Summary
Temporomandibular joint ankylosis is defined as bony or fibrous adhesion of the anatomic joint components accompanied by a limitation in opening the mouth, causing difficulties with mastication, speaking and oral hygiene as well as inadvertently influencing mandibular growth. Surgical treatment procedures include arthroplasty of the joint cavity with or without a reconstruction and a coronoidectomy, an autogenous costochondral rib graft, distraction osteogenesis and intensive mouth-opening exercise, corrective orthognathic surgery or alloplastic joint prostheses. The authors of this study would like to provide the reader with an evidence-based review of the literature in order to determine the most efficient way to manage TMJ ankylosis and re-ankylosis. The authors have concluded that in order to achieve a satisfactory and durable effective treatment, an individualized approach is necessary in each case.
Keywords: craniofacial deformity, mandibular deficiency, mandibular hypomobility, surgical treatment
Background
The temporomandibular joint (TMJ), from a functional point of view, is one of the most important joints in the human body. It consists of a condylar process of the mandible, temporal fossa, articular disc and joint capsule. The term “ankylosis” is of Greek origin (from the Greek word αγκυλος meaning: bent or crooked) and corresponds to a “stiff joint”, since it leads to a partial or total loss of mobility of the TMJ. The surgical treatment of TMJ ankylosis constitutes a set of highly controversial subjects.
Thus the aim of this study was to find a scientific background for the management of temporomandibular ankylosis.
Material and Methods
A literature search using Medline (1961–2010) and Science Direct (1990–2010) was made using the following terms: ankylosis, temporomandibular joint. The inclusion criteria for the review consisted of: controlled clinical trials, retrospective studies, case reports, and follow-up studies. Moreover, a citation search was conducted in reference lists of all papers included, resulting in the additional inclusion of 3 pioneer studies.
Results
Medline searching yielded 183 English language articles and Science Direct yielded 35 English language articles. The number of articles referring to humans was 165 in Medline and 30 in Science Direct. Finally, the number of studies included was 48. All findings from the following papers have been sorted according to the following subjects: classifications, etiology and occurrence, symptoms and complications, and treatment procedures of the temporomandibular joint ankylosis.
Classification
True temporomandibular joint ankylosis affects the joint, whereas false TMJ ankylosis is an extra-articular type [1]. According to the type of tissue growing in the intracapsular structures of the joint, ankylosis is classified as fibrous, bony or mixed [2,3].
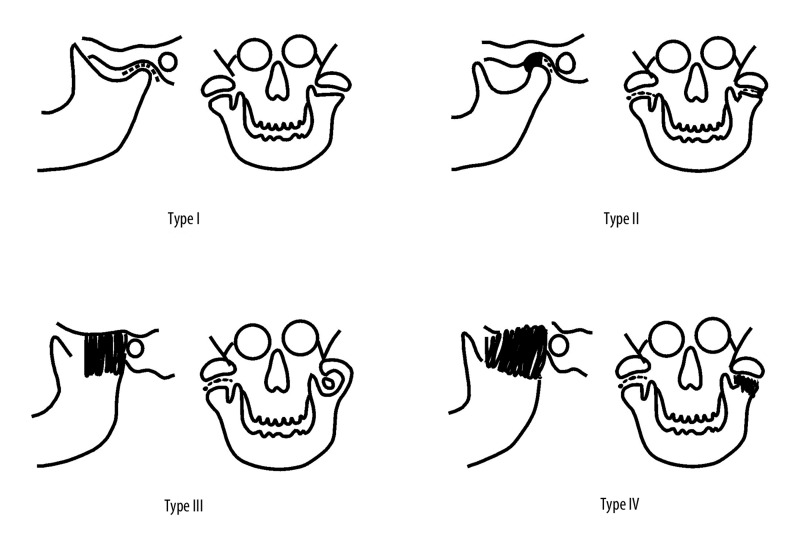
Taking into account the degree of TMJ mobility limitation, Sawhney [4] divided TMJ ankylosis into 4 types:
Type I: The head of the condylar process is visible but significantly deformed, with the fibroadhesions making TMJ movement impossible;
Type II: Consolidation of the deformed head of the condylar process and articular surface occurs mostly at the edges and in the anterior and posterior parts of the structures, and the medial part of the surface of the condylar head remain undamaged;
Type III: The ankylotic mass involves the mandibular ramus and zygomatic arch; an atrophic and displaced fragment of the anterior part of the condylar head is in a medial location;
Type IV: TMJ is completely obliterated by bony ankylotic mass growing between the mandibular ramus and cranial base (Figure 1).
