Abstract
Background
Sirtuin 1 (SIRT1) and deleted in breast cancer 1 (DBC1) are known as tumor suppressor or promoter genes. This may be due to their diverse functions and interaction with other proteins. Gastric adenocarcinoma is one of the most common malignancies, but little is known about its carcinogenesis. Therefore, we investigated the association of immunohistochemical expression of SIRT1, DBC1, p53, and β-catenin and their variable clinicopathological characteristics.
Methods
We obtained samples from 452 patients who underwent gastrectomy. Tissue microarray blocks were constructed and immonohistochemical staining was performed.
Results
Expression of DBC1 and SIRT1 was associated with lower histologic grade, intestinal type of Lauren classification, and lower pT (p<0.001) and pN stage (DBC1, p=0.002; SIRT1, p<0.001). Association between absence of lymphatic invasion, and SIRT1 (p=0.001) and DBC1 (p=0.004) was observed. Cytoplasmic β-catenin expression was associated with lower histologic grade, pT, pN, tumor-node-metastasis (TNM) stage, DBC1 (p<0.001), and SIRT1 (p=0.001). Expression of SIRT1 and DBC1 was not associated with p53 (p=0.063 and p=0.060). DBC1 was an independent good prognostic factor in multivariate analysis (p=0.012).
Conclusions
SIRC1 and DBC1 can be considered to be good prognostic factors in gastric adenocarcinoma.
Keywords: Stomach; Adenocarcinoma; DBC1 protein, human; SIRT1 protein, human
The class III histone deacetylase sirtuin (silent mating type information regulation 2 homolog) 1 (SIRT1) is a mammalian homologue of the Saccharomyces cerevisiae chromatin-silencing factor Sir2 that has emerged as an important regulator of aging.1 SIRT1 deacetylates diverse substrates including p53, peroxisome proliferator-activated receptor-γ co-activator-1α, forkhead transcription factor, nuclear factor κB (NF-κB), Ku70, MyoD1, histone, and β-catenin.2,3 Some studies have found that SIRT1 promotes cell survival by deacetylating p53 and attenuates p53 function downstream of the target gene. In addition, overexpression of SIRT1 is reported to be essential for cell growth and the survival of cancer cells.4 Up-regulation of SIRT1 is also reported in mouse malignant tumors and various human malignancies including prostate cancer, breast cancer, lymphoma, colon cancer, and gastric cancer.4-8 It has been suggested that the role of SIRT1 in carcinogenesis is accomplished by inactivation of tumor suppressor p53 protein which allows tumor cells to evade apoptosis.9 In human gastric cancer, the association between overexpression of SIRT1 and poor patient survival has been reported,10,11 but the exact mechanism for this connection has not be elucidated.
β-Catenin, a key regulator of Wnt signaling is also known to be an important regulator in cancer development. β-Catenin can play diverse roles in cadherin-mediated cell-cell adhesion, Wnt signaling transduction, and carcinogenesis.12 The relationships between intracellular localization of β-catenin and its role in carcinogenesis have been investigated in several studies.13 One study reported that SIRT1 promotes cytoplasmic localization of β-catenin in colon cancer.3 Another study reported a relationship between the cytoplasmic expression of β-catenin and lymph node metastasis, depth of invasion, and tumor location in gastric adenocarcinoma.12 The diverse functions of β-catenin in carcinogenesis are thought to be associated with its intracellular location. SIRT1 may be an important regulator of β-catenin in tumorigenesis, which could mediate the role of β-catenin by deacetylation.
Deleted in breast cancer 1 (DBC1) was first identified during the search for candidate tumor-suppressor genes that are homozygously deleted in human breast cancer.14 DBC1 directly binds to the catalytic domain of SIRT1 and inhibits deacetylase activity of SIRT1, then enhances p53 hyperacetylation, thereby increasing apoptosis.2,15 In another study, DBC1 was reported to stabilize estrogen receptors and to act as a co-activator of androgen receptor (AR); this means that DBC1 could act as a tumor promoter.16,17 In gastric adenocarcinoma, one study reported that expression of DBC1 was significantly associated with poor clinicopathologic variables such as high clinical stage (stage III and IV), lymph node metastasis, and shorter survival of patients.11
Gastric adenocarcinoma is one of the most common malignancies in the world, particularly in Korea.
Chemotherapy regimens including 5-fluorouracil, anthracyclines, and cisplatin are known to significantly improve survival in comparison to the best supportive care in advanced gastric adenocarcinoma.18 Gastric adenocarcinoma is a biologically and genetically heterogeneous cancer involving numerous genetic mutations and epigenetic alterations. Some other molecular alterations are known to occur during gastric carcinogenesis; among them, mutations of p53 are known to be involved in early gastric carcinogenesis.19 β-Catenin, an important regulator of the Wnt signaling pathway, is also known to play an important role in cancer development and the mutation of β-catenin is known as an early event in multistep carcinogenesis. Expression of cytoplasmic β-catenin can occur by mutations in APC, AXIN1, or CTNNB1. It is known that some gastric carcinomas have either CTNNB1 or APC mutations with expression of cytoplasmic β-catenin.19 Discovery of a more relevant molecular target or molecular marker is needed. Therefore, we investigated the expression and prognostic impact of SIRT1 and DBC1, emerging molecules involved in a variety of cancers, in gastric adenocarcinomas and their relationship with p53 and β-catenin. Also, many related clinicopathologic variables that have an effect on patient prognosis were investigated together.
