Abstract
People with cancer experience many unanticipated symptoms and struggle to communicate them to clinicians. Although researchers have developed patient-reported outcome (PRO) tools to address this problem, such tools capture retrospective data intended for clinicians to review. In contrast, real-time tracking tools with visible results for patients could improve health outcomes and communication with clinicians, while also enhancing patients’ symptom management. To understand potential benefits of such tools, we studied the tracking behaviors of 25 women with breast cancer. We provided 10 of these participants with a real-time tracking tool that served as a “technology probe” to uncover behaviors and benefits from voluntary use. Our findings showed that while patients’ tracking behaviors without a tool were fragmented and sporadic, these behaviors with a tool were more consistent. Participants also used tracked data to see patterns among symptoms, feel psychosocial comfort, and improve symptom communication with clinicians. We conclude with design implications for future real-time tracking tools.
1. Introduction
Many patients with cancer struggle to manage symptoms during treatment. These patients have to contend with a variety of symptoms at home—issues stemming from cancer progression, treatment regimens, and co-morbidities—and many rely on clinic visits to get help with managing these symptoms. Yet, patients have difficulty communicating the full extent of their symptoms to clinicians,1 as they manage symptoms away from the clinic, in between chemotherapy infusions, surgeries, radiation treatments, and follow-up appointments.2 Although common cancer treatment-related symptoms, such as pain or fatigue, can have serious consequences if they are not controlled,3 clinicians frequently underestimate the intensity of patients’ symptoms and undertreat them.4
Real-time tracking of symptoms by patients could address these problems. Patients who track their symptoms at home as they occur could share symptom severity, frequency, and duration with clinicians. Thus, clinicians could better understand and address symptom burden. In addition, patients with cancer who decide to undertake real-time tracking on their own could experience other benefits that so far have not been explored in the literature.
However, we do not fully understand how patients with cancer track their symptoms. To address this gap in knowledge, we first analyzed the natural tracking behaviors of 25 patients with breast cancer and then deployed a personal health information management tool with real-time tracking features to 10 of those patients. We deployed this tool as a technology probe, a type of user study in which technology is deployed, in part, with “the social science goal of understanding the needs and desires of users in a real-world setting”5 and not just to evaluate whether a technology is effective in a prescribed setting. This type of study is particularly valuable for the design of consumer health technologies, which tend to be used in a variety of settings and where a full range of real-life user needs cannot be identified fully in lab studies.
In this research, we define self-tracking as the measurement or observation and self report of bodily symptoms and their impact on daily activities and cognitive processes.6 A tracking tool is used to support self-tracking of issues of interest. Tracking tools can be as simple as a piece of paper and a pencil or as complex as an Excel spreadsheet with pivot tables and charts. Real-time tracking tools can support capturing health issues in the moment, as they occur.
2. Background
To address symptom management and communication during cancer care, researchers have developed patient-reported outcome (PRO) tools7,8,9,10 that raise clinician awareness of patients’ symptoms. PRO tools measure symptom distress and quality of life periodically or immediately prior to appointments using validated questionnaires. In a few research settings, computer-based tools periodically administer PRO questionnaires to patients and generate summaries for clinicians to review, typically at appointment times. Reported benefits of PRO tools include improved patient well-being,9 lower toxicity,7 and improved patient-clinician communication.8 However, existing PRO tools do not leverage features from real-time tracking or sensing applications that could provide a more complete picture of health status. The retrospective nature of PROs can encourage recall bias in the data.11 Many questions are framed in a manner that requires patients to recall events from the last few days or weeks, such as “how many times in the 7 days have you...” Events and behaviors that are less salient could be difficult to recall, because patients’ experience of the symptom at the time of reporting or recent extreme levels of the symptom might bias the results.12 Patients with cancer also frequently suffer from memory deficits as a result of “chemo brain,” which makes remembering symptom severity an even greater challenge.13 Although patients could use symptom assessment questionnaires like those in PRO tools for real-time tracking, such an approach would require that patients answer the full bank of the tool’s questions, which could be as many as 80 questions10 in length—often covering many more symptoms than any single patient cares to track. Choice ITPA, an interactive tailored patient assessment tool developed in Norway, comes closer to reducing patient burden, since it allows patients to answer tailored questions chosen from 19 problem categories. In our work, we explore further how patients can customize individual real-time metrics for their own needs.
