Abstract
INTRODUCTION
Cutaneous metastasis from gastric cancer is a rare occurrence. The linitis gastric carcinoma accounts only 8.7% of all gastric cancers.
PRESENTATION OF CASE
We report a case of female patient who was followed for linits cancer with peritoneal metastasis treated by six cycles of chemotherapy. After seventeen months of control, the relapse of the disease revealed by occurrence of cutaneous metastatsis.
DISCUSSION
Cutaneous metastasis from linit gastric is rare and the prognostic remains poor. The treatment is palliative.
CONCLUSION
This rare presentation should encourage the practitioners to biopsy any suspicion skin lesion.
Keywords: Cutaneous metastasis, Linitis gastric
1. Introduction
Cutaneous metastases from gastric cancer are very rare. Skin represents a common site for metastases from melanoma, lung, breast and colon cancers.1 The incidence of cutaneous metastases of the upper digestive tract carcinomas and of all gastric cancer is respectively less than 1% and 0.8%.2,3 They can occur as the first sign of the tumour or appear late during the course of the disease.4
We report the case of a female patient who presented initially a gastric linitis with peritoneal metastasis treated by six cycles of Epirubicine, Oxaliplatine and capecitabine. A partial response was first noted, but seventeen months later she presented a relapse revealed by cutaneous metastasis.
2. Case report
A 71-year-old woman was hospitalized because chronic diarrhea evolving for four months associated with weight loss of fifteen kilograms during one year. There was no abdominal pain or rectal syndrome. The clinical examination was unremarkable. The endoscopy revealed a non stenotic parietal infiltration of the gastric antrum. Histologic analysis found an infiltrating adenocarcinoma with dissociated cells. The tumour did not express Human epidermal growth-factor receptor 2. The abdominal computed tomography (CT) scan revealed an invasion of the stomach, peritoneal carcinomatosis and ascitis (Fig. 1). The computed tomography of the thorax and the blood electrolytes were normal. The oncological markers were elevated: ACE at 44 U/ml and CA 19-9 at 749 U/ml. The disease was staged at IV.
Fig. 1.

Abdomen scanner showed an infiltration of the gastric wall with peritoneal carcinomatosis and ascitis.
Our patient was treated by six cycles of chemotherapy including Epirubicin 50 mg/m2 intravenous bolus on one day every three weeks, oxaliplatine (Eloxatin) 130 mg/m2 intravenous over 2 h on one day every three weeks, and capecitabine (xeloda) 1250 mg/m2 oral continuously. During treatment, she presented a sensitive neuropathy grade I as side effect. A partial response was obtained after 6 cycles, with a gain of weight and a decrease the levels of biomarkers.
After seventeen months of good control of the disease, we noted the apparition of nodular lesion of the skin in the flank and the arm (Fig. 2).
Fig. 2.

Photo shows the occurrence a lesion in the arm. It was nodular, erythematous and well circumscribed with a size of 3 cm.
The lesion was not pruriginous and did not increase in size. An opinion dermatologic was then requested to identify the nature of the lesion. The biopsy was recommended and confirmed the diagnostic of cutaneous metastasis of gastric linitis (Figs. 3 and 4).
Fig. 3.
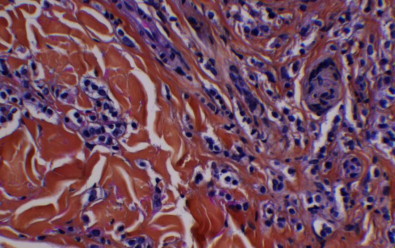
Skin histology shows an diffuse infiltration of subcutaneous tissue by signet ring tumour (hematoxylin and eosin: magnification 400×).
Fig. 4.
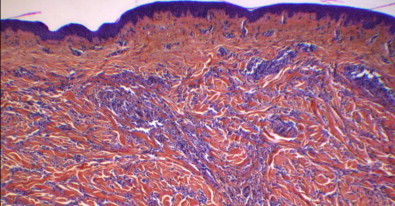
Skin histology shows an diffuse inflitration of subcutaneous tissue by signet ring tumour (hematoxylin and eosin: magnification 40×).
Clinically, the patient is asymptomatic. The computed tomography of the thorax and the abdomen found other lesions and confirmed the progression of the disease. Furthermore, the oncological blood markers were elevated. Subsequently, the patient was given chemotherapy with irinotecan at a dose of 180 mg per square (J1) and leucovorine 400 mg per square, fluoruracil at 400 mg per square in bolus and then 2400 mg per square on 46 h. The patient receives six cycles of chemotherapy whose tolerance was correct. After six cycles, taking into account of alteration of the clinical status with a performance status 3, we decided to establish a best supportive care.
3. Discussion
The cutaneous metastases represent 0.8% of all gastric cancers.3 The linitis gastric carcinoma accounts only 8.7% of all gastric cancers.5
A systemic medline database search on pubmed was conducted using the keywords the following Mesh “stomach neoplasms, skin metastases”. We found forty-one cases reported in the literature.
Among women, Breast cancer is the first cause of cutaneous metastases. The trunk and particulary the umbilical area, is a favored site.6
The term linitis gastric was first used by Brinton in 1854 who describe a diffuse increase in the connective tissue of the stomach. Then, H.M. Lyle reported a first exaustive study in 1911.7
On endoscopic examination, linitis gastric is characterized by thickened gastric folds and the rigidity of the involved portion of the stomach. The endoscopic biopsy has a sensibility of 50% only. Histologically, the linitis gastric corresponds to signet ring cells in a fribrous stroma.
