Summary
Background
The goal of this prognostic study was to investigate whether the duration of untreated psychosis (DUP) may have a prognostic value with regard to the further course of the illness.
Material/Methods
Fifty-eight patients (77% of the original study group) diagnosed with DSM III schizophrenia and later re-diagnosed with DSM IV T-R were assessed at 4 time points. Number of relapses, average time of inpatient treatment, number of inpatient readmissions, and severity of psychopathological symptoms were assessed at 1-, 3-, 7- and 12-year follow-ups. DUP information was obtained by clinical interview with patients and their families. The severity of symptoms was assessed using BPRS-SA, UCLA version.
Results
Increases in the number of relapses at follow-ups were more prominent in the group with a longer DUP (p<0.001). Decreases in the results of BPRS (symptom improvement) were more prominent in patients with a shorter DUP. The latter had significantly lower results than patients with a long DUP at each assessment except the index hospitalization (p equalled, respectively: 0.449; 0.002; 0.012; 0.034 and 0.014). Decreases in positive symptoms were greater in patients with a short DUP – significant at all except the 7-year follow-up (p equalled respectively: 0.230; <0.001; 0.011; 0.214; <0.001).
Conclusions
1) A positive correlation was found between DUP and the dynamics of general and positive symptoms and the number of relapses. 2) There was no significant relationship between DUP and the dynamics of negative symptoms, whereas the relationship between the time and number of re-hospitalizations was marginally significant.
Keywords: schizophrenia, course of illness, duration of untreated psychosis
Background
The duration of untreated psychosis is most frequently defined as the period between the occurrence of first positive symptoms and the commencement of treatment [1]. Some patients experience negative symptoms that are manifested in disordered behaviour for many years prior to the first symptoms of anxiety and depression, and subsequently, sometimes after several years, positive symptoms due to which they are diagnosed as psychotic. The variety of non-specific criteria for the onset of schizophrenia, discussed by authors including Häfner, such as negative symptoms and behaviour deficits, impaired thinking and concentration, anergia, psychomotor poverty, withdrawal, academic and employment problems, as well as the presence of proximal and distal prodromal symptoms, make it difficult to formulate an early diagnosis and to provide early treatment [2]. The criterion for the diagnosis of schizophrenia is the occurrence of positive symptoms. The beginning of treatment is usually considered to be the moment when adequate antipsychotic drugs are administered [3]. Demographic studies from various countries indicate that the duration of untreated psychosis ranges from 22 weeks to over 150 weeks, while the median is between 4 and 26 weeks [4–7].
The skewed distribution of the results obtained is the reason for the application of different statistical methods and the divergences in descriptions of the duration period as relatively long or short. Based on a review of studies, McGlashan defines the period as “short” when it does not exceed 6 months and “long” when it lasts more than 6 months [5].
In recent years various studies have been devoted to the search for universal predictors of the course of schizophrenia [8]. Risk factors and protective factors have been described in reference to both the clinical and social dimensions, and among the clinical factors, the duration of untreated psychosis (DUP) has been particularly focused on. One of the major goals of early intervention programs has been to identify patients with first-episode psychosis as soon as possible. These programmes were based on research outcomes, which often indicated that a longer duration of untreated psychosis predicts a more severe course of the illness [1–19].
The meta-analysis prepared by Perkins et al. in 2005 [10] demonstrates that a shorter duration of developing psychosis that is not subject to therapeutic intervention is followed by a more stable and fuller remission of general, positive and negative symptoms, a reduced number of relapses, and better general functioning (GAF, GAS). In 2004 Perkins et al. showed that shorter DUP, independently from premorbid functioning, can predict better clinical response [20]. Other studies (e.g., those by Johannessen et al or Kalla et al.) [11,12], focus particularly on the correlation between the DUP and social functioning. Patients with a longer DUP were less frequently employed, were single (mainly men), had poorer professional qualifications for finding a job, a weaker social network, and generally coped less well in their social lives. Peralta et al found that diffused premorbid social support and low socio-economic status seem to be relevant to prolonged DUP [21].
