Abstract
Objective
To assess the effectiveness of a hepatitis B virus (HBV) educational program in increasing HBV knowledge.
Methods
Using a cluster randomized control trial to recruit participants from the community-based organization in the Baltimore-Washington Metropolitan Area; a total of 877 Asian American participants completed a self-administered pretest. HBV knowledge was the outcome measure. The intervention group received a 30-minute educational program. After the educational program, the intervention group completed post-education survey. Six months after the education, all participants were followed by phone.
Results
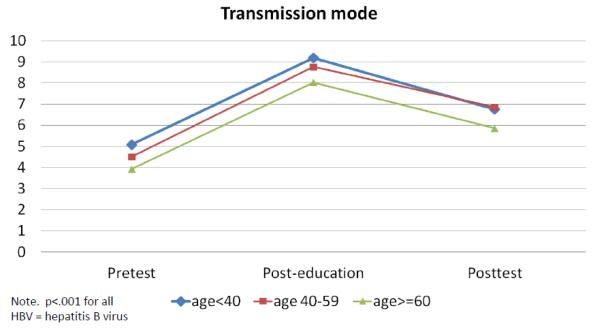
The intervention group showed significantly higher knowledge scores than the control group at the 6-months follow-up (between-group difference was 1.44 for knowledge of transmission modes and 0.59 for sequelae, p < 0.01). For the intervention group, the increase in knowledge of HBV transmission modes in post-education was much higher than that at the 6-month follow-up (4.18 vs. 2.07), p < 0.01) compared to baseline. Age was also an important factor on the educational effect: Those older than 60 years reported the lowest scores in all three points.
Conclusions
Findings suggest that this culturally integrated liver cancer educational program increased HBV knowledge. Differential strategies are needed to target age groups, separately educating those younger and those older.
Keywords: Knowledge of HBV infection, Asian Americans, Health disparity
Introduction
The most recent World Health Organization (WHO) estimates indicate that about 2 billion people worldwide have been infected with the hepatitis B virus (HBV), and that about 350 million live with chronic HBV infection. An estimated 600,000 persons die each year due to acute or chronic consequences of hepatitis B (WHO, 2008). Cirrhosis and primary liver cancer represent approximately 1 of 40 deaths (2.5%) worldwide (WHO, 2008). Approximately 30% of all cases of cirrhosis and 53% of hepatocellular carcinoma (HCC) can be attributed to HBV (Perz et al., 2006). HBV is second only to tobacco as a known human carcinogen (Lee et al., 2011).
In contrast to the vast population of infected persons, efforts to prevent and control HBV have met with increasing levels of success and hold promise for large reductions in disease burden in the future, with a great deal of credit stemming from hepatitis B vaccine (Shepard et al., 2006). In the U.S., however, Asian Americans and Pacific Islanders (AAPIs) account for over half of the 1.2 to 2 million chronic HBV cases (Chao et al., 2009). Approximately 15.5 million AAPIs—about 5% of the U.S. population—have the highest rate of HBV infection (U.S. Census Bureau 2007; Hwang et al., 2010). The number of people who have chronic HBV infection remains high because most AAPIs are immigrants from HBV-endemic areas (Lee et al., 2011). This excess risk can be attributed to high rates of HBV infection—particularly among foreign-born immigrants—combined with low levels of hepatitis B vaccination coverage due to cultural, linguistic, or financial barriers (Choe et al., 2005; Taylor et al., 2004, 2005; Thompson et al., 2003). The U.S. DHHS Office of Minority Health (OMH) warned that chronic HBV and liver cancer caused by HBV among AAPIs is one of the most serious but frequently neglected racial and ethnic health disparities in the U.S. (OMH, 2009).
