Health disparities prevail in the population of children and adolescents in foster care. Given their high rates of all health problems, including physical, mental health, and developmental, they are widely viewed to be one of the most vulnerable groups in the United States (US) (American Academy of Pediatrics (AAP), 2005; Ringeisen, Casanueva, Urato, & Cross, 2008; Simms, Dubowitz, & Szilagyi, 2000). Adolescents represent nearly half of those in foster care, and yet, little is known about health specific to this developmental age group, in particular, which adolescents experience poor health. The purpose of this paper is to describe the health profiles of adolescents in foster care. Data from the Foster Youth Health Project (Kools, Paul, Norbeck, & Robbins, 2009), a study of an intervention to improve health and developmental outcomes of adolescents in foster care, was used to systematically cluster adolescents into 13 mutually exclusive health profiles and then, to rank specific groups along a continuum of health from best to worst health status. The development of health profiles allows a systematic characterization of health patterns which can be useful for planning health services and policy.
Background and Significance
Of the 500,000 children in foster care in the US today, 46% are adolescents, aged 11–20 (Adoption and Foster Care Analysis and Reporting System, 2010). They are removed from their family homes for a variety of reasons, including abuse, neglect, abandonment, parental substance use and mental illness, and severe child behavioral problems (American Association of Child and Adolescent Psychiatry, 2006). Thirty-six percent remain in foster care for over 2 years and multiple foster home placements are commonplace, with children having an average of three and a range of 1–18 placements (Rubin, O’Reilly, Hafner, Xuan, & Localio, 2007). It has been well-documented that placement instability has a deleterious impact on health outcomes (Hardin, 2004; Mekonnen, Noonan, & Rubin, 2009; Newton, Litrownik, & Landsverk, 2000).
The overrepresentation of health problems in the foster care population has been substantiated over the last three decades (Chernoff, Combs-Orme, Risley-Curtiss, & Heisler, 1994; Clausen, Landsverk, Ganger, Chadwick, & Litrownik, 1998; Klee & Halfon, 1987; Schor, 1982; Simms, Dubowitz, & Szilagyi, 2000). The National Survey of Child and Adolescent Well-Being (NSCAW) has systematically studied the health needs of children in the child welfare system (Administration for Children and Families, 2003, 2005). In a representative NSCAW subsample of children in long term foster care (N=727), Jee and colleagues (2006) found that 30% had one or more chronic conditions and 52% had at least one mental health problem. The US Government Accountability Office (2009) reported 80% of children in foster care have significant physical health, mental health, and/or developmental needs and the AAP (2005) designated this population as children with special health care needs. Until recently, however, adolescents have been a part of the aggregate of children in foster care health research.
Researchers note that the overall health problems that children in foster care experience persist into adolescence. Health conditions increase and often worsen with length of stay and number of placements (Newton, Litrownik, & Landsverk, 2000; Rubin et al., 2007). Further, adolescent-specific health concerns are thought to be common in these adolescents, including negative risk taking, depression, and more severe levels of conduct disorders (Farruggia & Sorkin, 2009). Nearly half of adolescents in the child welfare system, including those in foster care placements, report at least one health risk behavior in the areas of substance use, risky sexual behavior, depression and suicidality, and delinquency (Leslie et al., 2010). While risk taking in adolescence is normative, risky behaviors tend to begin earlier and are more frequent and serious in adolescents in foster care (Farruggia & Sorkin, 2009). For example, foster care placement is associated with earlier sexual debut, earlier age of first pregnancy, and a greater number of sexual partners (Carpenter, Clyman, Davidson, & Steiner, 2001; Taussig, 2002). Likewise, rates of substance use and abuse are higher in foster care, especially in youth with conduct disorders (Vaughn, Ollie, McMillen, Scott, & Munson, 2007).
The Foster Youth Health Project (FYHP) was a longitudinal study, testing the effectiveness of a nursing intervention on the health outcomes of adolescents (ages 11–18) in foster care (Kools et al., 2009). Adolescents (N=136) and their newly assigned Court Appointed Special Advocates (CASAs) were randomized into treatment and control groups. The CASA is a community volunteer who develops a long-term relationship with a child or adolescent in foster care and advocates for the child’s needs while in placement, including placement appropriateness, stability, and safety. Most have little background or training in foster care health. Advanced practice nurses with expertise in adolescent health met with CASAs in the treatment group for a one-to-one bimonthly intensive consultation session about the health needs of their foster youth for a year. The purpose of the consultation sessions was twofold: to improve the individual CASA’s understanding of the adolescent’s health and to increase health targeted advocacy. Nurse-CASA discussions were centered on identifying adolescent health risks and problems, developing a health management plan, supporting the CASA-foster youth relationship, and following up on the adolescent’s progress. CASAs in the control group met with their youth as per standard practice without the nursing consultation sessions. Baseline and outcome measures at one year were examined for adolescents in both treatment and control groups, including measures of physical health, mental health, and social development.
One study measure of the FYHP was the Child Health and Illness Profile-Adolescent Edition (CHIP-AE), a multidomain measure of six dimensions of health. Adolescents from the total baseline sample reported higher rates of risk taking, including higher total risk behaviors and greater peer influence, as well as less resilience than adolescents in community populations. Girls had lower satisfaction with health and self-esteem and more physical and emotional discomfort than boys (Kools et al., 2009). These findings confirmed the awareness of higher risk taking in foster care, however, adolescent self-report of all health dimensions, in general, was much better than anticipated for this group, based on previous literature and qualitative data from this study. While we postulated several reasons for potential inflation of health status by this group (Kools et al., 2009), deeper analysis was needed to gain a more nuanced understanding of specific health vulnerabilities in this population. The taxonomy developed by Starfield, Riley and colleagues (Riley et al., 1998a; Starfield et al., 1993; Starfield et al. 1996), allowed us to examine the sample in a way that would avoid losing the distinctions of individual health data. Our outstanding question was: “Are there subgroups of adolescents within the sample who have particular health vulnerabilities based on profiles of health dimensions?” The use of the CHIP-AE Health Profiles allowed us to cluster and examine distinct groupings within the sample.
