Abstract
Purpose
Evaluate the accuracy of five different techniques for lower cervical pedicle screw placement.
Methods
Forty human cadaveric cervical spines were equally divided into five groups, and each group had eight specimens. Pedicle screws with dia. 3.5 mm were used. Group 1 was blind screw placement without any assistance; Group 2–5 was assisted by the X-ray fluoroscopy, virtual fluoroscopy navigation system, CT-based navigation system, and Iso-C 3D navigation system, respectively. Thereafter, cortical integrity of each pedicle was evaluated by anatomic dissection of the specimens.
Results
A total of 398 pedicle screws were inserted. In the Group 1–5, the average operation time per sample was 27 ± 3.0, 112 ± 10.3, 69 ± 6.4, 98 ± 11.0, and 91 ± 6.0 min, respectively. The outcome for excellent, fair and poor were 29 (36.3 %), 21 (26.2 %) and 30 (37.5 %) in Group 1; 35 (44.9 %), 29 (37.2 %) and 14 (17.9 %) in Group 2; 34 (42.5 %), 36 (45.0 %) and 10 (12.5 %) in Group 3; 70 (87.5 %), 10 (12.5 %) and 0 (0.0 %) in Group 4; 72 (90.0 %), 8 (10.0 %) and 0 (0.0 %) in Group 5.
Conclusions
Blind screw placement was surely unsafe. Lower cervical pedicle screw placement assisted by the CT-based navigation system or the Iso-C 3D navigation system significantly improved the accuracy compared to the fluoroscopy assistance and the virtual fluoroscopy navigation assistance.
Keywords: Navigation system, Computer-assisted operation system, Lower cervical spine, Pedicle screw placement
Introduction
Cervical pedicle screw placement is an advanced posterior fixation with great biomechanical benefit [1–3]. The clinical application of the cervical pedicle screw placement was limited because of a high cortical penetration rate (6.7–29 %) of a pedicle screw placement [4] and the high risk of vessel and nerve injury [5]. This was due to the anatomic variation of the cervical spine, the small size of the cervical pedicle and the low accuracy of the traditional assisted techniques. Therefore, improvement to the accuracy of the cervical pedicle screw placement is the key to reduce the complications and adverse effects [6]. The computer-assisted navigation system has been gradually applied into spine surgeries [7]. However, the natural value of the navigation system in the spinal surgical procedure was questioned [8]. Recent studies suggested that the accuracy of the pedicle screw placement in the lower thoracic and lumbar spine could be improved with a navigation system [9–11]. Compared to the traditional fluoroscopy, whether the navigation system could improve the accuracy in cervical pedicle screw placement remains debatable. Which kind of navigation system is desirable for the high-risk cervical procedure?
In the current study, we designed a random controlled study to assess the accuracy of pedicle screw placement in the lower cervical spine assisted by different navigation systems, i.e., the blind screw placement, the X-ray fluoroscopy screw placement, the virtual fluoroscopy navigation screw placement, the CT-based navigation screw placement, and the Iso-C 3D navigation screw placement. Our findings suggest that the CT-based navigation system and the Iso-C 3D navigation system have large advantages in assisting the lower cervical pedicle screw placement compared to the fluoroscopy assistance or the virtual fluoroscopy navigation assistance.
Materials and methods
Specimens
Forty adult spine cadavers including C1–T1 were fixed by formalin. The same amount of the posterior and bilateral soft tissues was reserved. CT scans through the section of pedicles were carried out for the measurement of the width, length and transverse angle to exclude those pedicles which were too narrow for screw placement. Two pedicles were excluded, in that those were too thin to insert the pedicle screw.
Study design
These specimens were randomly divided into five groups, and each group contained eight specimens. All procedures were performed by an experienced surgeon who had 12-year clinical experience in pedicle screw placement. The blind comparison and consequential statistical analysis were independently carried out by the other authors. The pedicles excluded were placed in the Group 2. Group 1 was blind screw placement without any assistance; Group 2–5 was assisted by the X-ray fluoroscopy, the virtual fluoroscopy navigation system, the CT-based navigation system, and the Iso-C 3D navigation system, respectively. Based on the data from the CT scan, the width and length in all the five groups were analyzed with an analysis of variance in completely randomized design and one-to-one q test, the result of which showed no significant difference among groups. It was believed that the five groups were comparable. The bilateral pedicles of C3–C7 were correspondingly analyzed by the paired t test, and no significant difference (p > 0.05) was observed. The data of the two pedicles of the same segment was therefore incorporated into one group for the statistic analysis.
