Abstract
Introduction
We hypothesized that fruit/vegetable intake and eating behaviors mediate the relationship between experimental condition and weight loss in a randomized trial evaluating a text-message based weight loss program.
Methods
Overweight/obese individuals from San Diego, CA (N=52 with complete data) were randomly assigned in 2007 into one of two groups for four months: 1) the intervention group that received 2-5 weight management text-messages p/day; 2) the usual-care comparison group. Three 24-hour recalls assessed fruit/vegetable intake change and the Eating Behavior Inventory (EBI) measured change in eating behaviors. Regression path models tested intervention mediation.
Results
Direct effects of the intervention were found for change in body weight (b=-3.84, R2=0.074), fruit/vegetable intake (b=2.00, R2=0.083), and EBI scores (b=7.15, R2=0.229) (ps < 0.05). The treatment group to weight change path was not statistically significant (b=-0.673, R2=0.208) when fruit/vegetable intake change and EBI score change were specified as intervention mediators in the model. The total indirect effect was 3.17 lbs. indicating that the indirect paths explained 82.6% of the total effect on weight change.
Discussion
Fruit/vegetable intake and eating behaviors mediated the intervention's effect on weight change. The findings suggest that sending text-messages that promote healthy eating strategies resulted in moderate short-term weight loss.
Keywords: SMS, mobile phone, obesity, diet, mediator, and health behavior
Introduction
In the U.S., 68% of adults age 20 and over are overweight or obese (Flegal et al., 2010) and by 2030, 50% are projected to be obese (Finkelstein et al., 2012). Obesity contributes to six of the ten leading causes of death in America, including heart disease, type 2 diabetes, certain cancers, and high blood pressure (Danaei et al., 2009). It is well known that for most people obesity is caused by a positive energy imbalance (NHLBI, 2007), which occurs primarily due to lack of physical activity and over consumption of an energy dense diet (Hill, 1998; Koplan, 1999). Fortunately, obesity is highly preventable and treatable with modifiable lifestyle changes (Curioni and Lourenço, 2005; Stiegler and Cunliffe, 2006). Research indicates that weight loss is best achieved through a combination of improved diet and physical activity behaviors (Knowler et al., 2002). Therefore, to reduce the burden of illness and disability caused by obesity, it is critical to design effective interventions that help individuals improve these behaviors.
One behavior that has been associated with an increase intervention-related weight loss success is the consumption of fruits and vegetables (Dolecek et al., 1997; Epstein et al., 2001; Weinsier et al., 2009). Because fruits and vegetables are high in water and fiber and low in energy density, consuming more of them can help increase satiety, reduce hunger, and decrease energy intake (Rolls et al., 2004). Another factor known to increase weight loss success is learning to manage other eating-related behaviors (e.g., healthy snacking, spacing of consumption, and self-monitoring of food intake) to reduce caloric intake. Frequent use of appropriate self-management strategies were related to weight loss when used in weight management interventions (BingBing and Dennis, 2000; Unick et al., 2010; Pellegrini et al., 2011). Increasing fruit and vegetable intake and healthy eating behaviors are important weight loss strategies, and therefore changes in these behaviors are potential mediators between an intervention program and weight loss outcomes.
Conducting a mediation analysis can provide information into the development of effective interventions for weight loss because mediators identify why and how interventions work. In its simplest form, mediation is when X (i.e., the independent variable) causes M (i.e., the mediator), which causes Y (i.e., the dependent variable) (MacKinnon et al., 2007). Statistical mediation occurs if, after adjusting for the influence of M on Y, the effect of X on Y is eliminated or diminished. Identifying mediators of the effect of an intervention program on weight loss informs theory and intervention design by providing evidence as to what mechanisms the intervention used to result in weight loss (Kraemer, 2002).