MATERIALS AND METHODS
Patients and samples
Archived formalin-fixed paraffin-embedded (FFPE) samples of gastric adenocarcinomas were obtained from 452 patients who underwent radical gastrectomy at Korea University Guro Hospital from January 2002 to December 2005. No patient had a prior history of neo-adjuvant chemotherapy.
Clinicopathologic data, including age, sex, and distant metastasis were obtained from medical records. Survival data was obtained from records of the Ministry of Public Administration and Security as well as from medical records. All slide glasses and specimen photos were reviewed and the histopathologic type, histologic grade, Lauren classification, depth of invasion, regional lymph node metastasis, and lymphatic invasion were evaluated. The reviewed cases were reclassified according to the Seventh American Joint Committee on Cancer/International Union Against Cancer Classification (AJCC/UICC) tumor-node-metastasis (TNM) cancer classification system.20 The World Health Organization classification system, which describes three main histological grades, including well, moderately, and poorly differentiated, was applied for histological typing and grading of adenocarcinoma.21 The mean follow-up period was 50.9 months (median, 53.3 months; range, 3 to 83 months). The median age was 60.5 years (range, 23 to 84 years) and the male to female ratio was 2.1. Forty percent (n=183) of patients were diagnosed with early gastric carcinoma and 59.5 percent (n=269) with advanced gastric carcinoma. This study was approved by the Institutional Review Board of Korea University Guro Hospital (KUGGR-2010-033).
Tissue microarray (TMA) and immunohistochemical staining
Hematoxylin and eosin-stained slide glasses of selected patients were reviewed. Representative portions from the leading edge of tumor infiltration were marked and used for tissue microarray construction. Tumor tissues of 2.0 mm core diameter were taken from donor FFPE blocks and arranged in empty recipient paraffin blocks to generate a TMA. One core per tumor was arrayed. The TMA blocks were cut into 4 µm slices for immunohistochemical staining. A standard streptavidin-biotin peroxidase complex method was used. After deparaffinization and rehydration, slides were heated in a microwave oven for 15 minutes in 10 mM citrate buffer (pH 6.0) and treated with 3% hydrogen peroxide for 20 minutes. We used the Bond-maX autostainer (Leica, Wetzlar, Germany). Antibodies used in this study were DBC1 (1:200, polyclonal, Abcam, Cambridge, MA, USA), SIRT1 (1:200, clone H-300, Santa Cruz Biotechnology, Santa Cruz, CA, USA), β-catenin (1:500, clone β-catenin-1, Dako, Carpinteria, CA, USA), and p53 (1:500, clone DO-7, Novocastra, Newcastle upon Tyne, England).
Analysis of immunohistochemical staining by optical microscope
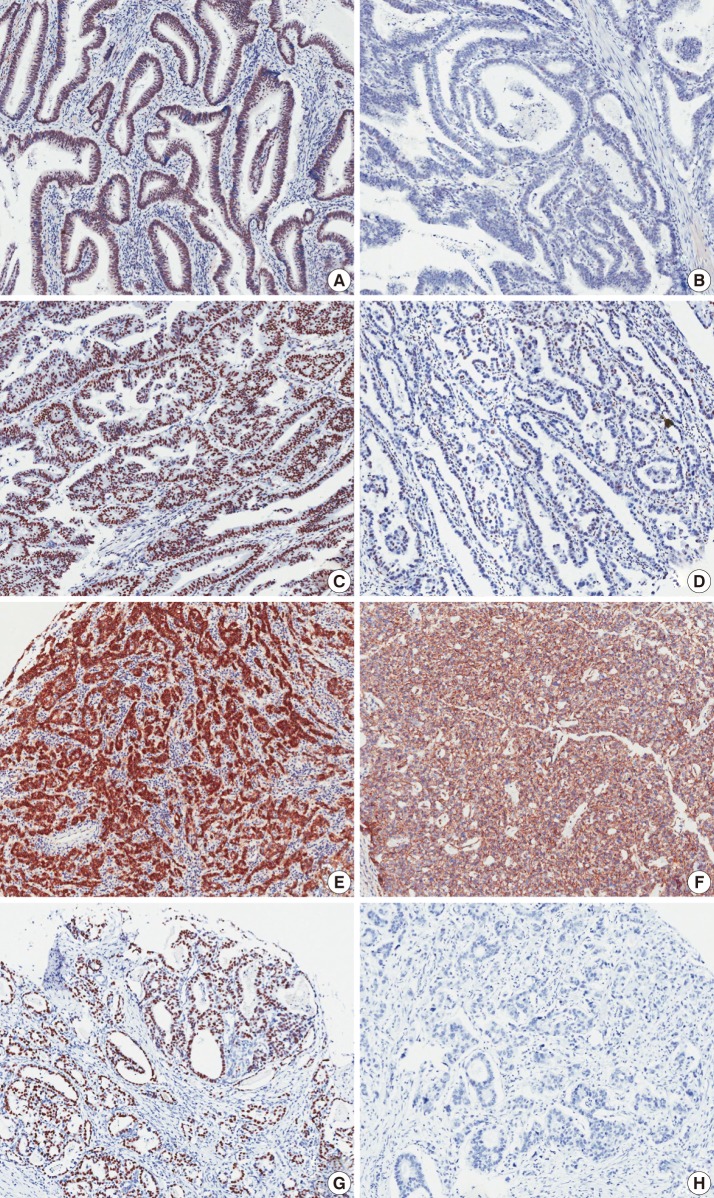
Immunohistochemical analysis by optical microscope was performed by two pathologist (Y.R.Kang and B.H.Kim). Immunohistochemical staining of p53 showed a nuclear staining pattern (Fig. 1). The nuclear staining intensity (0, no staining; 1, weak; 2, moderate; 3, strong) and percent areas of positive tumor cell nuclei were graded. When more than 50% of tumor cells showed a moderate or strong staining intensity, we considered it to be positive staining. To examine the correlation between the expression of p53 and other proteins, a cut-off value of 50% was applied to the p53.
