Abstract
INTRODUCTION
We present a rare case of mesenteric lymphangioma in a middle-aged female.
PRESENTATION OF CASE
A 56-year-old female was admitted to the hospital with upper abdominal pain. Abdominal computed tomography revealed a multicystic mass surrounding the mesentery. We made the decision to resect the mass, suspecting that was a mesenteric lymphangioma based on additional imaging studies. The tumor adhered strongly to parts of the duodenum and the upper jejunum. In order to preserve the jejunum, we dissected its serosa away from the tumor. Approximately 1 week after surgery the patient experienced a constriction of the third portion of the duodenum. Her symptoms were improved with conservative therapy, and she was discharged from the hospital 62 days after surgery.
DISCUSSION
Lymphangioma originating from the mesentery may have cause adhesions due to exfoliated tumor cells; it is necessary to be concerned about postoperative obstruction.
CONCLUSION
The preoperative diagnosis of lymphangioma is based on various imaging modalities.
Keywords: Mesenteric cystic lymphangioma, Adult female, Duodenal stricture, SMA syndrome
1. Introduction
Lymphangioma is a rare, benign tumor that typically develops during childhood. The tumor usually develops in the neck, with the axillary tumors the second most common site. It is rarely seen in the mediastinum and, less than 1% of cases occur in the mesentery and retroperitoneum. Lymphangiomas themselves are asymptomatic for the most part, but often results in complications such as secondary infection, rupture with hemorrhage, and volvulus or intestinal obstruction as the tumor increases in size. Lymphangioma is frequently difficult to diagnose, surgical resection is selected in many cases for the purpose of both diagnosis and treatment. We report our experience with a rare case of mesenteric lymphangioma in a middle-aged female.
2. Presentation of case
A 56-year-old female was admitted to geriatric research institute of an outside hospital with upper abdominal pain. Abdominal computed tomography (CT) revealed a multicystic mass, (about 10 cm in diameter) surrounding the mesentery. She was transferred to our hospital for close examination and treatment.
At the time of admission; she had no symptoms except for abdominal pain. Her past medical history was significant for hepatitis C infection and fracture of the right patella as the result of a traffic accident. Blood analyses were unremarkable, except for a slight elevation of aspartate aminotransferase 52 IU/L and alanine aminotransferase 57 IU/L respectively.
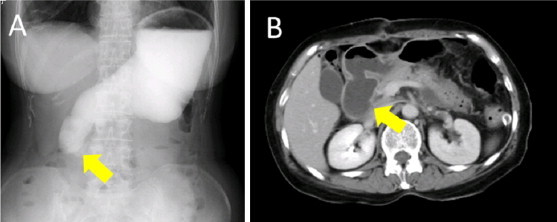
CT revealed that the mass was located in the intestinal mesentery behind the third portion of the duodenum (Fig. 1A and B). It appeared as an irregularly shaped, multilocular cyst with no contrast effect. Abdominal magnetic resonance imaging (MRI) showed low mass intensity on T1-weighted images and high intensity on T2-weighted images (Fig. 2A and B). Neither abdominal angiography nor endoscopic retrograde pancreatography (ERP) showed any abnormal findings. There was no accumulation of fluorodeoxyglucose positron emission transfer (PET). We therefore suspected that the mass was a mesenteric lymphangioma and performed resection for definitive diagnosis and treatment.
Fig. 1.
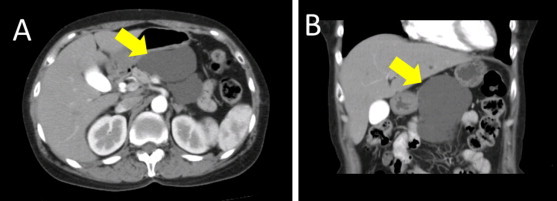
Abdominal computed tomography (CT) showing a mass involving the intestinal mesentery behind the third portion of the duodenum. Transverse section (A) and the axial section (B).
Fig. 2.
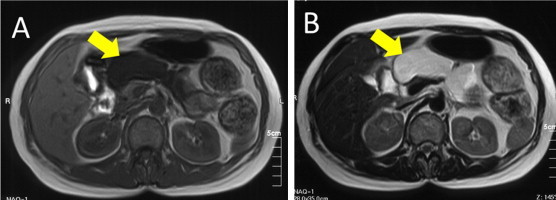
Abdominal magnetic resonance imaging: the mass has low intensity on T1-weighted images (A) and high intensity on T2-weighted images (B).
