Abstract
Objective
To determine the efficacy and effectiveness of training to improve primary care providers’ patient-centered communication skills and proficiency in discussing their patients’ health risks.
Methods
Twenty-eight primary care providers participated in a baseline simulated-patient interaction and were subsequently randomized into intervention and control groups. Intervention providers participated in training focused on patient-centered communication about behavioral risk factors. Immediate efficacy of training was evaluated by comparing the two groups. Over the next three years, all providers participated in two more sets of interactions with patients. Longer term effectiveness was assessed using the interaction data collected at 6 and 18 months post training.
Results
The intervention providers significantly improved in patient-centered communication and communication proficiencies immediately post-training and at both follow-up time points.
Conclusions
This study suggests that the brief training produced significant and large differences in the intervention group providers which persisted two years after the training.
Practice Implications
The results of this study suggest that primary care providers can be trained to achieve and maintain gains in patient-centered communication, communication skills and discussion of adverse childhood events as root causes of chronic disease.
Keywords: patient provider communication, adverse childhood events, adverse adult events, determinants of disease, training
Introduction
The literature documents the close relationship between psychological health and physical health (1–3) and supports the notion that poor psychological health (including traits and states such as depression, anxiety and negative affect) is a predictor of health risk behaviors such as smoking, high saturated fat consumption, physical inactivity, and risky sexual activity (4, 5). Additionally, it is well established that both poor psychological health and health risk behaviors are associated with increased morbidity and mortality in chronic medical illness (6).
The determinants of an individual’s health status are complex, but it has recently been suggested that some influences may be rooted in childhood maltreatment; the practice of risky behaviors or the experience of depression, for example, leading to chronic health outcomes, may be a direct or indirect result of these childhood determinants (7). Felitti’s work on this subject showed elevated odds ratios for a large number of chronic health conditions when an adult had experienced adverse childhood events (8). Subsequently, other large epidemiologic studies have reaffirmed this relationship (9, 10). Both the Centers for Disease Control and the World Health Organization have published the position that childhood maltreatment has long-term adulthood consequences of adverse health outcomes and risky health behaviors (11, 12).
These organizations and researchers further suggest that failing to ask patients about a history of childhood maltreatment obscures the relationship between abuse and health outcomes, and overestimates the strength of other predictive factors and therefore an important potential predictor of adult health problems and health risk behaviors is overlooked. We hypothesized that uncovering and discussing possible childhood determinants of those behaviors with patients would enhance providers’ attempts to address risky behaviors and would result in more success in helping patients to find solutions (13 – 15). (See Appendix A - for a more personal, clinical example.)
Given the role of primary care providers in behavioral risk reduction and chronic disease management, it seems appropriate to consider the primary care visit as an opportunity for such discussions. However, the literature suggests that discussions on health risk determinants rarely take place during the primary care visit (16). This is particularly true for topics about which patients may feel inhibited revealing sensitive information, unless the physician signals an interest in discussing these issues. However, many physicians feel their training does not prepare them to raise these topics in a short primary care encounter, especially one in which so many other pressing physical health problems must be addressed. Even physicians who internalize the importance of listening to behavioral health issues are often at a loss to know realistically how to incorporate them into their practice (17).
The literature documents that relationships between patients and their primary care providers can be enhanced by improvements in communication during the primary care visits (18–20). In particular, the patient-centered approach to communication between clinicians and patients has been gaining prominence in recent years (21 – 24). This approach includes key communication strategies such as eliciting patient perspectives, responding to patient concerns, giving information; partnership building; engaging the patient in participatory decision-making; and developing a follow-up health care plan together (23 – 25). This is a central recommendation of the Institute of Medicine report, “Crossing the Quality Chasm” (26).
Studies have demonstrated positive associations between elements of the patient-centered approach and patient satisfaction (23, 28, 29, 30), patient recall of the content of the health care visit (29), patient compliance (27), patient health outcomes (30 – 33), health care utilization (34) and provider satisfaction (35). More recently, Roter & Larson advocated for a change from the term “patient-centeredness” to the term “relationship-centeredness” to emphasize the relational reciprocity between patient and physician (36). We encouraged the providers to engage in more patient-centered communication to increase the likelihood that the interaction would be more closely aligned with the patient’s psychosocial needs and would therefore facilitate a discussion of childhood adversity.
The purpose of this study was to determine if high intensity communication training (37) with primary care health providers would improve patient-centered communication skills, as well as increase their proficiency in the elicitation of adverse childhood events and discussion of specific high risk health behaviors associated with these adverse events. We evaluated the training using simulated patient visits; actual patient visits were used to determine if training gains could be maintained over time. This study was designed, therefore, to determine both efficacy (assessment of an intervention under controlled conditions) and effectiveness (assessment of an intervention under ‘real life’ conditions). Given the important public health implications of the relationships between childhood adversity and adult health outcomes (10, 11), the training included substantial focus on communication about adverse childhood events.
We hypothesized that the trained providers would improve their skills in patient-centered communication and in the use of specific communication skills, relative to their baseline scores before training. We further hypothesized that the gains seen post-training would persist into actual clinical interactions between providers and their patients at both an initial visit, and at follow-up clinical interactions a year later.
2. Methods
The study was approved by the Institutional Review Boards at the University of New Mexico and the Johns Hopkins Bloomberg School of Public Health.
2.1 Study Setting and Participants
Primary care providers (physicians, physician assistants and nurse practitioners) were recruited to the study from the departments of General Internal Medicine (IM) and Family Practice (FP) of one university medical system. Twenty six of 60 (43%) eligible providers agreed to participate in the study and were randomized to receive training or serve as a control. The randomization process was stratified by gender and specialty, because prior studies have shown superior communication skills in female physicians and in primary care physicians (38, 39). Table 1 shows the demographic distribution of the providers, by practice type, treatment group, and sex. Chi-square analyses revealed no significant differences between the groups in terms of sex or practice type, either at baseline or at the final medical visit. Table 2 shows the distribution of the providers per treatment group and their enrolled patients at both first and second actual medical visits.