Research in the U.S. has shown that lack of knowledge about HBV is associated with lack of screening (Taylor et al., 2000, 2002; Thompson et al., 2002). To increase routine screening and vaccination for HBV among AAPIs, sustainable population-based HBV educational interventions are needed to decrease their risk of getting HCC and cirrhosis (Hsu et al., 2010; Juon et al., 2008; Nguyen et al., 2007; Taylor et al., 2000, 2005). Health educational programs for immigrant groups should be based on a thorough understanding of the target population’s health knowledge, beliefs, and practices (Hubbell et al., 1995). Culturally sensitive health initiatives should be implemented in AAPI communities to reduce the burden of chronic HBV infection and eliminate racial disparity in liver cancer incidence and mortality (Wu et al., 2007).
Nearly all studies of HBV knowledge among Asian Americans have focused on HBV awareness. Few studies have examined the effectiveness of culturally sensitive HBV education in improving HBV knowledge at immediate post-education and at 6-month follow-up. To spotlight the need for educational interventions, the goal of our paper was to examine the effect of intervention programs on HBV knowledge among Asian Americans in the Baltimore-Washington Metropolitan Area. To the best of our knowledge, this is the first study to assess changes in HBV knowledge after the post-education and 6-month follow-up.
Material and Methods
Overview of study design
Using a cluster randomized control design, Asian Americans age 18 and older were recruited from Chinese, Korean, and Vietnamese community-based organizations (CBOs) in the Baltimore-Washington Metropolitan Area. Each CBO was randomly assigned to either an intervention or control group. After completing the baseline survey, participants in the intervention group received a culturally integrated 30-minute liver cancer educational program; those in the control group received an English brochure developed by the National Institute of Diabetes and Digestive and Kidney Diseases: “What I need to know about Hepatitis B.” Intervention group participants also completed a post-education survey. After six months, all the participants were followed up and interviewed by telephone. Participants in the control group received a delayed intervention after the follow-up interview. This study protocol was approved by the Institutional Review Board of the Johns Hopkins Bloomberg School of Public Health.
Recruitment procedures
Between November 2009 and June 2010, self-identified Asian American adults in the targeted areas were recruited from various Chinese, Korean, and Vietnamese CBOs such as churches, temples, language schools, college cultural group organizations, Asian grocery stores, restaurants, and nail salons. Organizational membership was not required for participation. Those who had attended a previous educational program on HBV infection and liver cancer prevention were not eligible for our project.
To avoid contamination, the geographic location of participating CBOs was considered. Twenty-seven CBOs (15 for intervention, 12 for control) agreed to participate in our study. Korean participants were recruited predominantly from churches (n = 7, 70% of the organizations for Korean recruitment). Chinese participants were recruited predominantly from language schools (n = 5, 63% of Chinese participating organizations). Vietnamese participants did not have a predominant recruitment site because interventions were scattered in different venues (see more detail, Chen et al., 2012; Strong et al., 2012).
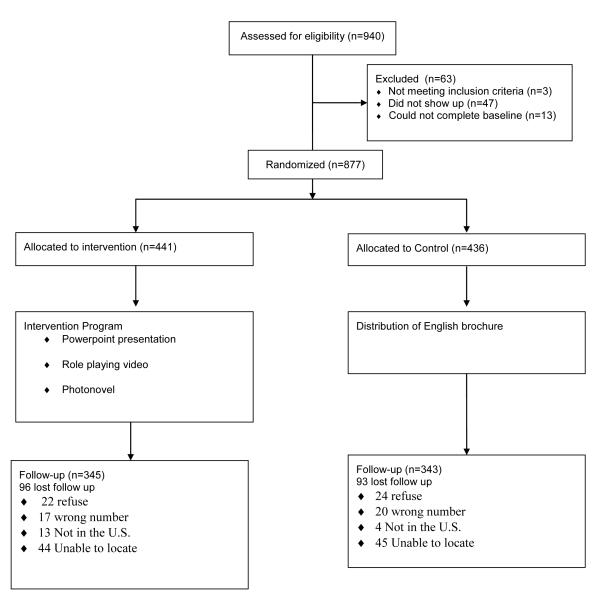
Figure 1 summarizes the study design. Of 940 potentially eligible participants from CBOs, 5% (n=47) did not show up. Of the 893 participants who came, 13 (1.5%) did not complete a baseline survey or did not participate in the education program. Of the total of 877 who completed the baseline survey, 441 (50.3%) were from the intervention group and 436 (49.7%) from the control group. Six month later, the proportions of intervention and control group participants with follow-up were 78.2% (n=345) and 78.7% (n=343), respectively.