Fig. 1.
Microscopic images of immunohistochemical staining. Sirtuin 1 (SIRT1) (A, B), deleted in breast cancer 1 (DBC1) (C, D), cytoplasmic β-catenin (E), membranous β-catenin (F), and p53 (G, H). The left panel shows positive staining (A, C, E, G) and right panel shows negative staining (B, D, F, H). Nuclear staining patterns are evident in SIRT1, DBC1, and p53 staining. β-Catenin figures show cytoplasmic staining (E) and membranous staining (F).
To analyze the β-catenin expression in tumor cells, the positivity of nuclear, cytoplasmic, and membranous staining was also scored. For nuclear and cytoplasmic staining, cases with tumor cells expressing more than 30% β-catenin were considered to be positive, and for membranous staining, cases with a pattern of loss of membranous β-catenin staining of more than 30% of tumor cells were regarded as negative (Fig. 1).
Analysis of immunohistochemical staining by image analyzer
Expression of DBC1 and SIRT1 were found mainly in the nuclei. To decrease the effects of observer biases, DBC1 and SIRT1 TMA slides were analyzed by an image analyzer program (IA). A Scanscope CS (Aperio, Vista, CA, USA) digital scanner was used for scanning of TMA slides. The scanned images were analyzed using an Aperio image analysis toolbox. A combination of the Genie histology pattern recognition tool (Aperio) and nuclear quantification cellular analysis tool (Aperio) was used to select tumor cells. The algorithm was adjusted to match the requirements of our particular marker and staining set. These adjustments include segmentation type, nuclear curvature threshold, size, roundness, compactness, and elongation. The output data contained the nuclear staining intensity (1+, 2+, 3+, and negative), positive tumor cell percentage, and cell count. The cut-off value of 30% was also applied to DBC1 and SIRT1 staining. When the sum of 2+ and 3+ cells exceeded 30% of the total tumor cells, the case was considered to be positive.
Statistical analysis
