Abstract
Purpose
To translate and assess the reliability and validity of a Chinese version of the Physical Activity Scale for the Elderly (PASE).
Methods
Participants included Chinese individuals >65 living in the community or assistive living facilities. At baseline, 73 subjects completed the translated PASE, and Chinese versions of 3 other scales to evaluate validity; the Timed-Up and Go (TUG), the Older American Resources Services Activities of Daily Living (OARS ADL), and the Activities Balance Confidence Scale (ABC). At follow-up, 66 subjects completed the PASE and a questionnaire to determine if there were any changes in health over the retest period.
Results
The mean baseline PASE-C score was 76.0 (±49.1) at baseline and 78.33 (±50.27) at follow up. Correlations between the PASE-C and other variables were: age r= −0.51; TUG r= −0.52; OARS ADL r= 0.56 and ABC score r=0.62. The retest reliability was ICC= 0.79 (95% confidence interval 0.68–0.86).
Conclusion
Our results indicate that the PASE-C has acceptable reliability and there is support for validity in the older Chinese population.
Keywords: physical activity, Physical Activity Scale for Elderly (PASE), elderly, Chinese
Introduction
Physical inactivity is a preventable risk factor for many chronic diseases including cardiovascular disease,[1] certain types of cancer [2], type 2 diabetes [3,4,5,6], respiratory disease [7, 8] and osteoporosis [9, 10]. Conversely, increased physical activity is associated with, among others; a healthy body mass index (BMI), [11] better mental health [12,13] dynamic balance [14] and a decreased risk of falls [15]. Despite the obvious health benefits of physical activity, 63% of all Canadians are not sufficiently active to benefit their health [16] with 17% of those under the age of 64 being completely inactive compared to 29% of adults 65 and older [17]. Moreover, the physical inactivity declines sharply with age [18]. Although the mean life expectancy of Canadians is 84 years, a considerable decline in health is seen around age 65 [17], making preventable health concerns of particular importance in older adults. In fact, the majority of community dwelling older adults with chronic disease are physically able to engage in adequate levels of physical activity but do not do so, increasing their risk for further decline in health [19]. In a recent review by Bean et al. [20], the authors reported that exercise increased mortality while decreasing morbidity and had a beneficial effect for almost all older adults, especially those suffering from chronic disease. Therefore, it is both necessary and important to measure and record physical activity levels in the older adults.
Methods of assessing physical activity range from objective approaches, such as accelerometers, to subjective approaches featuring participant self-report measures. While objective measurements provide robust, accurate data reporting on targeted factors such as bouts of movement, contextual information about the physical activity is not captured. In contrast, self-report measures enable us to determine the type of activity (e.g. leisure, household or work), the perceived difficulty and, in some instances, estimate the amount of energy expenditure [21]. Being able to quantify data through the use of self-report enables a practical and low cost (including reduced participant burden) option to capture data at a population level [22]. In a recent systematic review of self-report physical activity questionnaires Williams et al [21] reported on the content and format of 104 questionnaires of which 35 were designed for use within the elderly population. Of these 35 questionnaires, 7 enabled estimation of the metabolic equivalent or energy cost and 2 were able to be self-administered (the Physical Activity Questionnaire and the Physical Activity Scale for the Elderly). However, the Physical Activity Questionnaire [23] has 55 questions, and the Physical Activity Scale for the Elderly has only 12 items which is an important consideration for reasons of participant burden.
The Physical Activity Scale for the Elderly (PASE) is a commonly used self-report measurement of physical activity that captures information on the frequency, duration and intensity of various activities. It can be completed in less than 5 minutes and has been validated in numerous studies [24–28]. The PASE has been used to measure physical activity levels in older adults who live in rural areas [29], to assess physical fitness levels in older adults in primary care settings [14] and to determine predictors of physical activity [11,12]. Originally developed in Britain [30], the PASE has been used in North America, the Netherlands [27] and Japan [28].
Physical activity among older Canadians has principally been studied in the English speaking population [12,17], yet Canada is largely made up of growing groups of minorities. The Chinese community is one of the largest visible minorities in Canada, and this is especially notable in Vancouver, where the Chinese community, including those from China and Taiwan, make up more than 25% of Vancouver’s population [31,32]. Even with such a large representation in the overall population, the Chinese-speaking subjects are often excluded from research. Moreover a clinical assessment of physical activity is difficult because of language barriers preventing clinicians from using standardized measures. This exclusion may result in decreased distribution of research and health benefits to this population. Currently, there is not a Chinese version of the PASE. The purpose of this study was to translate the PASE into Chinese and then assess the two week test retest reliability and validity of the translated version.
Methods
Translation
The original PASE was translated from English to Chinese using a forward-backward procedure. Translation and back-translation were conducted independently by two bilingual translators, both with training in the area of physical activity. Back-translation is a common practice to verify that translation was properly performed [33]. Both translators were Chinese immigrants who are able to read and write in Chinese and English. Discrepancies between their translations were resolved by discussion between the translators and a third party mediator.