Figure 1.
TMJ ankylosis classification by Sawhney.
Taking into account heterotopic bone formation within the ankylotic mass, temporomandibular ankylosis was classified by Turlington and Durr [5] into 4 grades:
Grade 0: No bone islands visible;
Grade 1: Islands of bone visible within the soft tissue around the joint;
Grade 2: Periarticular bone formation;
Grade 3: Apparent bony ankylosis.
Grades 1, 2 and 3 are further classified as symptomatic (S) and asymptomatic (A). The symptomatic ossification includes: severe pain, decreased interincisal opening (15 mm or less), closed locking of the jaw, or decreased lateral or protrusive movement.
Etiology and Occurrence
The most common causes of ankylosis include trauma and local or systemic infections. The incidence of infectious ankylosis has recently decreased due to antibiotic therapy. Perinatal trauma from forceps is considered as a historical cause as well. Children are susceptible to a post-traumatic ankylosis. The underlying factors include: damage to the temporomandibular disc, age less than 10 years, and prolonged immobilization of the mandible after an intracapsular trauma [1]. Other etiological factors are: myositis ossificans, osteochondroma, rheumatoid arthritis, ankylosing spondylitis (Bechterew Disease), psoriatic arthritis [6], systemic lupus erythematosus, radiotherapy [7,8] or surgical treatment of TMJ [9]. TMJ ankylosis has also been described as a complication after orthognathic surgery [10].
The pathogenesis of ectopic bone formation is unknown. Pluripotential mesenchymal cells are stimulated to differentiate into osteoblastic and chondroblastic stem cells in an unknown mechanism of stimulation, with the bone matrix as the most likely agent [5].
TMJ ankylosis may occur during development or after completion of growth. Thus, 4 groups of affected patients may be distinguished [7]:
growing patients without dentofacial deformities;
growing patients with dentofacial deformities;
adults without dentofacial deformities;
adults with dentofacial deformities.
Each of these 4 groups requires an individual treatment protocol owing to its specific character and different clinical manifestations.
Symptoms and Complications
TMJ ankylosis developed in childhood is one of the most difficult and complex health problems. It leads to mandibular deformity and growth impairment, hinders oral feeding (mastication and swallowing of food) and speaking, and results in poor oral hygiene causing dental caries and periodontal disease. Deformed alveolar processes negatively affect the eruption and position of teeth. The facial profile of the affected patient is often described as “bird profile”. The lower face is considerably shortened, the deficient mandible is visibly retruded and lacks the chin, the cervical mental angle is obtuse and the nasolabial angle is larger than normal. The face is asymmetric with the chin significantly deviated to the affected side. Lip incompetence is observed, with the lower lip trapped under the maxillary front teeth. As the child grows, the face becomes more and more asymmetrical owing to a limited mobility of the mandible, impaired growth and abnormal function of the muscles. A prolonged ankylosis leads to muscle atrophy. Secondary elongation and hypertrophy of the coronoid process subsequently results in limited mandibular mobility [1–3]
Apart from causing physical changes in appearance, the condition has a severe negative effect on the psychosocial performance of juvenile patients and their tutors. Inability to enjoy eating as other people do, lack of willingness to play with their peers or participate in sports activities impair the quality of a young person’s life. Worsened aesthetics of their appearance frequently becomes a reason for depressive disorders.