Some studies, however, report null findings as to the correlation between the DUP and treatment outcome. The fact that no correlation was detected may partly stem from the temporal criteria differences in defining the onset of the illness, the occurrence of psychosis and the beginning of treatment, while various follow-up periods were investigated [3,13,22].
Objectives of the study
Research commenced during the patient’s first psychiatric admission, and the follow-up periods were 1, 3, 7 and 12 years after the index hospitalisation. This study was part of the Cracovian Prospective Study on the Course of Schizophrenia, which was conducted in real time, meaning that it relies on long-term observation of patients with schizophrenia, starting with the first episode and continuing throughout all years of living with the illness, and involving assessment of treatment outcomes and the efficiency of psychosocial intervention, as well as the role of prognostic factors. The purpose of this study was to determine whether the dynamics of long-term treatment outcomes in the 12-year follow-up (1997–2000) in patients suffering from schizophrenia are dependent on the duration of untreated psychosis (DUP). The indicators of treatment outcomes were: number of relapses, duration and number of inpatient readmissions, and intensity of psychopathological symptoms at subsequent follow-up assessments.
Study group
From among 80 patients with schizophrenia and diagnosed according to DSM III, which diagnosis was later confirmed with DSM IV – TR [22], the analysis included 58 patients who were assessed at all the aforementioned follow-up points, that is, 77% of the original study group. At the onset of the illness, the average age was 27.32 years (OS=6.20; range 18 to 44). Table 1 presents the prognostic demographic, social and illness-related factors that characterised the study group at the first psychiatric admission.
Table 1.
Characteristics of the study group at first admission, n=58.
| Number | Percentage | ||
|---|---|---|---|
| Demographic factors | |||
| Gender | Women | 34 | 59.0 |
| Men | 24 | 41.0 | |
| Marital status | Married | 20 | 34.0 |
| Single | 38 | 66.0 | |
| Education | Tertiary | 16 | 27.59 |
| Unfinished tertiary | 5 | 8.62 | |
| Secondary | 24 | 41.38 | |
| Vocational | 11 | 18.97 | |
| Primary | 2 | 3.45 | |
| Familial factors | |||
| Expressed emotions level | High | 42 | 72.41 |
| Low | 16 | 27.59 | |
| Social factors | |||
| Social functioning acc. to DSM III | Very good | 11 | 18.97 |
| Good | 15 | 25.86 | |
| Satisfactory | 18 | 31.03 | |
| Poor | 11 | 18.97 | |
| Very poor | 3 | 5.17 | |
| Employment | Full-time job (or study) | 37 | 63.79 |
| Sick leave (or dean’s leave from university) | 13 | 22.41 | |
| Part-time job | 1 | 1.72 | |
| No job | 7 | 12.07 | |
| Sexual adjustment before illness | No relationship | 29 | 50.00 |
| Unstable relationships | 9 | 15.52 | |
| Stable relationship | 20 | 34.48 | |
| Social contacts before illness | At least one deep, satisfying relationship outside the family | 9 | 15.52 |
| Many superficial relationships | 22 | 37.93 | |
| One superficial relationship | 11 | 18.97 | |
| Unsatisfactory or frustrating relationships | 10 | 17.24 | |
| No contacts outside the family | 6 | 10.34 | |
| Factors relating to illness | |||
| Onset of illness | Acute | 40 | 68.97 |
| Chronic | 18 | 31.03 | |
| Duration of untreated psychosis (DUP) | Up to 6 months | 37 | 63.79 |
| Over 6 months | 21 | 36.21 |
Material and Methods
The prodromal demographic and social factors were assessed with the use of a modified version of the Carpenter-Strauss prognostic scale. To evaluate expressed emotions, the semi-structured Camberwell Family Interview (CFI) was applied. Intensity of symptoms was measured with the UCLA-modified BPRS-LA scale. The follow-up data were gathered at subsequent intervals (1, 3, 7, and 12 years after the first psychiatric admission) with the use of the Alanen and Räkköläinen follow-up interview [15,19]. The analysis embraced the following independent variables:
– Duration of untreated psychosis (DUP) at 2 levels: up to 6 months, and over 6 months (2-level intragroup factor);
– Time of measurement – a repeated measure factor, with 3, 4, or 5 levels, depending on the indicator of treatment outcome.
