Abstract
INTRODUCTION
Tracheocutaneous fistula is a complication of tracheostomy. Tracheocutaneous fistulectomy followed by primary closure carries a high possibility of complications.
PRESENTATION OF CASE
An 11-year-old boy underwent surgery to repair a tracheocutaneous fistula, using skin and muscle flaps. A vertical incision was made around the fistula and 3 skin flaps were prepared: 2 hinge flaps, and 1 to cover the skin defect (advanced flap). The 2 hinged turnover flaps were invaginated by multiple layered sutures, and a strap muscle flap was placed over the resulting tracheal closure. An advanced skin flap was used to cover the area of the previous defect. The patient was extubated immediately after surgery. He was discharged on the sixth postoperative day without tracheal leakage or subcutaneous emphysema. The patient is currently doing well, with no respiratory symptoms and no recurrence at the postoperative 5 months.
DISCUSSION
Our technique is minimally invasive and has a low risk of lumen stenosis, other complications, or recurrence.
CONCLUSION
This technique demonstrates the multiple-layered closure of a tracheocutaneous fistula, using skin flaps and a muscle flap.
Keywords: Hinge flap, Muscle flap, Tracheocutaneous fistula
1. Introduction
Tracheocutaneous fistula is a complication of tracheostomy, and can be cosmetically unappealing and socially problematic. Tracheocutaneous fistulectomy followed by primary closure carries a high possibility of pneumomediastinum, pneumothorax, and wound breakdown.1,2 We describe a surgical procedure for closing a tracheocutaneous fistula, using skin and muscle flaps, to prevent both complications and recurrence.
2. Presentation of case
A now 11-year-old boy was admitted to an outside hospital at the age of 2 months for respiratory distress, where he underwent intubation. Further examination revealed that he was suffering from tricuspid atresia, a ventral septal defect, and pulmonary stenosis; he underwent a bidirectional Glenn procedure and creation of an atrial septal defect. Following this operation, he was diagnosed with subglottic stenosis due to technical difficulties with extubation. He received a tracheostomy at the age of 6 months. When he was 4 years old, he underwent laryngotracheoplasty using costal cartilage, which led to successful extubation at the age of 5 years. He subsequently underwent a total cavopulmonary connection with Gore-Tex, but a tracheocutaneous fistula had developed and was persistent.
He was referred to our hospital for primary closure of the fistula. Physical examination revealed a tracheocutaneous fistula, measuring 10 mm × 2 mm (Fig. 1a). Preoperative computed tomography (CT) showed that the fistula ran obliquely and was 2 cm in length, 3 mm in width, and 5 mm in height (Fig. 1b). Preoperative flexible fiberoptic endoscopy showed that the tracheal lumen was not stenotic and the tracheal wall was not inverted. A 10 Fr Nelaton catheter was easily passed through the fistula into the tracheal lumen (Fig. 1c). After closure of the long tracheocutaneous fistula, intraoperative flexible fiberoptic endoscopy showed that the tracheal lumen remained non-stenotic and the tracheal wall had not become inverted during surgery (Fig. 1d).
Fig. 1.
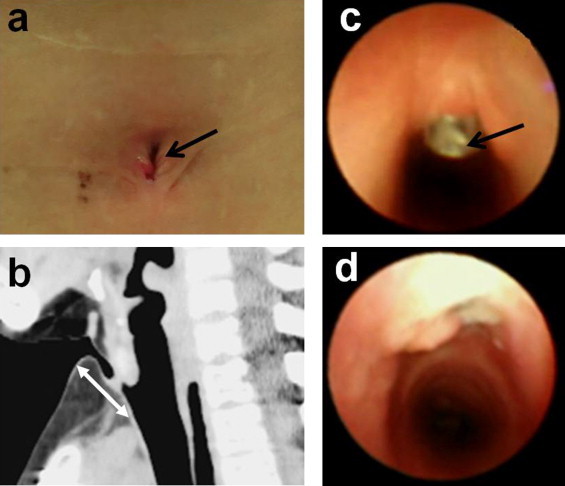
Physical examination, preoperative computed tomography (CT), and pre- and intraoperative bronchoscopy. (a) Physical examination showing a tracheocutaneous fistula of 10 mm × 2 mm (black arrow). (b) Preoperative CT showing an oblique tracheocutaneous fistula 2 cm in length (white arrow). (c) Preoperative flexible fiberoptic endoscopy showing a nonstenotic tracheal lumen and a non-inverted tracheal wall. A 10 Fr Nelaton catheter is visible passing into the tracheal lumen through the fistula (black arrow). (d) Intraoperative flexible fiberoptic endoscopy showing the tracheal lumen is not stenotic and the tracheal wall is not inverted after repair.