Treatment of the Temporomandibular Joint Ankylosis
The first steps in developing methods of surgical treatment of TMJ affected by ankylosis were taken in 1851. From 1850 to 1860, condylectomy and arthroplasty of the newly-created joint cavity were performed using a myofascial flap [11]. To the present day, all modalities of this surgical procedure have been applied.
The surgical treatment procedures include:
arthroplasty of the joint cavity;
arthroplasty and a free costochondral graft [12];
arthroplasty with temporalis myofascial flap insertion in the newly created joint cavity accompanied by a simultaneous unilateral coronoidectomy on the affected side or a bilateral coronoidectomy;
distraction of the ramus and body of the mandible on the affected side;
reconstruction of the joint using an alloplastic prosthesis [13,14];
arthroscopic laser-assisted preparation of the articular surfaces [15];
bilateral arthrotomy.
A necessary complement of the surgical treatment is physiotherapy (intensive mouth-opening exercise).
According to current knowledge, surgical treatment should not be postponed. Based on the Moss functional matrix theory, the surgery and function restoration of both the bones and neighbouring soft tissues release the growth potential of the mandible and prevent further development of the deformity [17,18].
Autogenous bone grafts
In many medical centres, various non-vascularised free autogenous bone grafts from the tibial or clavicular bone, sternoclavicular joint, iliac crest, metatarsal bone or metatarsophalangeal articulation are used [1,19]. In some centres, TMJ reconstruction was also performed using autogenous vascular grafts harvested from rib, iliac crest or tibial bones [20–23]. Another solution is to postpone surgery until growth completion. Further steps include joint reconstruction with another autogenous graft, and orthognathic surgery improving the facial appearance and occlusion.
Distraction osteogenesis
Distraction osteogenesis constitutes another reconstruction method applied to the TMJ structures damaged by ankylosis. A reverse L-osteotomy is made, creating a transport segment, which is advanced through the defect. New bone is created in the distraction gap and the leading edge of the transported bone fragment becomes enveloped by a fibrocartilaginous cap, thus reconstructing a neo-condyle and a pseudo-disc. The transport segment is advanced superiorly 0.5 mm twice a day until contact with the glenoid fossa is achieved. Further advancement provides a correction of the vertical deficiency of the mandibular ramus [24]. The long-term results are good provided intensive postoperative physiotherapy is carried out. A negative aspect of the distraction osteogenesis is the amount of bone left after the removal of affected tissues, limiting the possibility of creating a segment for the transporting distraction osteogenesis [25,26].
Alloplastic replacement of the temporomandibular joint
Another solution applied in order to reconstruct the TMJ is the use of alloplastic joint replacement, which thus far has been applied primarily in adult patients. Owing to the fact that the prosthesis is a mechanical device and not biological, it improves the quality of life, but its durability is unknown. Moreover, it has not been considered an attractive treatment method for growing patients until now. While performing the implantation of a TMJ replacement, it has to be noted that it requires alloplasty of all articular structures (both the mandibular condyle and the glenoid fossa). Based on clinical experience, priority is given to total joint replacement with a prosthesis protecting the glenoid fossa against damage resulting from the excessive impact of the “condyle” of the prosthesis [13,27–30].
Replacement of the joint with an alloplastic prosthesis in children as growing patients needs to be given careful consideration. According to Bisla et al. [31], the possibility of improving the joint function and quality of family and social life and – most importantly – the quality of life of the juvenile patient constitutes a reason for applying alloplastic prosthesis of TMJ. Following their own clinical experience, Mercuri et al. [14] specified the following circumstances in which this approach should be considered:
severe inflammation of TMJ involving damage of its structures and lack of response to other treatment methods;
recurrent fibrous or bony ankylosis not responsive to the modalities of treatment which have been hitherto applied;
failed (bone and soft) tissue grafts;
loss of vertical mandibular height and occlusal relationship due to bone resorption, trauma, developmental abnormalities or pathological lesions.