The following indicators of treatment outcome (ie, dependent variables) were selected:
– Number of relapses (assessment at 1-, 3-, 7- and 12-year follow-ups);
– Number of readmissions (assessment at 3-, 7- and 12-year follow-ups);
– Duration of readmissions (assessment at 3-, 7- and 12-year follow-ups);
– Intensity of symptoms measured using the BPRS.LA Scale: global psychopathology, positive syndrome and negative syndrome (assessment at index hospitalization and discharge at the first admission and subsequent follow-up points: 1, 3, 7 and 12 years after the first admission).
The independent variables formed a 2-factor research plan with 1 between-group factor (DUP) and 1 repeated measurement factor. The research plan took the form 2×3 in the case of number and duration of readmissions; 2×4 in the case of number of relapses; and 2×5 in the case of BPRS).
Analysis of variance (ANOVA) was used to analyze the results. The main effects of the dynamics and interactions between the factor of repeated measurement and the DUP were calculated. Whenever significant correlations were obtained, simple effects were calculated as well. The objective of the interaction analysis was to find out if the dynamic of change in 1 parameter is dependent on the DUP. In other words, the question under investigation was whether this dynamic is different for patients with a long DUP vs. patients with a short DUP. The significance of differences between the groups with long and short DUP at subsequent follow-up points was evaluated by means of simple effects analysis.
Results
The first series of analyses assessed the dynamics of numbers of relapses, numbers of readmissions, duration of readmissions and intensity of symptoms assessed using the BPRS, as well as the interaction between this dynamic and the DUP. The analysis of variance results are presented in Table 2.
Table 2.
Analysis of variance for dynamics of number of relapses and number and duration of readmissions for the entire study group and subgroups with short and long DUP.
| Analysed effect | Number of relapses | Number of readmissions | Duration of readmissions | |||
|---|---|---|---|---|---|---|
| F | p | F | p | F | p | |
| Change of treatment outcomes in course of illnessa) | 35.06 | <0.001* | 16.12 | <0.001* | 15.82 | <0.001* |
| Interaction between DUP and treatment outcomes in course of illnessa) | 2.87 | 0.038* | 2.48 | 0.089 | 3.05 | 0.051* |
Change was assessed based on the measurements at 1st, 7th and 12th follow-ups.
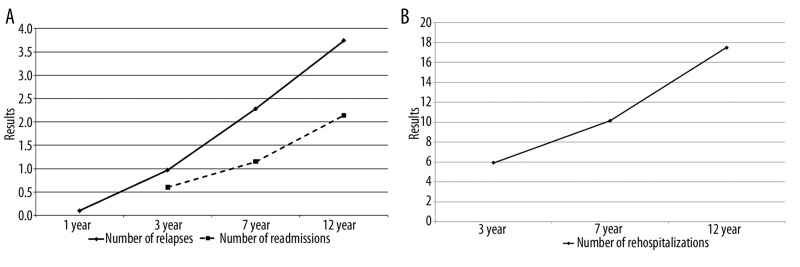
The analysis of variance showed that for all 3 dependent variables (number of relapses, number of readmissions, and duration of readmissions), the dynamic was statistically significant. At subsequent follow-up points, the results were higher for all the variables. This effect is illustrated by Figures 1A and B.
Figure 1.
(A) Dynamics of relapses and readmissions. (B) Dynamic of the duration of readmissions.