Methods
The FYHP had an experimental design and details of study methods are reported elsewhere (Kools et al., 2009). A subsequent, secondary health profile analysis was conducted for the purpose of this paper.
Participants
Participants included adolescents in foster care who were assigned to CASAs in three Northern California counties with urban and suburban populations. Adolescents were excluded from the study if they did not speak English or they had cognitive impairment, significant developmental delays, or major thought disorders. One adolescent was excluded as his first language was Vietnamese and he spoke little English and one was excluded as he was significantly developmentally delayed. The Committee on Human Research at the University of California, San Francisco, approved the study. A Judge (from the Family or Juvenile Court or Judicial Commission), as legal representative of the foster youth, gave consent and adolescents assented to study participation.
Measures
Data were collected on age, gender, and race/ethnicity, as well as the foster care variables of age at first placement, reason(s) for placement, length of time in foster care, number and types of placement.
For this paper, additional analyses were done on the CHIP-AE, a composite measure of health status with six domains (satisfaction with health, discomfort, disorders, risks, resilience, and achievement) and multiple subdomains within each domain. The CHIP-AE is an adolescent self-report instrument of subjective perceptions of the multidomain, complex nature of health: Satisfaction with health measures one’s perceptions of health and well-being, discomfort assesses physical and emotional sensations associated with health status, disorders are specific health conditions, risks are potential health-altering behaviors while resilience measures behaviors with potential to decrease likelihood of illness or injury, and achievement assesses one’s meeting of developmentally appropriate expectations (Riley et al., 1998a; Starfield et al., 1993; Starfield et al. 1996). The CHIP-AE is unique in that it does not have a parent or other proxy report, considering adolescents to be the optimal, most reliable reporters of their own health.
From the CHIP-AE, a taxonomy of adolescent health profiles was developed by Riley et al. (1998a), pairing hierarchical clustering with a conceptual approach using clinical and developmental experts. Using this taxonomy, it was thought that health patterns could be characterized as specific health profiles to guide interventions and service delivery for unique groups. The taxonomy was iteratively tested and refined with multiple, large and diverse samples of adolescents. Researchers garnered substantial evidence for the reliability, validity and applicability of the CHIP-AE across populations of young people, including community and clinic samples of varying age, race/ethnicity, and socioeconomic status (N>3200 over 10 years) (Starfield et al., 1995). Psychometric properties for the CHIP-AE have been documented to be good, including test-retest reliability (r=0.49–0.87), internal consistency (domain alphas 0.59–0.90) and criterion, convergent, and discriminant validity (Riley et al., 1998b; Starfield et al., 1995).
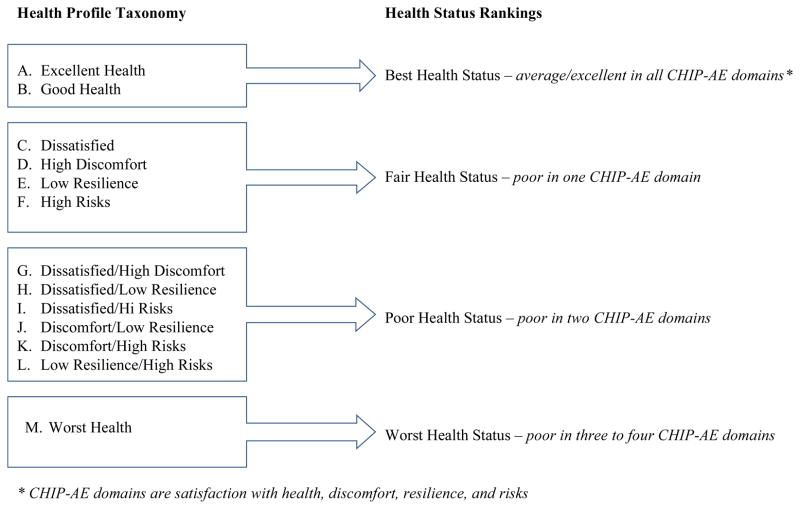
Four of the six CHIP-AE domains (satisfaction with health, risks, resilience, and discomfort) were used to generate 13 mutually exclusive, exhaustive health profiles (see Table 1). These four domains were thought to be most amenable to clinical intervention (Starfield et al. 1996).
Table 1.
Child Health and Illness Profile- Adolescent Edition, Health Profile Taxonomy
| Profile Type | Criteria | |
|---|---|---|
| A | Excellent health | Excellent health on three or four domains, with no domains of poor health |
| B | Good health | At least average on all domains, with excellent health on no more than 2 domains |
| C | Dissatisfied | Poor health on Satisfaction - score below 17 |
| D | High discomfort | Poor health on Discomfort - score above 23 |
| E | Low resilience | Poor health on Resilience - score below 17 |
| F | High risks | Poor health on Risks - score above 23 |
| G | Dissatisfied/high discomfort | Score below 17 on Satisfaction and above 23 on Discomfort |
| H | Dissatisfied/low resilience | Score below 17 on Satisfaction and Resilience |
| I | Dissatisfied/high risks | Score below 17 on Satisfaction and above 23 on Risks |
| J | Discomfort/low resilience | Score above 23 on Discomfort and below 17 on Resilience |
| K | Discomfort/high risks | Score above 23 on Discomfort and Risks |
| L | Low resilience/high risks | Score below 17 on Resilience and above 23 on Risks |
| M | Worst health | Poor health on three to four domains |
Domain scores indicating excellent health: Score above 23 on Satisfaction and Resilience and below 17 on Discomfort and Risks.
Domain scores indicating average health: Scores between 17 and 23 on any domain.
Domain scores indicating poor health: Scores above 23 on Discomfort and Risks and below 17 on Satisfaction and Resilience.
Note: From “A taxonomy of adolescent health: development of the adolescent health profile-types” by A.W. Riley et al., 1998, Medical Care, 36(8), p. 1232.
Analyses
Descriptive statistics, means and standard deviations for the continuous variables and frequencies and percents for the categorical variables, were calculated for all demographic and foster care placement variables.