The surgery of total replacement of TMJ by a prosthesis in a growing patient is not an easy procedure and should be carried out only in the most serious cases [32]. It cannot be performed in very small children, its application being restricted only to older non-adult patients.
Current levels of technological development, the constant introduction of innovative solutions in the field of materials and technology, detailed imaging such as computed 3D tomography and the preparation of stereolithographic models has allowed the construction of an individual prosthesis for each patient thanks to the application of CAD/CAM [33,34].
Whenever an alloplastic prosthesis is used, the following issues should be taken into account: scarring of tissues surrounding the TMJ as a reaction to the presence of a foreign body, loss of attachment of the lateral pterygoid muscle, compromising mobility of the joint, and loss of the mechanical properties of the prosthesis.
Discussion
The planning and performance (with high precision) of the first surgery on a pediatric patient are extremely important. Mistakes and complications at this stage may result in scarring and reankylosis, considerably deteriorating the local tissue condition and increasing the risk and complication rate of any subsequent operations.
According to a classic approach, autogenous tissues should be used in the treatment of developmental and functional disorders accompanying TMJ ankylosis in children. An autogenous costochondral rib graft is considered by some authors to be a “gold standard” for temporomandibular joint reconstructions in growing patients [4,35]. However, some recent studies have questioned the necessity for using a cartilaginous graft to restore or maintain mandibular growth [23,36]. Saeed and Kent [37] carried out retrospective examinations of 76 costochondral rib grafts in 57 patients. In consequence, they came to the conclusion that in the cases where no previous surgery of TMJ had been performed (due to the osteoarthroses or innate deformities), the reconstructions involving a free costochondral graft were successful.
Theoretically, autogenous grafts should grow together with the patient. In practice, however, post-surgical performance of grafts involves undesirable phenomena such as resorption, unpredictable overgrowth, secondary asymmetry and even reankylosis [38,39]. Peltomäki et al. [40] presented a hypothesis that a significant overgrowth of a costochondral graft used in reconstruction of TMJ may be caused by an excess of the cartilaginous tissue in the transplant. The cartilaginous cap of the graft thicker than 1 to 2 mm transfers too much of the rib growth centre which is located in the costochondral junction [12]. In consequence, the graft becomes overgrown and micromotion occurs at the junction of the cartilage and bone during normal mandibular movements. This may result in a tumour-like overgrowth and deformity of the graft [6,41]. Based on research reports [36,42] and clinical observations, the appropriate preparation and immobilization of the costochondral graft with the residual ramus of the mandible are considered critical. The intermaxillary fixation following reconstruction with a costochondral graft is maintained for approximately 10 days and then aggressive mouth-opening exercising begins. It is stated that prolonged postponing surgery is a mistake because it results in a gradual deterioration of the condition. Three-year-old children are able to cooperate well during the post-operative rehabilitation. Aggressive physiotherapy should be continued for approximately 1 year following the operation [41]. Early surgery also improves the psychosocial development of a child through the restoration of a normal facial appearance, the ability to enjoy eating, maintain oral hygiene and obtaining regular dental treatment.
In adults however, reconstruction with a free costochondral rib graft may be applied only in a limited number of cases due to the histomorphology of the rib of the fully grown patient. The rib is primarily composed of cortical bone, with only a small amount of cancellous bone. The capability of the graft to become incorporated into the host bone depends mostly on the local soft tissue at the donor site, as well as its ability to revascularize and take over the necessary functions. Vascularity of the recipient site becomes compromised due to the scar tissue resulting from preceding surgical procedures. Capillary vessels are able to penetrate the tissue to a depth of 180–220 μm, while the thickness of the scar tissue surrounding the bones which had already been submitted to surgery is 440 μm. This fact has to be taken into account while planning another reconstruction surgery with a free bone graft [43].