Design and Subjects
The translated version of the PASE was assessed using a prospective two week test-retest design. Subjects who had emigrated from China and were currently living in Vancouver, BC, Canada were recruited. Specifically, individuals who lived independently in the community or assisted living centers were targeted. Community dwelling subjects were recruited through advertisements posted in public areas populated by the Chinese community such as community centers and churches, while individuals in assisted living environments were recruited through multi-level care facilities and assisted living centers. To be eligible subjects had to be; 65 years older; able to read Chinese; and had to have lived in Canada for at least five years. Individuals with a Mini-Mental State Examination score of <23 [34] and those with significant self-reported muscle, joint, or neurologic conditions such as stroke, or Parkinson’s disease were excluded.
A sample size of 40 was determined to be relevant using Donner and Eliasziw tables for intraclass correlation coefficient (ICC) of reliability [35]. By using a preselected alpha level (0.05) and beta (0.20) the sample size was determined to test the hypothesis of detecting a significant difference between a minimal standard and expected ICC. Previous reports of ICC values for the PASE have ranged from 0.65 [28] to 0.84 [30]. We set the minimum acceptable ICC = 0.70 and expected 0.80. For validity we anticipated correlations of r ≥ 0.5 u’. Using a significance level of p < 0.05 and a β = 0.83 we determined a sample size of n=30 would be required [36].
Protocol
All tests were administered by trained research assistants fluent in Chinese (Cantonese and Mandarin). Testing of community-dwelling subjects occurred at a rehabilitation research laboratory or at a community center the subject frequented. Assisted living subjects were assessed at their care facility.
Data were collected during two visits approximately two weeks apart (baseline and follow-up). Baseline data collection included subject demographics (age, sex, marital status, education, number of years living in Canada) and presence of co-morbid conditions. To test for validity, subjects also completed the; Timed Up and Go (TUG) [37], Older American Resource and Services activities of daily living (OARS ADL) [38], and the Activities-specific Balance Confidence Scale (ABC) [39]. Subjects were then asked to complete the Chinese version of the PASE (PASE-C). At follow-up, the subjects completed the PASE-C as well as a questionnaire to determine if they had experienced a change in health status over the two past weeks. This study was approved by the Behavioural Research Ethics Board at the local university.
Measurements
PASE
The PASE is a short self-report measure of short-term activity in the elderly. The PASE items do not emphasize high intensity sports or recreation, but rather low intensity activities such as gardening, walking outdoors or performing light housework. The PASE is separated into two parts; the first part known as the ‘Leisure Time Activity’ has six questions that ask individuals to estimate their involvement in daily activities such as participating in light exercise during the past 7 days. Individuals respond “never”, “rarely”, “sometimes”, or “often.” Information regarding the type of activity performed and an average time spent on the activity per day is also recorded. These six questions are used to calculate the number of hours that are spent in each activity per day, over a 7-day period. The second part known as the ‘Household Activity’ has three questions that use a “yes” or “no” response format and ask about involvement in daily chores such as washing dishes or gardening over the past week. The final question asks about participation in paid or volunteer work, and the hours and type of work involved. To calculate a total score, the PASE items are weighted using values determined by the original authors [25].
The overall PASE score is computed by multiplying the amount of time spent (hours/day over a seven day period) and participation (yes or no) by the PASE weight value, and then summing each contribution for a total score. The PASE scores range from 0 to 500 or more where higher scores represent higher physical activity levels. The English version of the PASE was found to have good test-retest reliability (ICC = 0.84) [30] and significant correlations with measures of physical activity [25].
Activities-specific Balance Confidence Scale (ABC)
The ABC is a 16 item self-report tool that measures confidence with balance while performing a variety of different functional tasks. Each item on the ABC is scored between 0 (no confidence) and 100 (complete confidence) and total scores are derived by calculating the mean. Higher scores indicate greater balance confidence [39]. Both the English and Chinese versions have been found to have high reliability (ICC = 0.96 and ICC = 0.87 respectively) [39,40] and correlate well (r = 0.75) with a functional assessment of balance, the Berg Balance Scale [41].
Timed-Up-and-Go (TUG)
The TUG is a functional assessment of balance and mobility that tests a subject’s ability to stand up from a chair, walk a short distance and then sit back down. Times to the nearest tenth of a second are recorded. Times of greater than 30 seconds have been shown to predict subjects who are at risk of falling [37]. The measurement properties of the TUG have been investigated in numerous studies. As an example, it was found to have a strong correlation (r = −0.81) with the Berg Balance Scale [42], and excellent test retest reliability of ICC [2,1] = 0.97 in community dwelling older adults [43]. The Chinese version of the TUG was found to have excellent interrater reliability (r ≥ 0.93) and validity among Chinese population [44].
Older American Resource and Services – Activities of Daily Living Scale (OARS ADL)
The OARS ADL and IADL is a self-report measure of the subject’s ability to perform physical (e.g. feeding, dressing, grooming) and instrumental activities of daily living (e.g. using a telephone, shopping) [45]. The ADL and IADL section comprises of items 56–69 in the full OARS assessment. Each item is scored as either 1 (inability) or 0 (independent) and all item scores can be summed for an overall score (0–14) with low scores on the OARS ADL indicating higher levels of independence and ability. The OARS ADL has been found to be a reliable (r = 0.96) [46] and valid measure of independence in the elderly [38,46]. The Chinese version of the OARS ADL has been found to have excellent interrater reliability (r ≥ 0.93) and validity among Chinese populations [44].