According to the taxonomy, health profiles were derived based on previous scores on four of the CHIP-AE dimensions of health (satisfaction with health, risks, resilience, and discomfort) (Riley et al., 1998a; Starfield et al., 1996). A standard mean score of 20 with cut-off points of 17 and 23 (SD=5) on the scoring scale were used to cluster participants into the health profile taxonomy, using the 13 mutually exclusive health profiles (Table 1). Domains are scored in the direction of their name; “good health” in a domain is a score greater than 23 for satisfaction with health and resilience and less than 17 for discomfort and risks.
This scoring rubric was used to further categorize participants into the following four health status rankings: 1- Best Health Status (average or excellent health in all CHIP-AE domains), 2- Fair Health Status (poor health in one domain), 3- Poor Health Status (poor health in two domains), 4- Worst Health Status (poor health in three or all domains) (see Figure 1). Starfield, Riley, and colleagues (1993, 1996, 1998a) developed this strategy to characterize adolescents according to degree of potential health vulnerability. For example, based on CHIP-AE scores of <17 on resilience and >23 on risks, an adolescent would have the health profile of Low resilience/High risks. This health profile shows that the adolescent scored poorly in two domains on the CHIP-AE (resilience and risks). This adolescent, therefore, would be ranked as having Poor Health Status.
Figure 1.
Ranking of Health Status Using Health Profile Taxonomy
One-way analyses of variance (ANOVAs) were used to compare differences among the health status rankings (Best, Fair, Poor, Worst Health Status) in demographic (current age) and foster care variables (age at first placement, length of time in care). When an overall ANOVA was significant, the Bonferroni procedure was used to determine which groups differed significantly from each other. Chi-square tests were used to compare the four health status groups on gender and racial/ethnic groups and on reasons for and types of foster care placements. For significant overall chi-squares, Cramer’s V was used to interpret the strength of the relationships and the Bonferroni correction was used to identify any significant pairwise comparisons. Kendall’s tau was used to compare the four health status groups (Best, Fair, Poor, Worst Health Status) by developmental age groups (early adolescents, ages 11–13; middle adolescents, ages 14–16; late adolescents, ages 17–19).
Results
Sample Characteristics
Participants considered in this analysis were 136 adolescents in foster care from Northern California who were in the study at baseline. Their mean age was 14.80 years old (SD=1.89; range=11.20–18.86 years old) and 69 were female (50.7%). There were 65 African Americans (47.8%), 19 Latinos (14.0%), 12 Whites (8.8%), 10 Asian/Pacific Islanders (7.4%), and 30 others (22.1%), including those reporting more than one race/ethnicity, another race or ethnicity, or not reporting.
The mean age of first placement was 8.02 (SD=5.15, range=birth-16 years old). Most were first placed in foster care during adolescence (n=50, 36.8%), including 31 early (11–13 years old) and 19 middle (14–16 years old) adolescents. The next largest group was placed as infants or toddlers, from birth to 3 years old (n=33, 24.3%). Eight (5.9%) were placed during preschool (4–5 years old) and 25 (18.4%) were school-aged (6–10 years old). Twenty did not report age at first placement (14.7%).
Participants reported many reasons that contributed to their foster care placement. Predominant parental reasons included: parental substance abuse (n=85, 62.5%), neglect/abandonment (n=75, 55.1%), physical abuse (n=43, 31.6%), emotional abuse (n=39, 28.7%), parental incarceration (n=33, 24.3%), and parental mental illness (n=32, 23.5%). Predominant child-related contributors were aggressive behavior (n=40, 29.4%) and problems with peers (n=36, 26.5%). A host of other child reasons were reported, including running away, substance abuse, sexual risk taking, suicidal behavior, and truancy. While frequencies were small, it was noteworthy that 18 participants reported experiencing sexual abuse (14.0%) and three female participants were pregnant (2.2%). Participants could report more than one reason.
The mean time in foster care was 6.32 years (SD=4.83; range=one month to 17 years). Forty-three point four percent spent five or more years in care (n=59), 17.6% were in foster care three to four years (n=24), 16.9% from one to two years (n=23), 8.1% less than one year (n=11), and 14.1% (n=19) did not report time in care. Participants had a mean of approximately four placements (M=3.86; SD=3.66; range=one to 23 placements). Types of current placement included, group home (n=48, 35.3%), foster family home (n=36, 26.5%), and relative/kinship care (n=35, 25.7%).
Profiles of Health
Of the 136 participants in the FYHP at baseline, 131 participants had sufficient data to be clustered into the 13 mutually exclusive health profiles (see Table 2). Five participants were therefore excluded for missing data. The most frequently occurring of the 13 health profile types in this sample were: Excellent health (n=28, 21.4%), Good health (n=23, 17.6%), Worst health (n= 17, 13.0%), and High risks (n=16, 12.2%). The remaining participants were distributed across profiles with little discernible pattern. A school-based reference sample of adolescents had less Excellent health (n=116, 14.3%), Worst health (n=83, 10.3%), and High risks (n=73, 9.0%) profiles and more Good health profiles (n=230, 28.4%) than FYHP participants (Riley et al., 1998a) (Table 2).
Table 2.
Health Profile Types Frequencies
| Foster Youth Health Project N=136 | School-based Reference Samplea N=865 | ||||
|---|---|---|---|---|---|
|
| |||||
| Profile Type | Frequency | Percent | Frequency | Percent | |
| A | Excellent | 28 | 21.4 | 116 | 14.3 |
| B | Good health | 23 | 17.6 | 230 | 28.4 |
| C | Dissatisfied | 7 | 5.3 | 57 | 7.0 |
| D | High discomfort | 9 | 6.9 | 42 | 5.2 |
| E | Low resilience | 8 | 6.1 | 68 | 8.4 |
| F | High risks | 16 | 12.2 | 73 | 9.0 |
| G | Dissatisfied/high discomfort | 5 | 3.8 | 39 | 4.8 |
| H | Dissatisfied/low resilience | 4 | 3.1 | 27 | 3.3 |
| I | Dissatisfied/high risks | 3 | 2.3 | 15 | 1.9 |
| J | High discomfort/low resilience | 1 | .8 | 16 | 2.0 |
| K | High discomfort/high risks | 6 | 4.6 | 14 | 1.7 |
| L | Low resilience/high risks | 4 | 3.1 | 29 | 3.6 |
| M | Worst health | 17 | 13.0 | 83 | 10.3 |
| Total | 131 | 100.0 | 809 | 100.0 | |
| Missing | 5 | 56 | |||
| Total | 136 | 865 | |||
From: Riley, A. W., Green, B. F., Forrest, C. B., Starfield, B., Kary, M., & Ensminger, M. E. (1998a). A taxonomy of adolescent health: development of the adolescent health profile-types. Medical Care, 36(8), 1228–1236.
