Abstract
INTRODUCTION
Adrenal incidentalomas have a prevalence of at least 5% in the general population. Among these adrenal myelolipoma are rare nonfunctioning tumors of adrenal with an incidence of 0.1–0.2% as documented in CT and autopsy series. We report such a rare case of adrenal myelolipoma incidentally detected while evaluating a case of chronic nonspecific flank pain.
PRESENTATION OF CASE
38-year-old obese female patient, known hypertensive on treatment presented with nonspecific right flank pain since 1 year. Ultrasonography and Computed tomography of the abdomen showed right adrenal gland mass with fat density measuring 6.3 cm × 6.2 cm × 5 cm. Patient underwent right side adrenalectomy, post operatively patient had an uneventful recovery. Histopathological examination of the specimen revealed features of adrenal myelolipoma.
DISCUSSION
Myelolipoma is an uncommon, benign; tumor like lesion composed of mature adipose tissue admixed with hematopoietic cells. Most myelolipomas appear as unilateral adrenal masses. Adrenal myelolipomas are usually small and asymptomatic. CT or MRI detects the areas of gross fat with in the lesion. These tumors can present as acute abdomen following tumor hemorrhage which is more likely in myelolipomas greater than 4 cm in size, hence warrants adrenalectomy.
CONCLUSION
adrenal myelolipoma are rare benign tumors, incidentally detected on CT. CT or MRI is diagnostic. Large myelolipoma warrants surgery due to the risk of hemorrhage.
Keywords: Adrenal myelolipoma, Adrenal benign tumor
1. Introduction
An adrenal lesion discovered during imaging performed for unrelated reasons is referred to as an incidentaloma. Adrenal incidentalomas have a prevalence of at least 5% in the general population.1 Among these adrenal myelolipoma are rare nonfunctioning benign tumors of adrenal with an incidence of 0.1–0.2% as documented in Computed tomography and autopsy series.2 With the increasing use of Computed tomography they are now being encountered as chance findings. We report such a rare case of adrenal myelolipoma incidentally detected while evaluating a case of chronic nonspecific flank pain. Purpose of this case report is to highlight the disease characteristic, therapeutic approach and reasoning of these rare diagnoses with review of literature.
2. Presentation of case
38-year-old obese female patient, known hypertensive on regular treatment presented with nonspecific right flank pain since 1 year. Clinical examination is nothing contributory except for obesity, hypertension and mild tenderness over right flank. Her Hemogram and Thyroid profiles (T3-0.89 ng/mL; T4-9.8 μg/dL; TSH-1.71 μIU/mL) were with in normal range. Ultrasonography abdomen showed mixed echogenic predominantly hyperechoic lesion seen in the region of right adrenal gland. Computed tomography of abdomen revealed well defined hypodense fat density solid lesion (−120 HU) seen in the right adrenal gland measuring 6.3 cm × 6.2 cm × 5 cm (Fig. 1.) Urinary VMA levels estimated to be normal (56.0 μmol/24 h).Patient was planned for open right adrenalectomy under GA. Right adrenal gland is accessed with anterior approach using Kocher's incision. Intra operatively large tumor(Figs. 2 and 3) measuring about 7 cm × 7 cm × 5 cm was found in relationship with the superior pole of the right kidney, right adrenalectomy was done and specimen subjected for histopathological examination. Patient had an uneventful post operative recovery. Histopathological report revealed features of myelolipoma with an area of adrenal cortical tissue (Fig. 4)
Fig. 1.
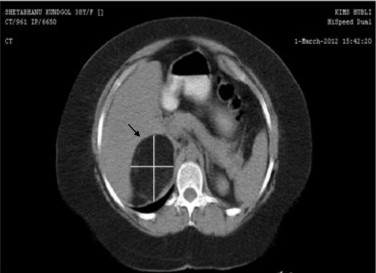
Computed tomography image showing(with pointer)well defined hypodense fat density solid lesion seen in the right adrenal gland measuring 6.3 cm × 6.2 cm × 5 cm suggestive of Right adrenal myelolipoma.
Fig. 2.
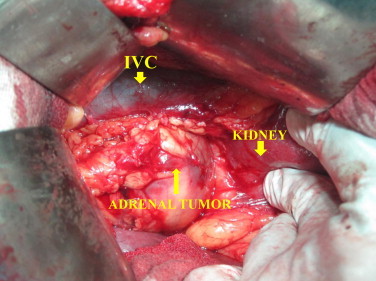
Intra-operative photograph showing large tumor in relationship with the superior pole of the right kidney.
Fig. 3.

Gross right adrenalectomy specimen showing globular well encapsulated gray brown to gray yellow mass with smooth external surface measuring 7 cm × 7 cm × 5 cm. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
Fig. 4.
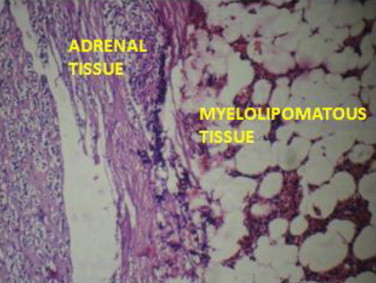
Microscopic picture showing myelolipoma with area of adrenal cortical tissue.