All the pedicles of the C3–C7 were inserted with pedicle screws according to the surgical pathway of cervical pedicle screw placement except the right side pedicles of C4 and C5 in the Group 2, which were excluded. The screws were made of titanium with a diameter 3.5 mm. The length of pedicles was measured by CT scan: 80 % of the length from the entry point to the anterior cortical bone of the vertebral body. During the surgical procedure, the tentative manipulation and change of the pathways were forbidden to reflect the most true outcome of different methods of the cervical pedicle screw placement. The surgical time was the summation of the single cervical pedicle screw insertion time from C3 to C7 in one specimen. The navigation system was initiative infrared navigation system (Stryker®Spine Navigation).
Group 1: the distance between the entry point and the lateral border of the lateral mass and as well as the transverse angle was measured on the basis of the CT scan. The distance between the entry point and the inferior border of superior articular process and the sagittal angle was determined from the oblique view of plain films. The transverse angle and sagittal angle for the pedicle screw placement were ensured by a protractor, and the screws were inserted without any assistance from a navigation system.
Group 2: according to the preoperative measurement of CT scan and X-ray plain film, screw placement was conducted with X-ray fluoroscopy assistance during the operation. A C-arm A–P and lateral view of X-ray fluoroscopy were examined, respectively, at the start point, 10 mm inside and the final point.
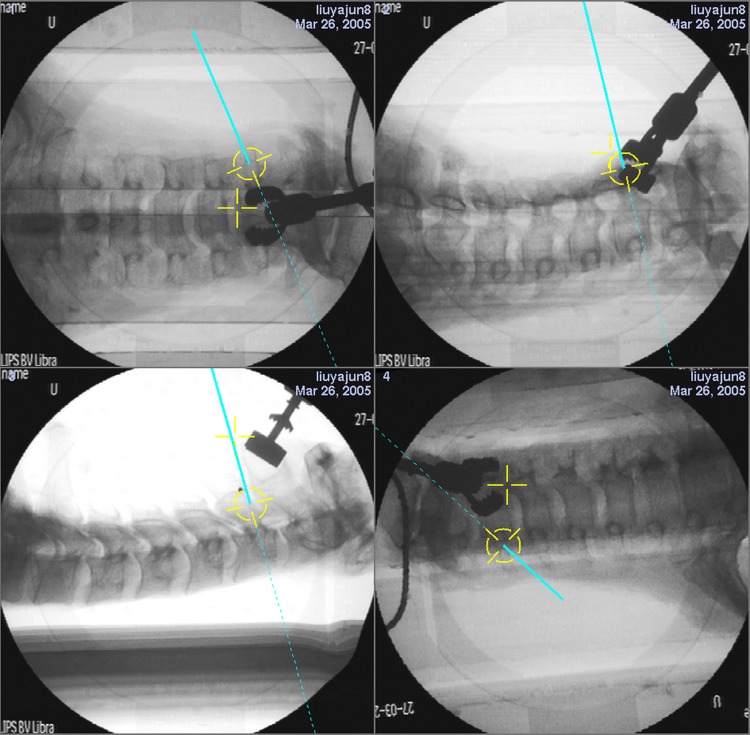
Group 3: the software for navigation system was Virtual Fluoroscopy V 1.0. The navigation system automatically registered after receiving the images of A–P view, lateral view and bi-oblique view from the C-arm. The pedicle screw placement was conducted by the 2D images. The placement point and sagittal angle were fixed with a pointer, and the transverse angle of placement was measured with a protractor. The screw hole was then drilled along the chosen trajectory (Fig. 1).
Fig. 1.