Further categorization by ranking resulted in the following health status groups: Group 1- Best Health Status (n=51, 38.9%), Group 2- Fair Health Status (poor in one domain) (n=40, 30.5%), Group 3- Poor Health Status (poor in two domains) (n=23, 17.6%), and Group 4- Worst Health Status (poor in three to all domains) (n=17, 13.0%). Health status rankings were similar to the normative sample, though the normative sample had less Worst Health Status (n=83, 10.3%) (see Table 3).
Table 3.
Health Status Ranking in Four Groups
| Foster Youth Health Project N=131 | School-based Reference Samplea N=809 | |||
|---|---|---|---|---|
|
| ||||
| Health Status Ranking | Frequency | Percent | Frequency | Percent |
| Best Health Status (avg or exc all domains) | 51 | 38.9 | 346 | 42.7 |
| Fair Health Status (poor in 1 domain) | 40 | 30.5 | 240 | 29.6 |
| Poor Health Status (poor in 2 domains) | 23 | 17.6 | 140 | 17.3 |
| Worst Health Status (poor in 3–4 domains) | 17 | 13.0 | 83 | 10.3 |
| Total | 131 | 100.0 | 809 | 100.0 |
From: Riley, A. W., Green, B. F., Forrest, C. B., Starfield, B., Kary, M., & Ensminger, M. E. (1998a). A taxonomy of adolescent health: development of the adolescent health profile-types. Medical Care, 36(8), 1228–1236.
The one-way ANOVAs comparing current age, age at first placement, and length of time in foster care among the four health status groups showed that there was a significant difference in current age (F=8.238, p<.001). Post hoc comparisons indicated that the mean age with Best Health Status (M=14.19, SD=1.87) was significantly different than age with Poor Health Status (M=16.36, SD=1.34) at p<.001. Likewise, the mean age with Fair Health Status (M=14.71, SD=1.93) was significantly different than age with Poor Health Status (M=16.36, SD=1.34) at p=.006 (see Table 4). There were no statistically significant differences in age at first placement or length of time in foster care between the four health status groups.
Table 4.
ANOVA: Mean Ages Among Health Status Groups
| Health Status Group | N | Mean | SD | F | p value |
|---|---|---|---|---|---|
| Best Health Status | 51 | 14.19 | 1.87 | 8.238 | .000 |
| Fair Health Status | 40 | 14.71 | 1.93 | ||
| Poor Health Status | 23 | 16.36 | 1.34 | ||
| Worst Health Status | 17 | 15.03 | 1.41 | ||
| Total | 131 | 14.84 | 1.90 |
Examining the relationship between gender and health status ranking indicated that girls reported significantly worse health than boys (p<.001). Only 35.3% and 42.5% of the Best Health and Fair Health Status groups were girls, while 82.6% and 70.6% of the Poor Health or Worst Health Status groups were girls.
When comparing developmental age group (early- ages 11–13; middle- ages 14–16; and late- ages 17+) and health status ranking, the results suggest early adolescents are in the best health and middle adolescents are represented in higher proportions as the health status ranking worsens. Forty-nine percent of the Best Health Status group were early adolescents; 50.0% of the Fair, 56.5% of the Poor, and 82.4% of the Worst Health Status groups were middle adolescents (Kendall’s tau=0.28, p<.001). There were no significant differences in racial or ethnic groups among the four health status groups (χ2(12,131)=9.743, p=.64).
Chi-square tests examining the association between reasons for placement and health status group resulted in significant comparisons for history of sexual abuse, aggressive behavior, substance abuse, parental death/suicide, and pregnancy (Tables 5 and 6). As the health status ranking gets worse, the proportion of adolescents who report a history of sexual abuse significantly increases (Kendall’s tau=.20, p=.025). For example, a greater percent of those with Worst Health Status had a history of sexual abuse (35.3%) than the percent of those with Best Health Status that reported sexual abuse (7.8%). Other noteworthy trends included greater percentages of adolescents with aggression, substance abuse, and suicidality (all 29.4%) who had Worst Health Status as compared with those who had Best Health Status with these problems (aggression 17.6%, substance abuse 5.9%, suicidality 2.0%). Those who experienced the death or suicide of a parent made up a greater proportion of those with Poor Health Status (17.4%) than those in the Best Health Status group (2.0%). All of the three pregnant adolescents (13%) were in the Poor Health Status group.
Table 5.
Percent within Health Status Group by Reason for Placement
| Profile in 4 Groups N=131* Percentage within Health Status Group | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Reason for Placement | n | Best Health Status | Fair Health Status | Poor Health Status | Worst Health Status | Total Sample |
| Aggressive behavior | 38 | 17.6 | 45.0 | 26.1 | 29.4 | 29.0 |
| Sexual abuse | 18 | 7.8 | 10.0 | 17.4 | 35.3 | 13.7 |
| Substance abuse | 12 | 5.9 | 10.0 | 0 | 29.4 | 9.2 |
| Suicidal | 12 | 2.0 | 10.0 | 8.7 | 29.4 | 9.2 |
| Parental death/suicide | 7 | 2.0 | 5.0 | 17.4 | 0 | 5.3 |
| Pregnancy | 3 | 0 | 0 | 13.0 | 0 | 2.3 |
5 participants missing
Table 6.