The cystic tumor surrounded the superior mesenteric artery (SMA) and the superior mesenteric vein (Fig. 3A and B). The growth seemed to arise from the cisterna chyli, located behind the SMA. The tumor was soft, had a thin wall, and was filled with easily aspirated lacteous fluid. Although it was adhered strongly to a part of both the duodenum and the upper jejunum, we were able to dissect the tumor away from these structures. In order to preserve the jejunum, it was necessary to perform extensive dissection to remove the tumor from the jejunal serosa.
Fig. 3.
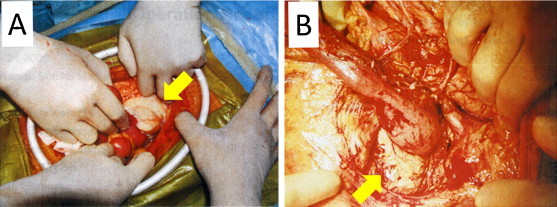
Intraoperative findings at the time of laparotomy (A). The tumor surrounds the superior mesenteric artery (B).
The cyst wall consisted of a monolayer of endothelial cells, small lymphatic spaces, abundant lymphoid tissue, and smooth muscle (Fig. 4A and B). The pathological diagnosis was mesenteric lymphangioma.
Fig. 4.
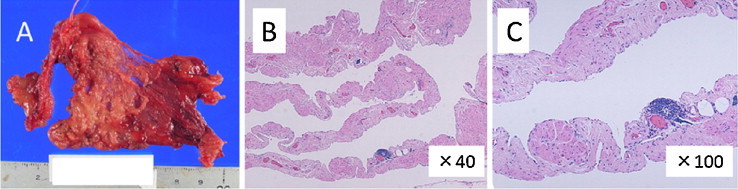
Histopathology: macroscopic (A) and microscopic (B and C) findings are shown. The cyst wall consists of a monolayer of endothelial cells, small lymphatic spaces, and abundant lymphoid tissue.
About 1 week after surgery, the patient began to experience abdominal pain and vomiting, making it impossible for her to swallow. Abdominal CT suggested edema and constriction of the intestine at the third portion of the duodenum. A contrast study of the upper digestive tract also suggested constriction in the same region (Fig. 5A and B). Upper gastrointestinal endoscopy, however, displayed no abnormal findings at the third portion of the duodenum. Based on these examinations, the constriction was thought to be due to SMA syndrome, although the wide resection of the jejunal serosa may also have contributed.
Fig. 5.
Upper digestive tract contrast study (A) and CT (B) revealing the intestinal constriction at the third portion of the duodenum.
Her symptoms improved with conservative therapy using total parenteral nutrition. The patient was able to tolerate oral intake after about 1 month, and was discharged from the hospital 62 days after the surgery. Over a long follow-up period, she has experienced no difficulties with eating and her nutritional state has remained stable. She has had no evidence of recurrence or duodenal stenosis for 5 years.
3. Discussion
Lymphangioma is a benign tumor that is rarely seen; it is present in fewer than 1 in 20,000 to 1 in 250,000 hospital admissions.1,2 Lymphangioma may occur at any age,3 although it typically develops during childhood. Although the origin of this tumor remains unclear, the cause is thought to be either trauma or an anomaly of the lymphatic system.1–7 Lymphangioma usually develops in the neck (75% of cases), but it can be seen in the axilla (25%), or rarely in the mediastinum (4–5%). It is very rarely seen in the mesentery and retroperitoneum (<1%).1,2,8,9 Thus, the present case of a mesenteric lymphangioma in an adult female is quite rare.
The tumor is classified into the 3 pathologic types of capillary, cavernous, and cystic.1,2,7 A cystic lymphangioma occurs in the abdominal cavity or retroperitoneum and has the following characteristics: the cyst wall consists of a monolayer of endothelial cells, small lymphatic spaces, abundant lymphoid tissue, and smooth muscle, and foam cells are present containing lipoid material in varying amounts.5 Such masses are also called hamartomas.1,7 Our patient's tumor was classified as a cystic lymphangioma.
