Abstract
INTRODUCTION
We report the case of a 66-year-old female undergoing elective nephrectomy for a non-functioning kidney in whom an incidental renocolic fistula was detected.
PRESENTATION OF CASE
She presented with recurrent urinary tract infections and left flank pain. Investigations revealed a nonfunctioning left kidney with a large staghorn calculus and features suggestive of xanthogranulomatous pyelonephritis (XPG). At nephrectomy, an incidental renocolic fistula was found and excised.
DISCUSSION
XGP is a rare, chronic inflammatory disorder of the kidney characterized by a destructive mass invading the renal parenchyma. Renocolic fistulae complicating XGP are uncommon and not widely reported in the literature.
CONCLUSION
Herein, we describe a case of XGP with renocolic fistula formation, its management and a review of the literature.
Keywords: Incidental, Renocolic, Fistula, Xanthogranulomatous, Pyelonephritis
1. Introduction
We report the case of a 66-year-old female undergoing elective nephrectomy for a non-functioning kidney in which an incidental renocolic fistula was detected. Histological analysis confirmed the presence of xanthogranulomatous pyelonephritis. She recovered well post-operatively.
2. Case
A 66-year-old female was referred to the Urology outpatient department with recurrent urinary tract infections over a ten-year period. She described ongoing left flank pain, increased frequency of micturition and intermittent dysuria. There was no haematuria or pneumaturia. Urine analyses revealed persistent pyuria with mixed colony count growth. Routine renal biochemistry was normal.
Plain films and ultrasound imaging of the left kidney demonstrated a large staghorn calculus filling the upper pole and middle calyces. A DMSA renogram demonstrated a non-functioning left kidney. Non-contrast CT revealed marked thinning of the left renal cortex and features suggestive of xanthogranulomatous pyelonephritis. The ureter was distended throughout its length (Fig. 1).
Fig. 1.
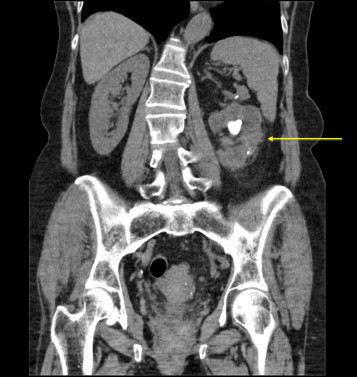
A non-contrast CT demonstrating a markedly thinned cortex with pernephric stranding and a large calculus. Features are suggestive of xanthogranulomatous pyelonephritis.
An elective left simple nephrectomy was planned. At nephrectomy, following division of a single renal artery and vein, the anteromedial renal cortex was found adherent to, and fistulating into the proximal descending colon (Figs. 2 and 3). The bowel was carefully dissected from the kidney and a small enterotomy was oversewn. Pus aspirated from the kidney cultured Proteus mirabilis.
Fig. 2.
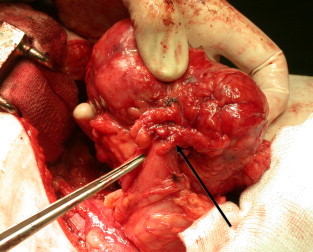
Arrow demonstrating bowel adherent to antermedial renal cortex.
Fig. 3.
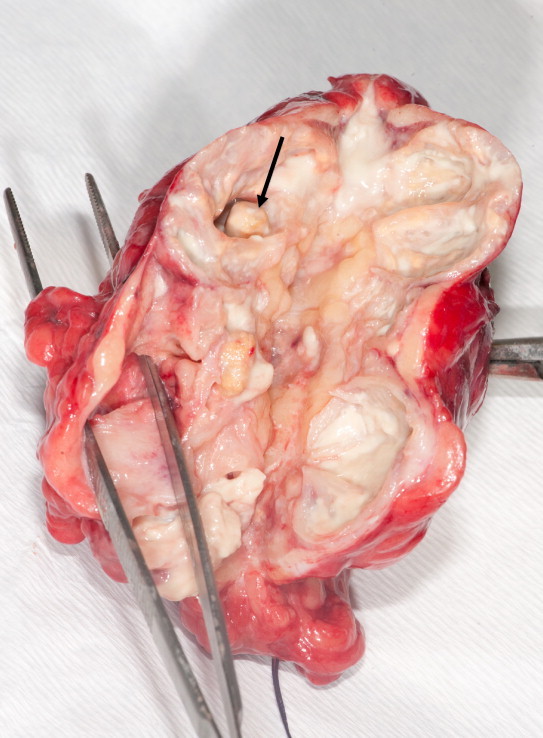
Abnormal kidney with thin cortex and multiple stones within the collecting system (arrow). Extensive pus present. Forceps demonstrates the fistulous tract through the cortex.
Histopathological analysis of the kidney showed renal calculi with associated xanthogranulomatous pyelonephritis. There was a segment of colonic mucosa attached to the renal parenchyma with extensive inflammation and fibrosis, consistent with a renocolic fistula.
The patient recovered well post-operatively. Upon review in the outpatients, her presenting flank pain and urinary tract infections had resolved.
3. Discussion
Xanthogranulamatous pyelonephritis (XGP) was first described by Schlagenhaufer in 1916.1 It is a process characterized histopathologically by suppuration, renal parenchymal destruction and the presence of lipid–laden foamy macrophages. XGP is more common in females, usually during the fifth and sixth decades of life, although it can occur at any age. It is rare in the pediatric population.2 It affects both kidneys with equal frequency. Its incidence is reported to be approximately 8% found in all kidneys removed or biopsied for inflammatory renal conditions (excluding glomerulonephritis).3
The precise aetiology is unknown however it is thought to occur in association with infection and/or chronic urinary tract obstruction such as staghorn calculi.4 Urinary tract calculi are present in 70–79% of patients with XGP.5 Other contributory factors are thought to include diabetes mellitus, immunocompromised states and abnormal lipid metabolism.