Data Analysis
Summary statistics were used to describe the characteristics of the sample and the PASE-C scores, as well as to provide insight as to whether certain statistical assumptions (e.g. normal distribution) were violated. PASE-C score parameters were reported as per the format of the original scale development [30]: i) the frequency of hours per day engaged in the activity, and ii) the percentage of subjects engaging in the activity during the 7 days.
We hypothesized that individuals living in assisted living groups would report overall lower PASE-C total scores than individuals who were married and/or living in the community. We also hypothesized that individuals who had not completed a high school education would report lower PASE-C scores than their counterparts. We did not expect to see a large significant difference between PASE-C scores for men and women [28]. These differences were assessed using the independent t-test with 95% confidence intervals. Floor and ceiling effects were operationalized as being less than or greater than 20% of the population expected to score at the end ranges of PASE-C scores [47].
Additional support for validity was evaluated using the Pearson product-moment coefficient of correlation between PASE-C scores and the TUG, OARS ADL, age, and the ABC. Correlations were hypothesized to be of a moderate (r ≥ 0.5) magnitude with positive correlations expected between the PASE-C and the ABC and OARS ADL and negative correlations with age and TUG times.
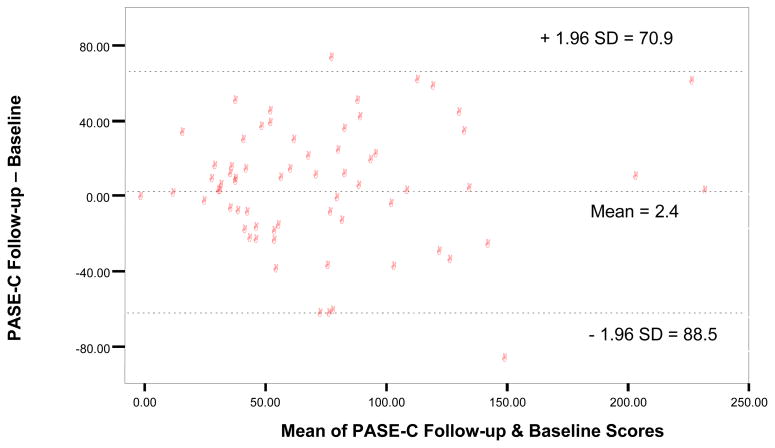
Retest reliability of the PASE was calculated using intraclass correlation coefficient (ICC1,k). Intraclass correlation coefficients above 0.75 are indicative of good reliability [36]. We hypothesized the ICC to be high (> 0.80) based on the reported range of ICC’s in the literature [25,30,48]. Item consistency was measured using a linear weighted, chance corrected, kappa (κw) and were performed using Analyse-it Software (Method Evaluation Edition, Analyse-it Software, Ltd., Leeds, England). A linear weighted kappa score was chosen because the response categories were ordinal and the differences between categories on the PASE were considered to be equal [49]. Higher κw scores (closer to 1) indicate greater agreement between scores [36]. Kappa scores were calculated using the four categories of response for items 1–6 (never, seldom, sometimes, or often) and two categories of responses for items 7–12 (yes or no). Kappa values from 0.00–0.20 are considered ‘slight’, 0.21–0.40 are ‘fair’, 0.41–0.60 are ‘moderate’, 0.61–0.80 are ‘substantial’, and 0.80–1.00 are ‘almost perfect’ [50]. Bland and Altman plots were derived in order to provide a visual representation of the level of agreement of PASE scores between the two testing sessions and to assess bias in the measure [51] particularly with respect to ceiling and floor effects.
The Standard Error of Measurement (SEM) and Minimal Detectable Difference based on the 95% confidence interval of the SEM multiplied by a correction factor were calculated to provide an indication where real change beyond measurement error, for group and individual values respectively, were also calculated [36].
Significance level was set at p < 0.05. All validity statistics were calculated using SPSS version 11.5.
Results
Demographics and PASE-C Scores
Seventy-three individuals were enrolled and provided baseline data, however, seven of these individuals were lost to follow-up. The majority of the group were women (71%) and the mean age of the group was 79.0 (± 8.5) years. The baseline mean group PASE-C score was 76.0 (± 49.1) and the group mean at follow-up was 78.33 (± 50.27) (table 1).
Table 1.
