead to diminution of the functional results.
It has been shown in several studies that patella baja can affect the patello-femoral joint mechanics and may result in diminished postoperative range of motion and anterior knee pain, and also cause impingement and wear of the polyethylene tibial insert, which are all undesirable outcomes [2,3,7–9,11,16–18], but pseudo-patella baja and its undesirable consequences have not yet been elucidated. In addition, since the causes and treatments of PB and PPB (and probably their impacts on the patient) are different, it is important to differentiate between PB and PPB [16].
Regarding the lack of data on PPB in TKA, our study was planned to investigate the occurrence of this common but often neglected complication associated with TKA.
In PPB, the problem lies in the fact that during the operation the joint line has been set higher than normal. Thus intra-operative awareness of patellar tracking, including knowledge of the joint line level, is of paramount importance if PPB is to be avoided [19,20]. PPB may be the result of excessive soft tissue release, a higher than normal femoral cut, or a larger insert thickness. The surgeon often looks only for extension flexion gaps, and once it has been determined that the gaps are equal in size, proceeds with the rest of the operation, thus it is recommended that the femoral cut be made carefully in order to avoid an inadvertent elevation of the joint line.
Thornton-Bott et al. demonstrated in 2006 that TKA surgery creates a pseudo-patella baja. PPB was introduced into 26.7% of their patients. They found that the incidence of pseudo patella baja increases with the extent of soft tissue release and with increase in insert thickness. They mentioned that TKA undergoing extensive soft-tissue release increases the risk of PPB by 100%. Their multi-center study included 266 patients with a normal patella position, and recorded the patients’ soft tissue release extent and tibial insert size. To investigate the effect of extensive soft-tissue releases, they split the patients into 3 groups: minimal releases, moderate releases, and extensive releases. In the minimal and moderate release groups 21% to 22% of patients were found to have pseudo-patella baja. In contrast, 47% of the extensive release group patients had PPB. Patients were further split into 3 groups to determine the effect of insert thickness on PPB. Small inserts were approximately 8 mm, medium inserts were between 10 mm to 12 mm, and large inserts were from 15 mm to 22 mm. They identified that about 25% of patients in the small and medium insert groups had developed a PPB, while 45% to 46% of the large insert group patients had a PPB, and they found no association between a PPB incidence and clinical outcome. They anticipate that those patients with PPB, however, may also develop true patella baja, as previously reported following TKA, and concluded that both true and pseudo-patella baja can cause patella pain and pathology [21].
In another 2006 study, Schwab et al retrospectively studied the results of reconstruction with use of a rotating-hinge endoprosthesis following excision of a distal femoral tumor in 43 patients who were followed clinically and radiographically for a minimum of 48 months; patella baja occurred in 9 of their patients. They concluded that Patella baja is a relatively common complication in endoprosthetic reconstruction, and has a negative impact on knee function. They also indicated that the position of the joint line deserves special attention in a distal femoral replacement. It is desirable to reconstitute the normal position of the joint line in order to maintain optimal patellofemoral biomechanics [22].
In summary, the incidence of the pseudo-patella baja may be reduced by the following: timely surgery, careful preoperative radiographic evaluation, conservative treatment of gonarthrosis, a stepwise algorithmic approach for flexion contracture correction, closely checking the patellar tracking, placing the joint line of the reconstruction as closely as possible to the natural joint line, and consistent early and prolonged rehabilitation with appropriate analgesia.
This issue requires further research to investigate the long-term effects of PPB and PPB/PB on the outcome of TKA.
Conclusions
Pseudo patella baja is not an uncommon finding after TKA, and is mainly due to technical problems in cutting the distal femur or excessive soft tissue release. By careful preoperative planning and not more than adequate soft tissue release or bone cutting, this complication can be avoided. Given the incidence and adverse effects of PPB in TKA, care must be taken to maintain the reconstructed joint line as close as possible to its natural position, which in turn may improve results of TKA and patients’ pain, range of motion, level of function and knee score.
Footnotes
Authors’ disclosure statement
The authors report no actual or potential conflict of interest in relation to this article.