Other researchers use ecological momentary assessment (EMA) methods to analyze cancer-related symptoms. EMA methods involve “the repeated collection of real-time data on participants’ momentary states in the natural environment.”11 Examples include reporting mood after a phone beep, or completing diary entries about stressful situations as they occur. In a study that compared fatigue in ovarian cancer patients undergoing the same treatment, subjects were asked to take up to five randomly timed assessments per day, capturing current fatigue, pain, nausea, trouble concentrating and mood.11 One subject commented that the tool was “fun” and “like a game,” but most others thought that randomly timed assessments felt like interruptions, and questions were a “constant reminder” of cancer. Like PRO tools, EMA methods have generally been designed for use by researchers or as an intervention by clinicians. However, we have deployed strategies that can be used by patients to accurately track symptoms that interest them most. Our goal is to inform the design of real-time tracking tools that can be adopted for use by patients and benefits not only clinicians, but patients themselves.
In contrast to existing PRO and EMA tools designed from the perspective of clinicians and researchers, we design real-time tracking tools from the patient-focused perspective of personal informatics tools—applications and devices that allow users to collect and reflect upon personal information.14 Some personal informatics tools in the consumer market already have capabilities that could be useful for recording cancer symptoms. Mobile tools—such as Tonic (www.tonicselfcare.com)—support flexible, recurring, real-time data capture for a configurable range of symptoms. Also, bathroom scales—such as FitBit’s Aria (www.fitbit.com)—track and automatically record weight, a crucial indicator of progress for some cancer cases. Yet, work remains to be done to facilitate support for the breadth of unanticipated symptoms that patients with cancer experience and to support sharing this data with clinicians. In this work, we deepen our understanding of what patients with cancer want from real-time tracking tools for symptom management.
Use of real-time tracking tools does not appear to be widespread among patients with cancer. A 2009 survey of 134 rural cancer patients and survivors indicated that about one-third tracked symptoms with some tool, such as a notebook or calendar, but we do not know whether tracking took place in the moment.15 Tools used were computer-based in only 12 cases. Questions remain regarding why the majority of patients did not track and reasons motivating those who did track. We have a gap in understanding real-time tracking behaviors that patients with cancer undertake on their own, and not at the behest of researchers or clinicians.
3. Methods
This work is part of a larger project on the personal information management practices of breast cancer patients during treatment. Our analysis of 25 breast cancer patients’ tracking behaviors spanned two smaller studies from the larger project. The purpose of the work presented in this paper is to describe patients’ tracking behaviors as well as the benefits and barriers to tracking health issues during treatment both without and with real-time symptom tracking technology. For the first study, we assessed 15 participants’ natural symptom tracking behaviors during cancer treatment “in the wild,” without access to our real-time tracking tool. For the second study, we investigated tracking behaviors and benefits that emerged when 10 participants used our personal health information management (PHIM) tool—called HealthWeaver—which included real-time tracking features. Our university’s internal review board approved both studies. For both studies, we recruited a convenience sample of local patients with breast cancer. Each participant enrolled in only one study and all were compensated. In this section, we provide details on procedures for each study and our data analysis.
3.1. In-the-wild Study Procedures: Needs Assessment
Our overarching goal for the In-the-wild Study was to understand breast cancer patients’ needs for managing personal health information during treatment. We followed all 15 participants for 6 weeks. Data collection included two 60–90 minutes interviews and observations in the home, an observation of a clinic visit, and two critical incident interviews over the telephone. We audio recorded interviews and documented observations with field notes. We refer to these participants as P1 through P15.
3.2. HealthWeaver Study Procedures: Technology Deployment
Based on findings from the In-the-wild study, we developed a tool called HealthWeaver to help patients manage their personal health information during treatment.16 HealthWeaver consisted of a website and a companion mobile phone application. We conducted 45-minute interviews 3 times over 4 weeks with each of the 10 participants. The initial interview took place before any tool use, while the second and third interviews focused on participants’ use of HealthWeaver for real-time tracking over the study period. We audio recorded interviews and documented observations with field notes. We also collected usage logs from participants’ use of HealthWeaver. We refer to the HealthWeaver study participants as HW-P16 through HW-P25.