Table 1.
Provider Distribution by Treatment Group, Practice Type and Gender.
| Control | Intervention | ||||
|---|---|---|---|---|---|
| Practice Type a | Male | Female | Male | Female | |
| FP | 5 | 3 | FP | 4 | 2 |
| IM | 2 | 2 | IM | 1 | 3 |
| ML* | 1 | 1 | ML | 0 | 2 |
| 8 | 6 | 5 | 7 | ||
| Total | 14 | 12 | |||
Practice Type: FP = Family Practice Physicians, IM = Internal Medicine Physicians, ML = Mid Level Providers (Physician Assistants and Nurse Practitioners).
Mid-level providers who participated were from both departments (Family Practice and Internal Medicine)
Table 2.
Providers and Enrolled Patients in Actual Medical Visits
| First Actual Medical Visit | Second Actual Medical Visit | |||
|---|---|---|---|---|
| Group | Provider | # Patients | Provider | # Patients |
| Intervention | 104 | 10 | 104 | 10 |
| 105 | 3 | 105 | 2 | |
| 106 | 1 | 106 | 0 | |
| 108 | 2 | 108 | 0 | |
| 110 | 4 | 110 | 3 | |
| 119 | 11 | 119 | 11 | |
| 120 | 10 | 120 | 10 | |
| 122 | 7 | 122 | 6 | |
| 127 | 3 | 127 | 3 | |
| 128 | 5 | 128 | 4 | |
| Control | 102 | 5 | 102 | 4 |
| 103 | 1 | 103 | 0 | |
| 109 | 2 | 109 | 2 | |
| 111 | 5 | 111 | 4 | |
| 112 | 8 | 112 | 6 | |
| 114 | 5 | 114 | 3 | |
| 115 | 4 | 115 | 3 | |
| 116 | 5 | 116 | 5 | |
| 124 | 8 | 124 | 6 | |
| 125 | 5 | 125 | 5 | |
| 126 | 7 | 126 | 5 | |
| 127 | 3 | 127 | 3 | |
| 129 | 2 | 129 | 2 | |
2.2 Training
Training consisted of three components: a full-day training, individualized feedback on video-taped interactions with simulated patients, and optional workshops to reinforce strategies for engaging the patient. Providers in the intervention group were required to attend the full-day training; the morning session included a lecture on adverse childhood events and their relationship to health outcomes, as well as a presentation of the study goals, procedures and instruments. The afternoon session was interactive and included role-play and training in patient-centered communication skills, health risk behavior assessment and referrals to other resources appropriate to childhood adversity, as well as elements of motivational interviewing. Intervention group participants were given continuing medical education (CME) credits for this activity, both intervention and control group participants were compensated with $100.00.
All study providers were audio-taped with a simulated patient at baseline, prior to any training. After the full-day training with the intervention group providers was completed, all study providers were again assessed with a second simulated patient. This interaction was video-taped so that the providers in the intervention group could be given individualized feedback on their performance based on training content (i.e. RIAS coding of skills and notation of discussion associated with targeted topic areas) (40).
In addition to the full-day training and individualized feedback on the video-taped simulated patient interactions, two optional workshops were made available to intervention group providers. One workshop was designed to illustrate the process of reflective writing, and how that might be useful to patients, following the work of Pennebaker (41) who has published extensively on patient health benefits of this technique. The second focused on motivational interviewing with role playing exercises to help providers talk with patients about the relationship between their adverse events and health status. Since participation in the workshops was optional, attendance was not monitored.
2.3 Assessment Procedures
2.3.1 Simulated Patient Interactions
Four equivalent standardized cases were developed to assess the effectiveness of training. For each case, the patient (male or female) with a chronic disease (diabetes or hypertension) had a stated goal of establishing a relationship with a new provider and to renew a prescription. The simulated patient was instructed to disclose additional information only if prompted by the provider so that underlying causes of risk behavior (i.e., ACE) would only be uncovered if the provider used the skills taught in the training. (See Appendix B. There were four simulated patients, one female and one male for each of the two cases.) Providers were randomly assigned to either Case A or B (hypertension or diabetes) with a male or female patient for the baseline simulation and the opposite case and gender for the follow up simulation.
The simulated patients were blind to the provider group assignment. The first simulation was audio taped. The second simulation was videotaped so that providers could receive feedback from trainers to further improve their communication skills while watching their own interactations with the simulated patient.
