Abstract
Mucinous cystadenocarcinoma (MCA) in the breast is a rare neoplasm. There have been 13 cases of primary breast MCA reported. The MCA presents as a large, partially cystic mass in postmenopausal woman with a good prognosis. The microscopic findings resemble those of ovarian, pancreatic, or appendiceal MCA. The aspiration findings showed mucin-containing cell clusters in the background of mucin and necrotic material. The cell clusters had intracytoplasmic mucin displacing atypical nuclei to the periphery. Histologically, the tumor revealed an abundant mucin pool with small floating clusters of mucin-containing tumor cells. There were also small cysts lined by a single layer of tall columnar mucinous cells, resembling those of the uterine endocervix. The cancer cells were positive for mucin (MUC) 5 and negative for MUC2 and MUC6. This mucin profile is different from ordinary mucinous carcinoma and may be a unique characteristic of breast MCA.
Keywords: Mucinous cystadenocarcinoma, Breast, MUC5, MUC2
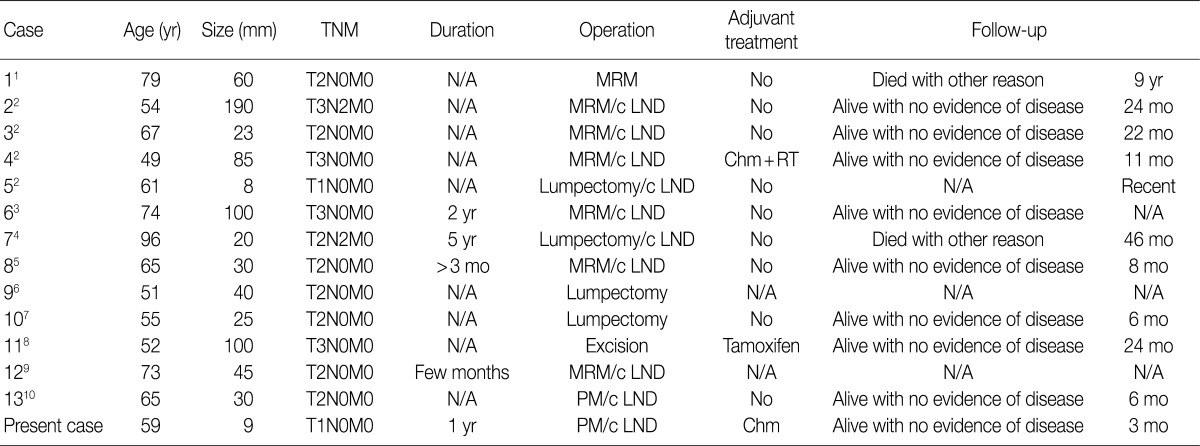
The primary mucinous cystadenocarcinoma (MCA) of the breast is an extremely rare neoplasm. The most common sites of MCA include the ovary, pancreas and appendix. Only 13 cases of primary MCA of the breast have been reported, since Koenig and Tavassoli reported the first 4 cases of MCA in 1998 (Tables 1, 2).1-10 The breast MCAs showed unique clinico-pathologic characteristics, distinguishable from ordinary mucinous carcinoma (MC) and signet ring cell carcinoma. Clinically, MCA in the breast is found in postmenopausal women and present as a relatively large, cystic mass with a favorable prognosis. Microscopically, the cysts are lined by tall columnar mucinous cells, resembling those of endocervical glands. The MCA tumors demonstrate consistent immunohistochemical staining (IHC) results with negative estrogen receptor (ER), negative progesterone receptor (PR), positive cytokeratin 7 (CK7), and negative cytokeratin 20 (CK20). The c-erbB2 IHC results are available in five cases.4,5,7-9 They are negative in four and positive in one with HER-2 gene amplification confirmed by fluorescence in situ hybridization.9
Table 1.
Clinical feature of mucinous cystadenocarcinoma in the breast
TNM, tumor-node-metastasis; N/A, not acquired; MRM, modified radical mastectomy; c LND, with lymph node dissection; Chm+RT, chromatography+radiation therapy; PM, partial mastectomy.
Table 2.
Immunohistochemical feature of mucinous cystadenocarcinoma in the breast
ER, estrogen receptor; PR, progesterone receptor; CK7, cytokeratin 7; CK20, cytokeratin 20; N, negative; P, positive.
