Abstract
Purpose
Odontoid fractures are the most common cervical spine fractures in the elderly. As the population ages, their incidence is expected to increase progressively. The optimal treatment of this condition is still the subject of controversy. The objective of this review is to summarize and compare the outcome of surgical and conservative interventions in the elderly (≥65 years).
Methods
A comprehensive search was conducted in nine databases of medical literature, supplemented by reference and citation tracking. Clinical status was considered the primary outcome. Fracture union and stability rates were considered secondary outcomes.
Results
A total of nineteen studies met the inclusion criteria. All studies were performed retrospectively and were of limited quality. There was insufficient data, especially from direct comparisons, to determine the difference in clinical outcome between surgical and conservative interventions. Osseous union was achieved in 66–85 % of surgically treated patients and in 28–44 % of conservatively treated patients. Fracture stability was achieved in 82–97 % of surgically patients and in 53–79 % of conservatively treated patients.
Conclusions
There was insufficient data to determine a potential difference in clinical outcome between different treatment groups. Surgically treated patients showed higher osseous union rates compared to conservatively treated patients, possibly because of different selection mechanisms. The majority of patients appears to achieve fracture stability regardless of the applied treatment. A prospective trial with appropriate sample size is needed to identify the optimal treatment of odontoid fractures in the elderly and predictors for the success of either one of the available treatments.
Keywords: Odontoid fractures, Elderly, Surgical treatment, Conservative treatment, Systematic review
Introduction
Odontoid fractures account for 9–18 % of all cervical spine fractures and are most frequently caused by either hyperextension or hyperflexion [5, 14, 20, 22, 34, 37]. In the elderly, odontoid fractures are the most common cervical spine fractures [17, 18, 20, 22, 29, 30, 35]. Moreover, as the population ages, these fractures will become increasingly relevant to clinical practice [37]. The optimal treatment of odontoid fractures in the elderly is, however, still subject to controversy. This age group typically suffers from an increased risk of operation complications when treated surgically as well as from an increased risk of non-union and prolonged treatment duration when treated conservatively.
The treatment for patients with fractures of the odontoid process should be based on fracture pattern (such as defined by Anderson and D’alonzo [1]), patient age, neurological deficits and the patient’s medical condition [20]. Many factors have to be taken into account to find the right balance between fracture healing and treatment complications. Based on these factors, the decision for either surgical or conservative treatment is made.
Surgical intervention is in most cases performed by anterior odontoid screw fixation or posterior atlantoaxial arthrodesis. The general presumption is that a surgical intervention leads to a stable cervical spine. However, the condition of the patient may deteriorate by undergoing (major) cervical spine surgery. Especially in the very old patient (≥80 years of age), a surgical intervention leads to significant risks for the patient.
An alternative to surgical stabilization is conservative treatment, involving rigid or non-rigid immobilization. Such treatment is often proposed to avoid the complications that may accompany spine surgery. However, this may result in non-union and prolonged fracture instability, requiring secondary surgery. This unnecessarily lengthens treatment duration and, worse, can cause significant deterioration of the cervical spine anatomy.
The objective of this review is to summarize and compare the outcome of surgical and conservative treatments for type II and III odontoid fractures in the elderly (≥65 years), focusing primarily on clinical outcome and secondarily on fracture union and stability rates.
Methods
Search methods for identification of studies
A comprehensive and systematic search was conducted in nine databases of medical literature: MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, Web of Science, CINAHL, Academic Search Premier, ScienceDirect, PEDro and RCT-registers up to April 2012. The MEDLINE search strategy is given in Table 1. The search strategy was adapted for the other databases. No restriction was made with regard to language or date. ‘Os odontoideum’ was included in the search, as this term is sometimes incorrectly used to describe odontoid fractures. References from the included studies were also screened in order to identify additional primary studies not previously identified. Two review authors (JH, WJ) working independently from one another examined titles and abstracts from the electronic search. Full articles were obtained if necessary. The third review author (CV) was consulted, if consensus was not reached.
Table 1.
The MEDLINE search strategy
| (“Odontoid fractures” OR “Odontoid fracture” OR “Os odontoideum” OR “c2 fracture” OR “c2 fractures” OR “c-2 fracture” OR “c-2 fractures” OR “dens fracture” OR “dens fractures” OR ((Fractures OR fracture OR fracture* OR injury OR injuries OR “Spinal Injuries”[mesh]) AND (odontoid OR odontoid* OR dens)) OR “Odontoid Process/injuries”[mesh]) AND (“Aged”[mesh] OR Aged OR “Aged, 80 and over”[mesh] OR Elderly OR Old* OR Elder* OR Geriatric*) NOT (“child”[mesh] NOT “aged”[mesh]) |
Criteria for considering studies for this review
References were selected if they met all of the following inclusion criteria:
The study design was either a randomised controlled trial, a non-randomised study with (concurrent or historical) control group or a case series
A minimum of ten subjects was included
The patients included suffered from acute, isolated type II or III odontoid fractures with or without associated luxation
The patients included were at least 65 years old or their data could be extracted separately from studies that also involved younger subjects
The criteria for inclusion were explicit (e.g. age range given, co-morbidity)
Number of patients deceased or lost to follow-up reported or included in appropriate statistical analysis
The study evaluated the results of any surgical and/or conservative treatment
Results were given for each distinct treatment in the study
The outcome(s) evaluated included at least one of the main clinically relevant outcome measures (e.g. using NDI, Smiley-Webster scale, CSOQ) and/or radiologically assessed union or stability data
Patients were not treated for odontoid fractures in the past that were unrelated to the reporting study
Patients did not suffer from systemic co-morbidity (e.g. rheumatoid arthritis)
The follow-up period was at least 2 weeks
The paper was published in a peer-reviewed journal
Clinical status was considered the primary outcome. The Neck Disability Index (NDI) was expected to be the most commonly used tool to assess clinical outcome. Therefore, the minimal clinically important difference (MCID/MCIC) for the NDI was predetermined to be 7.5 [6, 8, 38, 39].