The patient was extubated immediately after surgery. He was discharged on the sixth postoperative day without tracheal leakage or subcutaneous emphysema. One month after surgery, examination showed a well-healed repair and CT revealed that the tracheocutaneous fistula was completely closed, without any evidence of tracheal stenosis (Fig. 2a and b). The patient is currently doing well, with no respiratory symptoms and no recurrence at the postoperative 5 months.
Fig. 2.
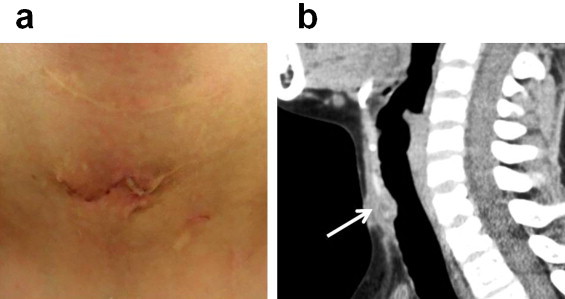
Postoperative findings. (a) One month after repair, the wound was well-healed. (b) CT showing the completely closed tracheocutaneous fistula without tracheal stenosis (white arrow: closure of a tracheocutaneous fistula).
3. Operative procedures
A vertical, longitudinal, spindle-shaped incision was made in the skin around the tracheocutaneous fistula. Three skin flaps were prepared, including hinge flaps on the right and left sides of the fistula, with the third flap (advanced flap) to the right of the hinge flaps to eventually cover the skin defect (Figs. 3a and 4a). Dissection was carried down to the peritracheal area, preserving an area of fibrotic subcutaneous tissue around the fistula (Fig. 4b). The hinged turnover flaps were sutured with 5-0 polydioxanone to make an inner lining for the trachea (Figs. 3b and 4c). The subcutaneous tissues around the fistula were then sutured with 4-0 nylon, using 4 layered sutures to invaginate the hinged flaps into the fistula (Figs. 3c–e and 4d). A right-sided sternohyoid muscle flap was then rotated into the closed fistula and fixed in place (Fig. 4e). A 6 mm Penrose drain was inserted to prevent subcutaneous emphysema or hematoma formation. Finally, the platysma was closed and the advanced skin flap was rotated to cover the surgical area (Figs. 3f and 4f). The Penrose drain was removed after 24 h.
Fig. 3.
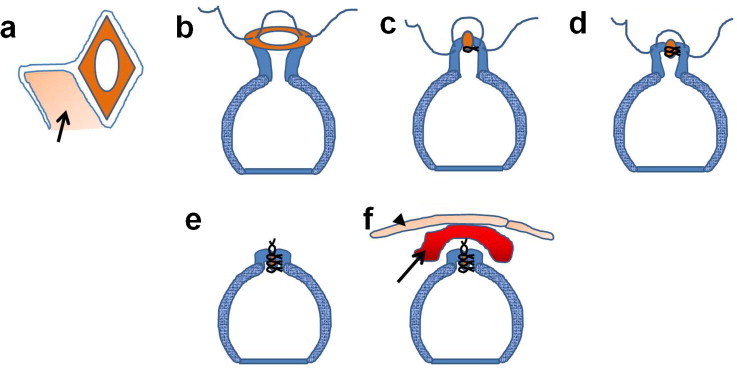
Schematic of operative procedures. (a) A vertical, longitudinal, spindle-shaped skin incision is created around the tracheocutaneous fistula. Hinge flaps are created to the right and left of the fistula, and an advanced skin flap (black arrow) is prepared to cover the skin defect. (b) The hinged turnover flaps are sutured with 5-0 polydioxanone to make an inner lining for the trachea. (c–e) The subcutaneous tissues around the fistula are sutured with 4-0 nylon in 4 layers; the multiple layered hinge flaps are invaginated into the fistula. (f) A right-sided sternohyoid muscle flap (black arrow) is rotated over the closed fistula and fixed in place. The platysma is closed and the rotated skin flap (advanced flap) sutured (black arrowhead).