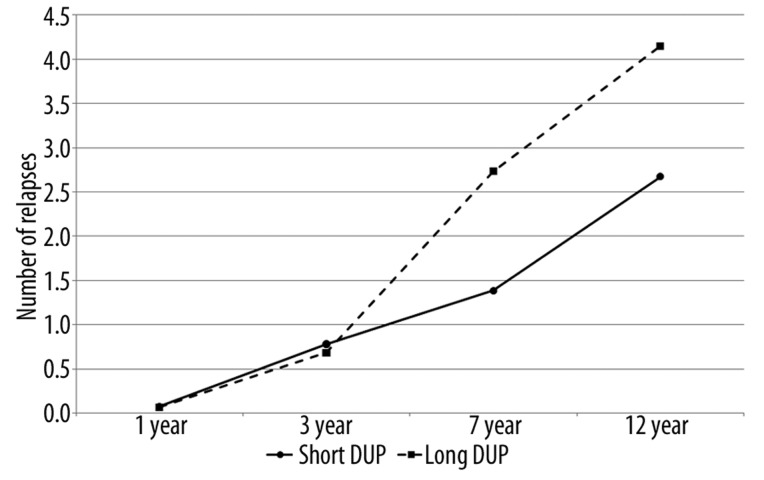
The dynamics of the number of relapses was not identical in the groups with long and short DUP (p<0.001). The increase in the number of relapses at subsequent follow-up points was higher in the group with the long DUP (Figure 2).
Figure 2.
Dynamics of increasing number of relapses for short and long DUP.
The analyses of simple effects demonstrated that the groups with long and short DUP did not differ significantly (with p equalling 0.937 and 0.794, respectively) at 1-year and 3-year follow-up. The difference became significant at the 7-year follow-up (p=0.036), but not at the 12-year follow-up (p=0.154). It may be assumed that the reason for this was the relatively high standard error at this point of measurement.
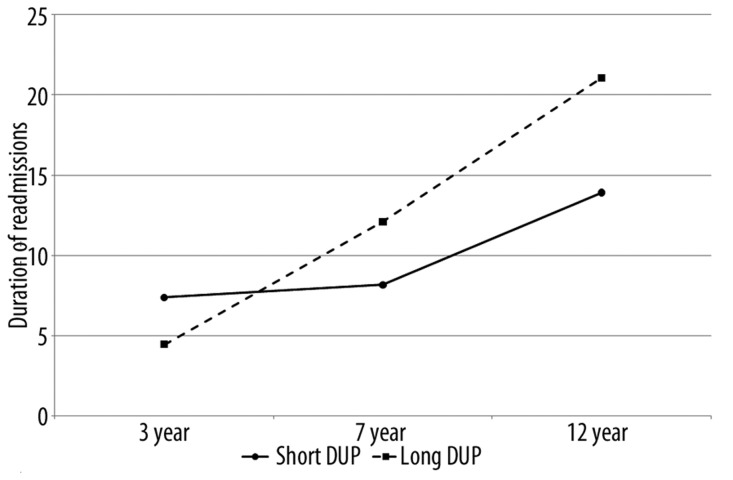
A marginally significant interaction was observed concerning duration of readmissions, between its dynamic and the DUP (p=0.051). This is shown in Figure 3.
Figure 3.
Dynamics of duration of readmissions for short and long DUP.
Interpretation of this interaction is complicated by the fact that no simple effects related to the comparison of the groups with short and long DUP at particular follow-up points provided any statistically significant findings (p amounted to: 0.43, 0.41 and 0.31, respectively). It may thus be conservatively stated that the dynamics of duration of readmissions seem to be stronger (increase more sharply) in the group with the longer DUP.
The second set of analyses addressed the BPRS-LA scale. It included 5 measurement points: index hospitalization, discharge, and 3-, 7- and 12-year follow-ups. As before, the dynamics of change at particular points were first investigated overall, and then in relation to the short and long DUP. The results of the analysis of variance (ANOVA) in relation to the dynamics of the general BPRS assessment and the interaction with DUP are presented in Table 3.
Table 3.
Analysis of variance for the dynamics of BPRS for the entire study group and subgroups with short and long DUP.
| Analysed effect | Global BPRS | Positive symptoms | Negative symptoms | |||
|---|---|---|---|---|---|---|
| F | P | F | P | F | p | |
| Change of treatment outcomes in course of illnessa) | 83.76 | <0.001* | 90.68 | <0.001* | 14.31 | <0.001* |
| Interaction between DUP and treatment outcomes in course of illnessa) | 2.78 | 0.028* | 4.89 | 0.001* | 0.27 | 0.896 |
Change was assessed based on the measurements at year 3, 7 and 12.