Fracture union and stability rates were considered the secondary outcomes.
Assessment of risk of bias for the included studies
Two review authors (JH, CV) working independently of each other conducted the risk-of-bias assessment and data extraction. Risk of bias of the individual studies was assessed with methodology scores based on the type of study concerned: Cochrane form II for RCTs [9], Cochrane form III for cohort studies [10], Cochrane form IV for patient control studies [11] and a self-designed appraisal form for uncontrolled case series based on three other studies [7, 12, 36]. The criteria for risk-of-bias assessments of case series are given in Table 2. Items were scored as positive if they fulfilled the criterium, negative when bias was likely or marked as inconclusive if there was insufficient information. Differences in the scoring of the risk-of-bias assessment and data extraction were discussed during a consensus meeting. If an item was scored positive, one point was awarded. The number of positively scored items was summated per study.
Table 2.
Criteria for risk-of-bias assessment (scored as ‘yes’, ‘no’, ‘inconclusive’ or ‘not applicable’)
| Criteria for ‘yes’ | |
|---|---|
| Key criteria | |
| Clear study objective (B) | Goal of the study mentioned and motivated |
| Criteria for inclusion explicit (B) | Inclusion criteria mentioned |
| Fractures appropriately described (B) | Classification system and radiological tools used mentioned |
| Distinction type II/III appropriate (B) | Classification system and radiological tools used mentioned |
| Mean age (range) (B) | Mean age and age range reported or computable |
| Selection bias ruled out | Methods for patient selection and inclusion mentioned |
| Mean follow-up (range) (R) | Follow-up data reported or computable |
| Surgical treatment(s) specified (B) | Types of performed surgical interventions described |
| Conservative treatment(s) specified (B) | Types of performed conservative interventions described |
| Clear criteria for measuring outcomes (B) | Outcome measures mentioned |
| Clinically relevant outcomes (e.g. NDI, Smiley-Webster Scale, CSOQ) (B) | Clinical outcome systematically evaluated |
| When clinical outcome reported: Is pre-treatment neurol status stated (B) | Pre-treatment status reported for comparison to post-treatment status |
| Results for surgical/conservative treatment separately given (R) | If applicable; results for treatments separately reported |
| Selective loss-to-follow-up ruled out (R), scored as: ‘yes’ (2 pt) ‘no, l.t.f.u. <20 %, but may not be a selective’ (1 pt) ‘no, l.t.f.u. >20 %’ (0 pt) → exclusion criterium ‘too little information/not described’ (0 pt) |
Number of patients lost to follow-up reported including its causes |
| Other criteria | |
| Valid statistical analysis undertaken (R) | Statistical analyses carried out; if impossible: ‘NA’ |
| Number of men and women given (B) | Gender distribution of included patients reported or extractable |
| Clinical evaluation independent of treating physician (R) | Evaluation carried out by independent party |
| Radiological evaluation independent and blinded to clinical results (R) | Evaluation carried out by independent party |
| Independence of investigators stated (R) | Independence specifically stated (no vested interest) |
| Quantification of outcomes (R), scored as: ‘yes, >5 scale-classification (3 pt) ‘yes, <5 scale-classification (2 pt) ‘yes, descriptive’(1 pt) ‘no’ (0 pt) ‘too little information’ (0 pt) |
Categorized according to the scale used for outcome measures |
B Concerning baseline data
R Concerning results
Data collection and analysis
Data was extracted onto separate, pre-developed forms depending on the type of study concerned. From each study, both demographic/descriptive data (e.g. study population, types of treatment, types of outcomes assessed, sample size, age, gender) and quantitative data regarding primary and secondary outcomes were extracted. With sufficient clinically and statistically homogeneous and comparable reported outcomes, data was planned to be pooled with the aid of Revman 5 for studies with control group and Excel for case series. To identify publication bias, funnel plots were planned to be examined. Secondary analysis was to be carried out based on fracture union and stability rates. Subgroup analysis was planned to be carried out based on fracture type.
Results
Search and selection results
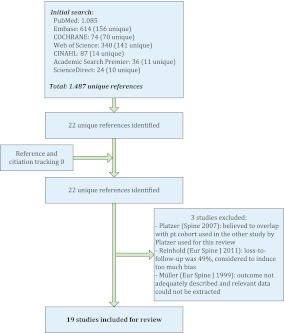
The initial search yielded 1,487 unique references; 159 studies were either discussed during the consensus meeting or a full-text version of the article was obtained. Additionally, reference and citation tracking were carried out that yielded no further references. A total of 22 studies was initially identified. Three of these studies were subsequently excluded [28, 31, 32]. The study by Platzer et al. [31] was excluded because the patient cohort in this study was believed to overlap with the patient cohort described in the other study by Platzer that was used for this review [30]. The study by Reinhold et al. [32] was excluded because loss-to-follow-up was 49 %, which was considered to induce too much bias. The study by Müller et al. [28] was excluded as the outcome was not adequately described and relevant data could not be extracted.