2.3.2 Actual Medical Visits
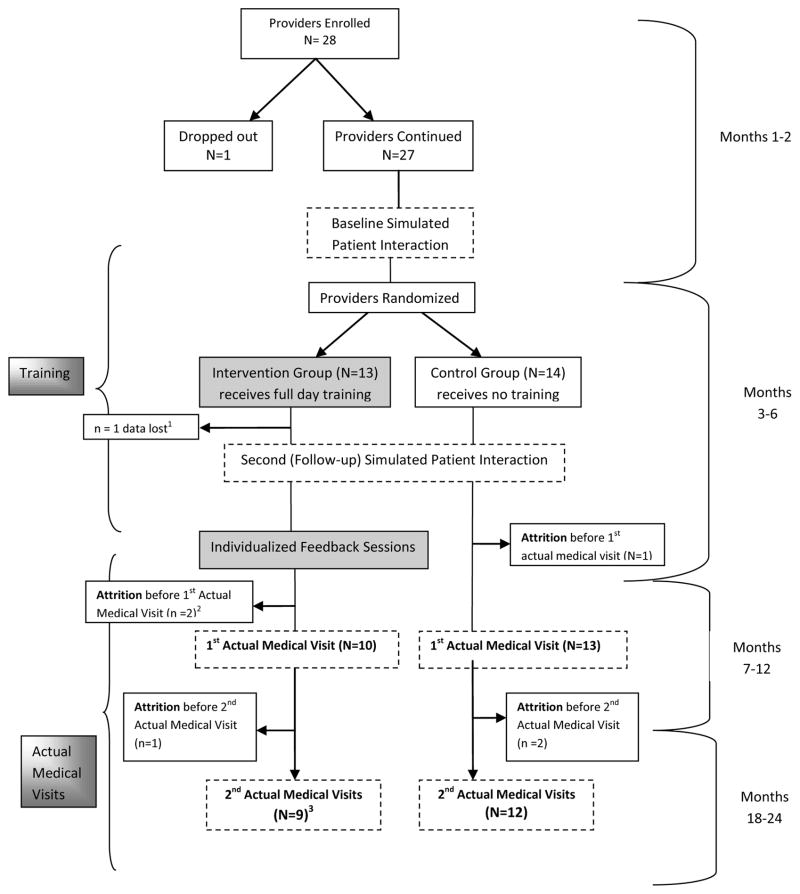
After training was complete for intervention providers, we implemented a study utilizing actual patients to determine whether the training continued to be effective under natural conditions. This trial utilized the results from a health risk assessment (HRA) to focus the communication in the annual medical visit on the determinants of risk behavior (such as experience of childhood adversity) and their relationships to short-term health outcomes and quality of life (See Helitzer et al., forthcoming, for a description of the HRA intervention). The medical dialogue for all study visits was audio-tape recorded. Figure 1 depicts the provider assignment, training, measurements and the timing of all study components.
Figure 1.
Provider Assignment, Training and Measurements. (Dotted lines indicate assessment activities; shadow boxes indicate intervention trainings)
1Recoding error resulted in lost data
2Attrition rates analyzed for between-group differences using a chi-square test and found to be non-significant.
3All “N’s” reported here reflect providers who had ≥1 patients enrolled; however providers who had only 1 patient visit are not included in the analysis.
2.4 Measures
2.4.1 Coding of Medical Visit Communication
The study’s simulations and actual medical visit recordings were coded with the Roter Interaction Analysis System (RIAS). The RIAS is a widely used coding system with demonstrated reliability and predictive validity in studies of patient-physician communication (36, 42, 43, 44). This system assigns each complete thought expressed by the patient and physician to 1 of 37 mutually exclusive and exhaustive codes or categories of communication. These categories can be manipulated to reflect groups of exchange representing 3 recognized functions of the medical interview: data gathering (open and closed biomedical and psychosocial questions), patient education and counseling about biomedical and psychosocial topics, and relationship building through emotionally responsive exchange (empathy, concern, approval, and reassurance) (45). A fourth function of partnership building (seeking patient opinion, asking for understanding, and checking for understanding through paraphrase and interpretation) is also reflected (22).
Individual RIAS codes were combined to create a patient-centeredness summary score; a ratio of all codes relating to socio-emotional and psychosocial elements of exchange (all partnership-building, psychosocial information and counseling, relationship-building, positive, negative, and social talk by providers and patients, all physician open-ended questions, and all patient questions) divided by codes that further the biomedical agenda (the sum of all physician and patient biomedical information and counseling, orientations, and physician closed-ended questions) (36). This summary score was used as a dependent variable in the analyses of the training and actual medical visit data (range = 0–5).
In addition to the standard RIAS codes, 21 communication proficiencies (shown in Table 3) that were related to the training content were documented as present or absent during the simulated patient interactions. These generic skills were chosen for training evaluation under the assumption that they would translate easily into proficiency in specific content discussion when the actual medical visit portion of the study began, and because one of the generic codes (003: elicitation of family history contributing factors) reflects attempts on the part of the provider to introduce discussion of ACE.
Table 3.
Communication proficiencies assessed during training phase
| Code | Name | Examples of Utterances |
|---|---|---|
| 001 | Identification of Problem (example: stress) | It sounds like things are really tough for you. This sounds like a lot of (stress) |
| 002 | Elicits Contributing Factors | What is making you feel this way – do you know? When you’re having trouble falling asleep, what are you thinking about? |
| 003 | Elicits Family History Contributing Factors | Is there a reason why you don’t see your parents? Did your father drink heavily? |
| 004 | Elicits Values, Beliefs about Problem | So you don’t necessarily see things the same way as your mother did – is that right? |
| 005 | Elicits (current) coping strategies | How are you coping with things/the stress right now? What do you do to relax? |
| 006 | Elicits other (current) support system information | Do you have friends who you can talk to about this? |
| 007 | Asks Depression Screen Questions | Would you say you have been feeling down in the dumps? Would you describe yourself as feeling sad, depressed or unhappy for more than 2 weeks? |
| 008 | Assess Readiness for Change | Have you been thinking about leaving your husband? Are you ready to make a change? |
| 009 | Discuss pros/cons of change | So you think it’d be better for your son if you left – is that right? And how about your health – are you thinking your health might also improve? |
| 010 | Discuss barriers, obstacles to change | Do you think you’d be able to support yourself if you left [husband]? So this is something you’ve tried to do before – what happened? |
| 011 | Discuss solutions to barriers | Do you have any family that could help temporarily? |
| 012 | Discuss available therapies, services | There are support groups, counseling services |
| 013 | Offer of help, support of doctor (non abandonment) | And I can always be reached, so I want you to call me. We’ll continue to work together on this. |
| 014 | Discuss costs, insurance, paperwork for proposed therapies | The costs of seeing a therapist are the same as the co-pay for this visit today. Your insurance will cover it. |
| 015 | Doctor gives materials | These booklets may be useful for reference. |
| 016 | Patient asks for materials | Do you have any materials for me to read? |
| 017 | Discussion of follow up plan, another appt. | I’d like to see you again in 2 weeks |
| 018 | Doctor asks for commitment to plan | Do you think you’ll be able to come back then? |
| 019 | Discussion of family/friend involvement | Would it help if your husband came along next time? |
| 020 | Referral/Other Professional | I’d like you to see Dr. C. My nurse will make an appointment for you. |
| 021 | Referral/Other Resources | Here’s a web site that may help you to understand this better. |
A ‘proficiencies summary score’ was computed as the sum of the 21 present/absent scores, and used as a dependent variable in the analysis of the training data (range = 0–21).