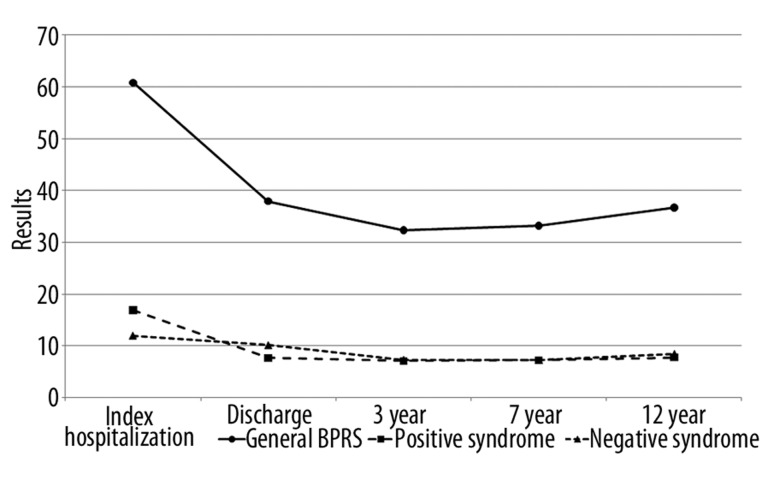
The results shown in Table 3 show that the dynamic was statistically significant for all the 3 indices of the BPRS. Figure 4 shows that all parameters decreased with time. The most noticeable decrease of the investigated parameters occurred between index hospitalization and discharge. Subsequently, between discharge and the 12-year follow-up, the changes were slight. This observation, however, refers to the analysis that does not take into account the impact of the DUP.
Figure 4.
Dynamics of global psychopathology, positive and negative syndrome in BPRS.
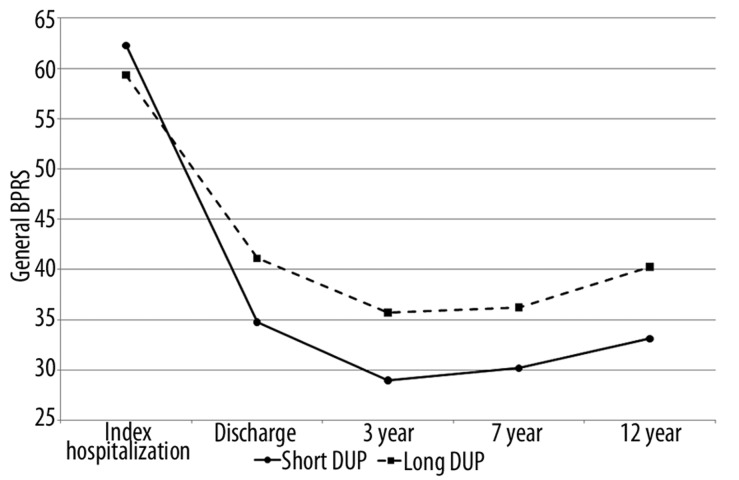
When that impact was considered, a number of interesting interactions emerged. Overall BPRS results were lower (i.e., improvement was noticed in symptomatology) in the patients characterised by short DUP (Figure 5). Between index hospitalization and discharge, those patients had better treatment outcomes than the patients with long DUP. Moreover, the outcomes were stable over time and better at the 3-, 7- and 12-year follow-ups. The effect proved statistically significant – the analysis of simple effects showed that patients with short DUP had significantly lower results than the patients with long DUP at each measurement point except for the first in-patient hospitalisation (ps: 0.449, 0.002, 0.012, 0.034 and 0.014, respectively).
Figure 5.
Dynamics of changing general BPRS for short and long DUP.