A total of 19 studies (all were case series) was eventually identified for this review, 5 with control groups (Fig. 1). Of these 19 studies, 11 systematically reported clinical outcome and hence were primarily included. The other eight studies that only reported union and stability rates were secondarily included. Only five studies compared outcomes for surgical treatment to conservative treatment in the elderly; in two of these studies, clinical outcome was assessed, four studies reported union data and all five reported data regarding fracture stability. Seventeen studies were published in English, one in French and one in German. The main characteristics of the included studies are given in Table 3. The results of the data extraction are given in Tables 4 and 5.
Fig. 1.
Flow chart for inclusion of studies
Table 3.
Characteristics of included studies
| Inclusion criteria | Interventions | Sample size | Number of pt. followed-up | μ Age (year) (range) μ = 79.7 |
Sex | CT/MRI for diagnosis | ||
|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||
| Primary included | ||||||||
| Seybold [33] | Type II–III | S & C | 22 | 18 | 77.9 (65–93) | 10 | 12 | ? |
| Hénaux [18] | Type IIB, >80 year | S | 11 | 9 | 85.4 (82–93) | 4 | 7 | Yes |
| Koech [22] | Type II, >65 year | C | 57 | 42 | 80 (67–91) | 9 | 33 | Yes |
| Platzer [30] | Type I–III, >65 year, “complete sets of clinical data”, surgical treatment | S | 62 | 56 | 71.4 (66–83) | 25 | 31 | Yes |
| Osti [29] | Type II, >65 year | S | 35 | 25 | 79.6 (65.1–94) | 18 | 15 | Yes |
| Hou [19] | Type II, >65 year, anterior screw fixation | S | 43 | 42 | 80.6 (65–92) | 24 | 19 | ? |
| Kaminski [German] [21] | OF/pseudoarthrosis, >70 year | S | 36 | 28 | 80.1 (70–93) | 14 | 22 | Yes |
| Butler [5] | Type II, external immobilization | C | 14 | 14 | ? (?–80) | Cannot retrieve | Yes | |
| Lefranc [French] [25] | Type II–III, >70 year | S & C | 27 | 22 | 80.7 (70–97) | 13 | 14 | ? |
| Molinari JSDT [26] | Type II, >65 year, ≥50 % odontoid displacement, posterior fusion | S | 26 | 21 | 79 (65–90) | 14 | 12 | ? |
| Molinari ESJ [27] | Type II, >65 year, ≤50 % odontoid displacement, external immobilization | C | 34 | 32 | 84 (71–99) | 17 | 17 | ? |
| Secondary included | ||||||||
| Dailey [13] | Type II–III, >70 year | S | 57 | 42 | 81.2 (70–96) | 27 | 30 | ? |
| Kuntz [24] | Type II, >65 year | S & C | 20 | 20 | 78.9 (66–92) | 12 | 8 | Yes |
| Koivikko [23] | Type II | C | 25 | 25 | ? (65–94) | Cannot retrieve | ? | |
| Börm [34] | Type II, >70 year | S | 15 | 15 | 81 (70–?) | Cannot retrieve | Yes | |
| Andersson [2] | Type II–III, >65 year | S & C | 29 | 27 | 78 (66–99) | 11 | 18 | ? |
| Berlemann [3] | Type II, >65 year | S | 19 | 19 | 75 (65–87) | 10 | 9 | ? |
| Hanigan [15] | Type II–III, >80 year | S & C | 19 | 19 | 86.2 (80–99) | 9 | 10 | ? |
| Hanssen [16] | Type II–III | C | 18 | 11 | 76 (65–87) | 10 | 8 | ? |
S surgical, C conservative, ? cannot tell or not retrievable
Table 4.
Results of data extraction
| μ Follow-up (mo)—(range) | Adverse effects | Baseline clinical status | Clinical outcome | |||
|---|---|---|---|---|---|---|
| μ = 29 | Surgical | Conservative | Surgical | Conservative | ||
| Primary included | ||||||
| Seybold [33] | 21 (0–109) | – | 1.25 (SW) | 1.92 (SW) | ||
| Hénaux [18] | 34 (2–116) | All ASIA E | 2.18 (SW) | |||
| Koech [22] | Median = 24 (9–24) | 1 × cervical collar-related decubitus ulceration, 2 × halo-vest-related pressure ulceration, 1 × decreased halothoracic pin tension | – | 2.05 (SW) | ||
| Platzer [30] | 24 (24–24) | 4 × mortality, 3 × reoperations | ASA average: 2.2 | 1.68 (SW) | ||
| Osti [29] | 74 (9.6–128) | 8.6 % mortality | All ASIA E | 1.65 (SW) | ||
| Hou [19] | 21.3 (18–24) | Frankel: 1 × C, 3 × D | 1.67 (Robinson’s criteria) | |||
| Kaminski [German] [21] | Clinical = 38, radiological = 23 (12–72) | 2 × screw misplaced, 1 × wound infection | 1 × ASIA D | Pain: 27/28 good-very good and 1 pt required pain killers, Activity: 20/28 very good, 6/20 good, 1/20 satisfying, 1/20 inadequate | ||