Virtual fluoroscopy navigation system assisted pedicle screw placement. The pedicle screw placement is inducted by the 2D images (A–P view, lateral view and bi-oblique view), with the pointer to determine the entry point, the sagittal angle and a protractor to determine the transverse angle
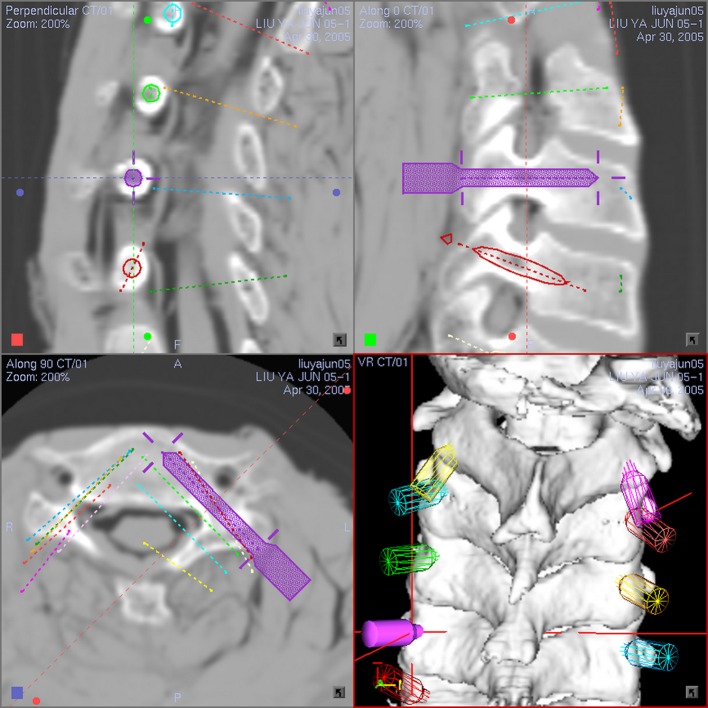
Group 4: the software for navigation system was CT-Based Spine Navigation 1.1. Preoperative CT scan (1 mm cuts) was obtained. The ideal axis and size for insertion of each pedicle screw were scheduled prior to the surgery at each level by defining the appropriate entry and target points on the 3D reconstructed images (Fig. 2). The surface registration of single vertebrae was adopted for registration in the CT-based navigation system. Once the point-to-point matching and surface matching process were completed, the navigation system measured the accuracy automatically. The next step would be taken if the error was reasonable (within 0.5 mm). Under the computerized 3D image guidance, the optional place point and direction were chosen with a pointer, the screw hole was then drilled along the chosen trajectory (Fig. 3).
Fig. 2.
Preoperative design of CT-based navigation system. The preoperative design of the left pedicle of C5 is taken as an example, the ideal entry point, sagittal angle, transverse angle and the appropriate length and diameter of the screw are illustrated
Fig. 3.
CT-based navigation system assisted cervical pedicle screw placement. According to the preoperative reconstructed 3D images, a pointer is used to determine the entry point and direction
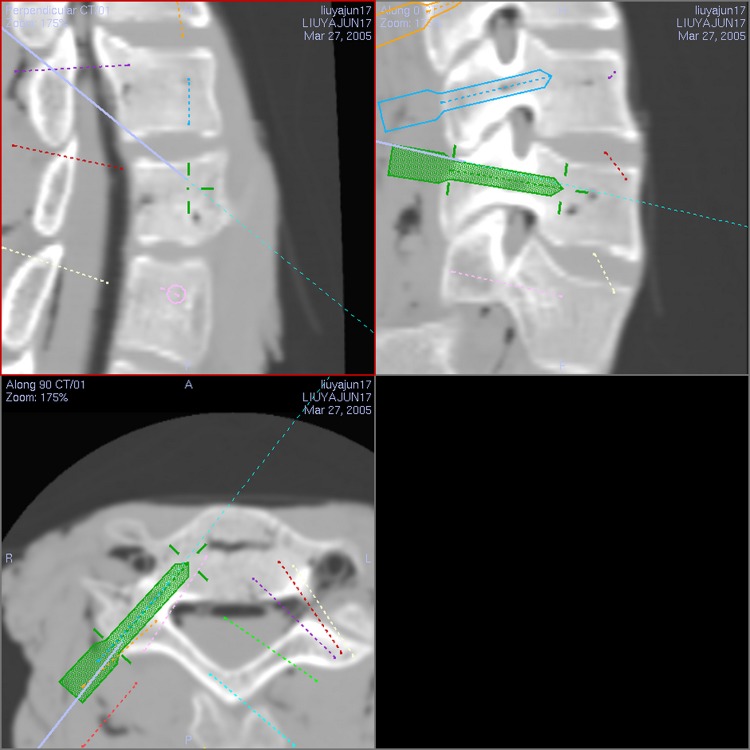
Group 5: the navigation system was CT-Based Spine Navigation 1.1. The navigation data were instantaneously taken from electric C-arm (SIREMOBIL Iso-C, Siemens, Germany) during the operation. The procedure of operation was basically similar to the Group 4, the only difference was the image collection method. The C-arm rotated 190° and collected 100 digital spot images, and then the reconstructed 3D images were uploaded into the navigation system. Simultaneously, the automatic registration of the navigation system was accomplished automatically. Transferred images could be used directly without the need of point-to-point matching or surface matching. Then the pedicle screw placement was inducted by the instantaneous reconstructed 3D images (Fig. 4).