A promising new way to deliver information and reminders and communicate with obese individuals about weight loss strategies is through text-messaging (Haapala, Barengo, Biggs, Surakka, & Manninen, 2009; Patrick et al., 2009). Text-messaging is an inexpensive, almost-instantaneous form of two-way communication that transmits brief written messages via a mobile phone and has many capabilities that can be harnessed for weight loss. For instance, depending on its function text messages can convey cues to action, prompts, goals, goal reminders, feedback and reinforcement; important constructs in several behavioral theories (Bandura, 1986; Stokols, 1992; Patrick et al., 2005). Unlike other modes of communication (e.g., brief advice, print material), text messaging is particularly unique in its ability to access individuals by mobile phone almost anywhere and anytime. If used properly, real-time access can be used to motivate individuals make healthful lifestyle decisions that are made continuously throughout the day, such as making healthful diet choices.
We are unaware of any research examining meditation in the context of a text-message based weight loss study. In this study, we used data from Patrick et al.'s (2009) Mobile Diet Intervention through Electronic Technology (mDIET) study to examine if fruit and vegetable intake and eating behaviors mediated the intervention effect on weight loss. mDIET was a randomized controlled trial of a text-message based weight loss intervention. We chose to test these two aspects of weight loss because they were the focus of the majority of the mDIET intervention content and were fairly uncorrelated variables (r = .19, p = .178). Fruit and vegetable intake served as a marker of diet quality, while eating behaviors served as an indicator of use of behavioral weight loss strategies. We hypothesized that fruit and vegetable intake and eating behaviors would mediate the relationship between treatment assignment (i.e., the intervention group vs. the comparison group) and weight loss explaining a significant amount of the effect of the intervention on participants’ weight change.
Methods
Study Design
Data for the current study were from Patrick et al.'s (2009) Mobile Diet Intervention through Electronic Technology (mDIET) study. This randomized controlled trial had two treatment groups: 1) the intervention group that received diet and physical activity weight related text-messages and 2) the usual-care comparison group that received print materials. Group assignment was by computer-generated simple randomization. Participants were recruited in 2007 and the intervention duration was four months. The Institutional Review Board at the University of California, San Diego, CA approved all study procedures, methods, and intervention strategies.
Inclusion Criteria and Participant Recruitment
Sixty-five overweight and moderately obese men and women were recruited in 2007 from San Diego, CA via newspaper ads, flyers, and online announcements on Craigslist. Eligible individuals were 25 to 55 years old, overweight or obese (BMI ≥ 25.0-39.9), not taking medications known to cause weight gain, and owned a mobile phone capable of sending and receiving text-messages. Individuals were assigned to either the comparison or intervention group by computer-generated simple randomization. Study staff and participants were blinded to the treatment assignment until after completion of the baseline measurements.
Measures
Assessments were performed at baseline and four-months post baseline at the UCSD research offices by trained staff blinded to participant group assignment. The primary outcome was body weight (lbs.) measured using a calibrated digital (American Weights & Measures, Rancho Santa Fe, CA).
Fruit and vegetable intake was measured with three 24-hour recalls at each measurement wave. Trained data collectors conducted dietary recalls for two weekdays and one weekend day using the University of Minnesota Nutrition Data System for Research (NDS-R) software (Schakel et al., 1988). Participants were taught how to measure food portions with 3-dimensional food models. The first interview was conducted in person and the second and third by phone. Participants received two-dimensional food models to use for the second assessment. Servings of fruits and vegetables per 1000 kcals were calculated by averaging values from the two intake records. This is a commonly used method to adjust for energy intake (Anderson et al., 2007; Velentzis et al., 2011). Change in the intake of fruit and vegetable servings was one of the potential mediator variables in this analysis.
Eating behaviors associated with weight loss and weight management behaviors were measured using with the 26-item Eating Behavior Inventory (EBI: Appendix I.) (O'Neil et al., 1979). Each behavior on the EBI is rated on a five-point scale (i.e., 1 = “Never or hardly ever” to 5 = “Always or almost always”). Summed scores can range from 26 to 130. Sample items include, “I refuse food offered to me by others” and “I decide ahead of time what I will eat for meals and snacks.” The EBI has good test-retest reliability (r = 0.74) (O'Neil et al., 1979). This questionnaire has been used in over 20 weight loss interventions studies, which have shown the EBI as a valid tool for assessing weight management behaviors (O'Neil and Rieder, 2005). Change in EBI score (i.e., points) from baseline to four months was the second selected mediator variable in this analysis.
