Abstract
INTRODUCTION
Tubercular infection of prosthetic joint arthroplasty is sporadically described, but its incidence is rising. Misdiagnosis is common because of disparate clinical presentation.
PRESENTATION OF CASE
We describe 1 hand, 2 hip and 2 knee prosthetic-joint infections due to Mycobacterium tuberculosis in patients without a previous history of tuberculosis. All of them were initially misdiagnosed as bacterial infections and unsuccessfully treated with antibiotic for a long period of time. Diagnosis was made by means of culture of periprosthetic tissues and histolopathological examination. Tuberculosis was cured in all patients, but two of them have had a permanent functional damage (one arthrodesis of the knee and one loss of hand function).
DISCUSSION
An aggressive diagnostic approach is required to make diagnosis of periprosthetic tubercular infection. The identification of the pathogen is advisable to test drug susceptibility.
CONCLUSION
The low index of suspicion of periprosthetic tubercular infection could delay a correct diagnosis with risk of permanent damage due to a late treatment. During any surgical revision of prosthetic joints with suspect infection culture for tuberculosis should be taken into consideration.
Keywords: Mycobacterium tuberculosis, Arthroplasty, Infection, Drug resistance
1. Introduction
Primary tubercular osteo-arthritis is well known, while periprosthetic tubercular infections are uncommon.1 In some cases, tissues trauma related with arthroplastic surgery could cause local reactivation of previous unrecognized tuberculosis, mimicking an early periprosthetic infection.2 In other patients, a haematogenous spread from a distant tubercular focus could be presumed.3
Aim of the present report is to describe 5 cases of periprosthetic infection due to Mycobacterium tuberculosis, initially misdiagnosed as bacterial infections, observed in the period 2005–2009 in an Italian tertiary care centre for bone infections.
2. Presentation of cases
2.1. Case 1
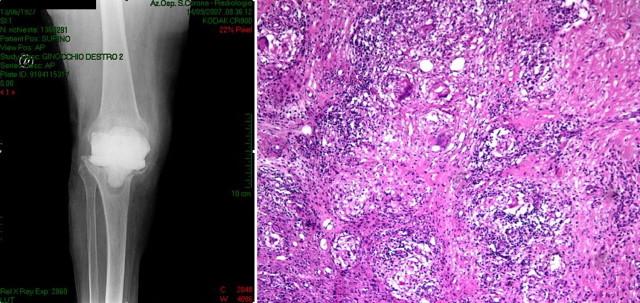
A 72-year-old diabetic immunocompetent woman was evaluated for a periprosthetic infection occurring 7 years after a total knee arthroprosthesis. She complained worsening local discomfort and aseptic loosing was initially diagnosed and treated with one stage replacement in another centre. The patient developed an early surgical site infection treated empirically with teicoplanin and ciprofloxacin. Debridement was also performed, but infection was not cured and the patients developed severe skin lesions and bone exposition, with radiological signs of osteomyelitis (Fig. 1). At time of our first assessment antibacterial treatment was withdrawn and 3 swabs of the skin lesion were performed without identification of bacteria. Two-stage exchange was performed. Because of major bone gap, an external fixation apparatus was also implanted. Six intraoperative cultures resulted negative for bacteria or fungi. Histological examination revealed granuloma with Langhans cells but negative Ziehl–Neelsen stain. One month later, cultures revealed M. tuberculosis with no antibiotic resistance. The chest X-ray was normal. Combination chemotherapy with isoniazid, rifampin and ethambutol was prescribed for 2 months. Isoniazid and rifampin were extended for other 10 months. At the end of treatment, infection was clinically resolved. Arthrodesis was performed with resolution of pain but poor functional result because of asymmetrical gait (Oxfort Knee Score: 24).4 One year later, the patient had no clinical signs of infection but she was able to walk only on crutches.
Fig. 1.

2.2. Case 2
A 79-year-old immunocompetent woman was evaluated for infection of a hip prosthesis implanted after traumatic fracture in another centre. She developed an early infection, empirically treated with broad-spectrum antibiotics. A fistula developed one year later, with isolation of Enterococcus faecalis. Antibiotic treatment with linezolid for 4 weeks was prescribed in the other centre with clinical improvement and resolution of the fistula. In spite of clinical improvement, the patient still had pain (Oxfort hip Score: 28). At the time of our first observation a labelled-leucocyte scintigraphy suggested the persistence of infection and ultrasound scan showed the presence of an abscess, subsequently drained (Fig. 2). A two-stage exchange was performed. Empirical treatment with teicoplanin and ciprofloxacin was prescribed. Cultures of surgical periprosthetic tissue specimens were negative. After 3 months, the spacer was removed and arthroprosthesis was reimplanted. Intra-operative cultures were repeated. Bacterial cultures were still negative, but one month later M. tuberculosis grew, and combination chemotherapy with isoniazid, rifampin and ethambutol was prescribed. No resistance to antitubercular drugs was documented. The chest X-ray was normal. Treatment was complicated by gastrointestinal discomfort and the patient, in spite of medical prescription of antimycobacterial drugs for at least 9 months, stopped the therapy after 5 months. In spite of this short course of treatment, the functional result was good (Oxfort hip Score: 40) after one year of follow up.