Demographic and mean differences in the PASE-C scores
| Sample Characteristics | N | Mean PASE-C (±SD) | t | 95% Confidence Intervals | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Sex | |||||
| Males | 19 | 94.20 (59.74) | 1.96 | −0.5 | 51.7 |
| Females | 47 | 68.62 (42.67) | |||
|
| |||||
| Living Environment | |||||
| Assisted Living | 34 | 50.54 (26.00) | −5.11 | −73.0 | −32.0 |
| Community Living | 32 | 103.03 (53.63) | |||
|
| |||||
| Marital Status | |||||
| Married | 26 | 102.15 (59.39) | −3.84 | −65.6 | −20.7 |
| Single/Widowed | 40 | 58.98 (31.75) | |||
|
| |||||
| Education | |||||
| < high school | 27 | 59.78 (34.99) | −2.30 | −51.22 | −3.63 |
| ≥ High school | 39 | 87.21 (54.53) | |||
t = t value from test of mean difference
SD = standard deviation
The most common Leisure Time Activity was walking outdoors (0.83 h/day) while only 0.02 h/day were spent on average in strenuous activity (table 2). The most participated Household Activity was light housework (91%) in contrast to only 4.5% participation in home repairs.
Table 2.
Frequency of the PASE-C items by sex, residential status and Kappa values for each PASE-C item
| PASE component | Frequency Total | Men | Women | Assisted Living | Community Living | No of categories | Kappa |
|---|---|---|---|---|---|---|---|
| Leisure time activity (h/day) | |||||||
| Walking outside home | 0.83 | 1.17 | 0.7 | 0.5 | 1.2 | 4 | 0.45 |
| Light sports and recreational activities | 0.35 | 0.53 | 0.28 | 0.3 | 0.4 | 4 | 0.33 |
| Moderate sports and recreational activities | 0.33 | 0.64 | 0.21 | 0.0 | 0.7 | 4 | 0.51 |
| Strenuous sports and recreational activities | 0.02 | 0.03 | 0.01 | 0.0 | 0.0 | 4 | 0.65 |
| Muscle strength/endurance exercise | 0.07 | 0.06 | 0.07 | 0.1 | 0.0 | 4 | 0.43 |
| Household activity (%) | |||||||
| Light housework | 90.9 | 73.7 | 97.9 | 94.1 | 87.5 | 2 | 0.78 |
| Heavy housework or chores | 28.8 | 36.8 | 25.5 | 2.9 | 56.3 | 2 | 0.64 |
| Home repairs | 4.5 | 15.8 | 0.0 | 2.9 | 6.3 | 2 | 0.39 |
| Lawn work or yard care | 9.1 | 15.8 | 6.4 | 0 | 18. 8 | 2 | 0.17 |
| Outdoor gardening | 6.1 | 10.5 | 4.3 | 0 | 12.5 | 2 | 0.85 |
| Caring for another person | 19.7 | 21.1 | 19.1 | 14.7 | 25.0 | 2 | 0.62 |
| Work-related activity | |||||||
| Work for pay or as a volunteer (h/day) | 0.16 | 0.68 | 0.20 | 0.7 | 0.5 | 2 | 0.92 |
Validity
The PASE-C scores were significantly (p = 0.001) higher for the community living group and subjects who were married. Although men had higher PASE-C scores as expected the difference was not statistically significant. PASE-C baseline scores correlated as hypothesized with age, activities of daily living (OARS ADL), TUG time and total ABC score. The correlations with the PASE-C and the validity measures were of the estimated magnitude and in the hypothesized direction. The specific correlations (all p < 0.0001) with the PASE-C scores were: age r = −0.51; TUG time r = −0.52; OARS ADL r = 0.56 and ABC score r = 0.62.
Reliability
The two week retest reliability of the PASE-C (n=66) was ICC = 0.79 (95% confidence interval 0.68–0.86). The SEM and MDD95 were 22.77 and 63.11 respectively. The spread along the continuum of the zero line in the Bland and Altman (figure 1) plot is relatively good with PASE-C scores ranging between 0 and 150, although there were a handful of individuals who were noted to be quite active. Eight percent of individuals scored <20 and no one in our sample recorded a score near the PASE maximum suggesting no or minimal floor or ceiling effect [47]. The Bland and Altman plot shows nearly equal distribution above and below the zero line, however, 5 subjects were identified in the Bland and Altman plot as falling outside the 95% limits of agreement with 4 of the 5 outliers reporting decreased scores at follow-up. Two of the outliers reported a decline in health (insomnia and a cold) that corresponded with a decrease in physical activity over the retest period. The remaining 3 subjects did not have clear reason for their large changes (greater than 2 standard deviations) in PASE-C scores, which may be indicative of bias.
Figure 1.
Difference versus Mean (Limits of Agreement Plot) of PASE-C Data (N=66)
Finally, table 2 shows kappa (κ) values and proportion of consistency for each item on the PASE. Kappa values below 0.40 were seen for three items (light sports and recreation, home repairs and lawn work). Values were seen as high as κ = 0.85 for the item ‘outdoor gardening’ and κ = 0.92 for ‘work for pay or as a volunteer’.