| Butler [5] | 66* (cannot retrieve) | – | CSOQ: neck pain (33.88 ± 27.08), shoulder/arm pain (35.10 ± 28.20), phys. symp. (38.57 ± 26.75), funct. disability (33.93 ± 18.04), psych. distress (45.24 ± 24.64) | |||
| Lefranc [French] [25] | 12 (cannot retrieve) | Neck pain, retropharyng. hematoma, neurol. signs | Rankin score average: 0.1 | Rankin score average: 0.7 | ||
| Molinari JSDT [26] | 14 (1–48) | 19.2 % mortality | – | 18.1 (NDI) | ||
| Molinari ESJ [27] | 15 (2–48) | 11.8 % mortality, 5.9 % collar-related complications | – | 15.7 (NDI) | ||
| Secondary included | ||||||
| Dailey [13] | 15 (3–62) | 1 × myocardial infarction | NA | NA | NA | |
| Kuntz [24] | Surg = 17, cons = 13 (0–36) | 1 × revision surgery, 1 × death after surgery | 1 × death | NA | NA | NA |
| Koivikko [23] | 12.2* (2–82) | NA | NA | NA | ||
| Börm [4] | 17* (cannot retrieve) | 1 × surgery related death | NA | NA | NA | |
| Andersson [2] | 51 (24–89) | 10 × died from unrelated causes during the follow-up period [S or C?] | NA | NA | NA | |
| Berlemann [3] | Clinical = 54, radiological = 30 (3.6–132) | 1 × hematoma requiring reoperation | NA | NA | NA | |
| Hanigan [15] | Surg = 44.8, cons = 19.9 (5–72) | 1 × mortality | 5 × mortality | NA | NA | NA |
| Hanssen [16] | 31 (6–60) | NA | NA | NA | ||
* For entire pt group studied (i.e. including pt <65 years), ASIA American Spinal Injury Association Impairment Scale, ASA American Society of Anesthesiologists Physical Status Classification System, SW Smiley-Webster score, CSOQ Cervical Spine Outcomes Questionnaire, NA not applicable/available
Table 5.
Results of data extraction—fracture healing
| Osseous union | Fracture stability | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgical | Conservative | Surgical | Conservative | |||||||||
| Union | Non-union | Cannot tell | Union | Non-union | Cannot tell | Stable | Unstable | Cannot tell | Stable | Unstable | Cannot tell | |
| Primary included | ||||||||||||
| Seybold [33] | 2 | 2 | 11 | 7 | ||||||||
| Hénaux [18] | 4 | 5 | 2 | 9 | 2 | |||||||
| Koech [22] | 17 | 25 | 15 | 41 | 1 | 15 | ||||||
| Platzer [30] | 52 | 4 | 6 | 52 | 10 | |||||||
| Osti [29] | 18 | 7 | 10 | 18 | 17 | |||||||
| Hou [19] | 36 | 6 | 1 | 41 | 1 | 1 | ||||||
| Kaminski [German] [21] | 28 | 0 | 8 | 28 | 0 | 8 | ||||||
| Butler [5] | 9 | 5 | 13 | 1 | ||||||||
| Lefranc [French] [25] | 9 | 1 | 6 | 4 | 7 | 10 | 0 | 10 | 0 | 7 | ||
| Molinari JSDT [26] | 7 | 14 | 5 | 21 | 0 | 5 | ||||||
| Molinari ESJ [27] | 2 | 30 | 2 | 11 | 21 | 2 | ||||||
| Secondary included | ||||||||||||
| Dailey [13] | 24 | 18 | 15 | 34 | 8 | 15 | ||||||
| Kuntz [24] | 4 | 2 | 3 | 6 | 5 | 4 | 2 | 6 | 3 | 5 | ||
| Koivikko [23] | 6 | 19 | 6 | 19 | ||||||||
| Börm [4] | 11 | 4 | 13 | 2 | ||||||||
| Andersson [2] | 14 | 1 | 3 | 2 | 6 | 3 | 14 | 1 | 3 | 2 | 6 | 3 |
| Berlemann [3] | 16 | 2 | 1 | 17 | 1 | 1 | ||||||
| Hanigan [15] | 2 | 3 | 5 | 4 | 5 | 5 | 0 | 8 | 1 | 5 | ||
| Hanssen [16] | 8 | 3 | 7 | 9 | 1 | 8 | ||||||
| SUM | 225 | 65 | 53 | 58 | 102 | 44 | 268 | 13 | 44 | 117 | 34 | 71 |
| % Including ‘cannot tell’ (sensitivity) | 66 % | 28 % | 82 % | 53 % | ||||||||
| % Excluding ‘cannot tell’ | 78 % | 36 % | 95 % | 77 % | ||||||||
| % In studies comparing S to C treatment | 85 % | 44 % | 97 % | 79 % | ||||||||
Risk-of-bias assessment
The results of the risk-of-bias assessment are given in Table 6. All studies were retrospective case series, with their associated limitations (such as missing data and variability in outcome assessment). Most baseline demographic data were adequately described in all studies, with scores ranging from 7 to 10 on a 11-point scale. However, baseline data regarding clinical status were poorly reported. Only six of the primary included studies systematically reported baseline clinical status and they all applied different tools for the pre- and post-treatment measurements. Data concerning the results of the studies were less extensively reported than baseline data. Scores ranged between 3 and 8 on a 11-point scale.
Table 6.