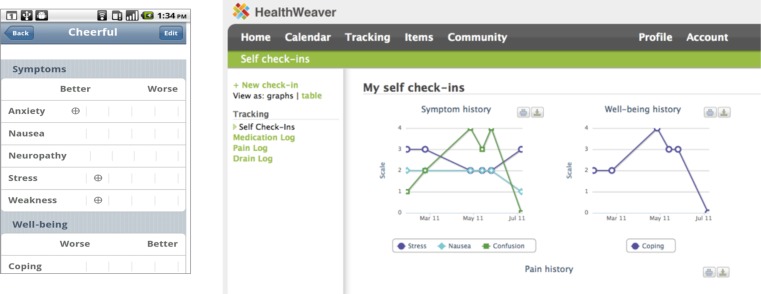
HealthWeaver enables real-time tracking through a ‘self check-in’ feature, a drain log, and a medication intake log. The check-in lets the patient track patient-selected health issues (“metrics”) on a 0 to 4 scale. HealthWeaver presents symptom, well-being, and pain metrics as sliders (see Figure 1 for the mobile interface). HealthWeaver provides a set of default metrics (e.g., nausea, stress, energy, coping) that the user can customize to their situation. The check-in feature enables the user to record her overall state, weight, blood pressure, and minutes of exercise. Users can log check-ins as frequently as they wish and can view graphs of their tracked metrics over time (see Figure 1 for the web interface). The drain log enables users to record drain fluid levels after surgery. Similarly, the medication intake log provided users with a way to log the medications they take. To learn about patients’ experiences using a tracking tool, we asked participants to use HealthWeaver to track at least one health issue, but did not prescribe how often they should track or what issues they should track.
Figure 1.
Health Weaver tracking feature screenshots: mobile check-in entry (left) and web-based tracking history graphing (right)
3.3. Data Analysis
All interviews were transcribed. The first author used open coding17 to identify emergent themes in de-identified transcripts from audiorecordings (P1-P15) and field notes (HW-P16 to HW-P25). The first author coded situations illustrating behavior related to self-tracking and symptom management to illustrate typical self-tracking behaviors, benefits, and barriers, until saturation17 was reached. Other authors who collected the data verified findings in discussions. We examined log data to verify usage patterns reported in interviews during the technology deployment study. During this analysis, we also enumerated the health issues brought up by participants during interviews and clinic visits.
4. Results
In the sections that follow, we describe how participants used self-tracking to manage their care, both without and with a real-time tracking tool. We begin by briefly describing our participants’ demographics and the range of health issues participants experienced compared to the health issues they tracked. We then describe how patients tracked their symptoms “in the wild”—when they did not have access to HealthWeaver or a similar dedicated tracking application. Finally, we discuss how the tracking behaviors differed for patients who were given access to HealthWeaver and the benefits they experienced from using the application.
4.1. Participant demographics
Our participants were all women who varied in age, occupation, and education level. The 15 patients who took part in the “in-the-wild” study ranged in age from 37–73 (mean=53). The 10 patients in the HealthWeaver deployment study ranged in age from 48–68 (mean=58). Treatments among all participants included chemotherapy, radiation therapy, surgery, hormonal therapy, or some combination of these. Among their occupations were grocery store clerk, airline operations employee, homemaker, and a retired biomedical researcher with advanced degrees. One participant described herself as homeless.
4.2. Complex range of symptoms managed
Cancer is a tremendously complex disease with a broad range of symptoms and side effects. Many cancer patients also have comorbidities that further complicate their health. We identified 47 distinct health issues that participants mentioned experiencing during their care (Table 1). These health issues included physical symptoms, psychosocial problems, and vital signs that were out of the normal range. Although tracking such a breadth of health issues posed a significant challenge, a few participants chose to track a subset of these issues with a tool, such as a notebook or calendar. More commonly, participants did not use tools to track symptoms that they had to manage, instead relying on memory.
Table 1.