In the case being reported here, the mass was only 9 mm, though the size before core biopsy was assessed to be 14 mm by ultrasound examination. Other characteristics of this new case share those clinical, cytological, and histopathological findings described in previously published cases (Tables 1, 2). In this paper, we present a rare cytologic finding of primary MCA in the breast and the characteristics of mucin (MUC).
CASE REPORT
Clinical summary
A 59-year-old postmenopausal woman presented with an illdefined, hard mass in her left breast for a year. Radiologic evaluations demonstrated a hypo-echoic mass (14 mm) with a speculated margin in ultrasonography and a focal asymmetric density in the upper medial portion by mammography. Fine needle aspiration followed by needle biopsy was performed with the diagnosis of MC and invasive carcinoma with abundant mucin pool formation, respectively. She underwent partial mastectomy with sentinel lymph node biopsy. The sentinel lymph node was free from metastasis. She has been followed for 3 months with chemotherapy for adjuvant treatment and remains disease-free.
Pathologic findings
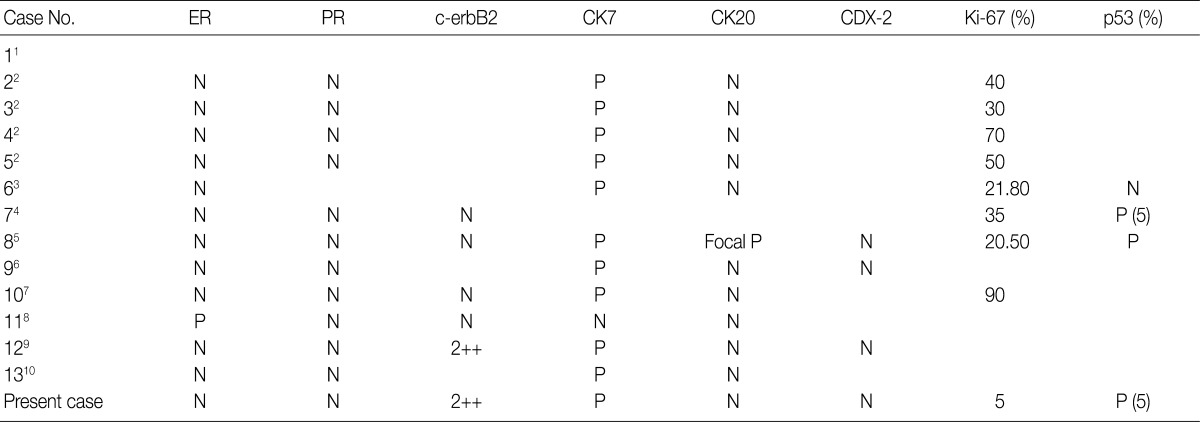
The aspiration showed a few scattered, variably sized, irregular clusters of columnar cells in the greenish blue mucinous background with necrotic debris. The columnar cells contained abundant mucin vacuoles in cytoplasm which had displaced their nuclei. The nuclear membrane was irregular and sharply angulated and the nuclei revealed a coarse chromatin pattern with prominent nucleoli (Fig. 1).
Fig. 1.
Cytologic features of mucinous cystadenocarcinoma. (A) A few scattered, variably sized, irregular clusters of columnar cells with pleomorphism and anisocytosis in a greenish blue mucinous background and necrotic debris. (B) The cells contain abundant mucin vacuoles in cytoplasm that attenuate and displace their nuclei. The nuclear membrane is irregular and sharply angulated and the nuclei reveal a coarse chromatin pattern with prominent nucleoli.