Figure 1. Flow of participants through randomized trial.
Intervention
The intervention was developed using the PRECEDE-PROCEED model which can help both in identifying factors affecting health behavior and in developing an educational message (Green and Kreuter, 1991). We also integrated focus group findings to integrate traditional beliefs of Asian Americans (Philbin et al., 2012). The intervention group received a single-session, educational program in their relevant language. Bilingual educators conducted each session after having the standard training.
Follow-up
About 78% (n = 688) of participants completed the phone survey at the 6-month follow-up. Those who dropped out of the study (attrition rate = 21.6%) were not independently associated with the intervention arm, age, gender, marital status, family history of HBV infection, health status, HBV screening, or HBV knowledge. Education, however, was associated with dropouts: Highly educated participants were more likely to follow up than their lower-educated counterparts (57.4% vs. 37.6%, p < 0.01).
Outcome Measures
The outcome measures were knowledge questions related to HBV infection, including the modes of HBV transmission (10 questions) and sequelae of chronic HBV (7 questions). Each correctly answered question was given a point; scores were summed within the two domains and combined to yield the final knowledge composite score. The sum of binary scores ranged from 0 to 10 for questions about modes of HBV transmission (n = 10, alpha = 0.91) and 0 to 7 for sequelae of HBV (n = 7, alpha = 0.78).
Covariates
We collected demographic and family history of HBV infection at pretest. We compared age, gender, education, country of birth, having health insurance, family history of HBV infection, self-reported physical health, and depressive symptoms between the intervention and control groups.
Statistical analysis
We compared baseline characteristics between the intervention and control groups with the Student’s t test for continuous variables and the Pearson’s χ2 test for categorical variables. For the effect of intervention on HBV knowledge, we compared the scores of the intervention and control groups at pretest and 6-month follow-up using t tests. Then, we used paired t tests to examine changes in knowledge scores between baseline and post-education, and between baseline and posttest. We also examined these changes by subgroup of Asian Americans and three age groups (<40, 40–59, ≥60). We analyzed participants data as part of their original random group assignment (n=877), following intent-to-treat (ITT) principles (with baseline values carried forward for missing values). We used STATA version 11 for all analyses (StataCorp, 2009).
Results
Table 1 presents the baseline characteristics for each group. The average age of the 877 respondents was 45.1 years; 58.5% were females; about 13% had less than high school education. Approximately two thirds of the respondents had health insurance. About 14% reported that they had a family history of HBV infection. To compare baseline characteristics between the intervention and control groups, only age differed significantly by intervention group.
Table 1.
Baseline descriptive characteristic, Baltimore-Washington Metropolitan Areas, 20092010
| Characteristics | Total (n=877) |
Intervention (n=441) |
Control (n=436) |
P value |
|---|---|---|---|---|
| Age, years (95%CI) | 45.1 (44.1, 46.1) | 46.9 (45.8, 48.7) | 43.3 (41.9, 44.6) | .03 |
| Women, no. (%) | 513 (58.5) | 254 (57.6) | 259 (59.4) | .63 |
| Country of birth | ||||
| -Korea, no. (%) | 294 (33.5) | 148 (33.6) | 146 (33.5) | .98 |
| -Vietnam, no. (%) | 280 (31.9) | 142 (32.2) | 138 (31.7) | |
| -China, no. (%) | 303 (34.5) | 151 (34.2) | 152 (34.9) | |
| Education, <high school, no. (%) | 116 (13.2) | 60 (13.6) | 56 (12.8) | .43 |
| Having health insurance, no. (%) | 581 (66.2) | 300 (68.0) | 281 (64.4) | .28 |
| Family history of HBVa, no. (%) | 126 (14.4) | 68 (15.5) | 58 (13.4) | .39 |
| Poor self-rated health, no. (%) | 52(5.9) | 26(5.9) | 26(6.0) | .31 |
| Depressed (CES-Db >16), no. (%) | 223 (25.5) | 115 (26.1) | 108 (24.9) | .69 |
| HBV screening (yes), no. (%) | 466 (53.3) | 245 (55.8) | 221 (50.7) | .14 |
| Knowledge of transmission, mean | 4.55 | 4.57 | 4.54 | .88 |
| Knowledge of sequelae , mean | 3.91 | 3.93 | 3.89 | .81 |
Note.