Health issues experienced by participants (*indicates one or more participants tracked issue with a tool)
| Acid Reflux | Cloudy vision | Fatigue* | Insomnia* | Pain - Back | Sores – Mouth |
| Anemia | Constipation | Fever | Loss of appetite* | Pain - Bone | Sore Throat |
| Anxiety | Dehydration | Hair loss* | Lump size change | Pain - Headache | Swelling - Arm |
| Bloating | Depression | Heart rate | Lymph edema | Pain - Joints | Swelling - Foot |
| Blood count* | Diarrhea | Hives* | Memory deficits | Pain - Leg | Swelling – Seroma* |
| Blood pressure* | Dizziness | Hot flashes* | Migraines | Pain - Mouth | Vaginal tear / dryness |
| Blood sugar* | Drain fluid* | Infection - Bladder | Nausea* | Pain - Stomach | Weight gain / loss* |
| Bruising | Dry cough | Infection - Thumb | Neuropathy | Rash |
4.3. Natural self-tracking behaviors of patients with breast cancer “in the wild”
Patients with breast cancer often deal with a large number of symptoms. Despite the complex nature of symptoms experienced by our participants, their tracking behavior tended to be sporadic and incomplete. In this section, we present data showing that the most common practice was to try to keep track of symptoms by relying on one’s memory, without using any tools at all. We then show that those participants who did use tools to track symptoms often develop their own idiosyncratic, self-devised systems, which were be both cumbersome and incomplete. Finally, we argue that the chief difficulty that patients with cancer face in trying to track is the lack of knowledge about what they should track and how to track. The healthcare system typically offers little support in this regard.
4.3.1. Patients rely on memory to track most health issues
Patients with cancer often experience a great deal of pain, stress, and anxiety, as well as “chemo brain,”—all of which makes it hard for them to concentrate and think clearly.13 In spite of such cognitive difficulties, our participants monitored most health issues by memory. Although participants talked about the importance of writing health information down during visits to make sure no information communicated by clinicians was missed, 17 of 25 participants (68%) did not write down any symptoms that they experienced between clinic visits.
During clinic visits, most participants relied on memory to discuss their symptoms and other health issues that occurred at home. Because the time between visits varied depending on the phase of treatment, participants had to recall the frequency and intensity of health issues that occurred anywhere from a couple of days to months before.
P5’s experience provides an illustrative example of the difficulties patients experience trying to remember their symptoms. P5 and her oncologist were trying to diagnose her irregular heartbeat during a clinic visit. The pulse oximeter test that P5 took the week before indicated an irregular heartbeat, which the oncologist believed happened because P5 was not feeling well. However, P5 could not say for sure that she felt poorly at that time to corroborate the oncologist’s theory. In addition, because P5’s irregular heartbeat was intermittent and they had not yet ordered an ECG, it could have been useful to know what was happening outside of the clinic to determine what events were co-occurring and how P5 felt in general, to see if the irregular heartbeat was due to stress, anemia, or some other reason. Unfortunately, P5 couldn’t offer the oncologist any symptom history data other than the limited information that she remembered.
This incident is characteristic of others that participants experienced, in which patients’ symptoms were challenging to diagnose because they lacked real-time data of those symptoms. Some participants said that it was easy to be inaccurate about how they felt in the past. P11 found that she “loses track of what happened when.” Most participants answered clinicians’ questions about past symptoms at the clinic visit from memory, but the accuracy of these assessments is unknown. Although relying on memory is problematic for patients who experience memory deficits, it is the predominant way that patients with cancer recall symptoms.
4.3.2. Patients devise their own systems using familiar tools when they track
Across both studies, 8 of the 25 participants (32%) tried to track symptoms using some kind of tool—paper or electronic. When patients did use tools to track health issues, they usually appropriated familiar tools used for other purposes, such as notebooks, calendars, and Microsoft Word documents, few of which were intended to be used to systematically track health issues in real-time.
For a small number of highly proactive participants who tracked health issues, tracking was a time-consuming activity. These participants devised their own tracking systems. For example, prior to her use of HealthWeaver, HW-P21 was in the habit of spending significant time aggregating her data from a paper-based journal where she tracked side effects, sleep, vitamins, food intake, medications, exercise, and blood sugars for diabetes. On a weekly basis, she transferred the data to Microsoft Word. When she had a clinic appointment, she typed up 4–6 page summaries of the data for her doctor. Although she estimated this effort taking 4 to 8 hours, HW-P21 found the task important enough to do “because I feel like the more information they [doctors] have, the better off I am going to be.” She had always taken this detailed tracking approach, starting with her diabetes. HW-P21 valued informing clinicians accurately about her symptom history enough to continue this time-intensive, self-devised tracking system over the long term. Yet HW-P21 was unusual in the thoroughness of her tracking practice.