Intervention Group
Each participant chose to receive two to five automatically scheduled, tailored, and sometimes interactive (i.e., asked for a specified response) text-messages a day on primarily diet and some physical activity weight management topics. Approximately 2/3 of the text messages related to diet, nutrition, food, or eating. Personal tailoring was accomplished by providing flexibility in the number and timing of receipt of messages each day. For example, users could choose different times during the day to receive a message—typically one in the morning and one in the evening, with one to three additional messages when the user thinks a reminder would be helpful. At the beginning of the intervention, participants also received a printed binder of materials organized by weekly weight management topics, each reinforced by several text-messages received that week. Monthly health counseling calls (5 to 15 minutes in duration) from a trained health coach provided encouragement and reinforcement of weight management topics.
The intervention was structured in weekly blocks based upon behavioral strategy topics known to positively influence weight management. The diet topics included: 1) goal setting (Knowler et al., 2002) and self-monitoring (Wing and Hill, 2001; Kruger et al., 2006); 2) understanding calories (Wardle et al., 2000); 3) volumetrics (i.e., consuming foods that are healthy and make one feel “full” such as fruits and vegetables) (Bell et al., 1998; Stubbs et al., 1998); 5) organization and meal planning (Kruger et al., 2006); 6) strategies for eating out (e.g., avoiding large portions and high energy dense foods (Guthrie et al., 2002; Duffey et al., 2007); and 7) strategies for creating healthy food environments (Stokols, 1992; Hill, 1998). Some example text-messages were: 1) Writing down what you ate and how you felt when you ate it will help you stay on track with your goals; 2) Organize your pantry so that healthier foods are facing forward and less healthier items are in the back and out of sight; 3) Find friends who share similar weight loss goals and support each other. It's fun to exchange healthy recipes too! Also included were picture messages, messages equivalent to text-messages in simplicity of content and message size that related to constructs such as serving size or tracking of personal weight status over time.
A database of over 3000 text and picture messages was developed. Approximately half of the messages were interactive (i.e., requested a reply) with the balance providing tips, suggestions, prompts, and reminders for improved behaviors. A total of 1500 rules programmed into the text-messaging system determined what message was sent based the weekly behavioral strategy, the day of week, and time of day, as well as other parameters including self-reported responses from the baseline EBI assessment (O'Neil et al., 1979; O'Neil and Rieder, 2005). The EBI was used to identify diet behaviors that were unique to each participant that were also known to contribute to increased caloric intake. From the EBI data, target goals were created. These goals were presented to the user via text-message and goal reminders served as prompts for food selection and behavioral improvements.
Comparison Group
The usual care comparison group received in the mail one to two pages of print materials each month for four months. Meant to reflect usual care non-tailored approaches to weight loss, print materials were more general than the binder received by the intervention group and included basic information and tips on weight loss, nutrition, walking, fruit and vegetables, and physical activity. Some of the topics and content overlapped information provided in the intervention group's binder and text-messages.
Statistical Analysis
The study had 80% power to detect a 5.7 lb. between group difference in body weight for a two-tailed test with alpha at .05. Treatment condition was coded as 0 and 1 for control and mDIET groups, respectively. Difference scores were computed for the mediator and outcome variables by subtracting the baseline value from the four-month post-baseline value. Regression path models were specified and estimated to test for multiple mediation (MacKinnon, 2008). All analyses were conducted using M-plus 6.1.
Results
Seventy-eight participants were randomized into the intervention group (n = 39) and comparison group (n = 39). Sixty-five participants completed baseline assessments and started the intervention. The analytical sample (N=52) was approximately 80% female and 75% Caucasian with a mean age of 46 (SD = 7.04) with a BMI of 32.8 (SD = 3.88). There were no differences in sample characteristics between the intervention and comparison groups, except for age—the intervention group was five years older (p = 0.007). See Patrick et al. (2009) for more information regarding demographics, a participant flow diagram, and loss/exclusions after randomization. Adherence to the text-message component of the intervention was calculated as the percentage of messages requesting a reply that prompted an actual response. During the first week, participants responded to all of the messages that requested a reply. By week 16, participants were responding to approximately two out of three messages.