HBV = hepatitis B virus;
Center for Epidemiologic Studies Depression Scale
Across all questions, the percentage of participants who got each item correct increased from baseline to post-education in the intervention group (See Table 2). In the pretest, less than 20% of participants in the intervention group had the correct answer on two questions: (1) eating food that had been pre-chewed by an infected person, and (2) breast feeding from an infected mother. About one third knew that HBV is significantly more contagious than HIV/AIDS.
Table 2.
Hepatitis B knowledge in the intervention group (n=441), Baltimore Washington Metropolitan Areas, 2009-2010.
| Knowledge | Questions | %Right answer Baseline |
%Right answer Post- education |
|---|---|---|---|
| HBV transmission mode (10) |
From infected mother to child during childbirth | 59.2 | 94.6 |
| By eating food prepared by an infected person | 45.2 | 95.0 | |
| By sharing a toothbrush with an infected person | 69.8 | 84.8 | |
| By sharing food with an infected person ^ J | 34.2 | 91.6 | |
| By sharing a razor with an infected person C.SS' | 62.6 | 92.1 | |
| By eating food that has been pre-chewed by an infected person | 16.6* | 62.6 | |
| By being coughed or sneezed by an infected person | 33.1 | 87.3 | |
| By having sexual intercourse with an infected person | 62.2 | 94.6 | |
| By holding hands with an infected person | 65.3 | 96.6 | |
| By breast feeding from an infected mother | 18.4* | 75.5 | |
| Sequelae of HBV (7) |
Hepatitis B can cause liver cancer | 70.3 | 96.1 |
| Chronic hepatitis B causes liver cancer and/or cirrhosis if not properly managed |
82.1 | 99.1 | |
| People with hepatitis B are infected for life | 38.8 | 64.4 | |
| Hepatitis B infection cannot be cured, but the disease can be managed | 52.4 | 76.6 | |
| The majority of chronic hepatitis-B patients have no symptoms | 43.8 | 81.6 | |
| Hepatitis B virus is significantly more contagious than HIV/AIDS | 33.6* | 85.5 | |
| A hepatitis B infected person, who looks and feels healthy, can still spread hepatitis B |
71.9 | 95.9 |
Table 3 shows the comparison of mean changes at the 6-month follow-up between intervention and control groups. These analyses were based on assigned intervention group at the time of randomization regardless of adherence status (i.e., intent-to-treat). The mean score of HBV knowledge increased significantly more in the intervention group than in the control groups (the between-group difference was 1.44 for transmission mode and 0.59 for sequelae, p < 0.01).
Table 3.
Changes in mean knowledge of hepatitis B virus infection at 6-month follow-up between intervention and control groups, Baltimore Washington Metropolitan Areas, 2009-2010
| HBV knowledge | Baseline |
Absolute change from
Baseline |
Between group
difference |
|---|---|---|---|
| Transmission mode** | 1.44** | ||
| Intervention (n=441) | 4.57 | 2.07 | |
| Control (n=436) | 4.54 | 0.63 | |
| Sequelae | 0.59* | ||
| Intervention (n=441) | 3.93 | 1.19 | |
| Control (n=436) | 3.89 | 0.60 |
Note.