Chi-square Tests
| Reason for Placement | n | χ2 | df | p value (2 sided) |
|---|---|---|---|---|
| Aggressive behavior | 38 | 8.261 | 3 | .041 |
| Sexual abuse | 18 | 8.890 | 3 | .031 |
| Substance abuse | 12 | 11.390 | 3 | .010 |
| Suicidal | 12 | 11.595 | 3 | .009 |
| Parental death/suicide | 7 | 8.723 | 3 | .033 |
| Pregnancy | 3 | 14.417 | 3 | .002 |
There were no significant differences in type of placement (foster family, group home, relative/kinship placement) among the four health status groups.
Discussion
Of the 13 mutually exclusive health profiles identified by Starfield, Riley, and colleagues (1993, 1995, 1996, 1998a), adolescents in this study were characterized as having four major health profiles: Excellent, Good, Worst, and High risks. With further ranking into health status groups, many (38.9%) reported that their health was good to excellent in four domains-- satisfaction with health, risks, resilience, and discomfort—or in the Best Health Status group. A positive self-report of good health includes a healthy view of the self and resilience in the face of adversity. These dimensions of health are important considerations in the designation of health profile and status as measured by the CHIP-AE and are strengths to be built upon. Having a positive self-conception and self-esteem despite adversity are health-promoting qualities (Benson et al., 2006; Guerra & Bradshaw, 2008). This dynamic is associated with resilience (Masten, 2000). A positive sense of self is one of the core competencies for positive youth development and when associated with other competencies, such as self-regulation, decision making skills, positive personal values, and interpersonal connectedness, serves as the foundation to reduce risk and prevent problem behavior (Guerra & Bradshaw, 2008).
An adolescent’s self-reported health, however, may not correlate with the perceptions that others have about the adolescent’s functioning. For example, adolescents often reported very good school performance, however, had very poor reading and writing skills during data collection. Likewise, the CASAs often presented contrasting portrayals of their adolescents’ health and abilities. These competing perceptions are important to notice and explore, yet, an adolescent’s positive self-conception is essential to reinforce.
While adolescents in the US are generally one of the healthiest developmental groups, prior research supports that those in foster care are at heightened risk for poor health (Newton, Litrownik, & Landsverk, 2000; Ringeisen et al., 2008; Rubin et al., 2007). The CHIP-AE has been able to uncover poorer self-reported health in other vulnerable populations than in the general population of adolescents. For example, a higher percentage of incarcerated males (69.8%) had three major health profiles—High risks, High risks/Low resilience, and Worst health profiles than a matched age school sample (37.3%). Only 6.4% of the incarcerated sample had an Excellent or Good health profile in contrast to 34.2% of the school sample (Forrest, Tambor, Riley, Ensminger, & Starfield, 2000). In addition, acutely and chronically ill teenagers as expected had higher disorders and discomfort scores on the CHIP-AE, but also demonstrated lower satisfaction with health and low self-esteem (Starfield et al., 1996). This foster care sample, however, reported better health than other groups of vulnerable adolescents. Potential reasons for this counterintuitive result must be explored.
The CHIP-AE posits that adolescents are the best and only appropriate reporters of their health, however, adolescents in foster care may portray their health status with a positive social bias (Kools et al., 2009). Placement transitions are commonplace in this group and are often the result of problem behaviors brought to the attention of those who evaluate home and school appropriateness. Presenting oneself in the most favorable light, with few problems may be a way to promote personal stability, including the least amount of attention from authority figures and the avoidance of life disruption. Previous research demonstrated that adolescents in foster care create a façade of healthy functioning and pseudoindependence to protect themselves from the uncertainty of foster care (Kools, 1997; Kools, 1999). Further, young people who have experienced past abuse by trusted adults may be reluctant to disclose vulnerabilities (Voices for Illinois Children, 2009). Self-protection strategies may shield the young person from further disappointment, rejection, and trauma, including losses associated with additional placement and school transitions. This positive self-portrayal is consistent with research that validated the theoretical conception that adolescents who are members of stigmatized groups may hold positive self views to protect themselves by way of rejecting how they think others may perceive them (Hillman, Wood, & Sawilowsky, 1998). Because of the potential influence of self-protection on adolescent perceptions of health, reports of foster caregivers, teachers, CASAs, and others who know the adolescent well may be necessary to get a full picture of both their strengths and health concerns.
Even with strong results that depict predominantly good health profiles, there was also close to a third of the sample (30.6%) who were ranked as having Poor or Worst Health Status (poor health in two to all four of the domains measured). This is more consistent with prior reports of 30% of children in foster care having chronic health conditions or concerns (Jee et al., 2006) and 50–80% having mental health and/or developmental problems (Jee et al., 2006; Kerker & Dore, 2006; Rubin et al., 2007). It is crucial here to note that there are specific subgroups of adolescents who experience particular vulnerability; they may not self-present in a positive way. In this study, there was a clear subgroup of adolescents who were engaging in high risk behaviors, including substance abuse and unprotected sex. In a longitudinal study of foster youth transition to adulthood, there were four distinct subgroups of youth, including the largest group (43%) designated as “distressed and disconnected” (Keller, Cusick, & Courtney, 2007). Similar to our sample, they had more traumatic experiences and problem behaviors that indicated higher risk.
Developmental trends are also important to note and perceptions of health are developmentally-mediated (Ryan-Wenger, 2003). Early adolescents had the best health profiles. Their health perceptions may have been skewed toward positive health, with low self-awareness about their health or health risks and a limited cognitive ability to consider long-term consequences of behavior (Steinberg, 2007). For example, there was a high incidence of obesity in the sample and it may be possible that these younger adolescents made little connection between current overweight and low physical activity and later consequences like diabetes, hyperlipidemia, and hypertension when they self-assess “healthiness.” Younger adolescents may have had less time and opportunity to engage in risky behaviors and/or experience the negative health consequences of these behaviors (Eaton et al., 2008). Middle adolescents, in contrast, represented the greatest proportion of those with Worst Health profiles. With increasing brain development, immature emotional and behavioral regulation, and vulnerability to peer influence (Steinberg, 2007), middle adolescents have increased self-awareness and rates of risk taking. Finally, there were too few late adolescents in the study to determine whether the direction of this negative trend would continue.