Fig. 4.
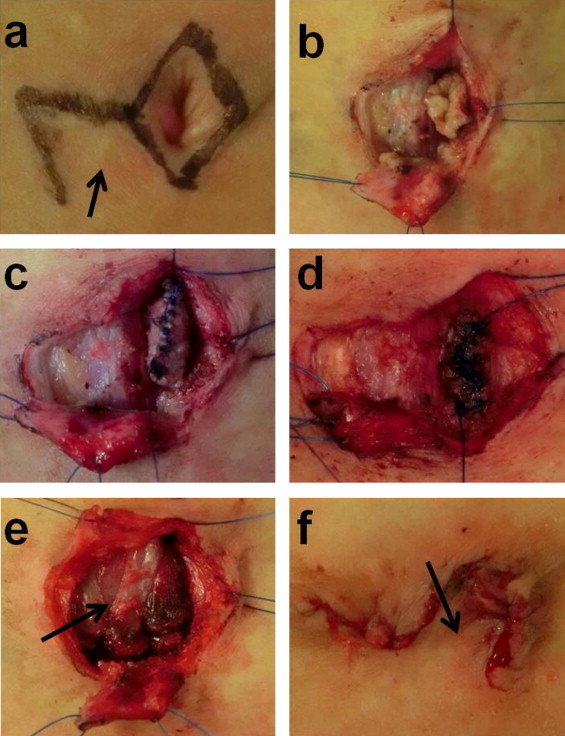
Intraoperative findings. (a) The longitudinal spindle-shaped skin incision is created vertically around the tracheocutaneous fistula. Two hinge flaps are created: 1 on the right side of the fistula and 1 on the left side of the fistula. An advanced skin flap is prepared to cover the skin defect (black arrow). (b) Dissection is carried down to the peritracheal area, preserving an area of fibrotic subcutaneous tissue around the fistula. (c) The hinged turnover flaps are sutured with 5-0 PDS to make an inner lining for the trachea. (d) The subcutaneous tissues around the fistula are sutured with 4-0 nylon in multiple layers (4 times). (e) A right-sided sternohyoid muscle flap (black arrow) is then rotated to cover the area of the closed fistula. (f) The platysma is closed and the rotated skin flap (advanced flap) covers the surgical site (black arrow).
4. Discussion
Several techniques are used to close tracheocutaneous fistulae.1–9 These include multiple layered primary closure with partial fistulectomy,3 bipedicle delayed flap closure with primary inversion of the edges of the fistula (fistulectomy with healing by secondary intention),1 closure by transplantation of an ear cartilage graft with muscle and fasciocutaneous flaps,4 and elevation and inward rotation of the epithelial lining of the tracheocutaneous fistula as a marginal flap, using a hinged turnover flap, with an additional V-Y advancement flap.2,5–9 It has been reported that primary closure with excision of the fistula tract down to the level of the trachea may result in tracheocele, pneumopericardium, pneumothorax, and pneumomediastinum.1,2,10–12
Closure with a turnover flap of skin and fibroadipose tissue means that the defect in the tracheal lumen is covered by the outer surface of the cutaneous flap. This minimizes the suturing required, and results in fewer problems with insufficiency of the repair.5–9 The epithelial layer of the hinged flap will eventually be replaced with a mucosal layer.6
Even though with invagination of two hinged turnover flaps into the fistula, using multiple layered sutures, it is possible to avoid narrowing the tracheal lumen. In addition, the strength of this closure could be disrupted by a sudden elevation of airway pressure such as that which accompanies paroxysmal coughing.9 Furthermore, a strap muscle flap was utilized to reinforce the fistula closure.3,5
By using an advanced skin flap or a skin flap by subcutaneous Z-plasty with which to cover the repair site, the suturing lines of the tracheal defect and the suturing lines of the skin defect are not in parallel, helping to prevent recurrence of the fistula. When the orfice of the tracheocutaneous fistula is large or the sacrring around the tracheocutaneous fistula is strong, Z-plasty may be more advantage. However, our technique is better and minimally invasive when the orfice of the tracheocutaneous fistula is small or the elasticity around the tracheocutaneous fistula is good. In our technique, it is important to make the repair flap thick, using multiple layers of suturing, to prevent leakage and to get successful results using this technique.9 But our technique will carry the possible difficulties of making skin flaps by the direction of the previous incisional scars.