Discussion
Mean score and contributing demographic factors
The mean score for the PASE-C in our sample was below reported PASE-C scores in other elderly populations such as the Japanese [28], Americans [14] and Canadians living in Saskatoon [12], but our values were relatively close to those reported for the Dutch population [27]. It is difficult to determine if the low PASE-C scores reflects a sedentary lifestyle among the elderly Chinese populations residing in Vancouver, or if the differences are more related to study group demographics that affect physical activity such as older age, decreased income, and education level [17]. In particular, the lower education level (40.9% less than high school education) and the inclusion of assistive living subjects in our sample may have contributed to the low mean PASE-C score we observed. The PASE-C scores did not significantly differ between men and women, as supported by other studies [27,28]. This may reflect the balance of gender typical activities on the PASE-C. Typically female activities, such as light housework and caring for others are balanced with more male typical roles such as home repairs and strenuous exercise. Consistent with the findings by the other studies, the majority of activities engaged in were of low intensity, such as walking outside and light housework [25,28,52].
The distribution of the scores indicates there is no floor or ceiling effects for the PASE-C in our sample [47]. Although floor effects (scores of 0) are possible, the range of items makes this unlikely. Moreover, because PASE-C scores can exceed 500, a ceiling effect is unlikely, even for highly active individuals [18].
Effect of living environment, marital status and education on PASE-C score
PASE-C scores correlated as expected based on our hypotheses. The correlations indicated that as age increases activity levels decrease, [53–55] individuals who are more independent with their activities of daily living (often suggestive of being less disabled) are also more physically active, and individuals who have reduced mobility are less physically active. Finally, individuals who are more confident with performing activities that challenge their balance are also more physically active. Moreover individuals living in assisted care centers were significantly less active than individuals living in the community. This finding is logical given that these individuals are not responsible for activities such as yard work, heavy housework, home repairs and/or caring for others and they tend to be more frail [55] in comparison to their community dwelling counterparts, thereby limiting their physical activity as indicated by their PASE-C scores.
Individuals who were married were significantly more active than those who were widowed or single. Married individuals were also more likely to live in the community, and are a more active and younger group in general. It is likely that a combination of factors, including social support [17,56,57], is contributing to the higher activities levels of this group. There is substantial literature linking low education levels to lower levels of physical activity and higher levels of obesity [57–60]. We also found that individuals with less than a high school education were significantly less active, potentially because of limited knowledge of the health benefits of physical activity.
Reliability scores
The overall score of the PASE-C is subject to fluctuations due to the short recall period of one week and the inclusion of items that are subject to weather conditions (outdoor gardening) or not performed regularly (lawn care or yard work) which may have contributed to the variation in items. Items with lower κ coefficients tended to be activities that were not done on a weekly, or even biweekly bases such as lawn work or yard care. These are also items in which the assisted living individuals would not have the opportunity or need to participate (heavy housework or laundry). Items with higher kappa values included those that were frequently performed, such as light housework or items that very few individuals reported participating in, such as outdoor gardening, home repairs or work or volunteering. These kappa results are similar to the results obtained when the PASE was translated into Japanese [28].
The PASE-C had good test-retest reliability [36] overall and fell between the reliability correlation Washburn and colleagues [30] reported for their postal (r=0.84) and telephone (r=0.68) samples in the original study of the PASE and was superior to the value reported by Hagiwara et al. [28] in their Japanese translation study (ICC = 0.65). One potential reason for the variation in coefficients is the retest period which was much shorter for our sample than that of either the 3–7 weeks for the Washburn study or 3–4 weeks in the Hagiwara study. The stronger correlation for Washburn’s postal group may reflect additional time reflecting on responses without the pressure or presence of a researcher whether in person or over the telephone. Alternatively the use of a Pearson’s correlation coefficient for retest reliability has been reported to be prone to systematic error [33, 36].
The five subjects falling outside the LOA on the Bland and Altman plot (figure 1) represents a reporting bias, with the tendency for PASE-C scores to decrease over the retest period. It is plausible that this bias may have been due to external factors such as weather, which could have interfered with opportunities for outside activity or alternatively there could have been a change in health status. In fact one of the outliers reporting having significant low back pain over the retest period while another indicated that they had a cold. These conditions were deemed sufficient to alter activity over the retest period and therefore may explain the different scores. If this is the case it would seem that the bias between test and retest in our sample is minimal.
Limitations
The results need to be considered with the following limitations in mind. A convenience sample of Chinese immigrants was used, and it may be possible that different results would have been obtained if a random sample of all eligible subjects in the Chinese population had been recruited. Obvious limitations to generalizability of the results include our exclusion of individuals with cognitive impairment and mobility issues related to muscle, joint, or neurologic conditions.
The PASE-C itself has possible limitations as well. Self-report measures are prone to overestimation or underestimation of the true energy expenditure related to activity [61]. Contributing to this is that participants may display social desirability bias and therefore report higher levels of household activities. Additionally, despite the short frame of reference (7 days) issues with recall resulting from early or advanced cognitive/memory limitation may generate a score that is not accurate for an individual’s regular activity level. Ultimately if the goal is to minimize measurement error related to these issues then objective measures should be used to provide a more precise and accurate estimate of the absolute level of activity. However objective measures also have limitations related to participant burden, cost and loss of contextual information. It is encouraging to note that previous findings have noted a moderate correlation between PASE and accelerometer data (r = 0.64) providing some objective validity for the PASE self-report data [26]. Finally, it seems plausible that there is a cultural bias present with some of the PASE-C items, and therefore they may not be sensitive and reflective of values related to the Chinese population. For instance some of the examples used to describe leisure time activities (i.e. shuffleboard) are likely to be unknown to individuals living in mainland China. Similarly examples of items on the PASE regarding work and household related activities (i.e. lumberjack and carrying wood) may not resonate with older adults in assisted living centers.