During the actual medical visit, discussion about 7 content-specific risk domains was documented as present or absent in the medical dialogue, substituting for the general 21 proficiencies measured at training. These topics were selected to reflect the domains included on the HRA: ‘diet, weight and exercise’, ‘risk taking behaviors’, ‘substance use’, ‘depression, anxiety and stress’, ‘suicide and violent behavior’, adverse adult events’, and ‘adverse childhood events’.
In order to ensure satisfactory inter-rater reliability, a random sample of 10% of all of the tapes was re-coded by a second coder. As in several other studies, the coding system demonstrated adequate inter-coder reliability for basic RIAS coding (average reliability greater than .85 based on a Pearson Correlation Coefficient between coders) (36). Of the 21 skill categories, 100% agreement was reached on 17; 91% agreement was reached on the remaining four categories. Eleven tapes from the actual medical visits were re-coded to analyze the coding of the content-specific domains; the agreement between coders was 100%.
2.5 Statistical Analyses
Several different analyses were undertaken with the training data (patient-centeredness and 21 proficiencies) and the actual medical visit data (patient-centeredness and 7 content-specific risk domains).
Pre-training differences were tested for significance using independent group t-tests to ensure that there were no pre-treatment differences between the intervention and control groups. The efficacy of training was then tested with two split plot analyses (one each for the patient-centeredness summary score and the proficiencies summary score) using pre- and post-training as repeated measures and group membership (intervention vs. control) as a between-subjects factor. For both variables, Cohen’s d was calculated as the difference between the time one and time two means for each group.
For the analyses of the the patient-centeredness summary score in the actual medical visit data, linear mixed models were used to test for between-group differences at both time points separately. These analyses allow for the random (physicians) and nested (physicians nested within group) effects. For the 7 content-specific risk domains which were scored as “present” or “absent”, generalized estimating equations were utilized to test for between-group differences at both time points separately. GEEs are appropriate for nested designs with dichotomous outcomes.
Effect size for the analysis of patient-centeredness in the actual medical visits was calculated as Hedges ‘g’ (the standardized difference between the groups accounting for within-cluster variance).
For all analyses, effect size measure for the control group was used as a baseline for a practice effect (i.e. the control group’s difference was interpreted as the effect of practice on post-training and scores from second actual medical visits) and was subtracted out of the effect size measure of the intervention group.
All statistical tests were evaluated for significance using an alpha of .05.
3. Results
3.1 Pre- and Post Training Simulated Interactions
The efficacy of the training was examined in terms of differences in provider communication proficiencies, and in the patient-centeredness summary score, which was used as a dependent variable in analyses.
No significant pre-training differences were found between the groups. As is reflected in Table 4, the interaction of time by group was significant, indicating that providers who received the training showed significant and differential improvements on both these variables; (Interaction significance tests: proficiencies summary score, F(1,24) = 5.86, p < .05, d= 1.60; patient-centeredness summary score, F(1,24) = 7.67, p < .05, d=.86).
Table 4.
Use of Communication Proficiencies and Patient-centered Communication During the Training Phase with Simulated Patients
| Measures of Medical Dialogue | Study Group | Time One Pre-Training Mean (SD) | Time Two Post-Training Mean (SD) | Time One vs. Time Two p | Group X Time Interaction p | Effect Size d |
|---|---|---|---|---|---|---|
| Use of 21 targeted skills -- All skills Combined1 | Intervention (n=12) | 6.58 (1.93) | 12.83 (3.61) | p <.001 | p= 0.026 | 1.602 |
| Control (n=14) | 6.50 (2.95) | 8.36 (3.67) | ns | 0.56 | ||
| Patient-Centeredness3 | Intervention (n=12) | 1.96 (1.04) | 3.56 (1.35) | p =.011 | p =.041 | .862 |
| Control (n=14) | 2.18 (1.04) | 2.38 (1.04) | ns | .11 |
Note:
Sum of 21 proficiencies coded as 0 = absent vs. 1 = present; range of possible scores is 0–21
Net effect of training in standard deviation units after subtracting out an estimated practice effect
Range of possible scores is 0–5
3.2 Actual Medical Visits
At the first actual medical visit, the result of the linear mixed model analysis revealed a significant difference in scores, favoring the intervention group providers, on the RIAS-based summary measure of patient-centeredness, F(1, 20.59) =8.43, p < .01. Hedges ‘g’ for this effect was .68.
The analysis of the 7 content-specific risk domains showed a significant difference between the intervention and control groups in the discussion of adverse childhood events, Wald’s χ2(1)=6.83, p<.001. Both of these differences favored the intervention group.
At the one-year follow up visit, the intervention group’s significantly higher patient-centeredness summary score was sustained, F(1, 17.16) = 5.48, p = .032. Hedge’s g for this effect was .69. Additionally, there continued to be a significant group effect, favoring the intervention group, for the discussion of adverse childhood events, Wald’s χ2(1)=6.01, p<.001. None of the other content-specific risk domains showed differences in frequency of discussion between the groups. All means are shown in Table 5.
Table 5.