p < 0.05;
p < 0.01;
Intent-to-treat method
The changes in HBV knowledge at post-education and at the 6-month follow-up were compared with baseline (see Table 4). In total, the scores of HBV knowledge of transmission modes from baseline to post-education (mean difference = 4.18, p < 0.001) and from baseline to 6-month follow-up (mean differences = 2.07, p < 0.01) increased for the intervention group. The HBV knowledge of sequelae was also significantly increased right after the intervention (mean difference = 2.07, p < 0.01) and at posttest (mean difference = 1.19, p < 0.01). Moreover, a dramatic increase in post-education was noted which was a much higher increase than posttest. For the control group, both knowledge scores were increased from baseline to posttest; however, the intervention group increased knowledge scores greater than the control group. Further analyses by subgroups of Asian Americans (i.e., Chinese, Korean, Vietnamese) showed the similar trend. All intervention effects were statistically significant.
Table 4.
Changes in mean knowledge of hepatitis B virus infection from baseline, post-education, and 6-month follow-up, Baltimore Washington Metropolitan Areas, 2009-2010
|
Baseline
(T1) |
Post-
education (T2) |
6-month
(T3) |
Change from
Tl toT2 |
Change from
Tlto T3 |
|
|---|---|---|---|---|---|
| Transmission mode | |||||
| Total (n=877)a | |||||
| Intervention | 4.57 | 8.75 | 6.64 4.18 | 2.07 | |
| Control | 4.54 | N/A | 5.17 | 0.63 | |
| Chinese (n=303) | |||||
| Intervention | 4.87 | 8.79 | 7.00 | 3.91 | 2.13 |
| Control | 5.01 | N/A | 5.58 | 0.57 | |
| Korean (n=294) | |||||
| Intervention | 4.13 | 8.80 | 5.91 | 4.68 | 1.78 |
| Control | 4.08 | N/A | 4.73 | 0.65 | |
| Vietnamese (n=280) | |||||
| Intervention | 4.70 | 8.64 | 7.03 | 3.94 | 2.33 |
| Control | 4.52 | N/A | 5.19 | 0.67 | |
| Sequelae | |||||
| Total (n=877) | |||||
| Intervention | 3.93 | 5.99 | 5.12 | 2.07 | 1.19 |
| Control | 3.89 | N/A | 4.49 | 0.60 | |
| Chinese (n=303) | |||||
| Intervention | 4.23 | 6.42 | 5.47 | 2.19 | 1.24 |
| Control | 4.58 | N/A | 5.16 | 0.59 | |
| Korean (n=294) | |||||
| Intervention | 3.41 | 5.64 | 4.53 | 2.22 | 1.12 |
| Control | 3.48 | N/A | 4.27 | 0.79 | |
| Vietnamese (n=280) | |||||
| Intervention | 4.14 | 5.92 | 5.35 | 1.77 | 1.21 |
| Control | 3.58 | N/A | 3.99 | 0.41 | |
Note. p < 0.001 for all;
Intent-to-treat method
To better understand the age effect on the educational program, we looked at the changes of knowledge score in three age groups (<40; 40-59; >60) in the intervention group. Figure 2 shows those older than 60 years reported the lowest knowledge scores of transmission mode in all three points. This age pattern was similar in knowledge of sequelae (figure not shown).
Figure 2. Changes of HBV knowledge scores by age for intervention group.