The advantage of distraction osteogenesis over other treatment methods means it is possible to initiate physiotherapy on the day following surgery, and there is no need to harvest bone from a donor site for the graft. This is extremely important in juvenile patients because it does not impose restrictions on their normal activity and involves no risk of a complication at the donor site (such as wound infection or oedema in the case of a rib graft). Another advantage is the simultaneous gradual soft tissue adaptation during distraction. It is also of importance that the amount and direction of bone lengthening is quite predictable, since the callus distraction may be controlled. A disadvantage of this is the fact that the distraction device has to remain in place for the period of distraction and subsequent bone healing. The high cost of the distraction device is also of importance.
Where the treatment was focused on reankylosis-induced symptoms, bone grafts lead to a high percentage of complications, which suggests that they should be applied only after serious consideration. Failure of first surgery aimed at reconstruction of TMJ and restoration of its mobility constitutes a serious problem. It leads to a complete growth disturbance and also frequently to reankylosis, requiring additional surgery involving preparation of the articular surfaces and application of another graft. In a case where the first operation of ankylosis and reconstruction of TMJ structures by means of a free costochondral graft proved to be a failure, using the same treatment method seems to be rather myopic [8].
A treatment by means of alloplasty should be considered in the cases of serious anatomical and functional disorders of TMJ, failure of the previous therapy carried out using a free bone graft, recurrent ankylosis, or unpredictable overgrowth [44], Although a patient-fitted individual CAD/CAM alloplastic joint reconstruction seems very expensive, its overall long-term cost is often equal to or less than that of autogenous TMJ reconstruction [13,44,45].
Failure to provide the patient with postoperative physiotherapy may lead to loss of the positive effect of surgical treatment [46,47]. Postoperative physiotherapy allows for the restoration of normal mandibular movements, activates growth of the bone (the Moss’ theory), restores physiological tonus of the masseter muscles, and frequently prevents need for further surgery.
Ankylosis of TMJ occurring in childhood, even if treated in a proper and complication-free manner, almost always requires revision surgeries to be performed in the future in order to improve symmetry and prevent growth disorders. After surgical treatment of ankylosis, all affected patients should be provided with orthodontic care. Proper orthodontic therapy prevents secondary deformities of the alveolar processes, corrects the position of teeth and prepares the patient for further orthognathic treatment.
Conclusions
Until now no single standard treatment protocol for temporomandibular joint ankylosis has been reported. The failure rate (determined as reankylosis) still remains high. If a limited incisal opening, chin deviation or facial deformities are also considered to be failures, the percentage is even higher.
Each method of TMJ reconstruction requires aggressive excision of the fibrous and bony pathological tissue causing ankylosis.
Irrespective of the surgical treatment applied, intensive physiotherapy is a matter of the highest importance. In spite of the generally accepted principles of surgical treatment of TMJ ankylosis, an individualized approach is a necessary condition for obtaining a satisfying and durable treatment effect.
