Abstract
Background
Prospective evaluation of atlanto-occipital dissociations (AODs) at a level 1 trauma centre within 5 years.
Methods
Over a period of 5 years (2005–2009), all CT scans of the skull base and the upper cervical spine due to traumatic injuries were prospectively entered into a database. Furthermore, in cases of confirmed AOD all empirical data were prospectively collected. A more detailed data analysis of all AOD patients was conducted 2 years post-trauma. If required, another prospective follow-up was performed.
Results
2,616 CT scans were performed in total. Out of these, there were five male patients with confirmed AOD. Thus, the total incidence was 0.2 %. AOD was associated with occipital condyle fractures in three out of the five cases. Three out of five patients (60 %) died due to the severity of the injury. It was possible to stabilise two patients surgically with a clinical/radiological follow-up 2 years post-surgery. At that time, one patient had an incomplete tetraplegia and was wheelchair ridden without needing ventilation, while the other patient suffered from post-traumatic stress disorder, but was able to walk and live alone.
Conclusions
AOD is a rarely seen injury, even in a level 1 trauma centre, and is associated with high morbidity and mortality. However, it is possible for adults to survive this severe occipito-cervical injury after surgical repair while maintaining the ability to walk. All the results and recommendations are still based on a low level of evidence, due to the low incidence of this injury.
Keywords: Atlanto-occipital dissociation, Surgery, Outcome
Introduction
Atlanto-occipital dislocations (AODs) and dissociations are rarely detected injuries, even in a level 1 trauma centre, and they are associated with a high level of mortality even during the preclinical phase [1–3]. An accurate incidence of AOD was reported by Bucholz and Burkhead [3] who reported an 8 % incidence (9 out of 112 victims of multiple traumas) of AOD following motor vehicle fatalities. Moreover, AOD was the single most common injury of the cervical spine in victims of multiple traumas, and the incidence in children was significantly higher than that in the adults in this series.
Up to now, the clinical incidence of this traumatic injury has only been based on retrospective estimates, which were dependent on the inclusion criteria [4, 5]. Despite the availability of several, radiological and conventional evaluation procedures for the detection of AOD [6–12], it still remains unclear as to whether the injury per se or the severity of comorbid trauma leads to death.
Only 48 publications with 79 retrospective patients were found in a literature research covering the period between 1966 and 2001 [13], and a literature search by Gregg et al. [14] identified only 135 cases of survived AOD. Moreover, the authors of this study found in the literature (Medline search) only six publications within the last 10 years including at least five patients with AOD (Table 1).
Table 1.
Original publications including at least five patients with AOD
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|
| 2011 | Chaput | 14 | ? | 8 | None | No patient survived with BDI >16 mm |
| 2010 | Cooper | 22 | ? | 7 | Study also included C1–C2 dislocation | 80 % of non-survivors had BDI of >16 mm; all non-survivors had GCS 3 |
| 2008 | Ben-Galim | 6 | – | 6 | Measurements e.g. BDI failed study included only survivors | Survival is rare but possible |
| 2007 | Horn | 33 | 16 | 22 | Measurements e.g. BDI failed | 9/17 adults, but only 1/16 children died children showed higher survival rate |
| 2006 | Bellabarba | 17 | ? | 17 | Study also included C1–C2 dislocation; study included only survivors; 17 cases within 8 years period by 3 centres | Even patients with severe neurological deficits may experience significant functional improvement |
| 2005 | Hosalkar | 16 | 16 | 5 | None | Single largest series of AOD in children-prompt treatment can result in increased survival |
1 year of publication, 2 authors name, 3 number of total cases, 4 number of children <18 years within the total cases, 5 total number of survivors, 6 study limitations, 7 outcome
The small number of cases explains the different treatment recommendations without any evidence, ranging from conservative therapy (distraction only) with neck support and Halo fixator to different cranio-cervical decompression and fusion methods [11, 14–20].
As a result, we conducted a prospective study, for which we included all cases of occipito-cervical injuries (C0–C1) in our hospital between 01/01/2005 to 12/31/2009 and performed a 2-year post-injury radiological and clinical follow-up, if needed.
With this study, we would like to describe our experiences with five AOD patients in detail for the first time after 5 years of prospective follow-up.