Results of risk-of-bias assessment of the individual studies
| Primary included | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Seybold [33] | Hénaux [18] | Koech [22] | Platzer [30] | Osti [29] | Hou [19] | Kaminski [21] | Butler [5] | Lefranc [25] | Molinari JSDT [26] | Molinari ESJ [27] | |
| Key criteria | |||||||||||
| Clear study objective | + | + | + | + | + | + | + | + | – | + | + |
| Criteria for inclusion explicit | + | + | + | – | + | + | + | + | + | + | + |
| Fractures appropriately described | + | + | + | + | + | + | – | + | + | + | + |
| Distinction Type II/III appropriate | + | + | + | + | + | + | – | + | + | ? | ? |
| Mean age (range) | + | + | + | + | + | + | + | + | + | + | + |
| Selection bias ruled out | + | + | + | – | + | + | + | + | + | + | + |
| Mean follow-up (range) | + | + | + | + | + | + | + | + | + | + | + |
| Surgical treatm. specified | + | + | NA | + | + | + | + | NA | + | + | NA |
| Conservative treatm. specified | – | NA | + | NA | NA | NA | NA | + | + | NA | + |
| Clear criteria for measuring outcomes | + | + | + | + | + | + | + | + | + | + | + |
| Clinically relevant outcomes | + | + | + | + | + | + | + | + | + | + | + |
| When clinical outcome reported: Is pre-treatment neurol status stated | – | + | – | + | + | + | + | – | + | – | – |
| Results for surg/cons treatm. separately given | + | NA | NA | NA | NA | NA | NA | NA | + | NA | NA |
| Selective l.t.f.u. ruled out | No, l.t.f.u. >20 % | Yes | Yes | Yes | No, l.t.f.u. >20 % | Yes | No, l.t.f.u <20 % | Yes | Yes | Yes | Yes |
| Other criteria | |||||||||||
| Valid statistical analysis | + | NA | NA | + | + | NA | NA | + | + | + | + |
| Number of men and women given or extractable | – | + | + | + | + | + | + | + | + | + | + |
| Clinical evaluation independent of treating physician | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? |
| Radiological evaluation independent and blinded | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? | ? |
| Independence of investigators stated | – | + | + | + | + | + | + | – | – | + | + |
| Quantification of outcomes | Yes, <5 scale | Yes, <5 scale | Yes, <5 scale | Yes, <5 scale | Yes, <5 scale | Yes, <5 scale | Yes, <5 scale | Yes, >5 scale | Yes, >5 scale | Yes, <5 scale | Yes, <5 scale |
| Results | |||||||||||
| Selection bias ruled out | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Baseline (max 11 points) | 8 | 10 | 9 | 9 | 10 | 10 | 8 | 9 | 10 | 8 | 8 |
| Results (max 11 points) | 5 | 6 | 6 | 7 | 5 | 6 | 5 | 7 | 8 | 7 | 7 |
| Secondary included | ||||||||
|---|---|---|---|---|---|---|---|---|
| Dailey [13] | Kuntz [24] | Koivikko [23] | Börm [4] | Andersson [2] | Berlemann [3] | Hanigan [15] | Hanssen [16] | |
| Key criteria | ||||||||
| Clear study objective | + | + | + | + | + | + | + | + |
| Criteria for inclusion explicit | + | + | + | + | + | + | + | + |
| Fractures appropriately described | + | + | – | + | + | + | + | + |
| Distinction Type II/III appropriate | + | + | + | + | + | + | + | + |
| Mean age (range) | + | + | + | + | + | + | + | + |
| Selection bias ruled out | + | + | – | + | + | + | – | + |
| Mean follow-up (range) | + | + | + | – | + | + | + | + |
| Surgical treatm. specified | + | + | – | + | + | + | + | NA |
| Conservative treatm. specified | NA | + | + | NA | + | NA | + | + |
| Clear criteria for measuring outcomes | + | + | + | + | + | + | + | + |
| Clinically relevant outcomes | – | – | – | +NE | +NE | +NE | +NE | – |
| When clinical outcome reported: Is pre-treatment neurol status stated | NA | NA | NA | +NE | +NE | +NE | – | NA |
| Results for surg/cons treatm. separately given | NA | + | NA | NA | + | NA | + | NA |
| Selective l.t.f.u. ruled out | No, l.t.f.u. <20 % | Yes | Yes | Yes | Yes | Yes | Yes | No, l.t.f.u. <20 % |
| Other criteria | ||||||||
| Valid statistical analysis | NA | + | + | + | – | – | – | – |
| Number of men and women given or extractable | + | + | + | + | + | + | + | + |
| Clinical evaluation independent of treating physician | ? | ? | ? | ? | ? | ? | ? | ? |
| Radiological evaluation independent and blinded | ? | ? | ? | ? | ? | ? | ? | ? |
| Independence of investigators stated | – | – | + | – | – | – | – | – |
| Quantification of outcomes | Yes, <5 scale | Yes, descr. | Yes, descr. | Yes, <5 scale | Yes, <5 scale | Yes, descr. | Yes, descr. | Yes, descr. |
| Results | ||||||||
| Selection bias ruled out | Yes | Yes | No | Yes | Yes | Yes | No | Yes |
| Baseline (max 11 points) | 8 | 9 | 7 | 10 | 11 | 10 | 10 | 8 |
| Results (max 11 points) | 4 | 5 | 6 | 5 | 6 | 4 | 6 | 3 |
+ Yes, - no, ? cannot tell, NA not applicable, NE not extractable for review purposes
Clinical outcome
A variety of tools was used to assess clinical outcome. The NDI, which was expected to be widely applied, was used in only two of the included studies. The Smiley-Webster scale was the most commonly applied tool to assess clinical outcome, used in five studies. The Cervical Spine Outcomes Questionnaire was used in one study, as were the Robinson’s criteria, Rankin score and a self-designed pain-and-activity scoring scale. These variations made it impossible for statistical analyses to be carried out and limited the comparisons that could be made.