In conclusion, this study presents data of the translation and validation of the measurement properties of a Chinese version of the PASE. The results obtained in this study indicate that the PASE-C is a valid and reliable measure suitable for use among the elderly Chinese population. The evolution of this tool will enable clinicians and researchers alike to capture physical activity data from an important population that has largely been overlooked to date.
Acknowledgments
This study was supported by an operating grant from the Canadian Institutes of Health Research (CIHR 72159). The authors would also like to express their gratitude to the persons who participated in this study.
References
- 1.Berlin JA, Colditz GA. A meta-analysis of physical activity in the prevention of coronary heart disease. Am J Epidemiol. 1990;132:612–28. doi: 10.1093/oxfordjournals.aje.a115704. [DOI] [PubMed] [Google Scholar]
- 2.Shephard RJ, Futcher R. Physical activity and cancer: How may protection be maximized? [review] Crit Rev Oncog. 1997;8:219–72. doi: 10.1615/critrevoncog.v8.i2-3.40. [DOI] [PubMed] [Google Scholar]
- 3.Haapanen N, Miilunpalo S, Vuori I, Oja P, Pasanen M. Association of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in middle-aged men and women. Int J Epidemiol. 1997;26:739–47. doi: 10.1093/ije/26.4.739. [DOI] [PubMed] [Google Scholar]
- 4.Hu FB, Sigal RJ, Rich-Edwards JW, Colditz GA, Solomon CG, Willett WC, et al. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. JAMA. 1999;282:1433–9. doi: 10.1001/jama.282.15.1433. [DOI] [PubMed] [Google Scholar]
- 5.Manson JE, Rimm EB, Stampfer MJ, Colditz GA, Willett WC, Krolewsk AS, et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet. 1991;338:774–8. doi: 10.1016/0140-6736(91)90664-b. [DOI] [PubMed] [Google Scholar]
- 6.Manson JE, Nathan DM, Krolewski AS, Stampfer MJ, Willett WC, Hennekens CH. A prospective study of exercise and incidence of diabetes among US male physicians. JAMA. 1992;268:63–7. [PubMed] [Google Scholar]
- 7.Lacasse Yves, Wong Eric, Guyatt Gordon H, King Derek, Cook Deborah J, Goldstein Roger S. Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease. Lancet. 1996;348:1115–9. doi: 10.1016/S0140-6736(96)04201-8. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Anto JM. Regular Physical Activity Modifies Smoking-related Lung Function Decline and Reduces Risk of Chronic Obstructive Pulmonary Disease: A Population-based Cohort Study. Am J Respir Crit Care Med. 2007;175:458–463. doi: 10.1164/rccm.200607-896OC. [DOI] [PubMed] [Google Scholar]
- 9.Farmer ME, Harris T, Madans JH, Wallace RB, Cornoni-Huntley J, White LR. Anthropometric indicators and hip fracture. The NHANES I Epidemiologic Follow-up Study. J Am Geriatr Soc. 1989;37:9–16. doi: 10.1111/j.1532-5415.1989.tb01562.x. [DOI] [PubMed] [Google Scholar]
- 10.Gregg EW, Cauley JA, Seeley DG, Ensrud KE, Bauer DC. Physical activity and osteoporotic fracture risk in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1998;129:81–8. doi: 10.7326/0003-4819-129-2-199807150-00002. [DOI] [PubMed] [Google Scholar]
- 11.Kvamme JM, Wilsgaard T, Florholmen J, Jacobsen BK. Body mass index and disease burden in elderly men and women: the Tromso Study. Eur J Epidemiol. 2010;25:183–193. doi: 10.1007/s10654-009-9422-z. [DOI] [PubMed] [Google Scholar]
- 12.Chad KE, Reeder BA, Harrison EL, Ashworth NL, Sheppard SM, Schultz SL, et al. Profile of physical activity levels in community-dwelling older adults. Med Sci Sport Exer. 2005;37:1774–1784. doi: 10.1249/01.mss.0000181303.51937.9c. [DOI] [PubMed] [Google Scholar]
- 13.Parker SJ, Strath SJ, Swartz AM. Physical activity measurement in older adults: relationships with mental health. J Aging Phys Activ. 2008;16:369–380. doi: 10.1123/japa.16.4.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Purath J, Buchholz SW, Kark DL. Physical fitness assessment of older adults in the primary care setting. J Am Acad Nurse Pract. 2009;21:101–107. doi: 10.1111/j.1745-7599.2008.00391.x. [DOI] [PubMed] [Google Scholar]
- 15.Ganz DA, Alkema GE, Wu S. It takes a village to prevent falls: reconceptualizing fall prevention and management for older adults. Inj Prev. 2008;14:266–271. doi: 10.1136/ip.2008.018549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The Secretariat for the Intersectoral Healthy Living Network. [Accessed on July 20, 2011.];The Integrated Pan-Canadian Healthy Living Strategy [monograph on the Internet]; 2005 Available from: http://www.phac-aspc.gc.ca/hl-vs-strat/pdf/hls_e.pdf.