Materials and methods
In our level 1 trauma centre (University Hospital Regensburg), a total of 2,616 CT scans (cranial and/or cervical CT, including multiple trauma CT) were made that included the base of the skull and the upper cervical spine during a prospective study between 01/01/2005 and 12/31/2009 (cut-off date). The indication with all of these cases was the detection or exclusion of a cerebral and/or cervical injury following trauma, according to the Advanced Trauma Life Support (ATLS) general treatment guidelines. In all cases, the scans were performed in layers of at least 1–2 mm between C0 and C2 including axial, sagittal, and coronal reconstruction of the condyle region (Siemens, Somatom Sensation-16, Germany). All CT scans were documented prospectively.
The six following radiological parameters were used for the exclusion/confirmation of AOD, whereby the radiographic methods were used either in isolation or in combination to evaluate AOD.
Type of dislocation
According to Traynelis et al. [21], the AOD was classified into three types based on the direction of dislocation: type 1, anterior; type 2, longitudinal; and type 3, posterior. Lateral, rotational, and multi-directional dislocations that could not be classified into one of these three types were considered separately and noted as “other type”.
Basion Dens Index (BDI)
According to Wholey et al. [10], a displacement of more than 10 mm between the basion and the tip of the odontoid was considered abnormal.
Basion Atlas Index (BAI)
According to Harris et al. [6, 7], a displacement of more than 12 mm or less than −4 mm between the basion and the posterior C2 line, or a displacement of more than 12 mm from the basion to dens was considered abnormal.
X-line
According to Lee et al. [8], the X-line method is considered abnormal if the line from the basion to the axis spinolaminar junction do not intersect C2 and if a line from the opisthion to the postero-inferior corner of the body of the axis does not intersect C1.
BC/OA powers ratio
According to Powers et al. [9], the ratio of the basion and posterior atlas arch distance (BC) divided by the opisthion and anterior atlas arch (OA) distance equal to or greater than one was considered abnormal.
Pang rule (22)
According to Pang et al. [22], four measurement points are set for each of the major joint dislocations in selected sagittal and coronal CT scans, in order to measure the immediate distance between occipital condyle and C1. The average of these eight measurements represents an interval (condyle-C1 interval [CCI]). A CCI value of 4 mm or more is considered as a confirmed AOD.
If an AOD was detected (interdisciplinary by radiology and trauma surgery), empirical data and the further clinical course of the patient, including injury pattern, were recorded in an additional database as follows: sex, age, cause of accident, comorbid trauma, initial Glasgow Coma Scale (GCS) rating, and Injury Severity Score (ISS).
Generally, confirmation of AOD was an indication for occipito-cervical stabilisation using an internal fixator and spondylodesis, irrespective of the severity of the comorbid trauma. Stabilisation of the cervical spine was performed up to the vicinity of C2/3, with the screws being inserted bilaterally using the “lateral mass screw” method. Several screws were bilaterally positioned in the occipital region.
Two years post-trauma, the lead author and another co-author performed a prospective follow-up, for which patients were contacted by telephone or in writing for an outpatient visit. Clinical follow-up and another CT scan of the condyle region (C0–C2) in 1–2 mm layers and reconstructions were conducted on this occasion, and the images were compared with those taken at the time of the trauma.
Results
A total of five male patients with AOD were identified out of 2,616 CT scans conducted. The mean age was 37.8 years (range 15–52), including one child (patient #5). Thus, the incidence of AOD in our population was 0.2 %. During the same time, 31 patients were diagnosed with occipital condyle fractures (OCFs) resulting in a clearly higher incidence of 1.19 % [23].
Three out of five patients had a combined trauma (AOD and OCF), and the incidence of such injuries in our study population was 3 out of 2,616 patients, i.e. 0.11 %.