All statistical analyses were performed using the SPSS ver. 12 (SPSS Inc., Chicago, IL, USA). Kaplan-Meier plots and the log-rank test were used to estimate survival rates. The overall survival period was applied to this study. Overall survival was calculated as the time from diagnosis to the date of death or the last follow-up date. The median survival was 53.3 months. Correlations between the immunohistochemical expression of proteins and the clinicopathological characteristics were analyzed by Pearson's χ2 tests, but histologic grade and pathologic stage were analyzed by a Spearman's rank tests.
Multivariate analysis was performed using the Cox proportional hazard model. In all statistical analyses, a p<0.05 was considered statistically significant.
RESULTS
Expression of DBC1 and SIRT1, and correlation with clinicopathologic characteristics
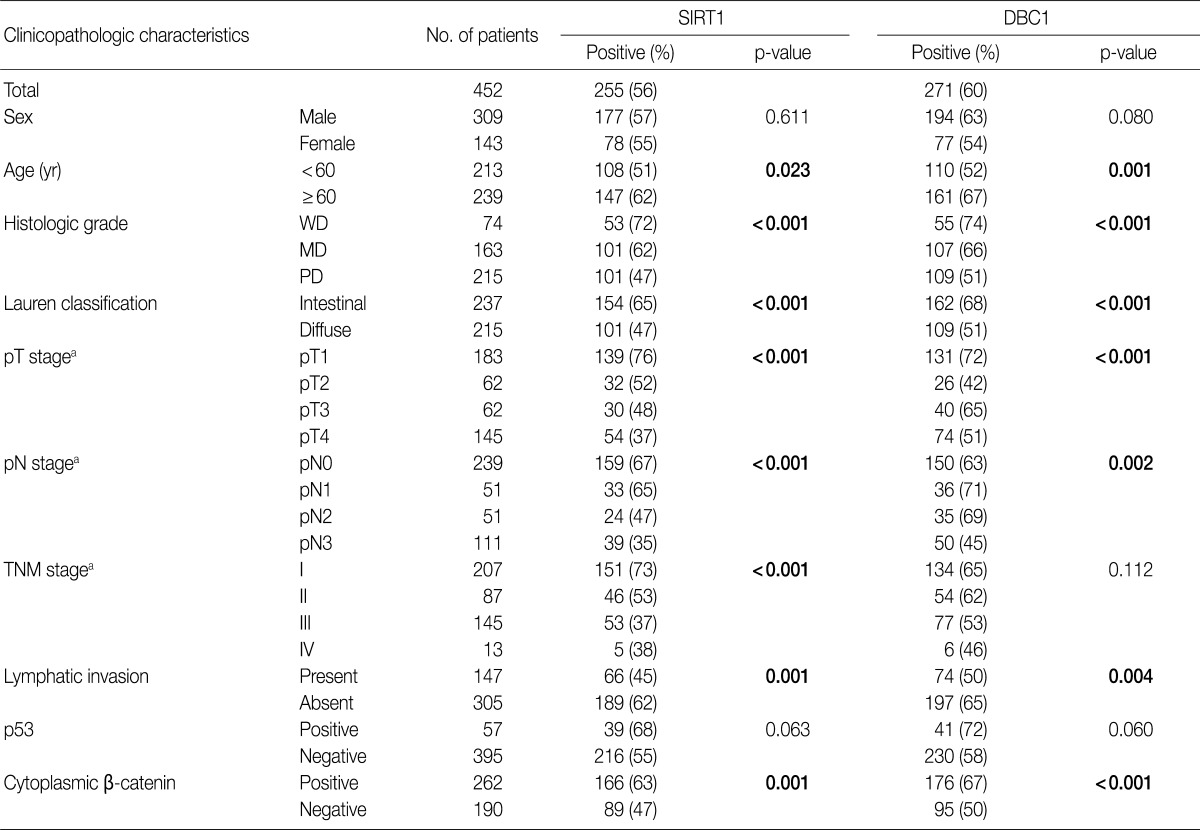
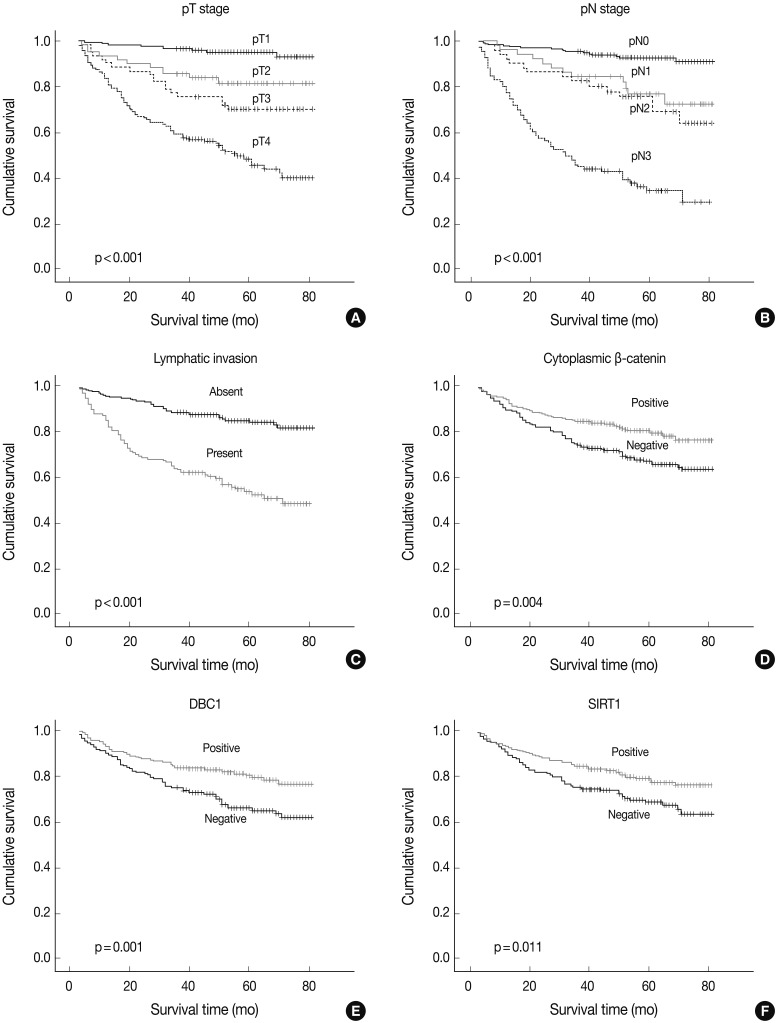
DBC1 and SIRT1 expression in gastric adenocarcinoma were observed in 271 (60%) and 255 (56%) patients. Expression of DBC1 and SIRT1 were significantly associated with lower histologic grade, intestinal type of Lauren classification, lower pathologic T stage (DBC1 and SIRT1, p<0.001), and lower pathologic N stage (DBC1, p=0.002; SIRT1, p<0.001). The lower TNM stage showed a significant association with SIRT1 (p<0.001), but not with DBC1 (p=0.112). A statistically significant association between the absence of lymphatic invasion and both SIRT1 (p=0.001) and DBC1 (p=0.004) was observed. Statistical associations between younger age (less than 60) and SIRT1 (p=0.023) and DBC1 (p=0.001) were also observed. However, neither sex was associated with SIRT1 (p=0.611) or DBC1 (p=0.080) expression (Table 1). SIRT1 (p=0.011) and DBC1 (p=0.001) showed significant association with better patient survival (Fig. 2). On regression analysis, expression of DBC1 and SIRT1 showed a significant linear association (p<0.001).
Table 1.
Correlations between clinicopathologic characteristics and the expression of SIRT1, DBC1, p53, and β-catenin
SIRT1, sirtuin 1; DBC1, deleted in breast cancer 1; WD, well differentiated; MD, moderately differentiated; PD, poorly differentiated; TNM, tumor-node-metastasis.
aAmerican Joint Committee on Cancer Cancer Staging Manual, 7th edition.
Fig. 2.
Kaplan-Meier survival plots. Pathologic T stage (A), pathologic N stage (B), lymphatic invasion (C), cytoplasmic β-catenin expression (D), deleted in breast cancer 1 (DBC1) (E), and sirtuin 1 (SIRT1) (F). The p-value is shown in each panel.