Fig. 4.
Iso-C 3D navigation system assisted cervical pedicle screw placement. The pedicle screw placement is inducted by the instantaneous reconstructed 3D images
Statistical method
The row × column Chi-square test and row × column segmental analysis were used to analyze the accuracy among the groups (α = 0.05). Operation time was assessed with an analysis of variance in completely randomized design and with one-to-one q test (α = 0.05).
Results
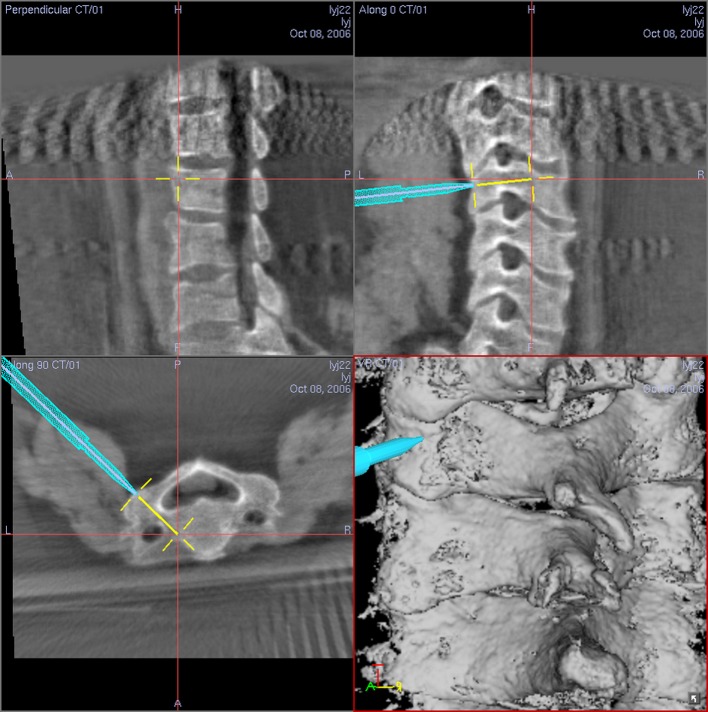
Evaluation of the results
The specimens were dissected according to the segment after the operation, and the accuracy of the pedicle screw placement was estimated by gross view (Fig. 5). The pedicles were divided into three categories: excellent (the screw was completely within the pedicle without penetration), fair (there was penetration in the isthmus by the screw thread and the penetration part was less than 1 mm), and poor (there was penetration in the isthmus by the screw and the penetration part was more than 1 mm). The latter one had a risk of injury to the vessels and nerve around. The excellent category and fair category could be considered together for the excellent/fair portion.
Fig. 5.
Evaluation of accuracy of the pedicle screw placement in gross view. a Excellent: the screw is totally in the pedicle without penetration. b Fair: there is penetration in the isthmus by the screw thread, and the penetrated part is no more than 1 mm. c Poor: there is penetration in the isthmus by the screw and the penetrated part is more than 1 mm
The ratio of the excellent/fair pedicle screw placement in the Group 4 (CT-based navigation) and Group 5 (Iso-C 3-dimensioned navigation) was both 100 %. No statistically significant difference was found in the overall rate of “excellent” and “fair” screws insertion between Groups 2 (fluoroscopy) and Group 3 (virtual fluoroscopy navigation). The overall rate of “excellent” and “fair” screw insertion in the Group 1 (blind placement) is the lowest among the five groups.
The operation time largely varied among the groups (Table 1). Overall, using a navigation system required more time in operation compared to the one without assistance.
Table 1.