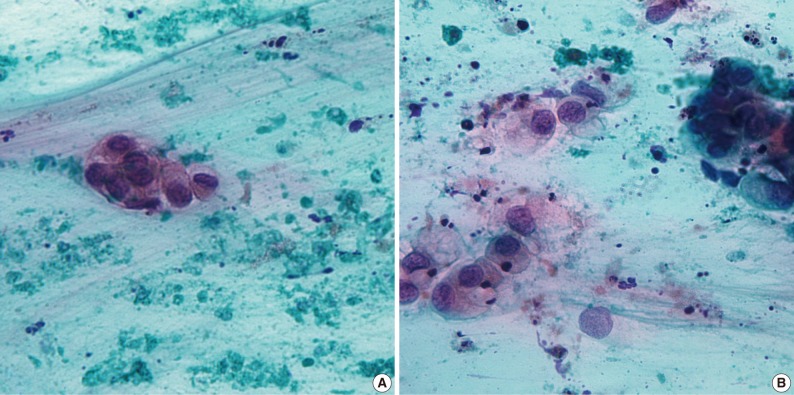
On gross examination, the cut surface showed an irregular, white to tan, solid and firm mass (9×7 mm), with a glistening appearance. Most MCAs in previous reports have demonstrated grossly cystic cut surfaces, except one case of MCA reported from Koenig and Tavassoli2 in 1998.1,3-10 The case in 1998 was small in size (8 mm) and had a grossly solid appearance. The present case was 9 mm in maximal diameter and did not contain a macroscopic cyst. It is assumed that the small size of the MCA meant that it did not produce enough mucin to fill out and dilate cysts and ductal structures. The microscopic findings revealed a few cysts and ductal carcinoma in situ, adjacent to the invasive carcinoma. The cysts were lined by a single layer of tall columnar mucinous cells with focal areas of micropapillary structures, resembling those of the uterine endocervix. The luminal space contained mucin (Fig. 2). The invasive cancer area contained an abundant mucin pool in stroma with floating cell clusters. The floating cells contained mucin vacuoles in cytoplasm displacing atypical nuclei to the periphery.
Fig. 2.
Histologic features of mucinous cystadenocarcinoma. (A) The tumor shows an abundant mucin pool in stroma with floating cell clusters. (B) The ductal carcinoma in situ is found in the form of small cysts, adjacent to the invasive carcinoma. The cysts are lined by a single layer of tall columnar mucinous cells with focal areas of micropapillary and small tufted structures, resembling those of the uterine endocervix. (C) The invasive cells are pleomorphic and contained mucin vacuoles in cytoplasm displacing atypical nuclei to the periphery. (D) Both the intracytoplasmic and extracytoplasmic mucin are stained by alcian blue.
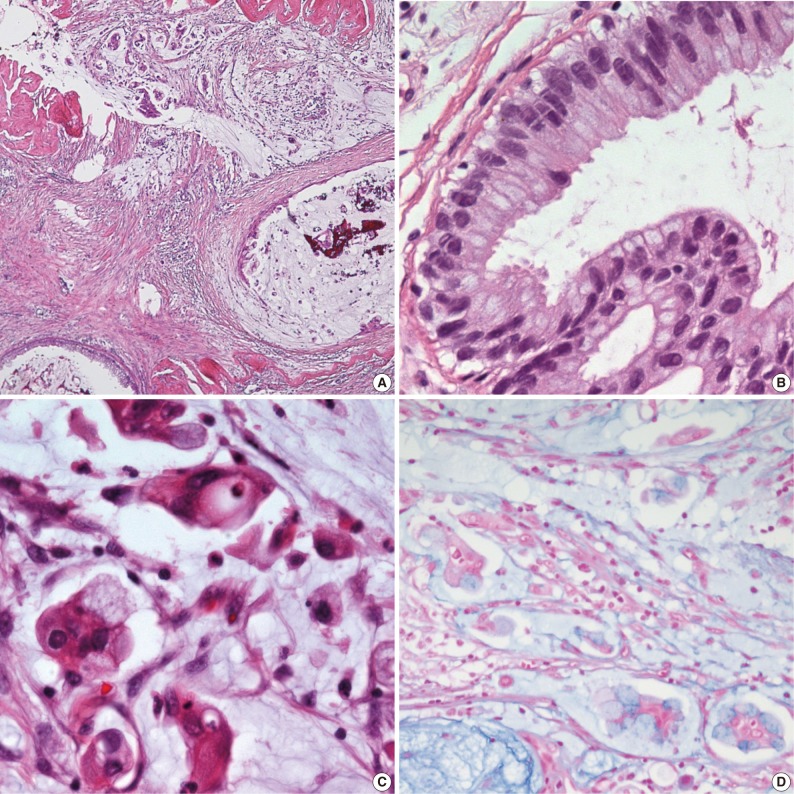
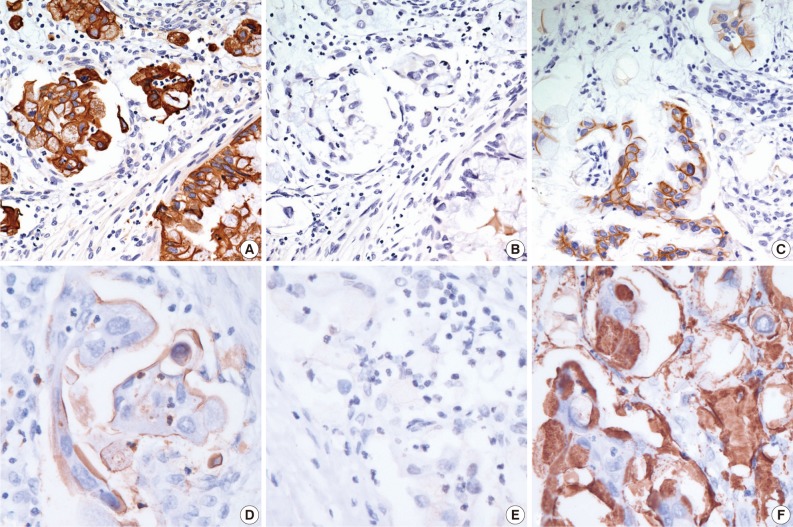