The clinical symptoms of a mesenteric lymphangioma are abdominal pain, vomiting, and constipation. As these symptoms are common to many diseases, creating a wide differential diagnosis, the specific diagnosis of mesenteric lymphangioma is challenging. Assessment by diagnostic imaging, including ultrasonography, CT, and MRI, is very important for the diagnosis of a mesenteric lymphangioma; in our patient, CT and MRI led to her diagnosis.5–7,10,11 These tests are also used to estimate the size of the tumor and its infiltration into the surrounding tissues. Some diseases can be confused on imaging with mesenteric lymphangioma; these include a pancreatic tumor, gastrointestinal stromal tumor (GIST), hemangioma and lymphangiosarcoma. In order to narrow the differential, FDG-PET is useful in the assessment of malignancy, ERP in the differentiation of pancreatic tumors, and angiography in the differentiation of hemangioma. Hwang et al. reported that FDG-PET is useful in differentiating mesenteric lymphangioma from metastatic colon cancer.12
Although mesenteric cystic lymphangioma is a benign tumor, it often has life-threatening complications such as secondary infection, rupture with hemorrhage, and volvulus or intestinal obstruction.8,13,14 Few methods are available for the treatment of mesenteric lymphangioma, surgical management being the most effective to prevent recurrence.1,5,8,9 OK432, a sclerotherapeutic agent consisting of an injectable, lyophilized incubation mixture of group A Streptococcus pyogenes, is the only medication known to be effective against lymphangioma. The tumor can be reduced in size by injecting OK432 into the cysts, and the agent is often used on the surface of a lymphangioma. There are very few available reports on the use of OK432 in treatment of mesenteric lymphangioma, although Tokuhara et al. did report on the use of OK432 sclerotherapy after subtotal resection of a mesenteric lymphangioma.15 OK432 may also be useful in cases with difficult complete resections, as in the present case.
Our patient experienced a duodenal stricture after surgical resection of a mesenteric lymphangioma. This stricture was attributed to intestinal edema and SMA syndrome; it is possible that there was a contribution from edema induced by her extensive jejunal and duodenal serosal dissection. SMA syndrome is a rare condition, resulting from vascular compression third part of the duodenum. SMA syndrome occurs in patients with decreased body mass, prolonged immobility, and scoliosis, and it may also be of congenital origin. Ultimately, it occurs from a narrowing of the angle between the SMA and the aorta.16,17 In our patient's, as the lymphangioma surrounded the superior mesenteric artery, we had to perform extensive dissection, including of the adipose tissue between the SMA and the aorta. This could certainly have caused SMA syndrome and the resulting duodenal stricture. Further surgery would have been very difficult given the extent of adhesions present; we therefore treated her SMA syndrome with conservative methods.16,17 As lymphangioma originating from the mesentery may cause adhesions from exfoliatiated cells, concern for postoperative obstruction was warranted. After 1 month of total parenteral nutrition, on total parenteral nutrition, she was able to tolerate oral intake.
4. Conclusion
We report a rare case of mesenteric lymphangioma in an adult. The preoperative diagnosis of lymphangioma was based on CT, MRI, and FDG-PET. We feel that it is important to involve various imaging modalities before making this diagnosis. It is also necessary to be vigilant for possible postoperative intestinal obstruction in patients in whom tumor resection from the serosa or mesentery of the intestine is difficult.
Conflict of interest statement
None.
Funding
None.
Ethical approval
The patient has provided permission to publish these features of this case and the identity of the patient has been protected.
Author contributions
Akira watanabe contributed the manuscript preparation. Hideki Suzuki, Tsutomu Kobayashi, Kenichiro Araki and Tatsuo Shimura performed the operation.