Fig. 2.

2.3. Case 3
A 92-year-old immunocompetent female was admitted at our hospital because of periprosthetic infection with a fistula. A total hip replacement was inserted 3 years before in another centre because of traumatic fracture treated in a first step with intramedullary nail (Fig. 3). The patient had good functional results for 2 years but then she was bedridden because of extreme pain. Taking into consideration the old age and the high anaesthesiology risk (ASA 4), one-stage replacement was performed. The intra-operative culture yielded oxacillin-resistant Staphylococcus epidermidis, and antibacterial treatment with vancomycin followed by linezolid was initially administered. However, histology revealed granuloma with Langhans cells and, after 40 days, M. tuberculosis was identified. The chest X-ray was normal. Combination chemotherapy with isoniazid, rifampin and ethambutol was prescribed. There were several interruptions in antimycobacterial treatment for nausea (rifampin was changed with levofloxacin after one month, but also this drug was discontinued). Treatment was completely stopped after 9 months. Follow up at 6 months after the end of treatment was negative for reactivation of infection. The patient was able to ambulate with a walking frame with no pain.
Fig. 3.

2.4. Case 4
An 80-year-old immunocompetent woman underwent a total knee arthroprosthesis in another centre for arthritic pain worsened after fall to the ground. In spite of the surgery, she still complained pain, particularly during walking. At time of our first observation a labelled-leucocyte scintigraphy was positive for prosthesis infection. The device was removed with a two-stage exchange. Broad-spectrum antibiotic treatment with vancomycin plus ciprofloxacin was also administered but the patient developed acute renal failure. Cultures of periprosthetic tissue specimens were negative, but histological examination showed granuloma with positive Ziehl–Neelsen stain (Fig. 4). M. tuberculosis grew from the culture and, therefore, the anti infective treatment was modified. Rifampin, isoniazid, and ethambutol were prescribed for 2 months, followed by rifampin and isoniazid for one year. Two months later there was a dehiscence of the surgical wound with discharge from sinus tract. Debridement with retention of spacer was performed with success. The patient was lost to follow up 6 months later because of an ischaemic heart attack that requires admission to cardiology. Few months later she died, but until then, no clinical signs of tuberculosis reactivation were evident.
Fig. 4.
2.5. Case 5
A 68-year-old immunocompetent man underwent a radio-carpic arthroprosthesis on the left hand in another centre (Fig. 5). Two years later he developed an abscess with a deep fistula unsuccessfully treated with ciprofloxacin in the absence of isolated pathogens. He had aortic valve stenosis that needed surgical repair, but the absence of infection was required before cardiac surgery. Debridement and removal of arthroprosthesis was performed in our hospital and antibiotic treatment with vancomycin and cefepime was started. Intraoperative cultures were negative for bacteria but histology showed granuloma with negative Ziehl–Neelsen stain. After 40 days M. tuberculosis was isolated. Antimycobacterial treatment with rifampin, isoniazid, pyrazinamide and ethambutol was prescribed for 2 months, followed by rifampin and isoniazid for one year. Infection was resolved but patient lost hand function.
Fig. 5.

3. Discussion
We describe 5 cases of periprosthetic joint infections due to M. tuberculosis in Caucasian, elderly patients without other risk factors for tuberculosis and without a previous clinical history of tubercular disease. Bone infection is described in 1–5% of patients with tuberculosis. Old age, steroid administration and immunosuppression (e.g. HIV infection) represent the most important risk factors, but tubercular bone infection should not be excluded in their absence.5–7 Before diagnosis of tubercular periprosthetic joint infection our patients were treated empirically with antibiotics, and tuberculosis was not suspected at time of surgery. In our centre the diagnostic work-up for severe persistent prosthetic joint infection includes histology and culture for bacteria, fungi and mycobacteria. Culture for M. tuberculosis requires long times (one month or longer), with possible delay of treatment when tuberculosis is not suspected. A rapid diagnosis performed with histological examination and molecular biology techniques8 could be helpful for the treatment of prosthetic joint infections due to M. tuberculosis since tuberculosis often does not cause early component loosening and patients could be treated successfully with prosthesis conservation. On the contrary, when diagnosis is late, tubercular osteomyelitis can induce severe bone damage with poor functional results.9 We did not employ molecular biology techniques and it is possible that the delayed diagnosis performed with “classical” culture played some role in the suboptimal functional results observed in some patients. Even if molecular techniques are employed, cultures must always be performed to obtain an antibiotic susceptibility test that is now highly recommended for the increasing number of drug-resistant tuberculosis. Probably we describe reactivations of old tuberculosis contracted in Italy when resistances were not widespread since all the Mycobacteria isolated in our patients were susceptible to first-line antitubercular drugs (rifampin isoniazid, ethambutol, pyrazinamide). At least 6–9 months of antitubercular treatment are generally recommended for patients with tubercular osteoarthritis, but longer therapies are described.10 Nonetheless, it can be difficult to complete the treatment in elderly people because of drug-related adverse events, like observed in our patients. Many report indicate the effectiveness of anti mycobacterial treatment associated with total arthroplasty,11 but diagnosis must be undisputed and invasive investigations are required in doubtful cases12 because of the long duration of antibacterial therapy.