5. Conclusion
We present a case demonstrating the technique of multiple-layered closure of a tracheocutaneous fistula, using skin flaps and a muscle flap. This technique avoids the complications generally associated with the closure of such defects.
Conflict of interest
The authors have no conflicts of interest to declare.
Funding
The authors have no sources of funding.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
YT wrote the paper; HY and TH interpreted the study design. All authors read and approved the final manuscript.
References
- 1.Jacobs J.R. Bipedicle delayed flap closure of persistent radiated tracheocutaneous fistulas. Journal of Surgical Oncology. 1995;59:196–198. doi: 10.1002/jso.2930590312. [DOI] [PubMed] [Google Scholar]
- 2.Lee B.J., Goh E.K., Wang S.G., Hwang S.M. Closure of large tracheocutaneous fistula using turn-over hinge flap and V-Y advancement flap. Journal of Laryngology and Otology. 2002;116:627–629. doi: 10.1258/00222150260171632. [DOI] [PubMed] [Google Scholar]
- 3.Schroeder J.W., Jr., Greene R.M., Holinger L.D. Primary closure of persistent tracheocutaneous fistula in pediatric patients. Journal of Pediatric Surgery. 2008;43:1786–1790. doi: 10.1016/j.jpedsurg.2008.01.010. [DOI] [PubMed] [Google Scholar]
- 4.Riedel F., Reinhart Goessler U., Grupp S., Bran G., Hörmann K., Verse T. Management of radiation-induced tracheocutaneous tissue defects by transplantation of an ear cartilage graft and deltopectoral flap. Auris, Nasus, Larynx. 2006;33:79–84. doi: 10.1016/j.anl.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Berenholz L.P., Vail S., Berlet A. Management of tracheocutaneous fistula. Archives of Otolaryngology – Head and Neck Surgery. 1992;118:869–871. doi: 10.1001/archotol.1992.01880080091020. [DOI] [PubMed] [Google Scholar]
- 6.Kamiyoshihara M., Nagashima T., Takeyoshi I. A novel technique for closing a tracheocutaneous fistula using a hinged skin flap. Surgery Today. 2011;41:1166–1168. doi: 10.1007/s00595-010-4393-y. [DOI] [PubMed] [Google Scholar]
- 7.Eliashar R., Sichel J.Y., Eliachar I. A new surgical technique for primary closure of long-term tracheostomy. Otolaryngology – Head and Neck Surgery. 2005;132:115–118. doi: 10.1016/j.otohns.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Rennekampff H.O., Tenenhaus M. Turnover flap closure of recalcitrant tracheostomy fistula: a simplified approach. Plastic and Reconstructive Surgery. 2007;119:551–555. doi: 10.1097/01.prs.0000246378.43769.6d. [DOI] [PubMed] [Google Scholar]
- 9.Nakamura K., Yamaguchi H., Horiguchi S., Hiramatsu H., Tsukahara K., Hirose H. Surgical techniques for closure of tracheostoma (Abstract in English) Journal of Japan Bronchoesophagology Society. 2001;52:331–335. [Google Scholar]
- 10.Briganti V., Tavormina P., Testa A., Oriolo L. Giant tracheocele following primary tracheostomy closure in a 3 year old child. Interactive Cardiovascular and Thoracic Surgery. 2004;3:411–412. doi: 10.1016/j.icvts.2004.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Koloutsos G., Barbetakis N., Kirodimos E., Samanidis G., Paliouras D., Vahtsevanos K. Pneumopericardium following tracheostomy closure. Tuberkuloz ve Toraks. 2009;57:205–207. [PubMed] [Google Scholar]
- 12.Wiel E., Fayoux P., Vilette B. Complications of surgical closure of tracheo-cutaneous fistula in pediatric patients – two case reports. International Journal of Pediatric Otorhinolaryngology. 2000;52:97–99. doi: 10.1016/s0165-5876(99)00289-x. [DOI] [PubMed] [Google Scholar]