Expression of cytoplasmic β-catenin and p53
A cytoplasmic, membranous, and nuclear pattern of β-catenin expression was observed in 262 (58%), 367 (81%), and 28 (6%) cases, respectively. The cytoplasmic expression of β-catenin was significantly associated with lower histologic grade (p<0.001), lower pT stage (p<0.001), lower pN stage (p<0.001), lower TNM stage (p<0.001), SIRT1 (p<0.001), and DBC1 (p<0.001) (Table 1). The membranous pattern of β-catenin was also associated with lower histologic grade (p<0.001), lower pT stage (p<0.001), lower pN stage (p=0.003), lower TNM stage (p=0.001), SIRT1 (p=0.002), and DBC1 (p=0.013). Cytoplasmic β-catenin expression also showed a significant association with better patient survival (p=0.004) (Fig. 2). Nuclear β-catenin expression had no significant statistical association with any clinicopathologic factors.
Expression of p53 showed a statistical association with lower histologic grade (p<0.001). No association between p53 expression and SIRT1 (p=0.063) or DBC1 (p=0.060) expression was observed (Table 1). No pattern of β-catenin showed any correlation with p53 expression (p=0.508, p=0.768, p=0.196, or membranous, nuclear, or cytoplasmic expression of β-catenin, respectively). Expression of p53 had no association with patient survival (p=0.545).
Correlation of DBC1, SIRT1, cytoplasmic β-catenin, and p53 expression
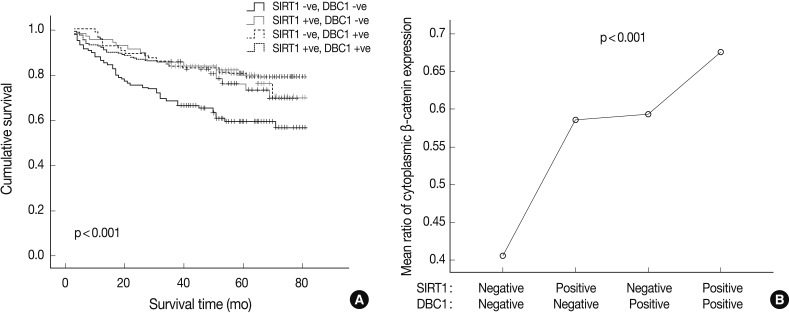
Simultaneous expression of both DBC1 and SIRT1 was significantly correlated with high expression of cytoplasmic β-catenin (p<0.001). However, the cases of concurrent negative expression of both DBC1 and SIRT1 showed no association with cytoplasmic β-catenin expression. Also, when DBC1 and SIRT1 were expressed as concurrent negative, it was significantly associated with poor patient survival (p<0.001) (Fig. 3). In contrast, there was no association between simultaneous expression of both DBC1 and SIRT1 and expression of p53 (p=0.089).
Fig. 3.
Kaplan-Meier survival curve (A) and ratio of cytoplasmic β-catenin expression (B) according to sirtuin 1 (SIRT1) and deleted in breast cancer 1 (DBC1) expression status. (A) Concurrent negative expression of the SIRT1 and DBC1 group is associated with poor survival. (B) The SIRT1(+) and DBC1(+) group is associated with high expression of cytoplasmic β-catenin (p<0.001).
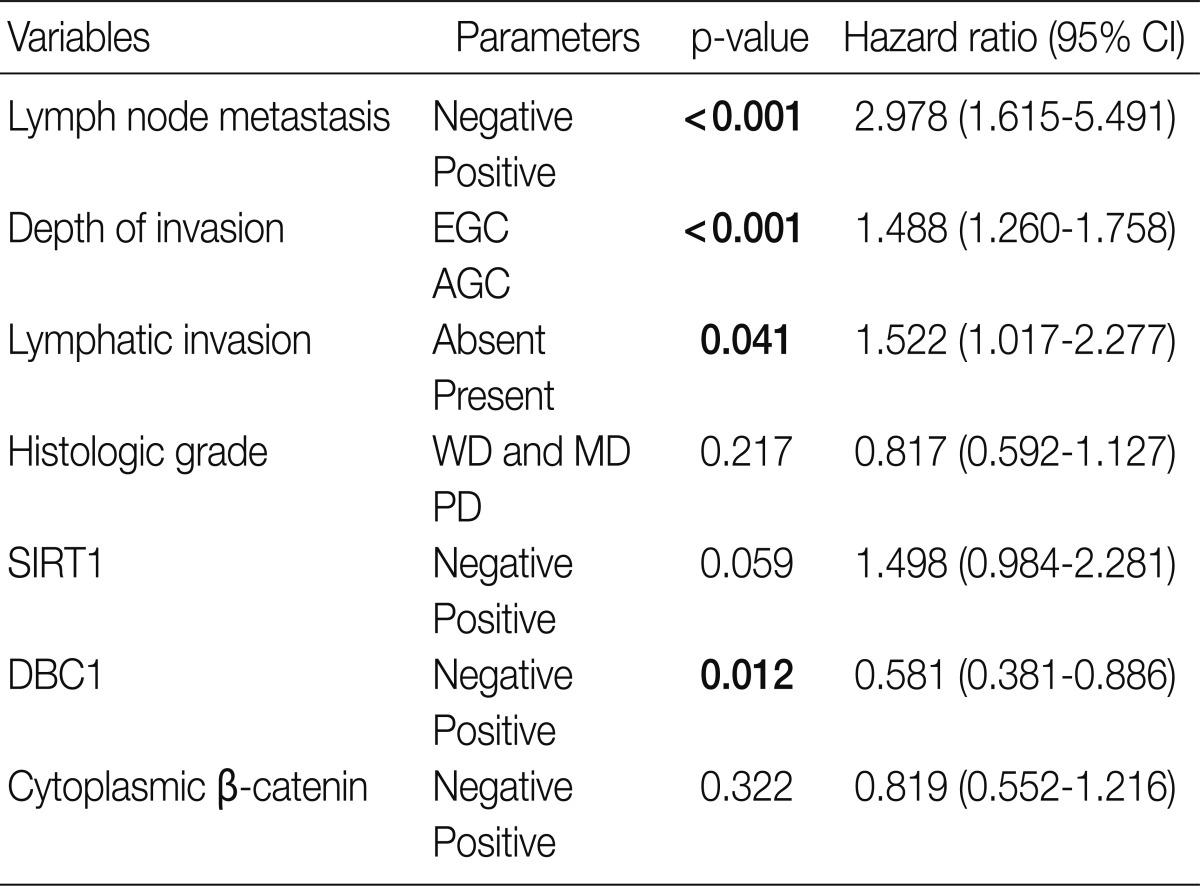
Multivariate analysis
We performed multivariate analysis with the clinicopathologic variables. DBC1 showed statistical significance in multivariate analysis (p=0.012) (Table 2). This means that expression of DBC1 was an independent good prognostic factor in gastric adenocarcinoma.