Discussion of the 7 HRA Content Areas and Patient-Centered Communication at 1st and 2nd Actual Medical Visits
| Content Area Discussed 1 | Group | 1st Actual Medical Visit Mean (SD) | Group Difference2 p Effect Size | 2nd Actual Medical Visit Mean (SD) | Group Difference3 p Effect Size |
|---|---|---|---|---|---|
| Diet, Weight & Exercise1 | Intervention (I) | .93 (.09) | ns | 1.00 (.00) | ns |
| Control (C) | .93 (.15) | .93 (.16) | |||
| Risk-Taking Behaviors | (I) | .62 (.33) | ns | .35 (.40) | ns |
| (C) | .58 (.36) | .48 (.36) | |||
| Substance Use | (I) | .70 (.26) | ns | .71 (.21) | ns |
| (C) | .82 (.26) | .67 (.35) | |||
| Depression, Anxiety & Stress | (I) | .79 (.28) | ns | .65 (.37) | ns |
| (C) | .72 (.25) | .74 (.29) | |||
| Suicide& Violent Behavior | (I) | .09 (.18) | ns | .07 (.19) | ns |
| (C) | .07 (.15) | .00 (.00) | |||
| Adverse Adult Events | (I) | .24 (.31) | ns | .16 (.19) | ns |
| (C) | .11 (.15) | .12 (.18) | |||
| Adverse Childhood Events | (I) | .43 (.19) |
p < .001 d=1.16 |
.30 (.17) |
p < .001 d=2.81 |
| (C) | .16 (.22) | .02 (.06) | |||
| Patient -Centeredness | (I) | 3.67 (1.30) |
p < .01 g = .68 |
3.30 (1.19) |
p < .05 g = .69 |
| (C) | 2.42 (.67) | 2.55 (.69) |
Note:
The means shown are weighted means for the frequency with which each content area was discussed (averaged within one provider over all his/her patients)
1st actual medical visit differences are reported to show that training gains were maintained into the clinical setting among the intervention group providers
2nd actual medical visit differences are reported to illustrate lasting effects of training/effects of optional workshops.
4. Discussion and Conclusion
This study was designed to determine both the efficacy and effectiveness of training to increase patient-centered communication, communication proficiency and discussion of targeted topics by primary care providers. Efficacy was assessed by analysis of physician interactions with simulated patients. Effectiveness was assessed by analysis of physician interactions in the clinical setting with their patients.
4.1 Efficacy of Training
These results support the conclusion that the provider training was efficacious at improving patient-centeredness communication, and at increasing provider communication proficiencies. Effect sizes for both these changes in the trained group immediately post-training were ‘large’ to ‘very large’ by commonly accepted standards. This result is consistent with a large-scale review which found that those training interventions defined as ‘high intensity’ (defined as >1 contact with trainees, involvement of research personnel, and more than one delivery modality), produced significant improvements in the communication behaviors of physicians, particularly the asking of more open-ended questions and fewer biomedically focused questions (37).
The RIAS-based patient-centeredness summary score reflects a variety of communication elements covered extensively in the training. In addition, the results of the analysis of provider communication proficiency show that training resulted in differential improvements among the intervention providers in the performance of the 21 communication skills. Given that training focused on both of these areas, it is not surprising that the intervention group demonstrated such a large increase on these variables, even after subtracting out an estimated practice effect.
It is worth noting that causal inferences about differences between intervention and control providers are weakened because the control group was not given a ‘placebo’ intervention. In ideal circumstances, control providers would have been offered a day-long psycho-educational seminar on a different topic. There is also the possibility that other non-specific effects related to group assignment may have occurred. These effects can be both positive, such as intervention providers changing behaviors as a result of being in the treatment arm; or negative, such as control group providers experiencing a ‘demotivation’ effect as a result of randomization to the control group, which had other drawbacks such as inability to accrue CME credits. A clear drawback for studies such as these is that it is challenging to blind participants (in this case, providers) to their group assignment and thus the causal inference drawn is open to challenge.
4.2 Effectiveness of Training in the Clinical Setting
In the actual medical visits at both the initial visit and one-year follow up, there were large and significant differences between the intervention and control groups in patient-centered communication and in the discussion of adverse childhood events. We interpret these results to indicate that the gains achieved after the training were maintained in the clinical setting, and perhaps enhanced by the optional workshops with the intervention group. Providers who attended the mid-intervention optional workshop (between medical visits 1 and 2) were motivatated to maintain their skills. Further, many stated that they believed additional discussion and role playing would reinforce their proficiency in discussing difficult subjects within the actual medical visit.
Due to data collection and coding protocols, we were unable to examine whether the patient or the provider initiated the discussion of childhood adverse events. In addition, the health-risk assessment (HRA) that patients filled out prior to their annual medical visits included questions about childhood adversity, possibly priming patients to raise these issues with their physicians regardless of the physicians’ group assignment. Despite the fact the some of the intervention group providers expressed discomfort discussing adverse childhood events and were concerned about raising this topic in a brief primary care encounter, the results suggest that the training provided skills to engage in this discussion no matter whether the topic was raised by the patient or the provider.
The available literature on provider training in communication skills suggests that while brief trainings can be effective, longer trainings, or those with follow ups that reinforce original training topics are more effective (46, 47). Training gains that occurred with the one-day exposure to the group training session and one-on-one feedback using the videotaped post-training sessions with the simulated patients indicate that intensive training was sufficient to change and maintain the improvement in communication behaviors.
When the study was proposed, the numbers of providers in the two clinical departments was approximately 90. 30 providers left the institution prior to the start of recruitment, greatly reducing the available number of providers from whom to recruit. Of the 60 eligible providers, less than half initially agreed to participate; those who didn’t cited concerns about the time burden and loss of confidentiality due to tape-recording. In addition, providers in this university practice were generally unfamiliar with health services research and its potential benefits to their practice. Those who did agree to participate were therefore more motivated to overcome these barriers and thus may represent an unusual population, which limits the generalizability of our results.
4.3 Practice Implications
The results of this study suggest that primary care providers can be trained to achieve and maintain gains in patient-centered communication, communication skills and discussion about adverse childhood events. In this study, the gains were maintained over a period of 24 months.