Other participants who valued self-tracking had suboptimal systems in place and did not always know how to improve them. For HW-P17, before she had access to HealthWeaver, her partner undertook tracking on her behalf by recording HW-P17’s health issues in a Microsoft Word document “of the size that would frighten the [Microsoft] Word team.” The partner asked her how she was doing and noted when she complained. HW-P17 described her partner’s process and its limitations:
“After I haven’t been complaining about something for a week, she’ll ask ‘are you still having this’ so she can draw out a pretty clear picture of when things started and stopped, but I don’t know….There is no particular thing to remind her [the partner] that four days in a row I complained about X and on the fifth I didn’t.”
HW-P17’s partner had to read back through the document every so often to prevent issues from slipping through the cracks. HW-P17 and her partner’s tracking system worked well enough to assess how HW-P17 had been doing recently. But her partner had to parse a large electronic document to recall HW-P17’s historical health issues, searching for specific terms that may have been called something else earlier.
The self-devised tracking systems of other participants were more fragmented and sporadic. P2, a diabetic going through treatment for a recurrence of breast cancer, strove to collect all her health information in one three-ring binder (Figure 2) and jot down issues as they came up in her black notebook beside her bed. But in practice she ended up tracking in many locations. She had a spreadsheet on her hard drive in which she sporadically recorded insulin levels, a health issue tracking diary in a LiveStrong handbook (Figure 2), and a Patient Orientation Guide where she recorded her blood pressure in chart format. P2 wanted to but had not yet begun using the LiveStrong diary. Some of these artifacts were at her mother’s house and others at her significant other’s house, limiting easy access to her tracking system. P2 was motivated to track and had some structured tracking tools at her disposal; yet she still had trouble consistently collecting all the data in one accessible place.
Figure 2.
Self-devised tracking tools used by P2: medication list in binder (left) and LiveStrong diary (right).
Another participant, P3, had a calendar that she sometimes used to jot down dates of symptom occurrences (e.g., hair loss) and a journal notebook where she recorded symptom information in narrative form alongside other observations about her life. For many participants like P2 and P3, such fragmentation of previously tracked data made it difficult to reflect upon how they were feeling or to later re-find data when it was needed.
Thus, self-tracking activities of participants who tracked ‘in the wild’ were time-consuming, fragmented, and sporadic. Aggregating the tracked data for reflection remained a challenge for all participants except HW-P21, but her ability to access and reflect on her data came at the cost of a significant time investment in her tracking process.
4.3.3. Patients have little guidance in deciding what and how to track
A major reason why patients have difficulties with tracking is that they are often left to work out for themselves what they need to track and how to track it. With cancer, knowing what to track is particularly difficult because there are so many possible health issues that can arise and some occur unexpectedly. Similarly, lacking tools made to collect tracking data, patients are left to design their own tracking systems, with varying success. For instance, notebooks, Word documents, and health diaries—such as the one used by P2—can easily capture the breadth of symptoms patients deal with. However, reflecting upon data collected in these tools was a challenge that few participants did successfully.
In terms of knowing what to track, clinicians sometimes suggested that patients track specific health issues to gauge likelihood of infection or toxicity. For example, some participants were asked to track surgery drain fluid, blood sugar, or temperature at home. However, patients often experienced many more symptoms than those suggested by clinicians. It was patients themselves who figured out which of these additional symptoms were important and which ones they needed to track systematically.
In terms of knowing how to track, support from the clinicians was even more lacking. Clinicians provided some participants with formatted paper logs for tracking drains, but for most other health issues, patients had to create their own logs on paper or in a spreadsheet. HW-P23 reflected, “Doctors do recommend it to you, but how are you going to do it? It was recommended in the mass amount of the paper you get at the beginning. So you read it later, and they don’t provide the system.” Thus, even when clinicians suggested that participants track particular health issues, this recommendation often came without specific guidance on how to track (e.g., frequency) or was buried in the paperwork that participants took home. As a result, participants devised their own systems with minimal guidance from clinicians.
4.4. Benefits of self-tracking for patients with breast cancer
The deployment of HealthWeaver as a dedicated tracking tool in the second study revealed relatively high usage by participants, and thus exposed key benefits of having access to a tracking tool. Some benefits directly related to the problems that patients experienced when they tracked on their own. First, participants used HealthWeaver frequently because tracking preserved important symptoms and treatment-related events without having to rely on memory. This tracked data allowed patients to see patterns when investigating problematic symptoms and monitor issues surrounding intense health events. Second, using HealthWeaver enabled participants to unify tracking data with other care-related information, making it easier for them to track consistently and to access their tracking history.