References
- 1.Losanoff J.E., Richman B.W., El-Sherif A., Rider K.D., Jones J.W. Mesenteric cystic lymphangioma. Journal of the American College of Surgeons. 2003;196:598–603. doi: 10.1016/S1072-7515(02)01755-6. [DOI] [PubMed] [Google Scholar]
- 2.Wani I. Mesenteric lymphangioma in adult: a case series with a review of the literature. Digestive Diseases and Sciences. 2009;54:2758–2762. doi: 10.1007/s10620-008-0674-3. [DOI] [PubMed] [Google Scholar]
- 3.Vanek V.W., Phillips A.K. Retroperitoneal, mesenteric, and omental cysts. Archives of Surgery. 1984;119:838–842. doi: 10.1001/archsurg.1984.01390190076018. [DOI] [PubMed] [Google Scholar]
- 4.Allen J.G., Riall T.S., Cameron J.L., Askin F.B., Hruban R.H., Campbell K.A. Abdominal lymphangioma in adults. Journal of Gastrointestinal Surgery. 2006;10:746–751. doi: 10.1016/j.gassur.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 5.de Perrot M., Rostan O., Morel P., Le Coultre C. Abdominal lymphangioma in adults and children. British Journal of Surgery. 1998;85:395–397. doi: 10.1046/j.1365-2168.1998.00628.x. [DOI] [PubMed] [Google Scholar]
- 6.Alqahtani A., Nguyen L.T., Flageole H., Shaw H., Laberge K.J.M. 25 years’ experience with lymphangiomas in children. Journal of Pediatric Surgery. 1999;34:1164–1168. doi: 10.1016/s0022-3468(99)90590-0. [DOI] [PubMed] [Google Scholar]
- 7.Losanoff J.E., Kjossev K.T. Mesenteric cystic lymphangioma: unusual cause of intra-abdominal catastrophe in an adult. International Journal of Clinical Practice. 2005;59:986–987. doi: 10.1111/j.1368-5031.2005.00554.x. [DOI] [PubMed] [Google Scholar]
- 8.Chen C.W., Hsu S.D., Lin C.H., Cheng M.F., Yu J.C. Cystic lymphangioma of the jejunal mesentery in an adult: a case report. World Journal of Gastroenterology. 2005;11:5084–5086. doi: 10.3748/wjg.v11.i32.5084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsukada H., Takaori K., Ishigro S., Tsuda T., Ota S., Yamamoto T. Giant cystic lymphangioma of the small bowel mesentery: report of a case. Surgery Today. 2002;32:734–737. doi: 10.1007/s005950200138. [DOI] [PubMed] [Google Scholar]
- 10.Yoo E., Kim M.J., Kim K.W., Chung J.J., Kim S.H., Choi J.Y. A case of mesenteric cystic lymphangioma: fat saturation and chemical shift MR imaging. Journal of Magnetic Resonance Imaging. 2006;23:77–80. doi: 10.1002/jmri.20474. [DOI] [PubMed] [Google Scholar]
- 11.Pui M.H., Li Z.P., Chen W., Chen J.H. Lymphangioma imaging diagnosis. Australasian Radiology. 1997;41:324–328. [PubMed] [Google Scholar]
- 12.Hwang S.S., Choi H.J., Park S.Y. Cavernous mesenteric lymphangiomatosis mimicking metastasis in a patient with rectal cancer: a case report. World Journal of Gastroenterology. 2009;15:3947–3949. doi: 10.3748/wjg.15.3947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jang J.H., Lee S.L., Ku Y.M., An C.H., Chang E.D. Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean Journal of Radiology. 2009;10:319–322. doi: 10.3348/kjr.2009.10.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chung J.C., Song O.P. Cystic lymphangioma of the jejunal mesentery presenting with acute abdomen in an adult. Canadian Journal of Surgery. 2009;52:E286–E288. [PMC free article] [PubMed] [Google Scholar]
- 15.Tokuhara K., Hamada Y., Watanabe K., Tanano A., Takada K., Sato M. A case of huge mesenteric lymphangioma managed by laparoscopy-assisted subtotal resection with sclerosing therapy. Japanese Society of Pediatric Surgeons. 2003;39:90–95. [Google Scholar]
- 16.Matheos E., Vasileios K., Ioannis B., Dimitrios Z., Kostas H. Superior mesenteric artery syndrome. Case Reports in Gastroenterology. 2009;3:156–161. doi: 10.1159/000209866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boldery J., Gleeson J., Jordaan J. Superior mesenteric artery syndrome following small bowel resection. ANZ Journal of Surgery. 2006;76:861–862. doi: 10.1111/j.1445-2197.2006.03887.x. [DOI] [PubMed] [Google Scholar]