Additionally, there appears to be gender specificity in health profiles. Adolescent girls were more often categorized in the Poor or Worst Health Status groups than adolescent boys. This study supports that girls in foster care are more vulnerable to poor health. Girls reported diminished self-esteem, less satisfaction with health, and more physical and emotional discomfort as subdimensions of health. These may be gender-specific responses to their histories of abuse, neglect, and other adverse experiences that led to their foster care placement.
Finally, many in the sample had the Worst Health profile; that is, poor health in three to four domains. In this study, high percentages of foster youth who reported aggressive behavior, a history of sexual abuse or past suicidal ideation or behavior had Worst Health profiles. Understanding and addressing the vulnerability of these adolescents are complex endeavors as they report significant problems across a wide spectrum of health issues.
Limitations
The participants in the study were adolescents who had CASAs and findings may not be generalizable to all youth in foster care. Because the numbers of children and adolescents in foster care far exceed the availability of CASAs, it is typical that those with the most complex and difficult issues are assigned CASAs (Bernstein, 2006); the sample is therefore unlikely to be biased toward a healthier group. While their demographic and placement histories are consistent with national statistics on the foster care population, these results may not reflect the experiences of adolescents in stable foster care or those in rural or suburban contexts in other regions of the country. This analysis was limited by the lack of a comparison group.
Use of the CHIP-AE may have limitations in the foster care population for being exclusively adolescent self-report. It may be necessary to incorporate foster caregiver or other parent proxy perceptions to mitigate the confounding nature of self-protection and to illuminate important health concerns that may be missed in these youth. Results of this study raised the possibility of worsening health status with age; however, there were insufficient adolescent participants to interpret a developmentally-related trend in health across adolescence. A study with larger cohorts of early, middle, and late adolescents is necessary to verify this potential trajectory or to verify that middle adolescents have a higher vulnerability that needs to be better understood.
Despite these limitations, the analytic strategy of health profile analysis allowed us to identify subgroups of adolescents in foster care who are particularly vulnerable to poor health, including girls and those with high risk behaviors (substance abuse, risky sexual behavior), aggression, a history of sexual abuse, or past suicidality. Early adolescence may be an opportune period to target prevention and early intervention efforts. For these reasons, the CHIP-AE may be a useful instrument (with the addition of parent proxy report), with both clinical and research applications. Detailed health profiles enable the identification of foster youth in most need of intervention as well as the ability to tailor interventions to address their specific health needs and concerns.
Clinical Implications
While many of the adolescents in this study may have inflated their health statuses or perceived their health to be better than others’ perceptions, it is important for clinicians to reinforce one’s perceived strengths as well as positive self-conceptions for all adolescents. This is one strategy believed to enhance resilience (Masten, 2000) and promote positive youth development (Benson et al., 2006). For adolescents in foster care who more clearly fall into Poor or Worst Health profiles, high risk behavior such as substance abuse and risky sexual behavior may be prominent markers. Individualized interventions may be tailored to assess individual risks, engage in risk and harm reduction strategies, and identify and promote personal strengths and resilience.
Interventions that not only reduce risk and increase personal assets and external resources, but incorporate protective processes such as social connectedness with a caring adult are critical. From syntheses of program effectiveness studies (DuBois, Holloway, Valentine, & Cooper, 2002; Roth, Brooks-Gunn, Murray, & Foster, 1998), formal mentoring programs like the Big Brother/Big Sister Program (Tierney, Grossman, & Resch, 1995; Jucovy & Herrera, 2009) and natural mentoring that comes from supportive nonparental relationships from within the adolescent’s social network (DuBois & Silverhorn, 2005; Bernat & Resnick, 2006) are among the strength-based approaches with potential to promote health and reduce risk for foster youth. More general positive youth development programs which incorporate mastery of life skills (e.g., academics, self-regulation, decision making/problem solving, anger management, resistance skills), are considered best practices and may be of help (Benson et al., 2006; Guerra & Bradshaw, 2008).
Findings from this study also suggest that developmental age and gender may influence health profiles. Early adolescence is a window of opportunity for health prevention interventions for adolescents in foster care and they should be considered a target population for these efforts. Prevention and intervention strategies targeted toward females may also be a fruitful approach, however, gender-based analyses of the efficacy of programs to date are lacking and we need more evidence of why specifically gender matters (Moretti, Odgers, Reppucci, & Catherine, 2011).
Despite potential problems of using the CHIP-AE in a foster care population, this instrument allows for the identification of adolescents with Poor to Worst Health profiles. Care providers often feel stymied, helpless, or hopeless to support and assist these vulnerable young people. Using an instrument like the CHIP-AE allows us to discover the specific array of problems, concerns, or needs that an individual adolescent in foster care is experiencing. In the intervention implemented in the larger study, the advanced practice nurses provided ongoing consultation with CASAs serving foster youth in the treatment group. In this model, the advanced practice nurse collaborated with the CASA to develop and prioritize a health problem list in order to break down the complexity of a youth’s health profile. This assisted the CASA to target advocacy for the most pressing health issues, thus making step-by-step progress in addressing serious and multifaceted problems, especially for those with the complex needs and problems seen in profiles indicating Poor to Worst Health Status. In this way, interventions were tailored for the unique health profile of an individual adolescent. This intervention is a model that could be useful to other child serving professionals. Further, separating out these most vulnerable of the vulnerable youth would allow case managers and clinicians to target limited resources to the adolescents in most need.
Acknowledgments
Funding Source: National Institute of Nursing Research, R01 NR08243
Community Collaborators: The Court Appointed Special Advocates Programs of San Francisco, Alameda, and Solano Counties in California
Foster Youth Health Project Nurses and Research Assistants: Aara Amidi-Nouri, PhD, RN, Bridget Gramkowski, MS, PNP, Erica Monasterio, MN, FNP-BC; Ekua Blankson, MS, PNP, Ceily Davis, MS, PNP, Rasheda Jones, MS, RN, and Cynthia Oei, MS, RN; Nancy Robbins, MSW (Project Director)
Participants: Many thanks to the young people in foster care and their Court Appointed Special Advocates who participated in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan Kools, Email: susan.kools@nursing.ucsf.edu, University of California, San Francisco, Department of Family Health Care Nursing, 2 Koret Way, Box 0606, San Francisco, CA 94143, Phone (415) 476-4040, Fax (415) 753-2161.