The comparison of five techniques for C3–C7 pedicle screw placement
| Group | N | OTa (min) | Excellent | Fair | Poor | E/F portion |
|---|---|---|---|---|---|---|
| 1 | 80 | 27 ± 3.0 | 29 | 21 | 30 | 62.5 % (50/80) |
| 2 | 78 | 112 ± 10.3 | 35 | 29 | 14 | 82.1 % (64/78) |
| 3 | 80 | 69 ± 6.4 | 34 | 36 | 10 | 87.5 % (70/80) |
| 4 | 80 | 98 ± 11.0 | 70 | 10 | 0 | 100 % (80/80) |
| 5 | 80 | 91 ± 6.0 | 72 | 8 | 0 | 100 % (80/80) |
aOperation time per specimen
The accuracy of the blind cervical pedicle screw placement according to the images prior to operation was the lowest. Compared to the blind and the X-ray fluoroscopy-assisted groups, the accuracy of cervical pedicle screw placement in the computer assisted groups together was significantly improved (p < 0.05). However, in the virtual fluoroscopy navigation system assisted groups, the outcome was still poor, which could injure the vessels and nerves. Compared to the X-ray fluoroscopy assisted cervical screw placement, the virtual fluoroscopy assisted cervical screw placement required less time, without improvement to the accuracy. CT assisted cervical screw placement and Iso-C 3D assisted cervical screw placement fielded a high percentage of accuracy among the three computer assisted groups. These methods surely improved the safety of the operation.
Discussion
The computer assistance system currently used in the spine surgery was mainly the infrared optical navigation with high resolution and 3D orientation. Although it is free of being interrupted by other equipments in the operation, it has limitations, for example, a piece of optically sensitive equipment is required for the information exchange and direct sunlight is prevented. There are three modes for the spinal navigation systems, fluoroscopy-based navigation system, CT-based navigation system, and intraoperative 3D C-arm navigation system.
Fluoroscopy-based navigation system is 2D image navigation. Experimental studies showed that there was no significant difference in the accuracy between traditional X-ray fluoroscopy and fluoroscopy-based navigation, indicating that the accuracy of navigation system itself was acceptable and close to the accuracy of traditional fluoroscopy. Furthermore, it might reduce the operation time and the radiation injuries to patients, nurses, and surgeons [7, 12]. However, some limitations of fluoroscopy images should be taken into account, such as the requirement of clinical experience for the interpretation of the spinal images, and the difficulties to decide accurate angles and entry point in cervical pedicle screw placement. These could result in high risks during the procedure. Thus, the cervical pedicle screw placement assisted by fluoroscopy-based navigation system was inadvisable for clinical application.
CT-based navigation system and Iso-C 3D navigation system both use 3D technique, which could accurately direct the entry angle and depth of the screws. Three-dimensional navigation systems were suitable for cervical pedicle screw placement with a high risk.
CT-based navigation system could make surgical plan prior to operation by identifying the morphologic variation of the pedicle and confirming the type and the inserting orientation of the screws. As the data of the CT scan was taken before operation, change to the position of a patient could occur because the 3D images do not reflect the real anatomic location and consequently might mislead the surgeon. During the process of registration, the errors from the selection of the reference points and manipulation might increase the operation time and decrease the accuracy of the navigation system.
Iso-C 3D navigation system could obtain the instantaneous 3D reconstructed images and automatically upload into the navigation system to achieve the auto-registration and auto-combination. Iso-C 3D navigation system integrates largely the advantages of fluoroscopy and CT-based navigation system, and reduces the manipulation error. Although the 3D images, especially the reconstructed images, were not as exact as CT images, the sections of the 3D images were of no difference from the CT images and could satisfy the need in accuracy. Our previous studies demonstrated that the safety and accuracy of the upper cervical screw placement and lumbar vertebrae with axial rotation were also substantially improved [13, 14]. Additionally, we performed an analysis of 818 cases of navigation assisted spine operations from December 2002 to November 2009 in our department. From December 2002 to October 2005, the number of navigation assisted spine surgery was 130 cases (3.71 cases per month in average). After the application of intraoperative 3D C-arm navigation in November 2005, the cases of operation were increased to 688 by November 2009 (14.04 cases per month in average). Intraoperative 3D C-arm navigation has become the principal mode of navigation used in our department, accounting for 99.27 % by November 2009. The usage of virtual fluoroscopy navigation and CT-based navigation has dramatically declined in our department since then. These data together suggest that the Iso-C 3D navigation system greatly improves the safety and accuracy of the operation [15]. Iso-C 3D navigation system thus may represent a promising approach, and might replace the fluoroscopy-based navigation system and CT-based navigation system in spine surgery before long.
In our study, the cervical motion segments of formalin fixed cadaver were immobile and the bone density was reduced. As a result, the screw insertion in the cervical part of cadaver was easier than that in clinical practice, and the obtained accuracy might be higher than that in clinical practice. This suggests that the firm immobility of the cervical spine and adequate exposure of the surgical region were the key points for the accuracy when using a navigation system. In clinical practice, to avoid the disturbance of the soft tissue, we immobilize the cervical spine through Mayfield cranial traction, sufficient dissection of musculature and the use of muscular relaxant. During the insertion of pedicle screws, we performed carefully and saw to the shift of the adjacent vertebrae and the drift of the navigation images caused by the force of screw placement. The conditions mentioned above could be solved by appropriate standstill during manipulation to ensure the navigation system to direct the accurate direction.