Discussion
Our study examined whether the lack of general knowledge of HBV and liver cancer prevention among Asian Americans can be reversed by a single session of culturally integrated education, with the increase of knowledge measured at post-education and 6-month follow-up compared to baseline knowledge. Our results are consistent with studies which demonstrated that culturally integrated HBV educational programs among Asian Americans substantially improved HBV and liver cancer prevention knowledge (Chao et al., 2009; Hsu et al., 2007; 2010). The consequence of high post-education knowledge scores is likely to improve HBV screening behavior of these high-risk populations. Indeed, higher knowledge of HBV was found to be predictive of HBV screening and liver cancer prevention behaviors (Lai et al., 2007; Ma et al., 2007). Communicating knowledge and potential actions that could reduce exposure to known risk factors is a critical cancer prevention strategy (Hiatt et al., 1999). Across the cancer control continuum, higher knowledge plays a crucial role in both primary and secondary prevention (Viswanath et al., 2006). It is widely accepted that increasing knowledge is an important step in the causal chain leading to health behaviors. Our study is unique in its focus in examining the changes of knowledge at multiple points—pretest, post-education, posttest—with a comparison group. This will help with the development of educational strategies that need additional attention in the future.
This culturally relevant HBV education designed specifically for Asian Americans in the target population’s languages significantly increased HBV knowledge. Especially, four out of five participants in the intervention group did not know two important transmission modes of HBV infection: eating food that had been pre-chewed by an infected person, breast feeding from an infected mother. After the educational session, they improved their knowledge of HBV by listening to a PowerPoint presentation and asking questions; however, a single-session community-based intervention alone did not overcome gaps by increasing their liver cancer awareness or by maintaining it to the extended period. Participants dramatically increased their knowledge at post-education; six months later, they increased their knowledge higher than pretest but lower than post-education. The results of our study suggest that we should continue to provide this type of educational program to keep up high-risk community members’ knowledge of HBV.
Similar to a previous study (Hsu et al., 2010), age was an important factor relating to changes of knowledge regarding HBV. Despite our focus on developing the simplest, clearest educational program possible—with adherence to cultural and linguistic needs to deliver the educational materials effectively—we found that older participants still learned significantly less than younger participants. The finding here is consistent with studies that suggest that older adults learn less health information than younger adults, regardless of the familiarity of the information (Brown et al., 2002; Pruthi et al., 2005). Lower post-education knowledge among older participants compared to younger counterparts can be attributed to low baseline HBV knowledge and low uptake of the information from educational materials among older adults (Mah et al., 1992). There is a call for implementation of specific educational programs for target age groups, separately educating those younger and those older.
This study had several limitations. A sampling frame from CBOs was used, but to minimize the sampling bias due to excluding those who do not attend these organizations regularly, we targeted Asian groceries, nail salons, and restaurants. Nevertheless, the majority of the sample was from the CBOs, so the study cannot be generalized to other Asian Americans who do not regularly attend any of the CBOs. Second, we cannot fully predict future preventive behaviors solely from increased HBV knowledge. Hence, our findings should be put together with additional information about HBV education of other Asian Americans throughout the U.S. to build a comprehensive understanding of this diverse high-risk population.
Our findings have implications for future interventional studies in light of our finding that older age is significantly associated with lower post-education and posttest knowledge, targeting intervention strategies to older participants are of value. Thus, differential educational strategies based on age group should be implemented. Finally, as many Korean Americans attend church, intervention strategies through churches will be effective to provide health education and ancillary health services. As many Chinese American children attend Chinese schools, intervention strategies through Chinese school will be effective.
Highlights.
This culturally integrated liver cancer education program has increased HBV knowledge and awareness among Asian Americans.
The intervention group showed significantly higher knowledge scores than the control group at the 6-month follow-up.
The increase in knowledge in post-education was much higher than that at the 6-month follow up compared to baseline
Differential educational strategies are needed to target subgroups of Asian Americans in consideration of age.
Acknowledgement
This research was supported by grant R25CA129042. We thank all participants of this study. We also appreciate the dedicated work of members of the research team.