Surgery versus conservative care in individual studies
Of the eleven studies reporting clinical outcome, only two studies compared surgical to conservative treatment [25, 33]. However, these two studies applied different tools to assess clinical outcome, using the Rankin score [25] (0 = without symptoms; 5 = major handicap) and Smiley-Webster (SW) scale [33] (1 = excellent; 4 = poor), respectively, and hence could not adequately be compared. One of these studies [25] showed statistically less morbidity in the surgery group (p = 0.037), but no significant difference in non-union at fracture site (p = 0.64) except for type II fractures (p = 0.028) [25]. However, this was a very small study, which makes these estimates unstable. The other study showed a slightly better clinical outcome in surgically compared to conservatively treated patients (average Smiley-Webster score 1.25 and 1.92, respectively). Statistical analysis of these results could not be performed due to the limited number of patients involved (n = 17) [33].
Outcome compared between studies
In the two studies applying the NDI, groups were evidently different; patients in one group had ≥50 % odontoid displacement and were treated surgically [26], those in the other group had ≤50 % odontoid displacement and were treated by external immobilization [27], still showing a slightly better outcome for surgically treated patients (18.1 and 15.7, respectively). This difference was, however, not clinically relevant. In the five studies evaluating the clinical outcome using the Smiley-Webster scale, both surgically and conservatively treated patients had an intermediate outcome [18, 22, 29, 30, 33]. The SW score for surgically treated patients averaged at 1.71, the SW score for conservatively treated patients averaged at 2.02. The remaining studies all used different instruments to assess outcome and hence could not be compared.
Osseous union
In eighteen studies reporting extractable union rates, four compared surgical to conservative treatment. In these four studies, union was achieved in 85 % (29/34) of the surgically treated patients and in 44 % (16/36) of the conservatively treated patients [2, 15, 24, 25]. The results were mainly based on X-ray data. In the individual studies no statistical analysis could be performed due to the small number of patients. In a comparison of all patients included in the eighteen studies, union was achieved in 66 % (225/343) of surgically treated patients and 28 % (58/204) of conservatively treated patients. When patients whose outcome was unclear are left out of the calculation, union was achieved in 78 % (225/290) of surgically treated and in 36 % (58/160) of conservatively treated patients. Again, in the individual studies no statistical analysis could be carried out because of the limited number of patients included.
Fracture stability
All nineteen studies reported extractable stability rates, showing fracture stability in the majority of patients regardless of their treatment. Stability was in most studies assessed with dynamic X-ray. In five studies comparing surgically to conservatively treated patients, stability was achieved in 97 % (35/36) and 79 % (37/47) of cases, respectively [2, 15, 24, 25, 33]. In a comparison of all patients included in the nineteen studies, stability was achieved in 82 % (268/325) of surgically treated patients and in 53 % (117/222) of conservatively treated patients. When patients whose outcome was unclear were left out of the calculation, stability was achieved in 95 % (268/281) of surgically treated patients and in 77 % (117/151) of conservatively treated patients.
Discussion
The studies identified for this review were all performed retrospectively, mostly without the use of a control group. Due to the small numbers of patients and the rather poor quality of the acquired data, no strong recommendations can be made with regard to the optimal treatment. A variety of tools was used to assess clinical outcome. The Smiley-Webster scale, the only instrument used in multiple studies, showed a slightly better outcome for surgically treated patients than for conservatively treated patients. However, pre-treatment status was poorly reported and the grounds for starting specific treatments are unknown. Osseous union in surgically treated patients was twice as high as in conservatively treated patients, but if non-union leads to stability (e.g. fibrous union), fracture stability is a more important and relevant parameter to evaluate. The results of this review indicate that fracture stability can be achieved in the majority of patients, regardless of the applied treatment or presence of osseous union. Adverse effects were common in both treatment groups, with mortality rates as high as 20 %. Complications related to the operation, such as screw misplacement, were the most common complications in surgically treated patients. Device-related complications, such as ulcerations, were the most common complication in patients treated conservatively.
Patient age in the included studies was more or less comparable. Mean age for surgically treated patients was 78.9 years. Mean age for conservatively treated patients was 80.0 years. In all but two studies, patients over 65 or 70 years old were included. Two studies included only patients aged over 80 years of age (in one of these studies, patients were treated surgically, in the other, patients were treated both surgically and conservatively). Surgically and conservatively treated groups described in the included studies may, however, not be comparable due to potential differences in a variety of other patient characteristics (i.e. co-morbidity, osteoporosis, severity of comminution). Outcome diversification per age group amongst the elderly was absent and needs further study. It is often postulated that treatment outcome depends on patient age [20]. Other factors must, however, play a role as well, as different studies have shown different outcomes for the same treatment, which cannot be explained by patient age alone (e.g. in the studies by Koech and Molinari [22, 27]).
No consensus exists as to the exact goal of treatment (debate remains as to whether it should be osseous union, fracture stability, or clinical outcome), nor as to how outcome should be measured. Many studies used osseous union rates as primary outcome, fibrous union was underexposed and the correlation with clinical outcome or fracture stability was not properly studied. The results of this review show no evidence that clinical outcome correlates better to fracture union than to fracture stability (i.e. that the quality of union, whether it be osseous or fibrous, is influential on clinical outcome).