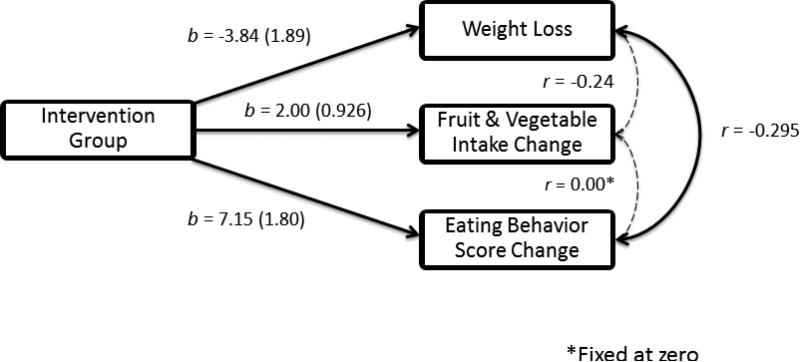
Unadjusted sample means for weight status, EBI scores, and fruit and vegetable intake over the course of the study are shown in Table 1. At the end of four months, the intervention group lost 5.09 lbs., (sd = 7.90) and the comparison group lost1.39 lbs.(sd = 5.90). The estimated difference in weight change between groups was -3.71 lbs. (se = 1.90, p = .051). Figure 1 displays the first path model which tested the direct paths from intervention group to change in weight, fruit and vegetable intake, and EBI scores and fit the data well (χ2(1) = .231, p = .631). This model includes only direct effects while adjusting for all other variables in the model. Significant direct effects of being in the intervention group were found for change in weight (b = -3.84, se = 1.89, p = .042, R2 = 0.074), fruit and vegetable intake (b = 2.00, se = 0.926, p = .031, R2 = 0.083), and EBI scores (b = 7.15, se = 1.80, p < .001, R2 = 0.229). Negative correlations were found between weight loss and change in fruit and vegetable intake (r = -0.24, p = .06), and weight loss and change in EBI score (r = -0.30, p = .02). The correlation between fruit and vegetable change and EBI score change was fixed at zero based on initial descriptive statistics (i.e., r = .19, p = .178).
Table 1.
Unadjusted means and standard deviations for weight, EBI1 scores, and fruit/vegetable intake by group.
| Baseline | 4 Months | Change | p-value2 | |
|---|---|---|---|---|
| Comparison | ||||
| Weight (lbs.) | 195.01 (29.38) | 193.67 (31.11) | -1.39 (5.90) | .243 |
| EBI Score | 72.19 (7.57) | 74.23 (6.58) | 2.04 (6.82) | .140 |
| Fruit/Vegetable Intake | 5.84 (3.04) | 4.33 (2.69) | -1.52 (4.22) | .079 |
| Intervention | ||||
| Weight (lbs.) | 192.85 (36.77) | 187.76 (40.04) | -5.09 (7.90) | .003 |
| EBI Score | 70.88 (6.21) | 79.62 (8.11) | 8.73 (6.23) | < .001 |
| Fruit/Vegetable Intake | 4.60 (3.01) | 5.08 (3.48) | 0.49 (2.33) | .297 |
EBI = Eating Behavior Inventory
p-value for paired t-test comparing difference within groups between baseline and 4 months.
Figure 1.
Path model of the adjusted direct effects of experimental group on weight loss, change in fruit & vegetable intake, and change in eating behaviors. The standard error for each unstandardized coefficient is presented in parentheses. Solid lines are statistically significant at p < .05.