In two patients Enterococcus and Staphylococcus were isolated together with M. tuberculosis. We think that these pathogens could be contaminant or co-pathogens, since infection has been completely resolved only when antitubercular treatment was started.
4. Conclusion
Our report clearly underlines that diagnostic work up for detection of M. tuberculosis (histology, culture, and possibly molecular biology techniques) must be performed in persistent prosthetic joint infections, also in the absence of previous clinical history of tuberculosis.
Conflict of interest statement
None.
Funding
None.
Ethical approval
We have obtained written consent from the patient to use clinical data for scientific purposes. Copy of the consent will be available on Editor's request.
Authors’ contributions
The study was designed by Giuliana Carrega and Giovanni Riccio. The manuscript was written by Giuliana Carrega. Data collection and analysis were done by Giuliana Carrega, Valentina Bartolacci, Giorgio Burastero, Giorgetta Casalino Finocchio, Agostina Ronca, and Giovanni Riccio.
References
- 1.Marmor M., Parnes N., Dekel S. Tuberculosis infection complicating total knee arthroplasty: report of 3 cases and review of the literature. Journal of Arthroplasty. 2004;19:397–400. doi: 10.1016/j.arth.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 2.Hugate R., Jr., Pellegrini V.D., Jr. Reactivation of ancient tuberculous arthritis of the hip following total hip arthroplasty: a case report. Journal of Bone and Joint Surgery. 2002;84-A:101–105. doi: 10.2106/00004623-200201000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Khater F.J., Samnani I.Q., Mehta J.B., Moorman J.P., Myers J.W. Prosthetic joint infection by Mycobacterium tuberculosis: an unusual case report with literature review. Southern Medical Journal. 2007;100:66–69. doi: 10.1097/01.smj.0000232972.50186.4c. [DOI] [PubMed] [Google Scholar]
- 4.Dawson J., Fitzpatrick R., Murray D., Carr A. Questionnaire on the perceptions of patients about total knee replacement surgery. Journal of Bone and Joint Surgery. 1998;80-B:63–69. doi: 10.1302/0301-620x.80b1.7859. [DOI] [PubMed] [Google Scholar]
- 5.Spinner R.J., Sexton D.J., Goldner R.D., Levin L.S. Periprosthetic infections due to Mycobacterium tuberculosis in patients with no prior history of tuberculosis. Journal of Arthroplasty. 1996;11:217–222. doi: 10.1016/s0883-5403(05)80023-3. [DOI] [PubMed] [Google Scholar]
- 6.Kaya M., Nagoya S., Yamashita T., Niiro N., Fujita M. Peri-prosthetic tuberculous infection of the hip in a patient with no previous history of tuberculosis. Journal of Bone and Joint Surgery – British Volume. 2006;88:394–395. doi: 10.1302/0301-620X.88B3.17006. [DOI] [PubMed] [Google Scholar]
- 7.Cansü E., Erdogan F., Ulusam A.O. Incision infection with Mycobacterium tuberculosis after total hip arthroplasty without any primary tuberculosis focus. Journal of Arthroplasty. 2011;26:505e1–505e3. doi: 10.1016/j.arth.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 8.De Nardo P., Corpolongo A., Conte A., Gentilotti E., Narciso P. Total hip replacement infected with Mycobacterium tuberculosis complicated by Addison disease and psoas muscle abscess: a case report. Journal of Medical Case Reports. 2012;6:3. doi: 10.1186/1752-1947-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee C.L., Wei Y.S., Ho Y.J., Lee C.H. Postoperative Mycobacterium tuberculosis infection after total knee arthroplasty. Knee. 2009;16:87–89. doi: 10.1016/j.knee.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 10.De Haan J., Vreeling A.W.J., Van Hellemondt G.G. Reactivation of ancient joint tuberculosis of knee following total knee arthroplasty after 61 years: a case report. Knee. 2008;15:336–338. doi: 10.1016/j.knee.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 11.Sidhu A.S., Singh A.P., Singh A.P. Total hip replacement in active advanced tuberculous arthritis. Journal of Bone and Joint Surgery – British Volume. 2009;91-B:1301–1304. doi: 10.1302/0301-620X.91B10.22541. [DOI] [PubMed] [Google Scholar]
- 12.Tuli S.M. General principles of osteoarticular tuberculosis. Clinical Orthopaedics and Related Research. 2002;398:11–19. doi: 10.1097/00003086-200205000-00003. [DOI] [PubMed] [Google Scholar]