Four patients sustained high-energy injuries in a motor vehicle accident, and one patient fell from a tree, and the average injury severity score (ISS) was 44.4 points. All five patients (100 %) with AOD were primarily diagnosed, and a Halo fixator was initially used for treatment in four out of five cases. Only one patient (patient #2) was primarily treated by means of occipito-cervical stabilisation using an internal fixator. On day 11 and 3 (post-trauma), respectively, the Halo fixator of patient #1 and #3 was removed and secondary occipito-cervical stabilisation was conducted. In one case (#1), postoperative CT scan documented unilateral C2 pedicle screw misplacement into the vertebral artery foramen (Fig. 1c), but without neurological deterioration. Therefore we performed no revision. After surgical treatment, patients received a soft collar for 6 weeks, no one received Halo vest again. Three out of five patients (60 %) died on day 2, 7 and 11, respectively, post-trauma due to the severity of their secondary traumatic brain injuries. Additional empirical data of the five patients can be found in Table 2. These data show clearly better radiological parameters (BDI, BAI, powers ratio, and pang rule) for both of the surviving adult patients (patient #1 and #2) compared to the two adult deceased patients (patient #3 and #4). The X-line was pathologic in all five cases, including the child (patient #5). Furthermore, the initial GCS showed clearly lower scores for all three died patients.
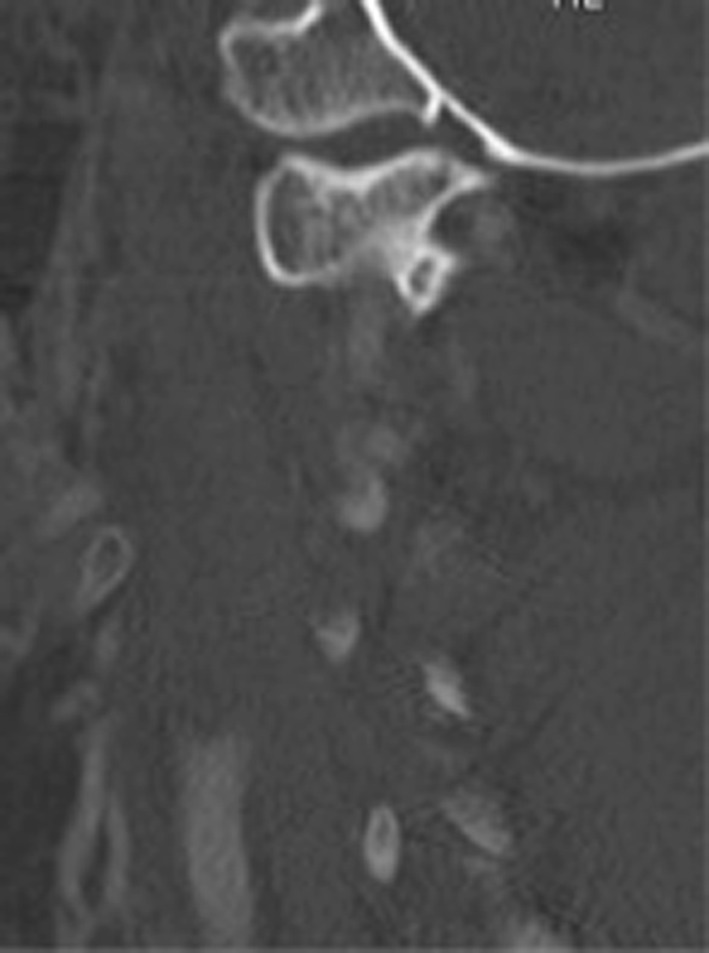
Fig. 1.
a Sagittal CT image: Pat. #1, AOD with anterior dislocation. b Sagittal CT image: Pat. #1, AOD with BDI measurement of 11 mm. c Sagittal CT image: Pat. #1, 1 year after occipito-cervical internal fixator from C0 to C2/3. CT scan documented asymptomatic unilateral misplacement of pedicle screw into the vertebral artery foramen
Table 2.
Data due to our study patients with AOD
| Patient # | GCS | ISS | Dislocation (18) | BDI (10) (mm) | BAI (6, 7) (mm) | X-line (8) | Powers (9) | Pang rule (22) (mm) | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 15 | 50 | Anterior | 11 | 11 | Abnormal | 0,89 | 11 | Nearly normal |
| 2 | 10 | 38 | Anterior | 15 | 13 | Abnormal | 1,18 | 8 | Tetraplegia |
| 3 | 3 | 42 | Anterior | 17 | 19 | Abnormal | 1,64 | 14 | Died |
| 4 | 3 | 42 | Anterior/longitudinal | 25 | 19 | Abnormal | 1,39 | 22 | Died |
| 5 (child) | 3 | 50 | Longitudinal | 13 | 7 | Abnormal | 0,84 | 6 | Died |
At the time of follow-up (2 years post-surgery), two patients were alive:
One patient (#1) (Fig. 1a, b, c) was unfit for work, but still able to walk and live alone. Due to the patient’s young age, the occipito-cervical implant was removed 22 months post-surgery. There were no radiological or clinical signs of instability following this procedure, but the mobility of the cervical spine was considerably improved.