We hypothesize that discussion of the underlying or root causes of disease, such as adverse childhood events, is important to improving health outcomes. Providers may be reluctant to talk about these issues because they raise difficult topics for which there may be no prospective treatment options and little evidence that discussing them will have any benefit. Doctors face competing demands within a brief patient visit and are disinclined to spend what limited time they have discussing sensitive topics that may open up “a Pandora’s Box”, putting them in an uncomfortable or awkward position of discussing subjects for which their training has not prepared them. However, there is evidence that the disclosure of traumatic events may reduce patient anxiety and improve patient outcomes (41), whether or not the disclosure involves the primary care provider directly.
The evidence reviewed here demonstrates that improvements can be made in provider communication skills; such skills have shown to be associated with improvement in patient outcomes, such as satisfaction and adherence to provider recommendations (23, 27, 28, 29). In addition, training can be useful to help focus interactions on specific content areas, even if those conversations are difficult or sensitive. To our knowledge, no other interventions have been tested to assess whether the gains in patient-centered communication and proficiency in discussing adverse events found in this study may lead to reductions in risk behavior. We are currently testing these hypotheses in the context of the HRA intervention study reported elsewhere.
Acknowledgments
We wish to thank the Departments of Family and Community Medicine and Internal Medicine at the University of New Mexico School of Medicine, the providers and simulated patients who participated in this study, and the ACE Study group for their assistance in making this study possible. In addition to the authors, team members who participated in the development of the training and the analysis of the data include (in alphabetical order): Stewart Duban, Denise Ernst, David Graeber, Richard Hough, Arthur Kaufman, Susan Larson, Samara Lloyd, Nancy Oestreicher, Karla Thornton, and Carolyn Voss. Finally, we acknowledge the financial support and personal encouragement of the Centers for Disease Control and Prevention, without which the study would not have been conducted.
Support: This research was supported through a grant from the Centers for Disease Control (RO1-CD-04-002).
Appendix A
Dr. O. is a primary care physician at our institution who shared with us the story of one of his patients – an obese woman whom he had been seeing for 14 years. He felt that he had had little success in helping her to address her eating or exercise behavior. In fact, he said, he felt like a failure as a physician with this patient. Dr. Felitti came to our institution in 2002 and Dr. O. was excited to hear the evidence suggesting that adult health risk behaviors like overeating may be related to childhood trauma and/or adversity. He was encouraged by Dr. Felitti to ask the patient whether she had experienced any childhood adversity. She disclosed that she had been abandoned by an alcoholic mother at a young age. She was unable as an adult to develop close and trusting relationships and therefore spent a lot of time home alone, eating. The provider felt that he had a much better understanding of the patient after this discussion and was able to arrive at a completely different recommendation for her focusing not on the obesity but on the development of a meaningful relationship. He encouraged her to adopt a dog who would give her unconditional love. He knew (without discussing this specific fact with her), that the dog would need to be walked, thereby surreptitiously inducing her to exercise. Six months later, she reported being in love with the dog and that she took the dog for a daily walk. Dr. O noted that her weight had decreased. The patient reported never having spoken about those childhood events before and both parties felt strongly that their relationship was enhanced by an increased sense of trust and understanding. The patient felt ‘heard’ and the physician felt empowered to incorporate that knowledge into a better treatment plan, one that addressed both the patients’ physical health as well as her mental health.
Appendix B
Appendix A-Simulated Patient Case A
| Case A |
|---|
|
Patient: Harriett/Harry Stock [Hyperactive, impatient, restless, too much exercise, underweight] Harriet’s husband is Duane, Harry’s wife is Linda, and daughter/son is named Morgan |
| Diagnosis: Annual Visit |
| Purpose of Case: Assess the patient/provider interaction with disclosure of traumatic life events |
| Characteristics of the Patient: You are a patient in your 40’s with a history of hypertension. You are dressed neatly with light makeup (if a woman). You are cooperative and friendly, seem full of energy, you are constantly tapping your foot through out the visit and use your hands a lot when you talk. You think of yourself as pretty healthy. Exercise all the time and take vitamins and eat only organic food. UNM recently shifted insurance carriers so you are here to establish with this provider. You also need a refill on your blood pressure meds. (Much later in the visit, you might be asking for a prescription for a sleeping aid because you sometimes have difficulty sleeping.) |
| Past Medical History: You have a history of high blood pressure, which was discovered 4 years ago. (For Harriett, this was after the birth of her daughter.) You think it’s under control; you are currently taking medication for it (name of drug). No other major health problems. You have no allergies to food or medication. During graduate school you had ulcers. Once you had shingles when you were up for your third year review (two years ago). High blood pressure was discovered after the birth of her daughter 4 years ago (female). High blood pressure was discovered in an annual physical 4 years ago (male). |
Social History: You work at UNM health sciences campus full time as an assistant professor in the department of neurosciences. Your topic of research is glial cell scanning. You are working on writing lots of grants to get funding for your research, so things have been pretty stressful lately. You are trying to get tenure track, “publish or perish”. You are going up for promotion in two years and you have to get enough publications by then or you will lose your job. So you have been exercising a lot to relieve stress. You exercise regimen includes running 5 miles in the morning, 2 hours of cardio and weights at the gym in the afternoon, and sometimes, depending on your situation at home, go for another run in the evening, another 2–5 miles.
|
Family History: Your parents were very healthy. Always pressuring to do well in school and get an education. Your parents argued a lot about how to raise the kids.