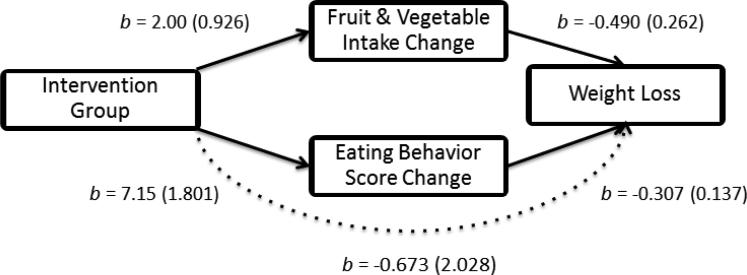
The mediation model is presented in Figure 2. This model depicts fruit and vegetable intake change and EBI score change as mediating the relationship between intervention group and weight change. The dotted line indicates that the direct path from intervention group to weight change is no longer statistically significant (b = -0.673, se = 2.03, p = .740). The R2 for weight change in the model is 0.208 and the total effect on weight change equaled the direct effect (.673) plus the indirect effect (3.17), which equaled 3.85 pounds (p = .042). The indirect effect is comprised of two paths (i.e., intervention group × fruit and vegetable intake change (2.00 x 0.49 = 0.98); and intervention group × EBI score change (7.15 × 0.307 = 2.19) , which resulted in a total indirect effect of 3.17 pounds (p = .014) and indicated that the indirect paths explained 82.6% of the total effect (3.17/3.85). A total of 31% of the indirect effect was related to FV intake change and 69% of the indirect effect is accounted for by the EBI score change.
Figure 2.
Mediation path model depicting how change in fruit & vegetable intake and change in eating behaviors mediate the relationship between experimental group and weight loss. The standard error for each unstandardized coefficient is presented in parentheses. Solid lines are statistically significant at p < .05.
Discussion
This study confirmed our hypothesis that fruit and vegetable intake and EBI scores mediated the effect of the experimental condition on weight loss. The mediation model revealed that the mDIET intervention had positive effects on fruit and vegetable intake and EBI scores that in turn had inverse effects on weight loss. This finding may be interpreted to mean that dietary intake has an influence on the effectiveness of weight loss treatment. This finding is consistent with previous research that indicated that fruit and vegetable intake (Dolecek et al., 1997; Epstein et al., 2001; Weinsier et al., 2009) and healthy eating behaviors (BingBing and Dennis, 2000; Unick et al., 2010; Pellegrini et al., 2011) are related to weight loss.
A unique contribution of the mediation analysis is that the results support behavior change theory that posits that prompts and reminders can serve as cues to action to help change behaviors of interest. The text messages provided performance feedback, encouragement and praise, which are posited as necessary for improving self-efficacy for behavior change (Bandura, 1986). Thus, text-messaging provided a platform for a behavior change intervention that implemented with high theoretical fidelity several of the behavior change techniques identified in Abraham and Michie's (2008) taxonomy drawn from theoretical frameworks such as social cognitive theory, control theory, and operant conditioning. While this study was not a direct test of whether or not a text message-based intervention was more effective than print materials or other intervention channels, the findings do suggest that because of the nature of a text message intervention, it may be a more viable channel for implementing behavior change theory techniques than a static print-based intervention.
Our analysis also suggests that other factors not in the mediation model may contribute to the relationship between the experimental group and weight loss. While a large proportion of the effect of the intervention was explained by the mediating pathways (i.e., 82.6%), the total R2 for weight change was 0.21 indicating that much of the between group variation in weight change was from factors not accounted for in the model and not related to being randomized to the intervention group. Individual differences in motivation to lose weight (Webber et al., 2010; Silva et al., 2011), sedentary time (Sugiyama et al., 2008), and home and neighborhood environment factors (Wegner et al., 2002; French et al., 2011) may explain additional variation in weight change in this sample. We did find that increased physical activity, measured with the 7-Day Physical Activity Recall (Sallis et al., 1985), was related to being in the intervention group but was not statistically related to body weight change and thus would not contribute to explaining the between group variation in weight change. It is also important to note that because positive behaviors can co-vary for individuals trying to lose weight, the mediators in the model may reflect proxy measures of non-measured factors related to weight loss and engagement in the intervention (Kraemer et al., 2001).