Footnotes
Source of support: Self financing
References
- 1.Kazanijan VH. Ankylosis of the temporomandibular joint. Surg Gyncol Obstet. 1938;67:333–48. [Google Scholar]
- 2.Akama MK, Guthua S, Chindia ML, Kahuho SK. Management of Bilateral Temporomandibular Joint Ankylosis in Children: Case Report. East African Medical J. 2009;86(1):45–48. doi: 10.4314/eamj.v86i1.46930. [DOI] [PubMed] [Google Scholar]
- 3.Motta A, Louro RS, Medeiros PJ, Capelli J. Orthodontic and surgical treatment of a patient with an ankylosed temporomandibular joint. Am J Orthod Dentofacial Orthop. 2007;131:785–96. doi: 10.1016/j.ajodo.2005.11.036. [DOI] [PubMed] [Google Scholar]
- 4.Sawhney CP. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986;77:29–38. [PubMed] [Google Scholar]
- 5.Durr ED, Turlington EG, Foote RL. Radiation treatment of heterotopic bone formation in the temporomandibular joint articulation. Int J Radiat Oncol Biol Phys. 1993;27:863–69. doi: 10.1016/0360-3016(93)90461-4. [DOI] [PubMed] [Google Scholar]
- 6.Zhi K, Ren W, Zhou H, Gao L, et al. Management of Temporomandibular Joint Ankylosis: 11year’s clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:687–92. doi: 10.1016/j.tripleo.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 7.Gundlach KK. Ankylosis of the Temporomandibular joint. J Cranio-Maxillo-Fac Surg. 2010;38:122–30. doi: 10.1016/j.jcms.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Kaban LB, Bouchard C, Troulis MJ. A Protocolfor Management of Temporomandibular Joint Ankylosis in Children. J Oral Maxillofac Surg. 2009;67:1966–78. doi: 10.1016/j.joms.2009.03.071. [DOI] [PubMed] [Google Scholar]
- 9.Loveless TP, Bjornland T, Dodson TB, Keith DA. Efficacy of Temporomandibular Joint Ankylosis Surgical Treatment. J Oral Maxillofac Surg. 2010;68:1276–82. doi: 10.1016/j.joms.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Wright GW, Heggie AC. Bilateral temporomandibular joint ankylosis after bimaxillary surgery. J Oral Maxillofac Surg. 1998;56:1437–41. doi: 10.1016/s0278-2391(98)90411-6. [DOI] [PubMed] [Google Scholar]
- 11.Humphry GM. Excision of condyle of lower jaw. Assoc Med J. 1856;4:61–62. doi: 10.1136/bmj.s3-4.160.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medra AMM. Follow up of Mandibular Costochondral Grafts after Release of Ankylosis of the TMJ. Br J Oral Maxillofac Surg. 2005;43:118–22. doi: 10.1016/j.bjoms.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Mercuri LG. Alloplastic vs. Autogenous Temporomandibular Joint Reconstruction. In: Indresano AT, Haug RH, editors. Oral and Maxillofacial Surgery Clinics of North America. 3. Vol. 18. Elsevier; Philadelphia: 2006. pp. 399–411. [DOI] [PubMed] [Google Scholar]
- 14.Mercuri LG, Alcheikh Ali F, Woolson R. Outcomes of Total Alloplastic Replacement with Peri-articular Autogenous Fat Grafting for Management of Re-ankylosis of the Temporomandibular Joint. J Oral Maxillofac Surg. 2008;66:1794–803. doi: 10.1016/j.joms.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 15.Moses JJ, Lee J, Arredondo A. Arthroscopic laser debridement of the temporomandibular joint fibrous and bony ankylosis: case report. J Oral Maxillofac Surg. 1999;56:1104–6. doi: 10.1016/s0278-2391(98)90266-x. [DOI] [PubMed] [Google Scholar]
- 16.Reid RR, Cooce H. Postoperative ionizing radiation in the management of heterotopic bone formation in the temporomandibular joint. J Oral Maxillofac Surg. 1999;57:900–5. doi: 10.1016/s0278-2391(99)90003-4. [DOI] [PubMed] [Google Scholar]