Source of support: Departmental sources
References
- 1.Sharma V, Tsailas PG, Maheshwari AV, et al. Does patellar eversion in total knee arthroplasty cause patella baja? Clin Orthop Relat Res. 2008;466(11):2763–68. doi: 10.1007/s11999-008-0347-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chonko DJ, Lombardi AV, Jr, Berend KR. Patella baja and total knee arthroplasty (TKA): etiology, diagnosis, and management. Surg Technol Int. 2004;12:231–38. [PubMed] [Google Scholar]
- 3.Blackburne JS, Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59(2):241–42. doi: 10.1302/0301-620X.59B2.873986. [DOI] [PubMed] [Google Scholar]
- 4.Blumensaat C. Die lageabweichungen und verren-kungen der kniescheibe. Ergeb Chir Orthop. 1938;31:149–223. [Google Scholar]
- 5.Caton J, Deschamps G, Chambat P, et al. Patella infera. Apropos of 128 cases. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317–25. [PubMed] [Google Scholar]
- 6.Grelsamer RP, Meadows S. The modified Insall Salvati ratio for assessment of patellar height. Clin Orthop Relat Res. 1992;(282):170–76. [PubMed] [Google Scholar]
- 7.Cameron HU, Jung YB. Patella baja complicating total knee arthroplasty. A report of two cases. J Arthroplasty. 1988;3(2):177–80. [PubMed] [Google Scholar]
- 8.Koshino T, Ejima M, Okamoto R, et al. Gradual low riding of the patella during postoperative course after total knee arthroplasty in osteoarthritis and rheumatoid arthritis. J Arthroplasty. 1990;5(4):323–27. doi: 10.1016/s0883-5403(08)80091-5. [DOI] [PubMed] [Google Scholar]
- 9.Weale AE, Murray DW, Newman JH, et al. The length of the patellar tendon after unicompartmental and total knee replacement. J Bone Joint Surg Br. 1999;81(5):790–95. doi: 10.1302/0301-620x.81b5.9590. [DOI] [PubMed] [Google Scholar]
- 10.Gatha NM, Clarke HD, Fuchs R, et al. Factors affecting postoperative range of motion after total knee arthroplasty. J Knee Surg. 2004;17(4):196–202. doi: 10.1055/s-0030-1248221. [DOI] [PubMed] [Google Scholar]
- 11.Flören M, Davis J, Peterson MG, Laskin RS. A mini-midvastus capsular approach with patellar displacement decreases the prevalence of patella baja. J Arthroplasty. 2007;22(6 Suppl 2):51–57. doi: 10.1016/j.arth.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Yang JH, Seo JG, Moon YW, Kim MH. Joint line changes after navigation-assisted mobile-bearing TKA. Orthopedics. 2009;32(10 Suppl):35–39. doi: 10.3928/01477447-20090915-57. [DOI] [PubMed] [Google Scholar]
- 13.Figgie HE, Goldberg VM, Heiple KG, et al. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am. 1986;68(7):1035–40. [PubMed] [Google Scholar]
- 14.Insall JN, Dorr LD, Scott RD, et al. Rational of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;(248):13–14. [PubMed] [Google Scholar]
- 15.Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–4. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 16.Grelsamer RP. Patella baja after total knee arthroplasty: is it really patella baja? J Arthroplasty. 2002;17(1):66–69. doi: 10.1054/arth.2002.28728. [DOI] [PubMed] [Google Scholar]
- 17.Grelsamer RP. Patellar malalignment. J Bone Joint Surg Am. 2000;82-A(11):1639–50. [PubMed] [Google Scholar]
- 18.Yoshii I, Whiteside LA, White SE, et al. Influence of prosthetic joint line position on knee kinematics and patellar position. J Arthroplasty. 1991;6(2):169–77. doi: 10.1016/s0883-5403(11)80013-6. [DOI] [PubMed] [Google Scholar]
- 19.Noyes FR, Wojtys EM, Marshall MT. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop. 1991;(265):241–52. [PubMed] [Google Scholar]
- 20.Noyes FR, Wojtys EM. The early recognition, diagnosis and treatment of the patella infera syndrome. Instr Course Lect. 1991;40:233–47. [Google Scholar]
- 21.Thornton-Bott PJ, Unitt L, Johnstone DJ, et al. Pseudo-patella baja following soft tissue balancing in total knee arthroplasty. Presented at the British Orthopaedic Association Annual Congress; Sept. 20–23, 2005; Birmingham, England. [Google Scholar]
- 22.Schwab JH, Agarwal P, Boland PJ, et al. Patellar complications following distal femoral replacement after bone tumor resection. J Bone Joint Surg Am. 2006;88(10):2225–30. doi: 10.2106/JBJS.E.01279. [DOI] [PubMed] [Google Scholar]