- 17.Shields M, Martel L. Healthy Living among Seniors. [Accessed on April 10, 2012.];Supplement to Health Reports Statistics Canada, Catalogue 82-003. 2004 16:7–20. Available from: http://www.statcan.gc.ca/pub/82-003-s/2005000/pdf/9086-eng.pdf. [PubMed] [Google Scholar]
- 18.Stephens T, Jacobs DR, Jr, White CC. A descriptive epidemiology of leisure-time physical activity. Public Health Rep. 1985;100:147–158. [PMC free article] [PubMed] [Google Scholar]
- 19.Ashe M, Eng J, Miller W, Soon J. Disparity between physical capacity and participation in seniors with chronic disease. Med Sci Sport Exer. 2007;39:1139–1146. doi: 10.1249/mss.0b013e31804d2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bean JF, Vora A, Frontera WR. Benefits of exercise for community-dwelling older adults. Arch Phys Med Rehabil. 2004;85:S31–42. doi: 10.1016/j.apmr.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Williams K, Frie A, Vetsch A, Dobbels F, Puhan MA, Rudell K. Patient-reported physical activity questionnaires: A systematic review of content and format. [Accessed 2012 Apr 01];Health and Qual Life Out. 2012 10:28. doi: 10.1186/1477-7525-10-28. http://www.hqlo.com/content/pdf/1477-7525-10-28.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dishman RK, Washburn RA, Schoeller DA. Measurement of physical activity. QUEST. 2001;53:295–309. [Google Scholar]
- 23.Liu B, Woo J, Tang N, Ng K, Ip R, Yu A. Assessment of total energy expenditure in a Chinese population by a physical activity questionnaire: examination of validity. Int J Food Sci Nutr. 2001;52:269–282. doi: 10.1080/09637480120044138. [DOI] [PubMed] [Google Scholar]
- 24.Dinger MK, Oman RF, Taylor EL, Vesely SK, Able J. Stability and convergent validity of the Physical Activity Scale for the Elderly (PASE) J Sports Med Phys Fitness. 2004;44:186–192. [PubMed] [Google Scholar]
- 25.Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA. The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 26.Washburn RA, Ficker JL. Physical Activity Scale for the Elderly (PASE): the relationship with activity measured by a portable accelerometer. J Sport Med Phys Fit. 1999;39:336–340. [PubMed] [Google Scholar]
- 27.Schuit AJ, Schouten EG, Westerterp KR, Saris WH. Validity of the Physical Activity Scale for the Elderly (PASE): according to energy expenditure assessed by the doubly labeled water method. J Clin Epidemiol. 1997;50:541–546. doi: 10.1016/s0895-4356(97)00010-3. [DOI] [PubMed] [Google Scholar]
- 28.Hagiwara A, Ito N, Sawai K, Kazuma K. Validity and reliability of the Physical Activity Scale for the Elderly (PASE) in Japanese elderly people. Geriatr Gerontol Int. 2008;8:143–151. doi: 10.1111/j.1447-0594.2008.00463.x. [DOI] [PubMed] [Google Scholar]
- 29.Allison MJ, Keller C, Hutchinson PL. Selection of an instrument to measure the physical activity of elderly people in rural areas. Rehabil Nurs. 1998;23:309–314. doi: 10.1002/j.2048-7940.1998.tb01811.x. [DOI] [PubMed] [Google Scholar]
- 30.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 31.Statistics Canada [database on the internet] Visible minority population, by province and territories. :c2006. [cited 2010 July 19]. Available at: http://www40.statcan.ca/l01/cst01/demo52a-eng.htm.
- 32.Statistics Canada [database on the internet] Visible minority population, by census metropolitan area. :c2006. [cited 2010 July 19] Available at: http://www40.statcan.ca/l01/cst01/demo53g-eng.htm.