3. Discussion
Myelolipoma is an uncommon, benign; tumor like lesion composed of mature adipose tissue admixed with hematopoietic cells. Most myelolipomas appear as unilateral adrenal masses; however similar lesions may develop in the extra-adrenal sites in the retropertoneum. The mean age at diagnosis is approximately 50 years, and most patients are asymptomatic. Sometimes however, patients have evidence of flank pain with or without a palpable mass or hematuria. Adrenal myelolipomas are detected as incidentalomas during imaging performed for unrelated reasons. The typical myelolipoma is a nonencapsulated but circumscribed lesion that is bright yellow with foci of tan-brown discoloration. At the microscopic level, the lesions are composed of mature adipose tissue with scattered islands of hematopoietic cells. Areas of necrosis, hemorrhage, cyst formation and calcification or ossification may also be evident, particularly in large tumors. Foci of myelolipomatous change may be found in cortical adenomas and cortical hyperplasia and with in otherwise normal adrenal glands. As a result it has been debatable whether myelolipomas are true neoplasms or reactive process.3 Bishop et al. recently demonstrated the clonal origin of these tumors.4
Radiological imaging of myelolioma show typical round, well- marginated encapsulated masses. However, the hallmark of imaging of these tumors by CT, ultrasound or MRI is identification of the areas of gross fat within the lesion. On CT, varying proportions of low density fat in myelolipomas are interspersed with foci of high attenuation myeloid tissue. The fat component should parallel the attenuation of retroperitoneal fat, with components of the mass having HU attenuation ranging from −150 to −50. Soft tissue component may enhance after contrast administration. On MRI, the sometimes heterogeneous foci of macroscopic fat have hyperintense signal on non-fat suppression T1-weighted images and should lose SI with fat suppression. If this high SI persists with fat-suppression techniques, hemorrhage should be suspected. The hematopoietic elements are typically intermediate SI on T1- and T2-weighted images and may enhance on post gadolinium images.5
Hsu et al. reported following 10-year single center experience that adrenal myelolipoma is uncommon and easily confused with malignancy when of large size (≥6 cm). Surgery may be reserved for symptomatic cases and those lesions that cannot reliably be diagnosed. Large tumors (≥6 cm) can be excised surgically or laparoscopically.6
Noble et al. reported that in most cases, a lesion was found at exploration that did not appear to be malignant.7
Myelolipoma can present as acute abdomen following tumor hemorrhage. These tumors generally do not warrant adrenalectomy unless there is concern regarding malignancy, which is rare, or bleeding into the lesion, which is more likely in myelolipomas greater than 4 cm in size. In general Patients with functional and/or ≥6 cm tumors should undergo adrenalectomy, those with nonfunctioning tumors ≤4 cm with benign imaging characteristics may be serially followed, and the appropriate management of lesions between 4 and 6 cm should consider factors such as radiographic characteristics, growth, and patient concern.
In our case patient was symptomatic and the tumor size was >6 cm; hence was subjected for surgery.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
4. Conclusion
Adrenal myelolipoma are rare benign tumors, incidentally detected on CT. CT or MRI is diagnostic. Large myelolipoma warrants surgery due to the risk of hemorrhage.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent taken.
Author contributions
Dr. Gurushantappa H. Yalagachin, Professor of surgery, Karnataka Institute of Medical Sciences, Hubli, Karnataka, India; Study design, data collection, data analysis with review of literature done by main author.
Dr. Bharath Kumar Bhat, Post graduate student, Department of Surgery, KIMS, Hubli; writing and data collection.
References
- 1.Song J.H., Chaudhry F.S., Mayo-Smith W.W. The incidental adrenal on CT: prevalence of adrenal disease in 1049 consecutive adrenal masses in patients with no known malignancy. American Journal of Roentgenology. 2008;190:1163–1168. doi: 10.2214/AJR.07.2799. [DOI] [PubMed] [Google Scholar]
- 2.Ichikawa H. Myelolipoma of the adrenal gland. British Journal of Radiology. 1981;69:777–779. doi: 10.1016/s0022-5347(17)54745-x. [DOI] [PubMed] [Google Scholar]; Ichikawa H. Myelolipoma of the adrenal gland. Journal of Urology. 1981;126:777–779. doi: 10.1016/s0022-5347(17)54745-x. [DOI] [PubMed] [Google Scholar]
- 3.Kenney P.J., Wagner B.J., Rao P., Heffess C.S. Myelolipoma: CT and pathological features. Radiology. 1998;208:8–95. doi: 10.1148/radiology.208.1.9646797. [DOI] [PubMed] [Google Scholar]
- 4.Bishop E., Eble J.N., Cheng L., Wang M., Chase D.R., Orazi A. Adrenal myelolipomas show nonrandom X-chromosome inactivation in hematopoietic elements and fat: support for a clonal origin of myelolipomas. American Journal of Surgical Pathology. 2006;30(July (7)):838–843. doi: 10.1097/01.pas.0000202044.05333.17. [DOI] [PubMed] [Google Scholar]
- 5.Rao P., Kenney P.J., Wagener B.J., Davidson A.J. Imaging and pathological features of myelolipoma. Radiographics. 1997;17:1373–1385. doi: 10.1148/radiographics.17.6.9397452. [DOI] [PubMed] [Google Scholar]
- 6.Hsu S.-W., Shu K., Lee W.-C., Cheng Y.-T., Po-Hui Chiang P.-H. Adrenal myelolipoma: a 10-year single-center experience and literature review. The Kaohsiung Journal of Medical Sciences. 2012;28(July (7)):377–382. doi: 10.1016/j.kjms.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Noble M.J., Montague D.K., Levin H.S. Myelolipoma: an unusual surgical lesion of the adrenal gland. Cancer. 1982;49:952–958. doi: 10.1002/1097-0142(19820301)49:5<952::aid-cncr2820490520>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]