Strengths and limitations
The limited number and poor quality of the included studies limits the strength of the results found in this review. Furthermore, type II and III fractures were analysed as one group. However, an evident type II fracture is more often treated surgically, whereas an evident type III fracture is most often treated conservatively. This may have flattened the findings. This choice was made as differentiation of these types is often difficult to make and would even further reduce the amount of data that could be used for this review, as this differentiation was also not made in all of the included studied. As a result, the subgroup analysis that was planned to be carried out based on fracture type has also lapsed.
Conclusions
Implications for clinical practice
Different treatment options for this condition have been extensively reported and their efficacy debated. Based on this review, the following conclusions can be drawn based on the three main outcome parameters.
Clinical outcome: There is insufficient data available to determine a potential difference in clinical outcome between surgical and conservative interventions in the elderly with isolated odontoid fractures
Osseous union: Surgically treated patients appear to show higher osseous union rates compared to conservatively treated patients, although selection mechanisms, especially regarding fracture type, might explain this difference
Stability: The majority of patients appears to achieve fracture stability regardless of the applied treatment
Implications for research
A prospective study with appropriate sample size is necessary to identify the optimal treatment of odontoid fractures in the elderly and predictors for the success of either one of the available treatments.
Acknowledgments
The authors are thankful to Mr. Jan Schoones of the Walaeus Library for carrying out the database search.
Conflict of interest
None.
References
- 1.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56(8):1663–1674. [PubMed] [Google Scholar]
- 2.Andersson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9(1):56–59. doi: 10.1007/s005860050009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berlemann U, Schwarzenbach O. Dens fractures in the elderly: results of anterior screw fixation in 19 elderly patients. Acta Orthop Scand. 1997;68(4):319–324. doi: 10.3109/17453679708996169. [DOI] [PubMed] [Google Scholar]
- 4.Borm W, Kast E, Richter HP, Mohr K. Anterior screw fixation in type II odontoid fractures: is there a difference in outcome between age groups? Neurosurgery. 2003;52(5):1089–1092. doi: 10.1227/01.NEU.0000057697.62046.16. [DOI] [PubMed] [Google Scholar]
- 5.Butler JS, Dolan RT, Burbridge M, et al. The long-term functional outcome of type II odontoid fractures managed non-operatively. Eur Spine J. 2010;19(10):1635–1642. doi: 10.1007/s00586-010-1391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carreon LY, Glassman SD, Campbell MJ, Anderson PA. Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J. 2010;10(6):469–474. doi: 10.1016/j.spinee.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 7.Chan K, Bhandari M. Three-minute critical appraisal of a case series article. Indian J Orthop. 2011;45(2):103–104. doi: 10.4103/0019-5413.77126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cleland JA, Fritz JM, Whitman JM, Palmer JA. The reliability and construct validity of the Neck Disability Index and patient specific functional scale in patients with cervical radiculopathy. Spine (Phila Pa 1976) 2006;31(5):598–602. doi: 10.1097/01.brs.0000201241.90914.22. [DOI] [PubMed] [Google Scholar]
- 9.Cochrane (2012) Cochrane form II for RCTs. http://dcc.cochrane.org/sites/dcc.cochrane.org/files/uploads/RCT.pdf. Accessed 1 March 2012
- 10.Cochrane (2012) Cochrane form III for cohort studies. http://dcc.cochrane.org/sites/dcc.cochrane.org/files/uploads/cohort.pdf. Accessed 1 March 2012
- 11.Cochrane (2012) Cochrane form IV for patient control studies. http://dcc.cochrane.org/sites/dcc.cochrane.org/files/uploads/patient-controleonderzoek.pdf. Accessed 1 March 2012
- 12.Cowley DE. Prostheses for primary total hip replacement: a critical appraisal of the literature. Int J Technol Assess Health Care. 1995;11(4):770–778. doi: 10.1017/S026646230000920X. [DOI] [PubMed] [Google Scholar]
- 13.Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI. Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine. 2010;12(1):1–8. doi: 10.3171/2009.7.SPINE08589. [DOI] [PubMed] [Google Scholar]
- 14.Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5(2):123–129. doi: 10.1016/j.spinee.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 15.Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in the elderly patient. Clin Res. 1993;41(3):A710. doi: 10.3171/jns.1993.78.1.0032. [DOI] [PubMed] [Google Scholar]
- 16.Hanssen AD, Cabanela ME. Fractures of the dens in adult patients. J Trauma. 1987;27(8):928–934. doi: 10.1097/00005373-198708000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Harrop JS, Hart R, Anderson PA. Optimal treatment for odontoid fractures in the elderly. Spine. 2010;35(21):S219–S227. doi: 10.1097/BRS.0b013e3181f32716. [DOI] [PubMed] [Google Scholar]