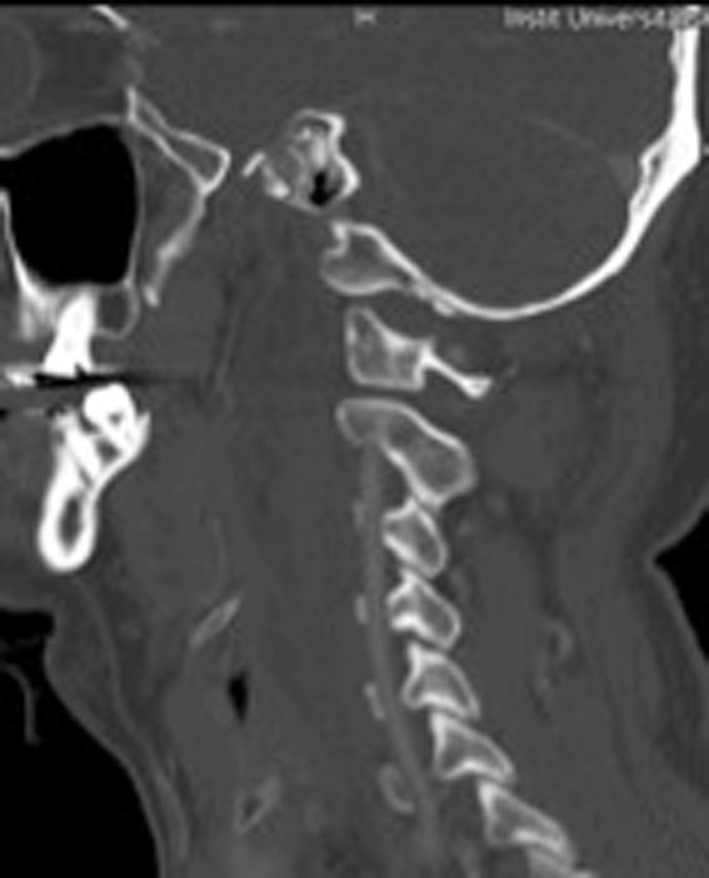
The other patient (#2) (Fig. 2) had an incomplete tetraplegia and was wheelchair-ridden and dependent on care without needing ventilation, while imaging showed an appropriate in situ position of the internal fixator following primary wound healing.
Fig. 2.
Sagittal CT image: Pat. #2, AOD with anterior dislocation; patient alive with tetraplegia
Discussion
Up to now, the small amount of information with regard to AOD incidence has been solely based on retrospectively or prospectively created databases, without any objective proof of possible inclusion or exclusion criteria [4, 5].
Furthermore, the methods used for the diagnosis of AOD have not been specified, even in current studies [15, 16]. With our prospectively designed study in a level 1 trauma centre (for the first time in the literature), all CT scans performed during a 5-year period—including cranial, cervical, and polytrauma CT scans—were primarily analysed and recorded with regard to existing AOD and occipital condyle fractures. The performance and indication, respectively, for CT were based on ATLS guidelines and criteria, and an adequate accident event was part of each case.
Out of 2,616 CT scans that were conducted over a period of 5 years, there were only five AOD cases, which were all primarily and consistently diagnosed by radiologists and/or trauma surgeons. Thus, the AOD detection rate and incidence, respectively, in our study were as low as 0.19 % i.e. 1–2 patients per 1,000 CT scans or a maximum of one patient per year. Chaput et al. [4] performed a retrospective analysis of a trauma database with a total of 1,174 patients over a 5-year period between 2005 and 2009 and identified a total of 14 AOD patients, resulting in an incidence of 1.19 %, which was clearly higher when compared to our study. However, empirical patient data have not been specified in this publication. One reason for the difference in incidence rates may be based on the fact that only few paediatric polytrauma patients were treated in our hospitals at the time of the study, while AOD is commonly found in paediatric trauma patients due to the smaller and horizontally aligned condyles: According to a Medline literature search by Gregg et al. [14], 135 case reports of AOD survivors were identified, including 80 children and 55 adults.