Steven M. Paul, University of California, San Francisco School of Nursing, Office of Research.
Rasheda Jones, Department of Family Health Care Nursing.
Erica Monasterio, Department of Family Health Care Nursing.
Jane Norbeck, Department of Community Health Systems.
References
- Administration for Children and Families. National Survey of Child and Adolescent Well-Being (NSCAW) CPS sample component Wave I data analysis report. 2005 Retrieved from http://www.acf.hhs.gov/programs/opre/abuse_neglect/nscaw/reports/cps_sample/cps_report_revised_090105.pdf.
- Administration for Children and Families. National Survey of Child and Adolescent Well-Being (NSCAW): One year in foster care Wave I data analysis report. 2003 Retrieved from http://www.acf.hhs.gov/programs/opre/abuse_neglect/nscaw/reports/nscaw_oyfc/oyfc_report.pdf.
- Adoption and Foster Care Analysis and Reporting System (AFCARS) The AFCARS report: Preliminary FY estimates as of July 2010. 17. US Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau; 2010. Retrieved from www.acf.hhs.gov/programs/cb/stats_research/index.htm#afcars. [Google Scholar]
- American Academy of Pediatrics (AAP) Fostering health: Health care for children and adolescents in foster care. 2. New York: AAP District II; 2005. Task Force on Health Care for Children in Foster Care. [Google Scholar]
- American Association of Child and Adolescent Psychiatry. Foster care: Facts for families. 2006;(64) Retrieved from http://www.aacap.org/cs/root/facts_for_families/foster_care.
- Benson PL, Scales PC, Hamilton SF, Sesma A, Hong KL, Roehlkepartain EC. Positive youth development so far: Core hypotheses and their implications for policy and practice. Search Institute Insights & Evidence. 2006;3(1):1–13. [Google Scholar]
- Bernat DH, Resnick MD. Healthy youth development: science and strategies. Journal of Public Health Management and Practice. 2006;(Suppl):S10–S16. doi: 10.1097/00124784-200611001-00004. [DOI] [PubMed] [Google Scholar]
- Bernstein RE. University Honors Program. Texas State University; 2006. Advocates in action: The impact of Court Appointed Special Advocates (CASAs) on the Child Welfare System. Paper 22. Retrieved from http://ecommons.txstate.edu/honorprog/22. [Google Scholar]
- Carpenter SC, Clyman RB, Davidson AJ, Steiner JF. The association of foster care or kinship care with adolescent sexual behavior and first pregnancy. Pediatrics. 2001;108(3):1–6. doi: 10.1542/peds.108.3.e46. [DOI] [PubMed] [Google Scholar]
- Chernoff R, Combs-Orme T, Risley-Curtiss C, Heisler A. Assessing the health status of children entering foster care. Pediatrics. 1994;93(4):594–601. [PubMed] [Google Scholar]
- Clausen JM, Landsverk J, Ganger W, Chadwick D, Litronik A. Mental health problems of children in foster care. Journal of Child and Family Studies. 1998;7:283–296. [Google Scholar]
- DuBois DL, Holloway BE, Valentine JC, Cooper H. Effectiveness of mentoring programs for youth: A meta-analytic review. American Journal of Community Psychology. 2002;30(2):157–197. doi: 10.1023/A:1014628810714. [DOI] [PubMed] [Google Scholar]
- DuBois DL, Silverthorn N. Natural mentoring relationships and adolescent health: Evidence from a national study. American Journal of Public Health. 2005;95(3):518–524. doi: 10.2105/AJPH.2003.031476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Lim C, Brener ND, Wechsler H for Disease Control Center. Youth Risk Behavior Surveillance—United States, 2007. MMWR Surveillance Summary. 2008;57(SS04):1–131. [PubMed] [Google Scholar]
- Farruggia SP, Sorkin DH. Health risks for older US adolescents in foster care: The significance of important others’ health behaviours on youths’ health and health behaviors. Child Care, Health and Development. 2009;35:340–348. doi: 10.1111/j.1365-2214.2009.00960.x. [DOI] [PubMed] [Google Scholar]
- Forrest CB, Tambor E, Riley AW, Ensminger ME, Starfield B. The health profile of incarcerated male youths. Pediatrics. 2000;105(1):286–291. [PubMed] [Google Scholar]
- Guerra NG, Bradshaw CP. Linking the prevention of problem behaviors and positive youth development: Core competencies for positive youth development and risk prevention. New Directions in Child and Adolescent Development. 2008;122:1–17. doi: 10.1002/cd.225. [DOI] [PubMed] [Google Scholar]
- Harden BJ. Safety and stability for foster children: A developmental perspective. The Future of Children. 2004;14(1):31–47. [PubMed] [Google Scholar]
- Hillman SB, Wood PC, Sawilowsky SS. The Protective Style Questionnaire: Self-protective mechanisms among stigmatized adolescents. Social Behavior and Personality. 26(1):29–38. [Google Scholar]
- Jee SH, Barth RP, Szilagyi MA, Szilagyi PG, Aida M, Davis MM. Factors associated with chronic conditions among children in foster care. Journal of Health Care for the Poor and Underserved. 2006;17(2):328–341. doi: 10.1353/hpu.2006.0062. [DOI] [PubMed] [Google Scholar]
- Jucovy L, Herrera C. High school mentors in brief: Findings from the Big Brothers Big Sisters school-based mentoring impact study. Public/Private Ventures: In Brief. 2009;8:1–3. Retrieved from http://www.ppv.org/ppv/publications/assets/313_publication.pdf. [Google Scholar]
- Keller TE, Cusick GR, Courtney ME. Approaching the transition to adulthood: Distinctive profiles of adolescents aging out of the Child Welfare System. Social Services Review. 2007;81(3):453–484. doi: 10.1086/519536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerker BD, Dore M. Mental health needs and treatment of foster youth: Barriers and opportunities. American Journal of Orthopsychiatry. 2006;76(1):138–147. doi: 10.1037/0002-9432.76.1.138. [DOI] [PubMed] [Google Scholar]