- 18.Henaux PL, Cueff F, Diabira S, et al. Anterior screw fixation of type IIB odontoid fractures in octogenarians. Eur Spine J. 2011;21(2):335–339. doi: 10.1007/s00586-011-2044-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hou Y, Yuan W, Wang X. Clinical evaluation of anterior screw fixation for elderly patients with type II odontoid fractures. J Spinal Disord Tech. 2011;24(8):75–81. doi: 10.1097/BSD.0b013e3182318517. [DOI] [PubMed] [Google Scholar]
- 20.Hsu WK, Anderson PA. Odontoid fractures: update on management. J Am Acad Orthopaedic Surg. 2010;18(7):383–394. doi: 10.5435/00124635-201007000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Kaminski A, Gstrein A, Muhr G, Muller EJ. Transarticular C1–C2 screw fixation: results of unstable odontoid fractures and pseudarthrosis in the elderly. Unfallchirurg. 2008;111(3):167–172. doi: 10.1007/s00113-007-1383-7. [DOI] [PubMed] [Google Scholar]
- 22.Koech F, Ackland HM, Varma DK, Williamson OD, Malham GM. Nonoperative management of type II odontoid fractures in the elderly. Spine. 2008;33(26):2881–2886. doi: 10.1097/BRS.0b013e31818d5407. [DOI] [PubMed] [Google Scholar]
- 23.Koivikko MP, Kiuru MJ, Koskinen SK, Myllynen P, Santavirta S, Kivisaari L. Factors associated with nonunion in conservatively treated type-II fractures of the odontoid process. J Bone Joint Surg Br. 2004;86(8):1146–1151. doi: 10.1302/0301-620X.86B8.14839. [DOI] [PubMed] [Google Scholar]
- 24.Kuntz C, Mirza SK, Jarell AD, Chapman JR, Shaffrey CI, Newell DW. Type II odontoid fractures in the elderly: early failure of nonsurgical treatment. Neurosurg Focus. 2000;8(6):e7. doi: 10.3171/foc.2000.8.6.8. [DOI] [PubMed] [Google Scholar]
- 25.Lefranc M, Peltier J, Fichten A, Desenclos C, Toussaint P, Le GD. Odontoid process fracture in elderly patients over 70 years: morbidity, handicap, and role of surgical treatment in a retrospective series of 27 cases. Neurochirurgie. 2009;55(6):543–550. doi: 10.1016/j.neuchi.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 26.Molinari RW, Dahl J, Gruhn WL, Molinari WJ. Functional outcomes, morbidity, mortality, and fracture healing in 26 consecutive geriatric odontoid fracture patients treated with posterior fusion. J Spinal Disord Tech. 2011;197(5):1229–1234. doi: 10.1097/BSD.0b013e31823e99e4. [DOI] [PubMed] [Google Scholar]
- 27.Molinari RW, Khera OA, Gruhn WL, McAssey RW. Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J. 2011;21(5):855–862. doi: 10.1007/s00586-011-2069-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8(5):360–365. doi: 10.1007/s005860050188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Osti M, Philipp H, Meusburger B, Benedetto KP. Analysis of failure following anterior screw fixation of Type II odontoid fractures in geriatric patients. Eur Spine J. 2011;20(11):1915–1920. doi: 10.1007/s00586-011-1890-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Platzer P, Thalhammer G, Oberleitner G, Schuster R, Vecsei V, Gaebler C. Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89(8):1716–1722. doi: 10.2106/JBJS.F.00968. [DOI] [PubMed] [Google Scholar]
- 31.Platzer P, Thalhammer G, Ostermann R, Wieland T, Vecsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976) 2007;32(16):1714–1720. doi: 10.1097/BRS.0b013e3180dc9758. [DOI] [PubMed] [Google Scholar]
- 32.Reinhold M, Bellabarba C, Bransford R et al (2011) Radiographic analysis of type II odontoid fractures in a geriatric patient population: description and pathomechanism of the “Geier”-deformity. Eur Spine J 20(11):1928–1939 [DOI] [PMC free article] [PubMed]
- 33.Seybold EA, Bayley JC. Functional outcome of surgically and conservatively managed dens fractures. Spine (Phila Pa 1976) 1998;23(17):1837–1845. doi: 10.1097/00007632-199809010-00006. [DOI] [PubMed] [Google Scholar]
- 34.Shears E, Armitstead CP. Surgical versus conservative management for odontoid fractures. Cochrane Database Syst Rev. 2008;4:CD005078. doi: 10.1002/14651858.CD005078.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tashjian RZ, Majercik S, Biffl WL, Palumbo MA, Cioffi WG. Halo-vest immobilization increases early morbidity and mortality in elderly odontoid fractures. J Trauma. 2006;60(1):199–203. doi: 10.1097/01.ta.0000197426.72261.17. [DOI] [PubMed] [Google Scholar]
- 36.University of Wales, College of Medicine (2011). Critical appraisal form. http://www.core-info.cardiff.ac.uk/thermal/FULL_COTS_critical%20appraisal%20FORM%20B%202007.pdf. Accessed 2 Sept 2011
- 37.White AP, Hashimoto R, Norvell DC, Vaccaro AR. Morbidity and mortality related to odontoid fracture surgery in the elderly population. Spine. 2010;35(9):S146–S157. doi: 10.1097/BRS.0b013e3181d830a4. [DOI] [PubMed] [Google Scholar]
- 38.Young BA, Walker MJ, Strunce JB, Boyles RE, Whitman JM, Childs JD. Responsiveness of the Neck Disability Index in patients with mechanical neck disorders. Spine J. 2009;9(10):802–808. doi: 10.1016/j.spinee.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 39.Young IA, Cleland JA, Michener LA, Brown C. Reliability, construct validity, and responsiveness of the neck disability index, patient-specific functional scale, and numeric pain rating scale in patients with cervical radiculopathy. Am J Phys Med Rehabil. 2010;89(10):831–839. doi: 10.1097/PHM.0b013e3181ec98e6. [DOI] [PubMed] [Google Scholar]