- 17.Moss ML, Rankow RM. The role of the functional matrix in mandibular growth. Angle Orthod. 1968;38:95–103. doi: 10.1043/0003-3219(1968)038<0095:TROTFM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.El-Mofty S. Cephalometric studies of patients with ankylosis of the temporomandibular joint following surgical treatment. Oral Surg. 1979;48:92–96. doi: 10.1016/0030-4220(79)90244-5. [DOI] [PubMed] [Google Scholar]
- 19.Mercuri LG, Swift JQ. Considerations for the Use of Alloplastic Temporomandibular Joint Replacement in the Growing Patient. J Oral Maxillofac Surg. 2009;67:1979–90. doi: 10.1016/j.joms.2009.05.430. [DOI] [PubMed] [Google Scholar]
- 20.Guelnick PJ, Sinsel NK. The “Eve” procedure: The transfer of vascularized seventh rib, fascia, cartilage and serratus muscle to reconstruct different defects. Plast Reconstr Surg. 1996;97:527–35. doi: 10.1097/00006534-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Taylor GI. Reconstruction of the mandible with free composite iliac crest bone graft. Ann Plast Surg. 1982;9:361–76. doi: 10.1097/00000637-198211000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Wax MK, Winslow CP, Hansen J, et al. A retrospective analysis of temporomandibular joint reconstruction with free fibula microvascular flap. Laryngoscope. 2000;110:977–81. doi: 10.1097/00005537-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Matukas VJ, Szymela VF, Schmidt JF. Surgical treatment of bony ankylosis in a child using a composite cartilage – bone iliac crest graft. J Oral Surg. 1980;38:903–5. [PubMed] [Google Scholar]
- 24.Stucki-McCornick S, Winick R, Winick A. Distraction osteogenesis for the reconstruction of the temporomandibular joint. NYSDJ. 1998;41:36–41. [PubMed] [Google Scholar]
- 25.Cascone P, Agrillo A, Spuntarelli G, et al. Combined surgical therapy of temporomandibular joint ankylosis and secondary deformity using intraoral distraction. J Craniofac Surg. 2002;13:401–9. doi: 10.1097/00001665-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Papageorge MB, Apostolidis C. Simultaneous mandibular distraction and arthroplasty in a patient with temporomandibular joint ankylosis and mandibular hypoplasia. J Oral Maxillofac Surg. 1999;57:328–33. doi: 10.1016/s0278-2391(99)90683-3. [DOI] [PubMed] [Google Scholar]
- 27.Mercuri LG. Considering total temporomandibular joint replacement. Cranio. 1999;17:44–48. doi: 10.1080/08869634.1999.11746076. [DOI] [PubMed] [Google Scholar]
- 28.Mercuri LG. Alloplastic temporomandibular joint reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:631–37. doi: 10.1016/s1079-2104(98)90028-2. [DOI] [PubMed] [Google Scholar]
- 29.Quinn PD. Lorenz prosthesis. Oral Maxillofac Surg Clin North Am. 2000;12:93–104. [Google Scholar]
- 30.Guarda NL, Manfredini D, Ferronato G. Temporomandibular joint total replacement prosthesis: current knowledge and considerations for the future. Int J Oral Maxillofac Surg. 2008;37:103–10. doi: 10.1016/j.ijom.2007.09.175. [DOI] [PubMed] [Google Scholar]
- 31.Bisla RS, Inglis AE, Ranawat CS. Joint replacement surgery in patients under thirty. J Bone Joint Surg Am. 1976;58:1098–106. [PubMed] [Google Scholar]
- 32.Ruddlesdin C, Ansell BM, Arden GP, Swann M. Total hip replacement in children with juvenile chronicarthritis. J Bone Joint Surg Br. 1986;68:218–22. doi: 10.1302/0301-620X.68B2.3958006. [DOI] [PubMed] [Google Scholar]