- Klee L, Halfon N. Mental health care for foster children in California. Child Abuse and Neglect. 1987;11:63–74. doi: 10.1016/0145-2134(87)90034-2. [DOI] [PubMed] [Google Scholar]
- Kools S. Adolescent identity development in foster care. Family Relations. 1997;46(3):263–271. [Google Scholar]
- Kools S. Self-protection in adolescents in foster care. Journal of Child and Adolescent Psychiatric Nursing. 1999;12(4):139–152. doi: 10.1111/j.1744-6171.1999.tb00063.x. [DOI] [PubMed] [Google Scholar]
- Kools S, Paul S, Norbeck J, Robbins N. Dimensions of health in young people in foster care. International Journal of Adolescent Medicine and Health. 2009;21(2):221–233. doi: 10.1515/ijamh.2009.21.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie LK, James S, Monn A, Kanten MC, Zhang J, Aarons G. Health-risk behaviors in young adolescents in the child welfare system. Journal of Adolescent Health. 2010;47(1):26–34. doi: 10.1016/j.jadohealth.2009.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten AS. Children who overcome adversity to succeed in life. University of Minnesota- Extension; 2000. Retrieved from http://www.extension.umn.edu/distribution/familydevelopment/components/7565_06.html. [Google Scholar]
- Mekonnen R, Noonan R, Rubin D. Achieving better health outcomes for children in foster care. Pediatric Clinics of North America. 2009;56(2):405–415. doi: 10.1016/j.pcl.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Moretti MM, Odgers C, Reppucci D, Catherine NLA. Serious conduct problems among girls at risk: Translating research into intervention. International Journal of Child, Youth and Family Studies, 1 &. 2011;2:142–61. [Google Scholar]
- Newton RR, Litrownik AJ, Landsverk JA. Children and youth in foster care: Disentangling the relationship between problem behaviors and number of placements. Child Abuse and Neglect. 2000;24(10):1363–1374. doi: 10.1016/s0145-2134(00)00189-7. [DOI] [PubMed] [Google Scholar]
- Riley AW, Green BF, Forrest CB, Starfield B, Kary M, Ensminger ME. A taxonomy of adolescent health: development of the adolescent health profile-types. Medical Care. 1998a;36(8):1228–1236. doi: 10.1097/00005650-199808000-00010. [DOI] [PubMed] [Google Scholar]
- Riley AW, Forrest CB, Starfield B, Green B, Kang M, Ensminger M. Reliability and validity of the adolescent health profile-types. Medical Care. 1998b;36(8):1237–1248. doi: 10.1097/00005650-199808000-00011. [DOI] [PubMed] [Google Scholar]
- Ringeisen H, Casanueva C, Urato M, Cross T. Special health care needs among children in the child welfare system. Pediatrics. 2008;122(1):e232–e241. doi: 10.1542/peds.2007-3778. [DOI] [PubMed] [Google Scholar]
- Roth J, Brooks-Gunn J, Murray L, Foster W. Promoting healthy adolescents: Synthesis of youth development program evaluations. Journal of Research on Adolescence. 1998;8(4):423–459. [Google Scholar]
- Rubin DM, O’Reilly ALR, Hafner L, Luan X, Localio AR. The impact of placement stability on behavioral well-being in foster care. Pediatrics. 2007;119(2):336–344. doi: 10.1542/peds.2006-1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan-Wenger NA. Early adolescents’definition of health: The development of a new taxonomy. Journal of Theory Construction and Testing. 2003 Sep 22;2003 Retrieved from http://www.allbusiness.com/professional-scientific/scientific-research/728543-1.html. [Google Scholar]
- Schor EL. The foster care system and health status of foster children. Pediatrics. 1982;69(5):521–528. [PubMed] [Google Scholar]
- Simms MD, Dubowitz H, Szilagyi MA. Health care needs of children in the foster care system. Pediatrics. 2008;106:909–918. [PubMed] [Google Scholar]
- Starfield B, Bergner M, Ensminger M, Riley A, Ryan S, Breen B, McGanhey P, Skinner A, Kim S. Adolescent health status measurement: Development of the Child Health and Illness Profile. Pediatrics. 1993;91(2):430–435. [PubMed] [Google Scholar]
- Starfield B, Forrest CB, Ryan SA, Riley AW, Ensminger ME, Green B. Health status of well vs. ill adolescents. Archives of Pediatric and Adolescent and Medicine. 1996;150(12):1249–1256. doi: 10.1001/archpedi.1996.02170370027003. [DOI] [PubMed] [Google Scholar]
- Starfield B, Riley AW, Green BF, Ensminger ME, Ryan SA, Kelleher K, Kim-Harris S, Johnston D, Vogel K. The adolescent Child Health and Illness Profile: A population-based measure of health. Medical Care. 1995;33(5):553–566. doi: 10.1097/00005650-199505000-00008. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Risk taking in adolescence: New perspectives from brain and behavioral science. Current Directions in Psychological Science. 2007;16(2):55–59. [Google Scholar]
- Taussig HN. Risk behaviors in maltreated youth placed in foster care: A longitudinal study of protective and vulnerability factors. Child Abuse and Neglect. 2002;26:1179–1199. doi: 10.1016/s0145-2134(02)00391-5. [DOI] [PubMed] [Google Scholar]
- Tierney JP, Grossman JB, Resch NL. Making a difference: An impact study of Big Brothers/Big Sisters. Philadelphia: Public/Private Ventures; 1995. [Google Scholar]
- United States Accountability Office. Foster care: State practices for assessing health needs, facilitating service delivery, and monitoring children’s care. 2009 GAO 09–26. Retrieved from http://www.gao.gov/new.items/d0926.pdf.
- Vaughn MG, Ollie MT, McMillen JC, Scott L, Munson M. Substance use and abuse among older youth in foster care. Addictive Behavior. 2007;32:1929–1935. doi: 10.1016/j.addbeh.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voices for Illinois Children. Supporting foster care youth on the way to adulthood. 2009 Retrieved from http://scholar.googleusercontent.com/scholar?q=cache:BbHoz4GK_8kJ:scholar.google.com/&hl=en&as_sdt=0,5.