|
| Case B |
|---|
|
Patient: Jane Velarde, Joe Velarde Jane’s husband is Alberto, Joe’s wife is Alison Children are daughter Sheri, age 15 and son Phil, age 17 Jane’s birth date is October 10, 1950 [Depressed, heavy drinker (male), smoking pot (female), overweight] |
| Diagnosis: establishing new provider |
| Purpose of Case: Assess the patient/provider interaction with disclosure of traumatic life events |
| Characteristics of the Patient: You are a patient age 55 with a history of asthma. You are dressed neatly with light makeup (if a woman). You are cooperative and friendly, but uncomfortable being at the doctor’s office. You think you are pretty healthy; always manage to make it to work. UNM recently changed insurance carriers so you have made this appointment to get established with this provider and get a refill on your asthma inhaler (Albuterol, Advair?) |
| Past Medical History: You have a history of asthma, you think it’s under control; you are currently taking medication for it in the form of an inhaler. No other major health problems. You have no allergies to food or medication. |
Social History: You have two kids Sheri who is 15 and Phil who is 17. You work at UNM main campus full time (male- maintenance technician, you just got transferred to do work at the President’s office where the standards are very high; female- administrative assistant at Office of Student Affairs your office is located in the Student Union Building. You are currently going through some rough times with your marriage, possibly getting separated and/or divorced
|
| Family History: Your mother had many health problems when you were young, you don’t really know what they were just that she couldn’t really take care of you and your siblings (2 sisters in California). Your father was an alcoholic who was verbally abusive to your mother and the kids. Mom tried to leave with the kids on numerous occasions but was never able to actually do it. Your siblings are in pretty good health as far as you know, they live out of state. |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Deborah L. Helitzer, Professor, Department of Family and Community Medicine, MSC 09-5040, 1 University of New Mexico, Albuquerque, NM 87131
Marianna LaNoue, University of New Mexico School of Medicine
Bronwyn Wilson, University of New Mexico School of Medicine
Brisa Urquieta de Hernandez, BUS, University of New Mexico School of Medicine.
Teddy Warner, University of New Mexico School of Medicine
Debra Roter, The Johns Hopkins Bloomberg School of Public Health
References
- 1.Smith BW, Zautra AJ. Vulnerability and resilience in women with arthritis: Test of a two factor model. J Consult Clin Psychol. 2008;76:799–810. doi: 10.1037/0022-006X.76.5.799. [DOI] [PubMed] [Google Scholar]
- 2.Coulehan JL, Schulberg HC, Block MR, Madonia MJ, Rodriguez E. Treating depressed primary care patients improves their physical, mental, and social functioning. Arch Intern Med. 1997 May 26;157(10):1113–20. [PubMed] [Google Scholar]
- 3.Mechanic D. Sociological dimensions of illness behavior. Soc Sci Med. 1995;41(9):1207–16. doi: 10.1016/0277-9536(95)00025-3. [DOI] [PubMed] [Google Scholar]
- 4.Paxton RJ, Valois RF, Watkins KW, Huebner ES, Drane JW. Associations between depressed mood and clusters of health risk behaviors. Am J Health Behav. 2007;31(3):272–283. doi: 10.5555/ajhb.2007.31.3.272. [DOI] [PubMed] [Google Scholar]
- 5.Strine TW, Chapman DP, Okoro CA, Balluz L. Health-Related quality of life, health risk behaviors and disability among adults with pain-related activity difficulty. Am J Public Health. 2005;95(11):2042–2048. doi: 10.2105/AJPH.2005.066225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 7.Sneed JR, Kasen S, Cohen P. Early-life risk factors for late-onset depression. Int J Geriatr Psychiatry. 2007;22(7):663–7. doi: 10.1002/gps.1727. [DOI] [PubMed] [Google Scholar]
- 8.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4) doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 9.Anda Felitti, Bremmer Walker, Whifield Perry, Dube Giles. The Enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. Eur Arch Clin Neurosci. 2006;256(3):174–86. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Surtees PG, Wainwright NWJ. The shackles of misfortune: Social adversity assessment and representation in a chronic-disease epidemiological setting. So Sci Med. 2007;64:1, 95–111. doi: 10.1016/j.socscimed.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Preventing Child Malteratement. [accessed 12/11/2009];Program Acitivities Guide. n.d [ http://www.cdc.gov/violenceprevention/pdf/PreventingCM-a.pdf]
- 12.Butchart A, Harvey AP. [accessed 12/11/2009];Preventing Child Maltreatment: a guide to taking action and generating evidence. 2006 http://whqlibdoc.who.int/publications/2006/9241594365_eng.pdf.
- 13.Becker-Blease KA, Freyd JJ. Research participants telling the truth about their lives: the ethics of asking and not asking about abuse. Am Psychol. 2006;61(3):218–226. doi: 10.1037/0003-066X.61.3.218. [DOI] [PubMed] [Google Scholar]
- 14.Read J. To ask, or not to ask, about abuse—New Zealand research. Am Psychol. 2007;62(4):325–6. doi: 10.1037/0003-066X62.4.325. [DOI] [PubMed] [Google Scholar]
- 15.Edwards VJ, Dube SR, Felitti VJ, Anda RF. It’s ok to ask about past abuse. Am Psychol. 2007;62(4):327–8. doi: 10.1037/0003-066X62.4.327. [DOI] [PubMed] [Google Scholar]
- 16.Wissow LS, Roter D, Larson SM, Wang MC, Hwang WT, Johnson R, Luo X. Mechanisms behind the failure of residents’ longitudinal primary care to promote disclosure and discussion of psychosocial issues. Arch Pediatr Adolesc Med. 2002 Jul;156(7):685–92. doi: 10.1001/archpedi.156.7.685. [DOI] [PubMed] [Google Scholar]
- 17.Mechanic D. Physician Discontent: Challenges and Opportunities. JAMA. 2003;290:941–946. doi: 10.1001/jama.290.7.941. [DOI] [PubMed] [Google Scholar]
- 18.Stewart MA, Roter D. Communicating with Medical Patients. Thousand Oaks, Calif: Sage Publications; 1989. [Google Scholar]