Glossary
Abbreviations
- HBV
hepatitis B virus
- HCC
hepatocelluar carcinoma
- CES-D
Center for Epidemiologic Studies Depression Scale
- CBO
community-based organization
- AAPI
Asian American and Pacific Islander
- ITT
intent-to-treat
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Brown SC, Park DC. Roles of age and familiarity in learning health information. Educational Gerontology. 2002;28:695–710. [Google Scholar]
- Chao SD, Chang ET, Le PV, Prapong W, Kiernan M, So SK. The Jade Ribbon Campaign: a model program for community outreach and education to prevent liver cancer in Asian Americans. J Immigr Minor Health. 2009;11:281–290. doi: 10.1007/s10903-007-9094-2. [DOI] [PubMed] [Google Scholar]
- Chao SD, Chang ET, So SK. Eliminating the threat of chronic hepatitis B in the Asian and Pacific Islander Community: A call to action. Asian Pacific J Cancer Prev. 2009;10:1–6. [PubMed] [Google Scholar]
- Chen L, Juon HS, Lee S. Acculturation and BMI among Chinese, Korean and Vietnamese Adults in Maryland. J Community Health. 2012;37:539–46. doi: 10.1007/s10900-011-9476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choe JH, Chan N, Do HH, Woodall E, Lim E, Taylor VM. Hepatitis B and liver cancer beliefs among Korean immigrants in western Washington. Cancer. 2005;104:2955–2958. doi: 10.1002/cncr.21518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiatt RA, Rimer BK. A new strategy for cancer control research. Cancer, Epidemiology, Biomarkers and Prevention. 1999;8:957–964. [PubMed] [Google Scholar]
- Hsu CE, Zhang G, Yan FA, Shang N, Le TJ. What made a successful hepatitis B program for reducing liver cancer disparities: an examination of baseline characteristics and educational intervention, infection status, and missing responses of at-risk Asian Americans. J Community Health. 2010;35:325–35. doi: 10.1007/s10900-010-9238-5. [DOI] [PubMed] [Google Scholar]
- Hsu C, Liu LC, Juon HS, Chiu YW, Bawa J, Tillman U, Li M, Miller J, Wang M. Reducing Liver Cancer Disparities: A community-based hepatitis-B prevention program for Asian-American communities. Journal of National Medical Association. 2007;99:900–907. [PMC free article] [PubMed] [Google Scholar]
- Hubbell FA, Chavez LR, Mishra SI, Magana JR, Burciaga Valdez R. From ethnography to intervention: Developing a breast cancer control program for Latinas. Natl Cancer Inst Monogr. 1995;18:109–15. [PubMed] [Google Scholar]
- Hwang JP, Mohseni M, Gor BJ, Wen S, Guerrero H, Vierling J. Hepatitis B and Hepatitis C prevalence and treatment referral among Asian Americans undergoing community-based hepatitis screening. American Journal of Public Health. 2010;100:S118–S124. doi: 10.2105/AJPH.2009.162776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon HS, Strong C, Oh TH, Castillo T, Tsai G. Public health model for prevention of liver cancer among Asian Americans. J Community Health. 2008;33:199–205. doi: 10.1007/s10900-008-9091-y. [DOI] [PubMed] [Google Scholar]
- Green LW, Kreuter MW. Health promotion panning: an educational and environmental approach. Mountain View; Mayfield, CA: 1991. [Google Scholar]
- Lee H, Hann HW, Yang JH, Fawcett J. Recognition and management of HBV infection in a social context. J Cancer Educ. 2011;26:S1–S6. doi: 10.1007/s13187-011-0203-5. [DOI] [PubMed] [Google Scholar]
- Lai CL, Nguyen TT, Hwang J, Stewart SL, Kwan A. Provider knowledge and practice regarding hepatitis B screening in Chinese-speaking patients. JCancer Educ. 2007;22:37–41. doi: 10.1007/BF03174373. [DOI] [PubMed] [Google Scholar]
- Ma GX, Fang CY, Shive SE, Toubbeh J, Tan Y, Siu P. Risk perceptions and barriers to hepatitis B screening and vaccination among Vietnamese immigrants. J Immigr Minor Health. 2007;9:213–220. doi: 10.1007/s10903-006-9028-4. [DOI] [PubMed] [Google Scholar]
- Mah Z, Bryant H. Age as a factor in breast cancer knowledge, attitudes and screening behavior. Canadian Medical Association Journal. 1992;146:2167–2174. [PMC free article] [PubMed] [Google Scholar]
- Nguyen TT, Taylor VM, Chen MS, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge and screening among Asian Americans. J Cancer Educ. 2007;22:266–272. doi: 10.1007/BF03174128. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health [Accessed May 2011];National hepatitis B initiative for Asian American and Pacific Islanders. 2009 http://www.omhrc.gov/templates/browse.aspx?lvl=2&lvlid=190.