Surprisingly, AOD diagnosis was associated with occipital condyle fractures in three out of five patients (60 %) in our study. Up to now, these combined injuries have been documented and published only by Ahuja et al. (three out of six patients; 50 %) [19].
Mortality in our study was 60 % (3 out of 5 patients), which is in line with results from other studies [4, 5]. For the three deceased patients including the child, an initial GCS of 3 points was shown, and the two adult patients needed temporary resuscitation at the accident site. This is consistent with the data published by Cooper et al. [5], who performed a retrospective analysis of hospital and autopsy patients: as in our study, there were no surviving AOD patients, with an initial GCS of 3 or who had been resuscitated. However, one case report described complete neurological recovery of a 31-year-old man with AOD who had an initial GCS of 3 [14].
A variety of radiographic measurements have been proposed for the diagnosis of AOD on a lateral cervical radiograph: According to Wholey et al. [10], a radiological displacement of more than 10 mm between the basion and dens (BDI) is considered abnormal. Moreover, and according to Dziurzynski et al. [25] the sensitivity for BDI is 100 % in CT scans, when the BDI is more than 10 mm. All five of our AOD patients including the child showed measurements of more than 10 mm.
A recent study [4] with 14 AOD patients in 2011 demonstrated 100 % mortality for cases with BDI measurements of more than 16 mm (4 out of 10 patients). In another recent study, 80 % of the deceased had BDI measurements of more than 16 mm [5]. Likewise, two of our three deceased patients showed measurements of 17 and 25 mm, compared to 11 and 15 mm, respectively, with the surviving patients. The only child in our study (age 15 years) showed BDI measurement of 13 mm, and died due to severe head injury. Therefore, a BDI value of 16 mm may in fact represent a limit in adult patients. On the other hand, and in accordance with Bellabarba et al. [26], the classification by Traynelis et al. [21] has had no clinical relevance for our treatment. Moreover, the instability allows all three categories to be present in one single patient [17].
Due to Powers et al. [9], a ratio of the basion-posterior atlas arch distance divided by the opisthion-anterior atlas arch distance greater than 1.0 is considered abnormal. This ratio has high predictive value. On the other hand, some authors [6–8, 24] found a lower sensitivity of the Power’s ratio. We have also seen confirmed AOD, although the Power’s ratio was clearly lower than 1.0 (Fig. 1a, b). On the other hand, clearly higher pathological measurements have been shown for both of the deceased adult patients (#3 and #4) (Figs. 3, 4) compared to the two adult surviving patients. Therefore, we can confirm that using only one imaging method may be insufficient for the reliable detection or exclusion of AOD [17]. Moreover, almost all the accepted measurements [6–12] have so far been based on conventional X-ray imaging with low case numbers, rather than on CT, which has become the “gold standard” for the detection/exclusion of AOD in the meantime.
Fig. 3.
Sagittal CT image: Pat. #3, patient died due to AOD on the 11th day post-trauma
Fig. 4.

Sagittal CT image: Pat. #4, patient died due to AOD on the seventh day post-trauma
Up to now, the only study based on CT scans in AOD patients was exclusively conducted in a paediatric population [22]. Therefore, it is difficult to apply these results to adult patients. However, we also used this measurement method for our study, although we had four adult patients in our study population, because these are the only valid measurements—collected with and without AOD detection—based on CT imaging [22]. The CCI index (Table 2) was clearly pathological for all of the five patients in our study, and the measurements exclusively showed bilateral dissociations.
If only native imaging is used for diagnosis, even severe AODs are overlooked [26]. Furthermore, it must be emphasised that imaging only provides a static momentary picture of the lying patient; however, the damage represents an extreme level of functional instability. Therefore, it must be considered, whether new measurement methods based on CT or even MRI should be evaluated in larger patient populations (including adults) in the future. However, MRI still does not play a vital role in the primary diagnostics of crash victims and polytrauma patients. And we cannot see a general indication for performing MRI imaging, when CT scans have shown consistently normal radiological measurements (BDI, BAI, Powers ratio and X-line). The classification suggested by Horn et al. [17], for applying an external orthesis in cases of only moderately abnormal signs in posterior ligaments or occipito-atlantal joints in MRI imaging (grade 1 injury), seems exaggerated in adult patients. We consider a cervical collar to be sufficient. However, it must be emphasised that the results and findings published by Horn et al. [17] are partially based on injuries in a paediatric population; approximately 50 % of the patients were aged 18 years or younger.