- 19.Stewart M. Continuity, care, and commitment: the course of patient-clinician relationships. Ann Fam Med. 2004;2(5):388–90. doi: 10.1370/afm.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart M. Reflections on the doctor-patient relationship: from evidence and experience. Br J Gen Pract. 2005;55(519):793–801. [PMC free article] [PubMed] [Google Scholar]
- 21.Laine C, Davidoff F. Patient-centered medicine. A professional evolution. JAMA. 1996;275(2):152–6. [PubMed] [Google Scholar]
- 22.Taylor K. paternalism, participation and partnership – The evolution of patient centerdness in the consultation. Patient Educ Couns. 2009;74(2):150–155. doi: 10.1016/j.pec.2008.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Anderson D. Dialogue and collaboration: a path for progress. Sci Pract Perspect. 2002 Jul;1(1):3. [PMC free article] [PubMed] [Google Scholar]
- 24.Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-Patient Communication: A Review of the Literature. Sco Sci Med. 1995;40:903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- 25.Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc. 2008;100(11):1275–85. doi: 10.1016/s0027-9684(15)31505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crossing the quality chasm. Institute of Medicine (IOM); 2001. [Google Scholar]
- 27.Frederikson LG. Exploring information-exchange in consultation: the patients’ view of performance and outcomes. Patient Educ Couns. 1995 Jul;25(3):237–46. doi: 10.1016/0738-3991(95)00801-6. [DOI] [PubMed] [Google Scholar]
- 28.Cecil DW, Killeen I. Control, compliance, and satisfaction in the family practice encounter. Fam Med. 1997 Oct;29(9):653–7. [PubMed] [Google Scholar]
- 29.Bertakis KD. The communication of information from physician to patient: a method for increasing patient retention and satisfaction. J Fam Pract. 1977;5(2):217–22. [PubMed] [Google Scholar]
- 30.Roter DL, Hall JA, Katz NR. Relations between physicians’ behaviors and analogue patients’ satisfaction, recall, and impressions. Med Care. 1987;25(5):437–51. doi: 10.1097/00005650-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Little P, Everitt H, Williamson I, Warner G, Moore M, Gould C, Ferrier K, Payne S. Preferences of patients for patient centered approach to consultation in primary care: observational study. BMJ. 2001;322:468–472. doi: 10.1136/bmj.322.7284.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greenfield S, Kaplan SH, Ware JE, Jr, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3(5):448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 33.Kaplan SH, Greenfield S, et al. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 34.Honda K. Factors Underlying Variation in Receipt of Physician Advice on Diet and Exercise: Applications of the Behavioral Model of Health Care Utilization. Am J Health Promot. 2004;18(5):370–77. doi: 10.4278/0890-1171-18.5.370. [DOI] [PubMed] [Google Scholar]
- 35.Smith RC, Lyles JS, Mettler JA, Marshall AA, Van Egeren LF, Stoffelmayr BE, Osborn GG, Shebroe V. A strategy for improving patient satisfaction by the intensive training of residents in psychosocial medicine: a controlled, randomized study. Acad Med. 1995;70(8):729–32. doi: 10.1097/00001888-199508000-00019. [DOI] [PubMed] [Google Scholar]
- 36.Roter D, Larson S. The Roter interaction analysis system (RIAS): utility and flexibility for analysis of medical interactions. Patient Educ Couns. 2002;46(4):243–51. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 37.Rao JK, Anderson LA, Inui TS, Frankel RM. Communication Interventions make a difference in conversations between physicians and patients: a systematic review of the evidence. Medical Care. 2007;45(4):340–349. doi: 10.1097/01.mlr.0000254516.04961.d5. [DOI] [PubMed] [Google Scholar]
- 38.Paasche-Orlow M, Roter DL. The Communication patterns of internal medicine and family practice physicians. JABFM. 2003;16:485–493. doi: 10.3122/jabfm.16.6.485. [DOI] [PubMed] [Google Scholar]
- 39.Roter DL, Hall JA, Aoki Y. Physician gendere Effects in medical communication: a meta-analytic review. JAMA. 2002;288:756–64. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 40.Roter D, Larson S. Use of an innovative video feedback technique to enhance communication skills training. Med Educ. 38(2):145–157. doi: 10.1111/j.1365-2923.2004.01754.x. [DOI] [PubMed] [Google Scholar]
- 41.Pennebaker JW, Seagal D. Forming a story: the health benefits of narrative. J Clin Psychol. 1999;55(10):1243–54. doi: 10.1002/(SICI)1097-4679(199910)55:10<1243::AID-JCLP6>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 42.Roter DL. Observations on methodological and measurement challenges in the assessment of communication during medical exchanges. Patient Educ Couns. 2003;50(1):17–21. doi: 10.1016/s0738-3991(03)00074-0. [DOI] [PubMed] [Google Scholar]
- 43.Newes-Adeyi G, Helitzer DL, Roter D, Caulfield LE. Improving client-provider communication: evaluation of a training program for women, infants and children (WIC) professionals in New York state. Patient Educ Couns. 2004;55(2):210–217. doi: 10.1016/j.pec.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 44.Nelson EL, Miller EA, Larson KA. Reliability associated with the Roter Interaction Analysis (RIAS) adapted for the telemedicine context. Patient Educ Couns. 2009 doi: 10.1016/j.pec.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Roter DL, Stewart M, Putnam SM, Lipkin M, Jr, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277(4):350–6. [PubMed] [Google Scholar]
- 46.Roter D, Rosenbaum J, de Negri B, Renaud D, Diprete-Brown L, Hernandez O. The effects of a continuing medical education programme in interpersonal communication skills on doctor practice and patient satisfaction in Trinidad and Tobago. Med Educ. 1998;32(2):181–9. doi: 10.1046/j.1365-2923.1998.00196.x. [DOI] [PubMed] [Google Scholar]
- 47.Butler L, Degner L, Baile W, Hack T, Brundage M, Bultz B, Carlson L, Davison J, Feldman-Steward D, Parker P, Tiishelman C, Thorne S, Laundry M. Developing communication competency in the context of cancer: a critical interpretive analysis of provider training programs. Psychooncology. 2005;14(10):861–72. doi: 10.1002/pon.948. discussion 873–4. [DOI] [PubMed] [Google Scholar]