Nonetheless, it may not be feasible to quantify the cost-effect, and predict clinical outcomes of these techniques based on the current cadaveric study. Moreover, it is also difficult to compare the accuracy of the experiments performed by different surgeons with various experiences in these techniques. Therefore, a large-scale randomized clinical study might warrant close investigation in the future.
Acknowledgments
This work was supported by a grant from the Beijing Nova Program (2007B023 to Yajun Liu), which is funded by Beijing municipal science and technology commission for science and technology talent cultivation plan.
Conflict of interest
None.
Footnotes
W. Tian and Y. Liu contributed equally to this work.
References
- 1.Barnes AH, Eguizabal JA, Acosta FL, Jr, Lotz JC, Buckley JM, Ames CP. Biomechanical pullout strength and stability of the cervical artificial pedicle screw. Spine (Phila Pa 1976) 2009;34(1):E16–E20. doi: 10.1097/BRS.0b013e3181891772. [DOI] [PubMed] [Google Scholar]
- 2.Dunlap BJ, Karaikovic EE, Park HS, Sokolowski MJ, Zhang LQ. Load sharing properties of cervical pedicle screw-rod constructs versus lateral mass screw-rod constructs. Eur Spine J. 2010;19(5):803–808. doi: 10.1007/s00586-010-1278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu R, Ebraheim NA, Skie M. Pedicle screw fixation in the cervical spine. Am J Orthop (Belle Mead NJ) 2008;37(8):403–408. [PubMed] [Google Scholar]
- 4.Miyamoto H, Uno K. Cervical pedicle screw insertion using a computed tomography cutout technique. J Neurosurg Spine. 2009;11(6):681–687. doi: 10.3171/2009.6.SPINE09352. [DOI] [PubMed] [Google Scholar]
- 5.Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine (Phila Pa 1976) 2000;25(8):962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 6.Yukawa Y, Kato F, Ito K, Horie Y, Hida T, Nakashima H, Machino M. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2009;18(9):1293–1299. doi: 10.1007/s00586-009-1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tjardes T, Shafizadeh S, Rixen D, Paffrath T, Bouillon B, Steinhausen ES, Baethis H. Image-guided spine surgery: state of the art and future directions. Eur Spine J. 2010;19(1):25–45. doi: 10.1007/s00586-009-1091-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verma R, Krishan S, Haendlmayer K, Mohsen A. Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5,992 pedicle screws. Eur Spine J. 2010;19(3):370–375. doi: 10.1007/s00586-009-1258-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Han W, Gao ZL, Wang JC, Li YP, Peng X, Rui J, Jun W (2010) Pedicle screw placement in the thoracic spine: a comparison study of computer-assisted navigation and conventional techniques. Orthopedics 33(8). doi:10.3928/01477447-20100625-14 [DOI] [PubMed]
- 10.Rajasekaran S, Vidyadhara S, Ramesh P, Shetty AP. Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa 1976) 2007;32(2):E56–E64. doi: 10.1097/01.brs.0000252094.64857.ab. [DOI] [PubMed] [Google Scholar]
- 11.Kosmopoulos V, Schizas C. Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 2007;32(3):E111–E120. doi: 10.1097/01.brs.0000254048.79024.8b. [DOI] [PubMed] [Google Scholar]
- 12.Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91(8):1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 13.Tian W, Weng C, Liu B, Li Q, Hu L, Li ZY, Liu YJ, Sun YZ. Posterior fixation and fusion of unstable Hangman’s fracture by using intraoperative three-dimensional fluoroscopy-based navigation. Eur Spine J. 2012;21(5):863–871. doi: 10.1007/s00586-011-2085-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tian W, Lang Z. Placement of pedicle screws using three-dimensional fluoroscopy-based navigation in lumbar vertebrae with axial rotation. Eur Spine J. 2010;19(11):1928–1935. doi: 10.1007/s00586-010-1564-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tian W, Liu YJ (2010) Intraoperative 3D C-arm and navigation opened a new era in spine surgery—analysis of 818 cases of navigation assisted spine surgery. In: The 7th annual meeting of CAOS-Asia, Thailand