Special staining and IHC on paraffin embedded tissue were performed. Both intracytoplasmic and extracytoplasmic mucin were stained by periodic acid-Schiff with diastase, alcian blue and mucicarcine, representing the acidic and neutral nature of mucin. The tumor cells were positive for CK7 and negative for CK20 and CDX-2. The IHC for MUC proteins was performed. The cancer cells were positive for MUC5 and MUC1 and negative for MUC2 and MUC6. Mucin of the intracytoplasm and stroma revealed positivity for MUC5 and negativity for the other MUC proteins (MUC1, MUC2, and MUC6). The hormone receptors, ER and PR, were negative. The c-erbB2 was 2-positive (Fig. 3), but silver in situ hybridization demonstrated no amplification of the HER-2 gene.
Fig. 3.
Immunohistochemical staining of mucinous cystadenocarcinoma. The tumor cells are positive for cytekeratin 7 (A) and negative for cytokeratin 20 (B). The hormone receptors, estrogen receptor and progesterone receptor, are negative and the c-erbB2 is 2-positive (C). The tumor cells are positive for mucin (MUC) 1 (D) along the cytoplasmic membrane and negative for MUC2 (E). Mucin of the intracytoplasm and stroma reveal positivity for MUC5 (F).
DISCUSSION
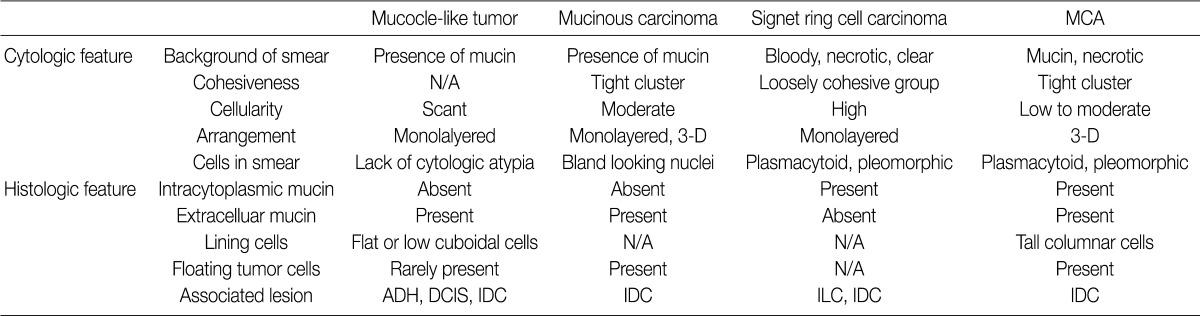
In the breasts, mucin-producing tumors are classified as MC, signet ring cell carcinoma (SRC), or mucocele-like tumors.11 The differences among mucin-containing tumors in the breast are shown in Table 3.12-14 MC and mucocele-like tumors are characterized by abundant extracellular mucin with floating neoplastic cells that do not contain intracytoplasmic mucin. The mucocele-like tumor is benign and the floating tumor cells are very rare. MC is specific type of invasive ductal caricinoma. The cytologic features show tight clusters of bland looking cells with moderate cellularity in the mucinous background.13 SRC demonstrates mucin only in the cytoplasm. The aspiration reveals a cellular smear of pleomorphic and plasmocytoid cells with intracytoplasmic mucin in the bloody or necrotic background.14 MCA has similar characteristics to both MC and SRC. The aspiration smears reveal tight clusters of mucin-containing cells of low to moderate cellularity in the background of mucinous and necrotic material. The histopathologic findings confirm both, intracytoplasmic and extracytoplasmic mucin.