In recent studies, the therapeutic approach favours dorsal stabilisation and spondylodesis to avoid secondary neurological damage [17, 19, 26]. For this, different implants and methods have been described [18].
In our facility, three out of five patients received bilateral occipito-cervical stabilisation using an internal fixator; two patients with unstable circulatory conditions were treated using a Halo fixator. Additional decompression via laminectomy was not performed in any of our cases, and there are differences in the literature with regard to the procedure and the evaluation of this method [26].
Based on the available data, therefore, it remains unclear as to whether indeed all AOD patients benefit from and require, respectively, sophisticated dorsal occipito-cervical stabilisation, or if temporary external stabilisation alone using a Halo fixator may be sufficient for some of these patients, i.e. a subgroup [19]. However, this would require larger patient population, in order to allow for the identification of procedural measurement limits.
There is no doubt that patients with confirmed AOD must receive immediate treatment in order to prevent secondary neurological damage, which may become manifest if AOD is detected secondarily after a certain period of time [19, 26].
Conclusions
AOD is a rarely seen injury, even in a level 1 trauma centre, and is associated with high morbidity and mortality. Rapid diagnosis by means of CT scans as a so-called “gold standard”, and treatment initiation using immediate occipito-cervical stabilisation (if possible) or temporary application of a Halo fixator are crucial, because it is possible for adults to survive this severe injury after surgical repair while maintaining the ability to walk. All results and recommendations are still based on a low level of evidence, due to the scarcity of this injury.
Conflict of interest
None.
References
- 1.Adams VI. Neck injuries: I. Occipitoatlantal dislocation—a pathologic study of twelve traffic fatalities. J Forensic Sci. 1992;37:556–564. [PubMed] [Google Scholar]
- 2.Alker GJ, Jr, OH YS, Leslie EV. High cervical spine and craniocervical junction injuries in fatal traffic accidents: a radiological study. Orthop Clin North Am. 1978;9:1003–1010. [PubMed] [Google Scholar]
- 3.Bucholz RW, Burkhead WZ. The pathological anatomy of fatal atlanto-occipital dislocations. J Bone Surg Am. 1979;61:248–250. [PubMed] [Google Scholar]
- 4.Chaput CD, Torres E, Davis M, Song J, Rahm M. Survival of atlanto-occipital dissociation correlates with atlanto-occipital distraction, injury severity score, and neurologic status. J Trauma. 2011;71:393–395. doi: 10.1097/TA.0b013e3181eb6a31. [DOI] [PubMed] [Google Scholar]
- 5.Cooper Z, Gross JA, Lacey JM, Traven N, Mirza SK, Arbabi S. Identifying survivors with traumatic craniocervical dislocation: a retrospective study. J Surg Res. 2010;160:3–8. doi: 10.1016/j.jss.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 6.Harris JH, Jr, Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. Am J Roentgenol. 1994;162:881–886. doi: 10.2214/ajr.162.4.8141012. [DOI] [PubMed] [Google Scholar]
- 7.Harris JH, Jr, Carson GC, Wagner LK, Kerr N. Radiologic diagnosis of traumatic occipitovertebral dissociation: 2. Comparison of three methods of detecting occipitovertebral relationships on lateral radiographs of supine subjects. Am J Roentgenol. 1994;162:887–892. doi: 10.2214/ajr.162.4.8141013. [DOI] [PubMed] [Google Scholar]
- 8.Lee C, Woodring JH, Goldstein SJ, Daniel TL, Young AB, Tibbs PA. Evaluation of traumatic atlantooccipital dislocations. Am J Neuroradiol. 1987;8:19–26. [PMC free article] [PubMed] [Google Scholar]