The immunohistologic exam must be carried to differenciate between secondary and primary tumour. The markers which recommended are GCDFP, PSA, TTF1, and estrogen and progesterone receptors. Nerverthless, melanoma and lymphoma are the also the differential diagnosis with signet ring cell carcinoma.8
Typically, linitis gastric is very aggressive disease, it infiltrates the gastric wall with involvement of peritoneum, lymph nodes. Metastatic of the skin is rare. It can probably be explained by haematogenous dissemination. No data are available in the literature regarding the physiopathology.
Cutaneous metastases may be the first indication of gastric cancer, but they can also occur some months or years after the diagnosis of the disease.9 In our case, the metastases are metachronous and they revealed the progression of the disease.
Clinically, as comparing with skin metastasis of the other cancer, we note no difference concerning the characteristic of the lesion. They usually appear as a single or multiples nodules, showing zosteriform or allergic contact dermatitis-like aspect, or as erysipelatoides carcinoma or cellulitis-like patterns.
The treatment of metastatic linitis gastric is palliative. The chemotherapeutic agents used 5-fluorouracil, cisplatine and adriamycine. About twenty of patients with failure of first line chemotherapy receive second line chemotherapy. It is based on trastuzumab with active chemotherapy with cisplatin and fluoropyridine for patients who are HER 2-neu positive, if not used as first line therapy.10
Irinotecan improves survival compared with best supportive care in patients with advanced gastric cancers who progress within six months after first line chemotherapy (median 4.0 versus 2.4 months; P = 0.023), Furthermore, Docetaxel and Paclitaxel show an activity with a response of 20%. For the patients who relapse > 3 months after first line chemotherapy, we can discuss with the patient the same treatment used in first line.11
Skin metastases are still a sign of poor prognosis. Indeed, Bordin and Weitzner reported that the duration of survival from the time of diagnosis of metastatic carcinoma in the skin is about 11.4 weeks, with a range of 2–34 weeks.12 The treatment is palliative.
For our case, there is an interval of twenty weeks since the diagnosis of the cutaneous metastasis.
4. Conclusion
In conclusion, we reported an unusual case of gastric cancer which was treated and showed an arm and flank skin relapse after seventeen months. This should encourage the practitioners to biopsy any suspicious skin lesion in patients with cancer history.
Conflict of interest statement
None.
Funding
None.
Consent
Written informed consent was obtained from the patient of the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal of request.
Author contributions
Mouna Kairouani participated in the care of the patient and wrote the article. Julie Perrin, Anne Dietemann-Barabinot and Rafik Diab participated in the care of the patient. Stephane Ruck validated content and form of the article. All authors read and approved the final manuscript.
References
- 1.Leffell D.J., Carucci J.A. Management of skin cancer. In: Devita V.T., Hellman S., Rosenberg S.A., editors. Cancer: principles and practice of oncology. 6th ed. Lippincott Williams & Wilkins; Philadelphia: 2001. pp. 1976–2002. [Google Scholar]
- 2.Brownstein M.H., Helwing E.B. Metastatic tumors of the skin. Cancer. 1972;29:1298–1307. doi: 10.1002/1097-0142(197205)29:5<1298::aid-cncr2820290526>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 3.Hu S.C., GS Chen G., Wu C.S., Chai C.Y., Chen W.T., Lan C.C. Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical center. Journal of American Academy of Dermatology. 2009;60:379–387. doi: 10.1016/j.jaad.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Beerman H. Some aspects of cutaneous maligancy. Archives of Dermatology. 1996;99:617–626. doi: 10.1001/archderm.99.5.617. [DOI] [PubMed] [Google Scholar]
- 5.Kim D.Y., Park Y.K., Joo J.K., Ryu S.Y., Kim Y.J., Kim S.K. Clinicopathological characteristics of signet ring cell carcinoma of the stomach. ANZ Journal of Surgery. 2004;74(December (12)):1060–1064. doi: 10.1111/j.1445-1433.2004.03268.x. [DOI] [PubMed] [Google Scholar]
- 6.Powell F.C., Coope A.J., Massa M.C. Sister Mary Joseph's nodule: a clinical and histologic study. Journal of the American Academy of Dermatology. 1984;10:610–615. doi: 10.1016/s0190-9622(84)80265-0. [DOI] [PubMed] [Google Scholar]
- 7.Albert F.R. Linitis plastic. The Lancet. 1923;202(5213):181–182. [Google Scholar]
- 8.Rutten A., Huschka U., Requena C., Rodriguez-Peralto J.L. Primary cutaneous signet-ring cell melanoma: a clinic-pathologic and immunohistochemical study of two cases. The American Journal of Dermatopathology. 2003;25(5):418–422. doi: 10.1097/00000372-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Browstein M.H., Helwig E.B. Patterns of cutaneous metastasis. Archives of Dermatology. 1973;107:80–86. [PubMed] [Google Scholar]
- 10.The NCCN guidelines for practice cancer; 2012.
- 11.Okines A., Verheij M.J., Allum W. Gastric cancer: Esmo Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology. 2010;21(Suppl. 5):V50–V54. doi: 10.1093/annonc/mdq164. [DOI] [PubMed] [Google Scholar]
- 12.Bordin G.M., Weitzner S. Cutaneous metastases as a manifestation of internal carcinoma: diagnostic and prognostic significance. The American Journal of Surgery. 1972 [PubMed] [Google Scholar]