Table 3.
Comparison of mucin-producing tumors in the breast
MCA, mucinous cystadenocarcinoma; N/A, not availale; ADH, atypical ductal hyperplasia; DCIS, ductal carcinoma in situ; IDC, invasive ductal carcinoma; ILC, infiltrating lobular carcinoma.
Mucin is a high molecular weight glycoprotein that consists of one protein core and O-linked carbohydrate side chains attached.15 Epithelial cells produce two types of mucin. One is secretory mucin (MUC2, MUC5, and MUC6) and the other is trans-membrane mucin (MUC1, MUC3, MCU4, MUC12, and MUC17).16 They are expressed differently according to the types of organs and tumors. For example, MC of the colon shows high positivity for MUC2.17 SRC of the colon shows MUC2 and MUC4 positivity.16 Among breast cancers, MC expresses mainly MUC2 along with a low level of MUC1, while SRC of the breast has a high level of MUC1 expression with a variable level of MUC2.18 In the breasts, MUC5 is not frequently observed. MCs of the breast express MUC5 in only small proportions (less than 5%).19 In our case of MCA reported here, the MUC IHC demonstrates a high level of expression of MUC5 and no expression of MUC2 or MUC6. This mucin profile is different from ordinary mucinous carcinoma arising in the breast and other organs. MUC5-positive and MUC2-negative immunoprofiles have not been reported before, in breast carcinoma.
Because of the rarity of mammary MCA, the diagnosis has to be made cautiously. Thus metastasis from distant organs should be initially considered. The usual immunoprofiles to rule out metastasis from distant MCA are following: CK7 positive, CK20 negative, and CDX-2 negative. These results can help to exclude the possibility of metastatic MCA from the ovary, pancreas, and gastrointestinal tract. Being MUC5 positive and MUC2 negative may be the unique characteristics of MCA in the breast, together with the immunoprofiles of being CK7 positive, CK20 negative, CDX-2 negative, ER negative, and PR negative.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Rosen PP, Scott M. Cystic hypersecretory duct carcinoma of the breast. Am J Surg Pathol. 1984;8:31–41. doi: 10.1097/00000478-198401000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Koenig C, Tavassoli FA. Mucinous cystadenocarcinoma of the breast. Am J Surg Pathol. 1998;22:698–703. doi: 10.1097/00000478-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Domoto H, Terahata S, Yamazaki T, Sato K, Takeo H, Tamai S. Mucinous cystadenocarcinoma of the breast showing sulfomucin production. Histopathology. 2000;36:567–569. doi: 10.1046/j.1365-2559.2000.00918-3.x. [DOI] [PubMed] [Google Scholar]
- 4.Honma N, Sakamoto G, Ikenaga M, Kuroiwa K, Younes M, Takubo K. Mucinous cystadenocarcinoma of the breast: a case report and review of the literature. Arch Pathol Lab Med. 2003;127:1031–1033. doi: 10.5858/2003-127-1031-MCOTBA. [DOI] [PubMed] [Google Scholar]
- 5.Chen WY, Chen CS, Chen HC, Hung YJ, Chu JS. Mucinous cystadenocarcinoma of the breast coexisting with infiltrating ductal carcinoma. Pathol Int. 2004;54:781–786. doi: 10.1111/j.1440-1827.2004.01755.x. [DOI] [PubMed] [Google Scholar]
- 6.Coyne JD, Irion L. Mammary mucinous cystadenocarcinoma. Histopathology. 2006;49:659–660. doi: 10.1111/j.1365-2559.2006.02471.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee SH, Chaung CR. Mucinous metaplasia of breast carcinoma with macrocystic transformation resembling ovarian mucinous cystadenocarcinoma in a case of synchronous bilateral infiltrating ductal carcinoma. Pathol Int. 2008;58:601–605. doi: 10.1111/j.1440-1827.2008.02278.x. [DOI] [PubMed] [Google Scholar]