Table 2.
Multivariate analysis results
CI, confidence interval; EGC, early gastric cancer; AGC, advanced gastric cancer; WD, well differentiated; MD, moderately differentiated; PD, poorly differentiated; SIRT1, sirtuin 1; DBC1, deleted in breast cancer 1.
DISCUSSION
SIRT1 is a NAD+-dependent protein deacetylase that deacetylates diverse proteins as mentioned above.22-24 The first identified target of SIRT1 is the p53 tumor suppressor gene. SIRT1 deacetylates p53 and attenuates its ability for cell-cycle arrest and apoptosis, so the role of SIRT1 is considered to be tumor promotion in carcinogenesis.7,22,23,25 Another protein, DBC1, which is a SIRT1-associated protein, negatively regulates SIRT1 activity on p53 and inhibits tumor promoting activity of SIRT1.2,15,26 These two proteins, SIRT1 and DBC1, are thought to play a critical role in carcinogenesis. However, in gastric adenocarcinomas, only a few studies have been conducted with human tissue samples and their results are contrary to the previously known relationship between SIRT1 and DBC1.10,11 Therefore, in this study, we examined the expression of SIRT1 and DBC1 in human gastric adenocarcinomas and analyzed the association with SIRT1, DBC1, p53, β-catenin, and clinicopathologic variables.
We examined SIRT1 and DBC1 expression with an image analyzer. SIRT1 and DBC1 positive expression showed a direct correlation with each other, a result that is in concordance with previous study data.11 One study reported that expression of DBC1 and SIRT1 was significantly associated with shorter overall survival and greater risk of death, while expression of DBC1 is an independent prognostic factor for disease recurrence and poor survival outcome. However, in this analysis, conflicting results were produced. DBC1 and SIRT1 expression were correlated with better survival and good prognostic factors including lower histologic grade, intestinal type of Lauren classification, lower pathologic T (DBC1 and SIRT1, p<0.001) and N stage (DBC1, p=0.002; SIRT1, p<0.001), and absence of lymphatic invasion (SIRT1, p=0.001; DBC1, p=0.004). Notably, simultaneous expression of both DBC1 and SIRT1 was significantly correlated with high expression of cytoplasmic β-catenin (p<0.001) and better patient survival (p<0.001). We analyzed SIRT1 and DBC1 expression by an image analyzer that was optimized for the counting of nuclear protein expression to decrease intraobserver or interobserver bias in positive cell counting. The resultant data showed mostly similar survival data and a similar relationship between the expression of these two proteins and clinicopathologic variables. We concluded that there was no critical error in interpreting the immunoexpression of SIRT1 and DBC1 in TMA slides. Of course, other biases including selection bias, preservation of tissues, conditions of tissue staining, and so on may lead to an interpretation error, but this is an ineluctable consequence of using both an image analyzer and optical microscope.
We also analyzed p53 expression of gastric adenocarcinomas in association with SIRT1, DBC1, and β-catenin expression. Only lower histologic grade was associated with p53 expression (p<0.001).
Some recent study results indicate that SIRT1 could serve as a tumor suppressor by interaction with other proteins such as β-catenin, BRCA1, histone protein, and NF-κB.3,24,27-29 Therefore, we also examined the expression of β-catenin in gastric adenocarcinomas and analyzed its association with SIRT1 and DBC1 expression. Cytoplasmic, membranous, and nuclear expression of β-catenin were separately scored and analyzed. Cytoplasmic and membranous β-catenin expression showed significant associations with SIRT1 and DBC1 expression, lower histologic grade, lower tumor stage, and prolonged patient survival. Correlations between nuclear SIRT1 expression and β-catenin expression in the cytoplasm and cell membrane in concordance with a previous study that investigated colon cancer tumorigenesis.3 On the other hand, nuclear expression of β-catenin in this study was not correlated with SIRT1 expression, which may be due to the difficulty in counting positive nuclei in the presence of cytoplasmic staining. Therefore, we evaluated the relationship between the expression of cytoplasmic β-catenin and the others. Significant associations between SIRT1 and β-catenin in the cytoplasm and cell membrane suggest that SIRT1 expression suppresses the localization of β-catenin to the nucleus, and significantly attenuates its ability to activate transcription. This hypothesis could explain how SIRT1 and cytoplasmic β-catenin expression is correlated in gastric adenocarcinoma patients and how SIRT1 and β-catenin positive patients show better survival results. Similar to this hypothesis in this study, simultaneous expression of both DBC1 and SIRT1 showed significant associations with a high expression of cytoplasmic β-catenin (p<0.001) and better patient survival (p<0.001).