There are strengths and limitations of this study. First, 24-hour recalls of fruit and vegetable intake are likely biased as it is known that all types of self-reported dietary measures contain systematic measurement error of under-reporting or over-reporting of certain foods(Ziegler and Filer, 1996; Schatzkin et al., 2003). However, we used multiple 24-hour recalls instead of a single 24-hour recall at each wave, which has been shown to increase their validity (Willett, 1998). Second, the generalizability of the conclusions is limited because the sample was small and was comprised of predominantly Caucasian women. Third, the study was also limited by the short intervention period of 16 weeks. As a result, the amount of weight loss was modest and we do not know if the weight loss changes were maintained for any length of time after the intervention was discontinued, or if further weight loss occurred in either group. Fourth, 20% of the participants did not complete the intervention. Participant dropout was not related to study condition, or to initial status on body weight, EBI scores, or fruit and vegetable consumption. However, the extent of the loss to follow-up and analysis of only cases with complete data could result in biased estimates if change in the mediators or weight change was associated with dropout.
Conclusion
The primary contribution of this study is the identification of intervention mediators that explain how a low intensity and easily disseminated text-message program worked to influence weight loss in the treatment group. These findings suggest that treatments for weight loss that include promotion of fruit and vegetable intake and personalized tailored messages directed at changing eating behaviors can produce modest beneficial health changes at least in the short-term. However, these findings need to be replicated in further studies. Nonetheless, investigators interested in addressing the public health crisis of obesity should consider the findings from this study when designing weight loss interventions.
Highlights.
A path mediation model of weight loss in a randomized trial of a text-message based weight loss intervention is tested.
We hypothesized that fruit/vegetable intake and eating behaviors would be intervention mediators.
In the model the total indirect effect explained 82.6% of the total effect of the intervention on weight loss.
Sending text-messages that promote healthy eating strategies resulted in moderate short-term weight loss.
Acknowledgements
Clinical Trial Registration Number: #NCT00415870.
Sources of Support/Funding
This project was supported by a grant from the National Cancer Institute, R21 CA115615 (PI: Dr. Kevin Patrick).
Appendix I
Eating Behavior Inventory (EBI) Items (O'Neil et al., 1979).
Each behavior on the EBI is rated on a five-point scale: 1) Never or hardly ever; 2) Some of the time; 3) About ½ the time; 4) Much of the time; 5) Always or almost always
I carefully watch the quantity of food that I eat.
I eat foods that I believe will aid me in losing weight.
I keep one or two raw vegetables available for snacks.
I record the type and quantity of food that I eat.
I weigh myself daily.
I refuse food offered to me by others.
I eat quickly compared to most other people.
I consciously try to slow down my eating rate.
I eat at only one place in my home.
I use the same placemat and other utensils for each meal.
I eat and just can't seem to stop.
I eat in the middle of the night.
I snack after supper.
My emotions cause me to eat.
I buy ready to eat snack foods for myself.
I shop when I'm hungry.
I shop from a list.
I leave food on my plate.
I serve food family style.
I watch TV, read, work, or do other things while I eat.
If I'm served too much, I leave food on my plate.
Generally, while I'm at home, I leave the table as soon as I finish eating.
I keep a graph of my weight.
I eat when I'm not really hungry.
I store food in containers where it is not readily visible or in a closed cabinet.
I decide ahead of time what I will eat for meals and snacks.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
Dr. Patrick is co-owner of, and receives income from, Santech, Inc, which is developing products related to the research described in this paper. The terms of this arrangement has been reviewed and approved by the University of California, San Diego, in accordance with their respective conflict of interest policies. Dr. Norman has received consulting income from Santech.