- 33.Streiner DL, Norman GN. Health Management Scales: a practical guide to their development and use. United States: Oxford Medical Publications; 2003. [Google Scholar]
- 34.Katzman R, Zhang MY, Ouang-Ya-Qu, et al. A Chinese version of the Mini-Mental State Examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol. 1988;41:971–8. doi: 10.1016/0895-4356(88)90034-0. [DOI] [PubMed] [Google Scholar]
- 35.Donner A, Eliasziw M. Sample size requirements for reliability studies. Stat Med. 1987;6:441–448. doi: 10.1002/sim.4780060404. [DOI] [PubMed] [Google Scholar]
- 36.Portney L, Watkins M. Applications to practice. 2. New Jersey: Prentice Hall Health; 2000. Foundation of clinical research. [Google Scholar]
- 37.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 38.Doble SE, Fisher AG. The dimensionality and validity of the Older Americans Resources and Services (OARS) Activities of Daily Living (ADL) Scale. J Outcome Meas. 1998;2:4–24. [PubMed] [Google Scholar]
- 39.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 40.Hsu PC, Miller WC. Reliability of the Chinese version of the Activities-specific Balance Confidence Scale. Disabil Rehabil. 2006;28:1287–1292. doi: 10.1080/09638280600638414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hatch J, Gill-Body KM, Portney LG. Determinants of balance confidence in community-dwelling elderly people. Phys Ther. 2003;83:1072–1079. [PubMed] [Google Scholar]
- 42.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67:387–389. [PubMed] [Google Scholar]
- 43.Steffen TM, Hacker TA, Mollinger L. Age-and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed up and Go Test, and gait speed. Phys Ther. 2002;82:128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 44.Lin MR, Hwang HF, Hu MH, Wu HD, Wang YW, Huang FC. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004;52:1343–1348. doi: 10.1111/j.1532-5415.2004.52366.x. [DOI] [PubMed] [Google Scholar]
- 45.Fillenbaum GG, Smyer MA. The development, validity and reliability of the OARS multidimensional functional assessment questionnaire. J Genontol. 1981;35(4):428–434. doi: 10.1093/geronj/36.4.428. [DOI] [PubMed] [Google Scholar]
- 46.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 47.Andresen E. Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil. 2000;81(Suppl 2):15–20. doi: 10.1053/apmr.2000.20619. [DOI] [PubMed] [Google Scholar]
- 48.Nakano K. Perfectionism, self-efficacy, and depression: preliminary analysis of the Japanese version of the Almost Perfect Scale-Revised. Psychol Rep. 2009;104:896–908. doi: 10.2466/PR0.104.3.896-908. [DOI] [PubMed] [Google Scholar]
- 49.Cohen J. Weighted kappa: nominal scale agreement provision for scaled disagreement or partial credit. Psychol Bull. 1968;70:213–220. doi: 10.1037/h0026256. [DOI] [PubMed] [Google Scholar]
- 50.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 51.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 52.Washburn RA. Assessment of physical activity in older adults. Res Q Exerc Sport. 2000;71(2 Suppl):S79–88. [PubMed] [Google Scholar]
- 53.Bauman A, Bull F, Chey T, Craig CL, Ainsworth BE, Sallis JF, Bowles HR, Hagstromer M, Sjostrom M, Pratt M and The IPS Group. The International Prevalence Study on Physical Activity: results from 20 countries. [Accessed 2012 Apr 10];Int J Behav Nutr Phy. 2009 6:21. doi: 10.1186/1479-5868-6-21. http://www.ijbnpa.org/content/6/1/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guthold R, Ono T, Kathleen L, Strong KL, Chatterji S, Morabia A. Worldwide Variability in Physical Inactivity: A 51-Country Survey. A J Prev Med. 2008;34:486–494. doi: 10.1016/j.amepre.2008.02.013. [DOI] [PubMed] [Google Scholar]
- 55.Horgas AL, Wilms H, Baltes MM. Daily Life in Very Old Age: Everyday Activities as Expression of Successful Living. The Gerontologist. 1998;38:556–568. doi: 10.1093/geront/38.5.556. [DOI] [PubMed] [Google Scholar]
- 56.Bopp M, Wilcox S, Laken M, McClorin L. Physical activity participation in African American churches. J Cult Divers. 2009;16:26–31. [PubMed] [Google Scholar]
- 57.Tse MM. Therapeutic effects of an indoor gardening programme for older people living in nursing homes. J Clin Nurs. 2010;19:949–958. doi: 10.1111/j.1365-2702.2009.02803.x. [DOI] [PubMed] [Google Scholar]
- 58.Hurkmans EJ, Maes S, de Gucht V, Knittle K, Peeters AJ, Ronday HK, et al. Motivation as a determinant of physical activity in patients with rheumatoid arthritis. Arthritis Care Res. 2010;62:371–377. doi: 10.1002/acr.20106. [DOI] [PubMed] [Google Scholar]
- 59.Strandhagen E, Berg C, Lissner L, Nunez L, Rosengren A, Toren K, et al. Selection bias in a population survey with registry linkage: potential effect on socioeconomic gradient in cardiovascular risk. Eur J Epidemiol. 2010;25:163–172. doi: 10.1007/s10654-010-9427-7. [DOI] [PubMed] [Google Scholar]
- 60.Kvamme JM, Wilsgaard T, Florholmen J, Jacobsen BK. Body mass index and disease burden in elderly men and women: the Tromso Study. Eur J Epidemiol. 2010;25:183–193. doi: 10.1007/s10654-009-9422-z. [DOI] [PubMed] [Google Scholar]
- 61.Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. [Accessed 2012 Apr 04];Int J Behav Nutr Phys Act. 2008 5:56. doi: 10.1186/1479-5868-5-56. http://www.ijbnpa.org/content/5/1/56. [DOI] [PMC free article] [PubMed] [Google Scholar]