Multivariate analysis was performed with SIRT1 and DBC1. In multivariate analysis, lymph node metastasis (p<0.001), depth of invasion (p<0.001), and lymphatic invasion (p=0.041) were consistent independent prognostic factors. DBC1 expression was also an independent good prognostic factor (p=0.012). However, in a previous study, expression of DBC1 was an independent prognostic factor for disease recurrence and poor survival outcome.11 This discordant result may be due to observation error in interpretation of immunohistochemical staining slides. SIRT1 did not show prognostic significance in multivariate analysis.
Recent studies indicate that SIRT1 can serve as both a tumor promoter and a tumor suppressor.3 Some malignant tumors such as breast cancer, colon cancer, and prostate cancer are known to have increased nuclear expression of SIRT1.4,6,7 However, in some tumors including glioblastoma, bladder cancer, and ovarian cancers, reduced expression of SIRT1 was also found.30 These contradictory findings may be attributable to the diverse functions of SIRT1, which can interact with both tumor suppressors and tumor promoters. In this study, we analyzed SIRT1, β-catenin, and p53 together. It appears that expression of SIRT1 is closely associated with the cytoplasmic expression of β-catenin in gastric adenocarcinoma. This finding could explain why SIRT1 positive groups showed better survival. The relationship between SIRT1 and p53 in gastric adenocarcinoma is unclear in these study results. We could not find a relationship between SIRT1 and p53 (p=0.063). Therefore, we believe this weak correlation may be due to a partial relationship between SIRT1 and p53. In another study, expression of p53 showed no significant correlation between SIRT1 expression cases and negative cases.10 In spite of the interaction between SIRT1 and p53, immunohistochemical correlation may or may not exist. More intense research dealing with SIRT1 and SIRT1-related protein is necessary to understand the diverse roles of SIRT1 in gastric carcinogenesis.
In some studies, the various roles of DBC1 have been examined. First of all, DBC1 was found to augment signals of apoptosis via relocalization of the DBC1 C-terminal fragment into the mitochondria.26 DBC1 is also able to regulate the transcriptional activity of some nuclear hormone receptors including retinoic acid receptor α and AR.26 DBC1 is known to inhibit SIRT1 through a direct protein to protein interaction and thus promotes p53 mediated apoptosis.2 However, mutation of DBC1 does not direct binding to SIRT1, so it should not affect enzymatic activity of SIRT1 and the acetylation state of SIRT1 substrates including p53.2 In this regard, a negative correlation is expected between SIRT1 and DBC1 expressions. However, in this study, expression of DBC1 was significantly correlated with SIRT1 expression (p<0.001).
In agreement with our data, some study results revealed upregulation of DBC1 in various types of malignancies. Moreover, recent studies have reported a positive correlation of SIRT1 and DBC1 expression in human cancer tissues.8,11 These results may be due to the recently identified diverse functions of DBC1 other than inhibition of SIRT1.16,26 Though DBC1 expression of gastric adenocarcinoma is associated with SIRT1 expression, the role of DBC1 in gastric carcinogenesis may be other than inhibition of SIRT1.
In summary, expression of DBC1, SIRT1, and cytoplasmic and membranous β-catenin in gastric adenocarcinoma showed significant correlations with each other. Furthermore, expressions of these three proteins were associated with lower histologic grade, lower tumor stage, and better patient survival. However, there was no evident association between SIRT1 and p53 protein. The role of SIRT1 and DBC1 in gastric carcinogenesis should be considered carefully in correlation with other proteins that interact with SIRT1 and DBC1.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Guarente L, Picard F. Calorie restriction: the SIR2 connection. Cell. 2005;120:473–482. doi: 10.1016/j.cell.2005.01.029. [DOI] [PubMed] [Google Scholar]
- 2.Kim JE, Chen J, Lou Z. DBC1 is a negative regulator of SIRT1. Nature. 2008;451:583–586. doi: 10.1038/nature06500. [DOI] [PubMed] [Google Scholar]
- 3.Firestein R, Blander G, Michan S, et al. The SIRT1 deacetylase suppresses intestinal tumorigenesis and colon cancer growth. PLoS One. 2008;3:e2020. doi: 10.1371/journal.pone.0002020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen WY, Wang DH, Yen RC, Luo J, Gu W, Baylin SB. Tumor suppressor HIC1 directly regulates SIRT1 to modulate p53-dependent DNA-damage responses. Cell. 2005;123:437–448. doi: 10.1016/j.cell.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 5.Hida Y, Kubo Y, Murao K, Arase S. Strong expression of a longevity-related protein, SIRT1, in Bowen's disease. Arch Dermatol Res. 2007;299:103–106. doi: 10.1007/s00403-006-0725-6. [DOI] [PubMed] [Google Scholar]