References
- Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Annals of Behavioral Medicine: a publication of the Society of Behavioral Medicine. 2007;34:304–12. doi: 10.1007/BF02874555. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall, Inc; Englewood Cliffs: 1986. [Google Scholar]
- Bell E, Castellanos V, Pelkman C, Thorwart M, Rolls B. Energy density of foods affects energy intake in normal-weight women. American Journal of Clinical Nutrition. 1998;67:412–420. doi: 10.1093/ajcn/67.3.412. [DOI] [PubMed] [Google Scholar]
- BingBing Q, Dennis KE. The adoption of eating behaviors conducive to weight loss. Eating Behaviors. 2000;1:23–31. doi: 10.1016/s1471-0153(00)00003-9. [DOI] [PubMed] [Google Scholar]
- Curioni CC, Lourenço PM. Long-term weight loss after diet and exercise: a systematic review. International Journal of Obesity. 2005;29:1168–74. doi: 10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJL, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine. 2009;6:e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolecek T, Stamler J, Caggiula A, Tillotson J, Buzzard I. Methods of dietary and nutritional assessment and intervention and other methods in the Multiple Risk Factor Intervention Trial. The American Journal of Clinical Nutrition. 1997;65:196S–210S. doi: 10.1093/ajcn/65.1.196S. [DOI] [PubMed] [Google Scholar]
- Duffey KJ, Gordon-Larsen P, Jacobs DR, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. The American Journal of Clinical Nutrition. 2007;85:201–8. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obesity Research. 2001;9:171–8. doi: 10.1038/oby.2001.18. [DOI] [PubMed] [Google Scholar]
- Finkelstein EA, Khavjou OA, Thompson H, Trogdon JG, Pan L, Sherry B, Dietz W. Obesity and severe obesity forecasts through 2030. American Journal of Preventive Medicine. 2012;42:563–570. doi: 10.1016/j.amepre.2011.10.026. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA: The Journal of the American Medical Association. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- French SA, Gerlach AF, Mitchell NR, Hannan PJ, Welsh EM. Household obesity prevention: take Action--a group-randomized trial. Obesity. 2011;19:2082–8. doi: 10.1038/oby.2010.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guthrie JF, Lin B-H, Frazao E. Role of food prepared away from home in the American diet, 1977-78 versus 1994-96: changes and consequences. Journal of Nutrition Education and Behavior. 2002;34:140–50. doi: 10.1016/s1499-4046(06)60083-3. [DOI] [PubMed] [Google Scholar]
- Haapala I, Barengo NC, Biggs S, Surakka L, Manninen P. Weight loss by mobile phone: a 1-year effectiveness study. Public Health Nutrition. 2009;12:2382–2391. doi: 10.1017/S1368980009005230. [DOI] [PubMed] [Google Scholar]
- Hill JO. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–1374. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koplan JP. Caloric imbalance and public health policy. JAMA: the Journal of the American Medical Association. 1999;282:1579–1581. doi: 10.1001/jama.282.16.1579. [DOI] [PubMed] [Google Scholar]
- Kraemer HC. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Stice E, Kazdin AE, Offord DR, Kupfer DJ. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Kruger J, Blanck HM, Gillespie C. Dietary and physical activity behaviors among adults successful at weight loss maintenance. International Journal of Behavioral Nutrition and Physical Activity. 2006;3:17. doi: 10.1186/1479-5868-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. Lawrence Erlbaum; New York, NY: 2008. [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHLBI . Overweight and Obesity. Bethesda, MD: 2007. [Google Scholar]
- O'Neil PM, Currey HS, Hirsch AA, Malcolm RJ, Sexauer JD, Riddle FE, Taylor CI. Development and validation of the Eating Behavior Inventory. Journal of Psychopathology and Behavioral Assessment. 1979;1:123–132. [Google Scholar]
- O'Neil PM, Rieder S. Utility and validity of the Eating Behavior Inventory in clinical obesity research: a review of the literature. Obesity Reviews. 2005;6:209–216. doi: 10.1111/j.1467-789X.2005.00192.x. [DOI] [PubMed] [Google Scholar]