- 8.Rakici S, Gönüllü G, Gürsel SB, Yildiz L, Bayrak IK, Yücel I. Mucinous cystadenocarcinoma of the breast with estrogen receptor expression: a case report and review of the literature. Case Rep Oncol. 2009;2:210–216. doi: 10.1159/000253866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Petersson F, Pang B, Thamboo TP, Putti TC. Mucinous cystadenocarcinoma of the breast with amplification of the HER2-gene confirmed by FISH: The first case reported. Hum Pathol. 2010;41:910–913. doi: 10.1016/j.humpath.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 10.Sentani K, Tashiro T, Uraoka N, et al. Primary mammary mucinous cystadenocarcinoma: cytological and histological findings. Diagn Cytopathol. 2012;40:624–628. doi: 10.1002/dc.21638. [DOI] [PubMed] [Google Scholar]
- 11.Rosen PP. Rosen's breast pathology. 3rd ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2009. pp. 515–534. [Google Scholar]
- 12.Cheng L, Lee WY, Chang TW. Benign mucocele-like lesion of the breast: how to differentiate from mucinous carcinoma before surgery. Cytopathology. 2004;15:104–108. doi: 10.1111/j.1365-2303.2004.00130.x. [DOI] [PubMed] [Google Scholar]
- 13.Laucirica R, Bentz JS, Khalbuss WE, Clayton AC, Souers RJ, Moriarty AT. Performance characteristics of mucinous (colloid) carcinoma of the breast in fine-needle aspirates: observations from the College of American Pathologists Interlaboratory Comparison Program in Nongynecologic Cytopathology. Arch Pathol Lab Med. 2011;135:1533–1538. doi: 10.5858/arpa.2010-0652-CP. [DOI] [PubMed] [Google Scholar]
- 14.Kelten C, Akbulut M, Zekioglu O, Kapkac M, Erhan Y, Ozdemir N. Signet ring cells in fine needle aspiration cytology of breast carcinomas: review of the cytological findings in ten cases identified by histology. Cytopathology. 2009;20:321–327. doi: 10.1111/j.1365-2303.2008.00630.x. [DOI] [PubMed] [Google Scholar]
- 15.Lau SK, Weiss LM, Chu PG. Differential expression of MUC1, MUC2, and MUC5AC in carcinomas of various sites: an immunohistochemical study. Am J Clin Pathol. 2004;122:61–69. doi: 10.1309/9R66-73QE-C06D-86Y4. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen MD, Plasil B, Wen P, Frankel WL. Mucin profiles in signet-ring cell carcinoma. Arch Pathol Lab Med. 2006;130:799–804. doi: 10.5858/2006-130-799-MPISCC. [DOI] [PubMed] [Google Scholar]
- 17.Chu PG, Chung L, Weiss LM, Lau SK. Determining the site of origin of mucinous adenocarcinoma: an immunohistochemical study of 175 cases. Am J Surg Pathol. 2011;35:1830–1836. doi: 10.1097/PAS.0b013e3182299c25. [DOI] [PubMed] [Google Scholar]
- 18.Hanski C, Hofmeier M, Schmitt-Gräff A, et al. Overexpression or ectopic expression of MUC2 is the common property of mucinous carcinomas of the colon, pancreas, breast, and ovary. J Pathol. 1997;182:385–391. doi: 10.1002/(SICI)1096-9896(199708)182:4<385::AID-PATH861>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 19.Matsukita S, Nomoto M, Kitajima S, et al. Expression of mucins (MUC1, MUC2, MUC5AC and MUC6) in mucinous carcinoma of the breast: comparison with invasive ductal carcinoma. Histopathology. 2003;42:26–36. doi: 10.1046/j.1365-2559.2003.01530.x. [DOI] [PubMed] [Google Scholar]