- 9.Powers B, Miller MD, Kramer RS, Martinez S, Gehweiler JA., Jr Traumatic anterior atlanto-occipital dislocation. Neurosurgery. 1979;4:12–17. doi: 10.1227/00006123-197901000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Wholey MH, Bruwer AJ, Baker HL., Jr The lateral roentgenogram of the neck; with comments on the atlanto-odontoid-basion relationship. Radiology. 1958;71:350–356. doi: 10.1148/71.3.350. [DOI] [PubMed] [Google Scholar]
- 11.Dublin AB, Marks WM, Weinstock D, Newton TH. Traumatic dislocation of the atlanto-occipital articulation (AOA) with short-term survival. With a radiographic method of measuring the AOA. J Neurosurg. 1980;52:541–546. doi: 10.3171/jns.1980.52.4.0541. [DOI] [PubMed] [Google Scholar]
- 12.Kaufman RA, Dunbar JS, Botsford JA, McLaurin RL. Traumatic longitudinal atlanto-occipital distraction injuries in children. Am J Neurorad. 1982;3:415–419. [PMC free article] [PubMed] [Google Scholar]
- 13.Hadley MN. Diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery. 2002;50(Suppl):105–113. doi: 10.1097/00006123-200203001-00018. [DOI] [PubMed] [Google Scholar]
- 14.Gregg S, Kortbeek JB, Du Plessis S. Atlanto-occipital dislocation: a case study of survival with partial recovery and review of the literature. J Trauma. 2005;58:168–171. doi: 10.1097/01.TA.0000151184.08273.82. [DOI] [PubMed] [Google Scholar]
- 15.Chattar-Cora D, Valenziano CP. Atlanto-occipital dislocation: a report of three patients and a review. J Orthop Trauma. 2000;14:370–375. doi: 10.1097/00005131-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Govender S, Vlok GJ, Fisher-Jeffes N, Du Preez CP. Traumatic dislocation of the atlanto-occipital joint. J Bone Joint Surg Br. 2003;85:875–878. [PubMed] [Google Scholar]
- 17.Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N. Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine. 2007;6:113–120. doi: 10.3171/spi.2007.6.2.113. [DOI] [PubMed] [Google Scholar]
- 18.Vaccaro AR, Lim MR, Lee JY. Indications for surgery and stabilization techniques of the occipito-cervical junction. Injury. 2005;36(Suppl 2):44–53. doi: 10.1016/j.injury.2005.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Ahuja A, Glasauer FE, Alker GJ, Jr, Klein DM. Radiology in survivors of traumatic atlanto-occipital dislocation. Surg Neurol. 1994;41:112–118. doi: 10.1016/0090-3019(94)90107-4. [DOI] [PubMed] [Google Scholar]
- 20.Mouchaty H, Perrini P, Conti R, Di Lorenzo N. Craniovertebral junction lesions: our experience with the transoral surgical approach. Eur Spine J. 2009;18(Suppl 1):13–19. doi: 10.1007/s00586-009-0988-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Traynelis VC, Marano GD, Dunker RO, Kaufman HH. Traumatic atlanto-occipital dislocation. Case report. J Neurosurg. 1986;65:863–870. doi: 10.3171/jns.1986.65.6.0863. [DOI] [PubMed] [Google Scholar]
- 22.Pang CP, Wilberger JE. Traumatic atlanto-occipital dislocation with survival: case report and review. Neurosurgery. 1980;7:503–508. doi: 10.1227/00006123-198011000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Mueller FJ, Fuechtmeier B, Kinner B, Rosskopf M, Neumann C, Nerlich M, Englert C. Occipital condyle fractures. Prospective follow-up of 31 cases within 5 years at a level 1 trauma centre. Eur Spine J. 2012;21:289–294. doi: 10.1007/s00586-011-1963-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ben-Galim PJ, Sibai TA, Hipp JA, Heggeness MH, Reitman CA. Internal decapitation: survival after head to neck dissociation injuries. Spine. 2008;33:1744–1749. doi: 10.1097/BRS.0b013e31817bb0e0. [DOI] [PubMed] [Google Scholar]
- 25.Dziurzynski K, Anderson PA, Bean DB, Choi J, Leverson GE, Marin RL, Resnick DK. A blinded assessment of radiographic criteria for atlanto-occipital dislocation. Spine. 2005;30:1427–1432. doi: 10.1097/01.brs.0000166524.88394.b3. [DOI] [PubMed] [Google Scholar]
- 26.Bellabarba C, Mirza SK, West AG, Mann FA, Dailey AT, Newell DW, Chapman JR. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine. 2006;4:429–440. doi: 10.3171/spi.2006.4.6.429. [DOI] [PubMed] [Google Scholar]