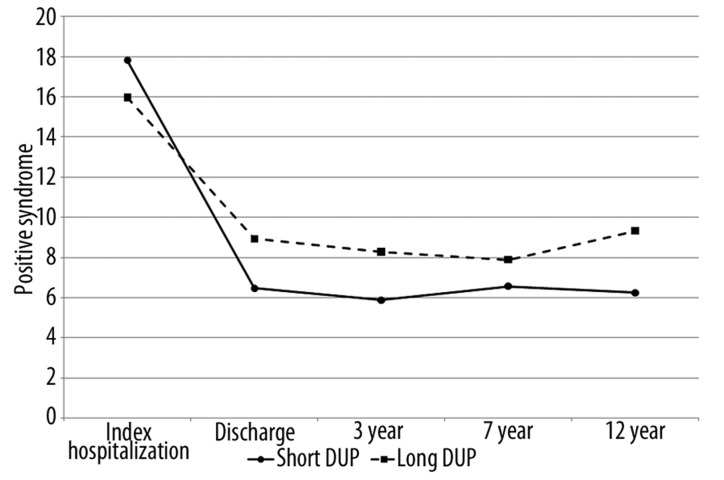
The results for the positive syndrome were similar to those for general psychopathology. The reduction of positive symptoms was greater in patients with short DPU (Figure 6).
Figure 6.
Dynamics of changing positive syndrome in BPRS for short and long DUP.
In contrast with the overall PBRS result, at the 7-year follow-up the difference between the 2 groups was not statistically significant (p for all the simple effects measuring the differences between the group at particular follow-up points was 0.230; <0.001, 0.011; 0.214; < 0.001, respectively).
Discussion
Our findings confirm the predictive value of the DUP for the course of schizophrenia, as measured by number of relapses, duration of readmissions, and severity of general and positive symptoms.
One noteworthy finding is the long-term improvement in positive symptoms, assessed by means of the BPRS scale. This improvement was more noticeable in patients characterised by a short duration of untreated psychosis. The symptom improvement was long-lasting, not only between intake and discharge from the ward, but also at all the follow-up points (3-, 7- and 12-year). Bottlender et al. obtained similar results for a 15-year follow-up period – longer DUP involved more intense negative and positive symptoms and general psychopathology, as well as more impaired functioning overall [14]. Assessment over shorter follow-up periods yielded comparable findings. Barnes et al., with a 1-year follow-up period, corroborated the correlation between the longer DUP and severity of positive and negative symptoms and social functioning. Moreover, this finding did not depend on the age of the patients, the severity of their symptoms or their level of social functioning at the beginning of treatment. The correlation with the negative syndrome, which was not present in the Cracovian study, should probably be ascribed to the shortness of the follow-up period when this syndrome is noticeably dynamic [16]. Similarly, Schimmelmann, in his study of 636 patients, incorporating an 18-month follow-up period, found that longer DUP was connected with weaker remission of positive symptoms, a more serious course of schizophrenia, and poorer general functioning both before the onset of the illness and later [17]. The comprehensive meta-analysis by Perkins et al., evaluating 43 publications devoted to the DUP, demonstrated that the findings indicate that a shorter duration of untreated psychosis was connected with symptom improvement in terms of measured general psychopathology, positive and negative symptoms, and functioning [10].
Our study did not produce any results to confirm a correlation between DUP and the dynamics of the negative syndrome. Likewise, studies published worldwide do not report a correlation between the DUP and neuro-cognitive functions or changes in the morphology of the brain [10,24]; yet the negative syndrome is frequently correlated with these variables [18]. The absence of such correlations suggests that the DUP is a more modifiable factor of the illness. Moreover, relapses are regarded as dependent not only on the developing illness but also on environmental factors [19]. The risk of relapse after the first psychotic episode is very high – according to Perkins, as many as 90% of patients experience a relapse during the years immediately following the first episode [10]. In our study, the increment of the number of relapses at subsequent follow-up points was higher in patients who had a long DUP. Nevertheless, the correlation between the number of relapses and the longer DUP proved to be statistically significant only at the 7-year follow-up point (K7). The ambiguous result in relation to the 12-year period may correspond with the divergences encountered by other researchers. De Haan et al discovered a statistically significant correlation between DUP and the risk of relapse, which was confirmed by an assessment after 2 years [25]. Wiersma et al., investigating a 15-year period, as well as Robinson et al., did not encounter any correlations between the duration of untreated psychosis and relapses [13,23].