- 6.Kuzmichev A, Margueron R, Vaquero A, et al. Composition and histone substrates of polycomb repressive group complexes change during cellular differentiation. Proc Natl Acad Sci U S A. 2005;102:1859–1864. doi: 10.1073/pnas.0409875102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huffman DM, Grizzle WE, Bamman MM, et al. SIRT1 is significantly elevated in mouse and human prostate cancer. Cancer Res. 2007;67:6612–6618. doi: 10.1158/0008-5472.CAN-07-0085. [DOI] [PubMed] [Google Scholar]
- 8.Lee H, Kim KR, Noh SJ, et al. Expression of DBC1 and SIRT1 is associated with poor prognosis for breast carcinoma. Hum Pathol. 2011;42:204–213. doi: 10.1016/j.humpath.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 9.Saunders LR, Verdin E. Sirtuins: critical regulators at the crossroads between cancer and aging. Oncogene. 2007;26:5489–5504. doi: 10.1038/sj.onc.1210616. [DOI] [PubMed] [Google Scholar]
- 10.Feng AN, Zhang LH, Fan XS, et al. Expression of SIRT1 in gastric cardiac cancer and its clinicopathologic significance. Int J Surg Pathol. 2011;19:743–750. doi: 10.1177/1066896911412181. [DOI] [PubMed] [Google Scholar]
- 11.Cha EJ, Noh SJ, Kwon KS, et al. Expression of DBC1 and SIRT1 is associated with poor prognosis of gastric carcinoma. Clin Cancer Res. 2009;15:4453–4459. doi: 10.1158/1078-0432.CCR-08-3329. [DOI] [PubMed] [Google Scholar]
- 12.Czyzewska J, Guzińska-Ustymowicz K, Ustymowicz M, Pryczynicz A, Kemona A. The expression of E-cadherin-catenin complex in patients with advanced gastric cancer: role in formation of metastasis. Folia Histochem Cytobiol. 2010;48:37–45. doi: 10.2478/v10042-010-0017-z. [DOI] [PubMed] [Google Scholar]
- 13.Ciocca DR, Calderwood SK. Heat shock proteins in cancer: diagnostic, prognostic, predictive, and treatment implications. Cell Stress Chaperones. 2005;10:86–103. doi: 10.1379/CSC-99r.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamaguchi M, Meth JL, von Klitzing C, et al. DBC2, a candidate for a tumor suppressor gene involved in breast cancer. Proc Natl Acad Sci U S A. 2002;99:13647–13652. doi: 10.1073/pnas.212516099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao W, Kruse JP, Tang Y, Jung SY, Qin J, Gu W. Negative regulation of the deacetylase SIRT1 by DBC1. Nature. 2008;451:587–590. doi: 10.1038/nature06515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fu J, Jiang J, Li J, et al. Deleted in breast cancer 1, a novel androgen receptor (AR) coactivator that promotes AR DNA-binding activity. J Biol Chem. 2009;284:6832–6840. doi: 10.1074/jbc.M808988200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trauernicht AM, Kim SJ, Kim NH, Boyer TG. Modulation of estrogen receptor alpha protein level and survival function by DBC-1. Mol Endocrinol. 2007;21:1526–1536. doi: 10.1210/me.2007-0064. [DOI] [PubMed] [Google Scholar]
- 18.Park SH, Lee SI. Recent advances in chemotherapy of gastric cancer. Korean J Med. 2012;82:417–426. [Google Scholar]
- 19.Jang BG, Kim WH. Molecular pathology of gastric carcinoma. Pathobiology. 2011;78:302–310. doi: 10.1159/000321703. [DOI] [PubMed] [Google Scholar]
- 20.Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC cancer staging handbook: from the AJCC cancer staging manual. 7th ed. New York: Springer; 2010. [Google Scholar]
- 21.Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC Press; 2010. [Google Scholar]
- 22.Vaziri H, Dessain SK, Ng Eaton E, et al. hSIR2(SIRT1) functions as an NAD-dependent p53 deacetylase. Cell. 2001;107:149–159. doi: 10.1016/s0092-8674(01)00527-x. [DOI] [PubMed] [Google Scholar]
- 23.Luo J, Nikolaev AY, Imai S, et al. Negative control of p53 by Sir2alpha promotes cell survival under stress. Cell. 2001;107:137–148. doi: 10.1016/s0092-8674(01)00524-4. [DOI] [PubMed] [Google Scholar]
- 24.Kyrylenko S, Kyrylenko O, Suuronen T, Salminen A. Differential regulation of the Sir2 histone deacetylase gene family by inhibitors of class I and II histone deacetylases. Cell Mol Life Sci. 2003;60:1990–1997. doi: 10.1007/s00018-003-3090-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford J, Jiang M, Milner J. Cancer-specific functions of SIRT1 enable human epithelial cancer cell growth and survival. Cancer Res. 2005;65:10457–10463. doi: 10.1158/0008-5472.CAN-05-1923. [DOI] [PubMed] [Google Scholar]
- 26.Kim JE, Lou Z, Chen J. Interactions between DBC1 and SIRT 1 are deregulated in breast cancer cells. Cell Cycle. 2009;8:3784–3785. doi: 10.4161/cc.8.22.10055. [DOI] [PubMed] [Google Scholar]
- 27.Mullan PB, Quinn JE, Harkin DP. The role of BRCA1 in transcriptional regulation and cell cycle control. Oncogene. 2006;25:5854–5863. doi: 10.1038/sj.onc.1209872. [DOI] [PubMed] [Google Scholar]
- 28.Wang RH, Zheng Y, Kim HS, et al. Interplay among BRCA1, SIRT1, and survivin during BRCA1-associated tumorigenesis. Mol Cell. 2008;32:11–20. doi: 10.1016/j.molcel.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yeung F, Hoberg JE, Ramsey CS, et al. Modulation of NF-kappaB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 2004;23:2369–2380. doi: 10.1038/sj.emboj.7600244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin SJ, Defossez PA, Guarente L. Requirement of NAD and SIR2 for life-span extension by calorie restriction in Saccharomyces cerevisiae. Science. 2000;289:2126–2128. doi: 10.1126/science.289.5487.2126. [DOI] [PubMed] [Google Scholar]