- Perz JF, Armstrong GL, Farrington LA, Hutin YJF, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. Journal of Hepatology. 2006;45:529–538. doi: 10.1016/j.jhep.2006.05.013. [DOI] [PubMed] [Google Scholar]
- Philbin MM, Erby LAH, Lee S, Juon HS. Hepatitis B and liver cancer among three Asian American sub-groups: A focus group inquiry. J Immigr Minor Health. 2012;14:858–68. doi: 10.1007/s10903-011-9523-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruthi RS, Tornehl C, Gaston K, Lee K, Moore D, Carson CC, Wallen EM. Impact of race, age, income, and residence on prostate cancer knowledge, screening behavior, and health maintenance in siblings of patients with prostate cancer. European Urology. 2005;50:64–69. doi: 10.1016/j.eururo.2005.09.024. [DOI] [PubMed] [Google Scholar]
- Shepard CW, Simard EP, Finelli L, Fiore AE, Bell BP. Hepatitis B virus infection: epidemiology and vaccination. Epidemiol Rev. 2006;28:112–125. doi: 10.1093/epirev/mxj009. [DOI] [PubMed] [Google Scholar]
- StataCorp . Stata Statistical Software. Release 11.0 Stata Corporation; College Station, TX: 2009. [Google Scholar]
- Strong C, Lee S, Tanaka M, Juon HS. Ethnic differences in prevalence and barriers of HBV screening and vaccination among Asian Americans. J Community Health. 2012;37:1071–80. doi: 10.1007/s10900-012-9541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Yasui Y, Burke N, Nguyen T, Chen A, Acorda E, Choe JH, Jackson JC. Hepatitis B testing among Vietnamese American men. Cancer Detection and Prevention. 2004;28:170–177. doi: 10.1016/j.cdp.2004.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. J Community Health. 2005;30:477–490. doi: 10.1007/s10900-005-7282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Jackson JC, Chan N, Kuniyuki A, Yasui Y. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. J Community Health. 2002;27:151–163. doi: 10.1023/a:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VM, Jackson JC, Pineda M, Pham P, Fischer M. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. J Cancer Educ. 2000;15:51–55. doi: 10.1080/08858190009528654. [DOI] [PubMed] [Google Scholar]
- Thompson MJ, Taylor VM, Jackson JC, Yasui Y, Kuniyuki A, Tu SP, Hislop TG. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. Journal of Cancer Education. 2002;17:222–226. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- Thompson MJ, Taylor VM, Yasui Y, Hislop TG, Jackson JC, Kuniyuki A, Teh C. Hepatitis B knowledge and practices among Chinese Canadian women in Vancouver, British Columbia. Canadian Journal of Public Health. 2003;94:281–286. doi: 10.1007/BF03403606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau [Accessed April 2011];American Community Survey. 2007 http://www.census.gov/acs/www/index.html.
- Viswanath K, Breen N, Meissner H, Moser RP, Hesse B, Steele WR, Rakowski W. Cancer knowledge and disparities in the information age. Journal of Health Communication. 2006;11:S1–S17. doi: 10.1080/10810730600637426. [DOI] [PubMed] [Google Scholar]
- Wu CA, Lin SY, So SK, Chang ET. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco bay area, California. Asian Pacific J Cancer Prev. 2007;8:127–134. [PubMed] [Google Scholar]
- World Health Organization [Accessed April 2011];Hepatitis B. 2008 http://www.who.int/mediacentre/factsheets/fs204/en/