Despite the lack of statistically significant correlations between DUP and the number and duration of readmissions, a higher increment in number and duration of readmissions can be observed in patients who had a longer DUP. The literature on the subject relates longer duration of untreated psychosis to a variously defined more severe course of schizophrenia [10]. Both relapses and number and duration of readmissions can be considered indicators of this severity. All these indicators are connected with other factors, both biological and environmental, which complicates research on the “pure” impact of the DUP, and requires an extremely critical approach. At the same time, any attempts to control the described variables may bring up ethical considerations.
This article focuses on clinical findings. Internationally, a great deal of research has proven a correlation between DUP and social factors, such as prodromal functioning, employment, social network, and dependence on familial relations, especially the intensity of expressed criticism [11,12,26]. The observed interactions could be more thoroughly understood if a broad spectrum of such factors was examined.
Conclusions
A positive correlation was found between the duration of untreated psychosis and the dynamics of general and positive symptoms and the number of relapses.
There was no significant relationship between the duration of untreated psychosis and the dynamics of negative symptoms, whereas the relationship between the time and number of re-hospitalizations was marginally significant.
A replication of some, and lack of confirmation of other, long-term results leads us to conclude that there is still a need for further studies on the duration of untreated psychosis.
Footnotes
Source of support: Departmental sources
References
- 1.Häfner H, editor. Risk and Protective Factors in Schizophrenia. Steinkopff Verlag; Darmstadt: 2002. [Google Scholar]
- 2.Crow TJ, MacMillan JF, Johnson AL, Johnstone EC. A randomised controlled trial of prophylactic neuroleptic treatment. Br J Psychiatry. 1986;148:120–27. doi: 10.1192/bjp.148.2.120. [DOI] [PubMed] [Google Scholar]
- 3.Klosterkoetter J. Predicting the onset of schizophrenia. In: Häfner H, editor. Risk and Protective Factors in Schizophrenia. Steinkopff Verlag; Darmstadt: 2002. pp. 193–207. [Google Scholar]
- 4.Häfner H. Onset and early course as determinant of the further course of schizophrenia. Acta Psychiatr Scand. 2000;102(Suppl 407):44–48. [PubMed] [Google Scholar]
- 5.Fariis S, Larsen TK, Melle I, et al. Methodological pitfalls in early detection studies – the NAPE Lecture 2002. Acta Psychiatr Scand. 2003;107:3–9. doi: 10.1034/j.1600-0447.2003.02600.x. [DOI] [PubMed] [Google Scholar]
- 6.Wunderink A, Nienhujs NJ, Sytema S, Wiersma D. Treatment delay and response rate in first episode psychosis. Acta Psychiatr Scand. 2006;113:332–39. doi: 10.1111/j.1600-0447.2005.00685.x. [DOI] [PubMed] [Google Scholar]
- 7.McGlashan TH. Duration of untreated psychosis in first episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999;46:899–907. doi: 10.1016/s0006-3223(99)00084-0. [DOI] [PubMed] [Google Scholar]
- 8.Norman RM, Malla AK. Duration of untreated psychosis: a critical examination of the concept and its importance. Psychol Med. 2001;31:381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- 9.Norman RM, Malla AK, Verdi MB. Understanding delay in treatment for first episode psychosis. Psychol Med. 2004;34:255–66. doi: 10.1017/s0033291703001119. [DOI] [PubMed] [Google Scholar]
- 10.Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162(10):1785–804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 11.Johannessen JO, Larsen TK, McGlashan T. Duration of untreated psychosis: An important target for intervention in schizophrenia. Nord J Psychiatry. 1999;53(4):275–83. [Google Scholar]