- 33.Mercuri LG, Edibam NR, Giobbie-Hurder A. 14-Year Follow-Up of a Patient Fitted Total Temporomandibular Joint Reconstruction System. J Oral Maxillofac Surg. 2007;65:1140–48. doi: 10.1016/j.joms.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 34.Mercuri LG. Discussion on: Van Loon et al., 1995: Evaluation of temporomandibular joint prostheses: review of the literature from 1946 to 1994 and implications for future prosthesis designs. J Oral Maxillofac Surg. 2005;53:996–97. doi: 10.1016/0278-2391(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 35.MacIntosh RB. The use of autogenous tissue in temporomandibular joint reconstruction. J Oral Maxillofac Surg. 2000;58:63–69. doi: 10.1016/s0278-2391(00)80019-1. [DOI] [PubMed] [Google Scholar]
- 36.Ellis E, Schneiderman ED, Carlson DS. Growth of the mandible after replacement of the mandibular condyle: An experimental investigation in Macaca mulatta. J Oral Maxillofac Surg. 2002;60:1461–71. doi: 10.1053/joms.2002.36124. [DOI] [PubMed] [Google Scholar]
- 37.Saeed NR, Kent JN. A retrospective study of the costochondral graft in TMJ reconstruction. Int J Oral Maxillofac Surg. 2003;32:606–9. doi: 10.1054/ijom.2003.0418. [DOI] [PubMed] [Google Scholar]
- 38.Perrott DH, Umeda H, Kaban LB. Costochondral graft construction/reconstruction of the ramus/condyle unit: Long-term follow-up. Int J Oral Maxillofac Surg. 1994;23:321–28. doi: 10.1016/s0901-5027(05)80046-3. [DOI] [PubMed] [Google Scholar]
- 39.Kaban LB, Perrott DH. Discussion: Unpredictable growth pattern of costochondral graft. Plast Reconstr Surg. 1992;90:887–89. [PubMed] [Google Scholar]
- 40.Peltomäki T, Vahatalo K, Ronning O. The effect of unilateral costochondral graft on the growth of the marmoset mandible. J Oral Maxillofac Surg. 2002;60:1307–14. doi: 10.1053/joms.2002.35729. [DOI] [PubMed] [Google Scholar]
- 41.Matsuura H, Miyamoto H, Ishimaru J-I, et al. Effect of partial immobilization on reconstruction of ankylosis of the temporomandibular joint with an autogenous costochondral graft: an experimental study in sheep. Br J OMS. 2001;39:196–203. doi: 10.1054/bjom.2001.0623. [DOI] [PubMed] [Google Scholar]
- 42.Perrott DH, Kaban LB. Temporomandibular joint ankylosis in children. Oral Maxillofac Clin North Am. 1994;6:187–99. [Google Scholar]
- 43.Mercuri LG. Alloplastic temporomandibular joint reconstruction. J Oral Surg. 1998;85:631–37. doi: 10.1016/s1079-2104(98)90028-2. [DOI] [PubMed] [Google Scholar]
- 44.Saeed NR, Hensher R, McLeod N, Kent JN. Reconstruction of the Temporomandibular Joint Autogenous Compared with Alloplastic. Br J Oral Maxillofac Surg. 2002;40:296–98. doi: 10.1016/s0266-4356(02)00139-0. [DOI] [PubMed] [Google Scholar]
- 45.Mercuri LG. Commentary. Condyle Replacement after Tumor Resection: Comparison of Individual Prefabricated Titanium Implants and Costochondral Grafts. Oral Surg Oral Med, Oral Pathol, Oral Radiol, Endodontol. 2009;108:153–55. doi: 10.1016/j.tripleo.2009.01.027. [DOI] [PubMed] [Google Scholar]
- 46.Mercuri LG. Temporomandibular Joint Reconstruction. In: Fonseca R, editor. Oral and Maxillofacial Surgery. Chapter 51. Elsevier; Philadelphia: 2008. pp. 945–60. [Google Scholar]
- 47.Maki MH, Al-Assaf DA. Surgical management of temporomandibular joint ankylosis. J Craniofac Surg. 2008;19:1583–88. doi: 10.1097/SCS.0b013e31818ac12c. [DOI] [PubMed] [Google Scholar]
- 48.Guarda-Nardini L, Manfredini D, Ferronato G. Total temporomandibular joint replacement: A clinical case with a proposal for post-surgical rehabilitation. J Cranio-Maxillofac Surg. 2008;36:403–9. doi: 10.1016/j.jcms.2007.11.007. [DOI] [PubMed] [Google Scholar]