XGP can behave and appear somewhat like a renal cell carcinoma. It can locally invade into adjacent structures with reported cases involving the spleen, pancreas or duodenum. Grossly, it appears as a mass of yellow tissue with focal necrosis and hemorrhage.
Malek and Elder6 described a classification system of XGP based upon the extent of inflammation of the kidney and its adjacent tissue:
Stage 1: localized disease confined to the renal parenchyma,
Stage 2: involving perinephric fat,
Stage 3: extending into Perinephric spaces.
The presentation is variable and patients may complain of a dull, persistent flank ache and associated fevers, malaise and weight loss. Urine cultures are often positive for Escherichia coli and Proteus species (found in up to 95% of positive cultures). The radiological diagnosis is suggestive but non specific, as appearances can be similar to those of a renal cell carcinoma.
Definitive treatment is en bloc surgical resection of the kidney. Usually this is a unilateral process however, in the rare case of bilateral XGP, successful bilateral partial nephrectomy has been performed.7
Renocolic fistulae are an uncommon complication of XGP with no large case series in the literature. Other reported fistula formation in XGP include enterocutaneous and nephrocutaneous fistualtions. Parsons et al.3 described the first series of four patients with fistula formation in XGP, including the first reported case of a pediatric XGP with renocolic fistula formation. One of the four patients had a pre-operative diagnosis of a renocolic fistula following retrograde pyelography. Majeed et al.8 similarly describe a series of four cases of renocolic fistulae with underlying XGP. Within these four cases, all of the renocolic fistulae were identified incidentally intraoperatively and pre-operative imaging did not detect the presence of a fistula. It is possible that impacted stone in the presence of infection could cause necrosis of the thinned cortex with perinephric abscess formation and perforation into the adjacent colon.9
Radiological diagnosis of a renocolic fistula in the setting of XGP is often difficult in the absence of clinical suspicion. CT and barium enema appear to have limited roles in identifying renocolic fistulae however retrograde pyelography has been utilized to radiologically confirm the presence of a fistula.4,10
Our case describes an unusual finding of a renocolic fistula which was incidentally found at the time of nephrectomy and was not suggested on pre-operative imaging. We present a pictorial account of the fistula's appearance and management. Ultimately, nephrectomy and excision of the fistula is the recommended treatment of choice.
4. Conclusion
We conclude that the potential complication of an xanthogranulomatous pyelonephritic kidney fistulating into adjacent structures should be considered in patients who present for nephrectomy with a suspected diagnosis of xanthogranulomatous pyelonephritis.
Conflict of interest statement
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Ronan McDermott – first author; Catherine Dowling – second author
Mazen Alsinnawi – third author
Ronald Grainger – consultant surgeon/fourth author
References
- 1.Schlagenhaufer F. Ueber eigentumliche Staphylomykosen der Nieren und des pararenalen Bindegewebes. Frankfurter Zeitschrift fur Pathologie. 1916;19:139–148. [Google Scholar]
- 2.Yazaki T., Ishikawa S., Ogawa Y., Takahashi S., Nemoto S., Rinsho K. Xanthogranulomatous pyelonephritis in childhood: case report and review of English and Japanese literature. Journal of Urology. 1982;127:80–83. doi: 10.1016/s0022-5347(17)53616-2. [DOI] [PubMed] [Google Scholar]
- 3.Parsons M.A., Harris S.C., Grainger R.G., Ross B., Smith J.A., Williams J.L. Fistula and sinus formation in xanthogranulomatous pyelonephritis. A clinicopathological review and report of four cases. British Journal of Urology. 1986;58(5):488. doi: 10.1111/j.1464-410x.1986.tb05452.x. [DOI] [PubMed] [Google Scholar]
- 4.Zafranloo S., Gerard P.S., Bryk D. Xanthogranulomatous pyelonephritis in children: analysis by diagnostic modalities. Urologic Radiology. 1990;12:18–21. doi: 10.1007/BF02923958. [DOI] [PubMed] [Google Scholar]
- 5.Rafal R.B., Kosovsky P.A., Markisz J.A. Xanthogranulomatous pyelonephritis in an infant. Urology. 1991;37:553–556. doi: 10.1016/0090-4295(91)80323-y. [DOI] [PubMed] [Google Scholar]
- 6.Malek R.S., Elder J.S. Xanthogranulomatous pyelonephritis. A critical analysis of 26 cases and of the literature. Journal of Urology. 1978;119:589–593. doi: 10.1016/s0022-5347(17)57559-x. [DOI] [PubMed] [Google Scholar]
- 7.Perez L.M., Thrasher J.B., Anderson E.E. Succussful management of bilateral xanthogranulomatous pyelonephritis by bilateral partial nephrectomy. Journal of Urology. 1993;149:100. doi: 10.1016/s0022-5347(17)36011-1. [DOI] [PubMed] [Google Scholar]
- 8.Majeed H.A., Mohammed K.A., Salman H.A. Renocolic fistula as a complication to xanthogranulomatous pyelonephritis. Singapore Medical Journal. 1997;38(March (3)):116–119. [PubMed] [Google Scholar]
- 9.Flood H.D., Jones B., Grainger R. Ureterocolic fistula: a unique complication of extracorporeal shock wave lithotripsy. Journal of Urology. 1992;147:122–124. doi: 10.1016/s0022-5347(17)37154-9. [DOI] [PubMed] [Google Scholar]
- 10.Tundidor Bermudez A.M. A renocolic fistula diagnosed by retrograde pyelography. Archivos Espanoles de Urologia. 1999;52(September 7):788–790. [PubMed] [Google Scholar]