- 12.Kalla O, Aaltonen J, Wahlstrom J, et al. Duration of untreated psychosis and its correlates in first-episode psychosis in Finland and Spain. Acta Psychiatr Scand. 2002;106:265–75. doi: 10.1034/j.1600-0447.2002.02302.x. [DOI] [PubMed] [Google Scholar]
- 13.Wiersma D, Nienhuis FJ, Sloff CJ, Giel R. Natural course of schizophrenic disorders: a 15-year follow-up of a Dutch incidence cohort. Schizophr Bull. 1998;24:75–85. doi: 10.1093/oxfordjournals.schbul.a033315. [DOI] [PubMed] [Google Scholar]
- 14.Bottlender R, Sato T, Jager M, et al. The impact of the duration of untreated psychosis prior to first psychiatric admission on the 15-year outcome in schizophrenia. Schizophr Res. 2003;62:37–44. doi: 10.1016/s0920-9964(02)00348-1. [DOI] [PubMed] [Google Scholar]
- 15.Alanen YO, Räkköläinen V, Rasimus R, et al. Psychotherapeutically oriented treatment of schizophrenia: Results of 5-year follow-up. Acta Psychiatrica Scandinavica. 1985;71(319):31–49. doi: 10.1111/j.1600-0447.1985.tb08522.x. [DOI] [PubMed] [Google Scholar]
- 16.Barnes TRE, Leeson VC, Mutsatsa SH, et al. Duration of untreated psychosis and social function: 1-year follow-up study of first-episode schizophrenia. Br J Psychiatry. 2008;193:2003–9. doi: 10.1192/bjp.bp.108.049718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schimmelmann BG, Huber ChG, Lambert M, et al. Impact of duration of untreated psychosis on pre-treatment, baseline, and outcome characteristics in an epidemiological first-episode psychosis cohort. J Psychiatr Res. 2008;42:982–90. doi: 10.1016/j.jpsychires.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 18.Mosiołek A, Łoza B. Co mierzą testy neurokognitywne w schizofrenii? Via Medica. 2004;1(2):113–19. [in Polish] [Google Scholar]
- 19.Cechnicki A. Prospektywne badania przebiegu schizofrenii – nawrót i rehospitalizacja jako kryterium wyników leczenia. Postępy Psychiatrii i Neurologii. 1997;5(Suppl 2):7–15. [in Polish] [Google Scholar]
- 20.Perkins D, Liebermann JA, Gu H, et al. Predictors of antipsychotic treatment response in patients with firs-episode schizophrenia, schizoaffective and schizophreniform disorders. Br J Psychiatry. 2004;185:18–24. doi: 10.1192/bjp.185.1.18. [DOI] [PubMed] [Google Scholar]
- 21.Peralta V, Cuesta M, Martinez-Larrea JA, et al. Duration of untreated psychotic illness. The role of premorbid social support networks. Soc Psychiatry, Psychiatry Epidemiol. 2005;40:345–49. doi: 10.1007/s00127-005-0905-2. [DOI] [PubMed] [Google Scholar]
- 22.Wciórka J, editor. Wyd: Amerykańskie Towarzystwo Psychiatryczne. Arlington VA: Wrocław; 2008. Kryteria diagnostyczne według DSM IV-TR. Qick reference to the diagnostic criteria from DSM IV-TR Polish edition Elsevier Urban&Partner. [Google Scholar]
- 23.Robinson D, Werner MG, Alvir JM, et al. Predictors relapse following response from a first episode of schizophrenia or schizoaffective disorder. Arch Gen Psychiatry. 1999;56:241–47. doi: 10.1001/archpsyc.56.3.241. [DOI] [PubMed] [Google Scholar]
- 24.Galińska B, Szulc A, Tarasow E, et al. Duration of untreated psychosisi and proton magnetic resonance spectroscopy (1H-MRS) findings in first episode schizophrenia. Med Sci Monit. 2009;15(2):CR82–88. [PubMed] [Google Scholar]
- 25.De Haan L, Linszen DH, Lenior MEI, et al. Duration of untreated psychosis and outcome of schizophrenia: Delay in intensive psychosocial treatment versus delay in treatment with antipsychotic medication. Schizophr Bull. 2003;29:341–49. doi: 10.1093/oxfordjournals.schbul.a007009. [DOI] [PubMed] [Google Scholar]
- 26.Compton MT, Chien VH, Leiner AS, et al. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Soc Psychiatry Psychiatr Epidemiol. 2008;43:975–82. doi: 10.1007/s00127-008-0397-y. [DOI] [PubMed] [Google Scholar]