- Patrick K, Intille SS, Zabinski MF. An ecological framework for cancer communication: implications for research. Journal of Medical Internet Research. 2005;7:e23. doi: 10.2196/jmir.7.3.e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K, Raab F, Adams M, Dillon L, Zabinski M, Rock C, Griswold W, Norman G. A text message–based intervention for weight loss: randomized controlled trial. Journal of Medical Internet Research. 2009;11 doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini CA, Verba SD, Otto AD, Helsel DL, Davis KK, Jakicic JM. The comparison of a technology-based system and an in-person behavioral weight loss intervention. Obesity. 2011;20:356–363. doi: 10.1038/oby.2011.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolls BJ, Ello-Martin JA, Tohill BC. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutrition Reviews. 2004;62:1–17. doi: 10.1111/j.1753-4887.2004.tb00001.x. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Haskell W, Wood P, et al. Physical activity assessment methodology in the Five City Project. American Journal of Epidemiology. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. Journal of the American Dietetic Association. 1988;88:1268–71. [PubMed] [Google Scholar]
- Schatzkin A, Kipnis V, Carroll RJ, Midthune D, Subar AF, Bingham S, Schoeller DA, Troiano RP, Freedman LS. A comparison of a food frequency questionnaire with a 24-hour recall for use in an epidemiological cohort study: results from the biomarker-based Observing Protein and Energy Nutrition (OPEN) study. International Journal of Epidemiology. 2003;32:1054–1062. doi: 10.1093/ije/dyg264. [DOI] [PubMed] [Google Scholar]
- Silva MN, Markland D, Carraça EV, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB, Teixeira PJ. Exercise autonomous motivation predicts 3-yr weight loss in women. Medicine and Science in Sports and Exercise. 2011;43:728–37. doi: 10.1249/MSS.0b013e3181f3818f. [DOI] [PubMed] [Google Scholar]
- Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Medicine. 2006;36 doi: 10.2165/00007256-200636030-00005. [DOI] [PubMed] [Google Scholar]
- Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. American Psychologist. 1992;47:22–6. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- Stubbs RJ, Johnstone AM, Harbron CG, Reid C. Covert manipulation of energy density of high carbohydrate diets in “pseudo free-living” humans. International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity. 1998;22:885–92. doi: 10.1038/sj.ijo.0800676. [DOI] [PubMed] [Google Scholar]
- Sugiyama T, Healy GN, Dunstan DW, Salmon J, Owen N. Joint associations of multiple leisure-time sedentary behaviours and physical activity with obesity in Australian adults. The International Journal of Behavioral Nutrition and Physical Activity. 2008;5:35. doi: 10.1186/1479-5868-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unick JL, Jakicic JM, Marcus BH. Contribution of behavior intervention components to 24-month weight loss. Medicine and Science in Sports and Exercise. 2010;42:745–53. doi: 10.1249/MSS.0b013e3181bd1a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velentzis LS, Keshtgar MR, Woodside JV, Leathem AJ, Titcomb A, Perkins KA, Mazurowska M, Anderson V, Wardell K, Cantwell MM. Significant changes in dietary intake and supplement use after breast cancer diagnosis in a UK multicentre study. Breast Cancer Tesearch and Treatment. 2011;128:473–82. doi: 10.1007/s10549-010-1238-8. [DOI] [PubMed] [Google Scholar]
- Wardle J, Parmenter K, Waller J. Nutrition knowledge and food intake. Appetite. 2000;34:269–75. doi: 10.1006/appe.1999.0311. [DOI] [PubMed] [Google Scholar]
- Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self-monitoring and weight loss in a 16-week Internet behavioral weight loss intervention. Journal of Nutrition Education and Behavior. 2010;42:161–7. doi: 10.1016/j.jneb.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Wegner KE, Smyth JM, Crosby RD, Wittrock D, Wonderlich SA, Mitchell JE. An evaluation of the relationship between mood and binge eating in the natural environment using ecological momentary assessment. The International Journal of Eating Disorders. 2002;32:352–61. doi: 10.1002/eat.10086. [DOI] [PubMed] [Google Scholar]
- Weinsier RL, Johnston MH, Doleys DM, Bacon JA. Dietary management of obesity: evaluation of the time-energy displacement diet in terms of its efficacy and nutritional adequacy for long-term weight control. British Journal of Nutrition. 2009;47:367. doi: 10.1079/bjn19820048. [DOI] [PubMed] [Google Scholar]
- Willett W. Nutritional Epidemiology. 2nd ed. Oxford University Press; USA, New York: 1998. [Google Scholar]
- Wing RR, Hill JO. Successful weight loss maintenance. Annual Review of Nutrition. 2001;21:323–41. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- Ziegler EE, Filer LJ. International Life Sciences Institute-Nutrition Foundation. Seventh. ed. ILSI Press; Washington, D.C.: 1996. Present Knowledge in Nutrition. [Google Scholar]