Third, because HealthWeaver came with a set of default and optional metrics based on our previous research, our participants had a starting point for figuring out what to track. Finally, regular use of HealthWeaver by participants also uncovered new benefits to tracking, such as better communication with clinicians and psychosocial comfort derived from consistent collection and occasional reflection on the data.
HealthWeaver use was more popular than anticipated. When an easy-to-use tracking system was available to them, participants used it more than was required for study participation. Participants were only required to track 1 health issue, but ended up tracking an average of 8.8 metrics. HealthWeaver was set up with 4 default metrics and a dozen other metrics were available for them to choose from. If participants wanted to create their own custom metrics, they could do so by customizing the tool’s settings. Four out of the 10 participants who used HealthWeaver created their own custom metrics to track health issues, including “did all stretches”, “surgical discomfort”, and “knee pain.” Some participants even employed workarounds to generate new custom metrics in units that weren’t initially supported by HealthWeaver. For example “took all pills” was a well-being parameter that one participant created on the 0–4 scale, because she preferred using check-ins over the medications log feature. These participants actively made their own decisions about what was most useful to track and varied greatly in what they chose to track in HealthWeaver.
Patients appreciated having tracking data and information related to their cancer care unified. HW-P18 thought that having information such as her health calendar, clinical contacts, and tracking data “all in one place, without shuffling any papers” was very important. HW-P21 agreed: “I definitely feel more empowered. Instead of having 50 pieces of paper all over, I have it all right in front of me.” Rather than tracking on a standalone device disconnected from the rest of the cancer care experience, patients were able to use HealthWeaver to track symptoms and manage other care-related information in one place. The unification of data made it easier for patients to collect all the information they needed to share with clinicians during appointments and to feel confident they could find a piece of care related information when they needed it.
4.4.1. Patients use a tracking tool to reflect on patterns and overcome memory deficits
When patients tracked data in HealthWeaver, they could reflect on symptom patterns. The tracked data provided better answers than relying on memory alone, because the check-in graphs provided an interactive, visual representation of the historical data that facilitated pattern finding. Five HealthWeaver study participants explicitly stated how useful the tool was for capturing and graphing symptoms to understand and problem solve health issues.
For example, HW-P19 thought surgery was a major enough event that she decided to undertake tracking. Tracking pain after surgery helped her figure out that she developed an infection. “So I was able to look back and see, I wasn’t feeling this bad, what’s going on now?” After her post-surgical drains were taken out, fluid was not being absorbed, causing swelling. HW-P19 was able to see the relationship between her post-surgical pain and when the swelling developed. When she visited her clinician, she confirmed that the cause of her pain was a seroma, a common side effect of surgery, as she had suspected. Given her newfound understanding of her symptoms, HW-P19 said she thought the check-in graphs were the most valuable HealthWeaver feature.
Another participant, HW-P23, tracked her symptoms during radiation therapy. She knew extreme fatigue was a common side effect of radiation, but she often had insomnia as well. She started tracking sleep and fatigue to see if they were related: “How am I gonna figure out what [the fatigue] related to, but if I put down did I have a bad night or not, then I can see it’s pretty clearly related to that [sleeplessness] rather than radiation.” Although she said she suspected it before, “it was more black and white there [on the HealthWeaver graph], so that was useful.”
4.4.2. Patients use tracking to support communication with clinicians
Regular tracking with HealthWeaver enabled participants to recall symptoms during clinic visits and discuss specific health issues with clinicians. With HealthWeaver, participants were able to capture symptoms and their intensity on a regular basis close to the time that the symptom occurred. Thus, they could provide a more accurate picture of their symptom history to their clinicians. In one case, HW-P17 had an appointment with the oncologist coming up, so she had been trying to carefully monitor her symptoms. Because she was in a 2-week break from chemo, her symptoms had changed and she wanted to accurately recall these changes. HealthWeaver enabled her to share her symptoms with her doctor. Also, having a concrete tracking history of a particularly troublesome symptom—hip pain—helped her clinician address it more readily:
“It was very useful for me to be able to lay out what was going on to my doctor, to show this is what’s happening. I was able to show her that my hip was getting worse over time and that she should take it a little more seriously, [given] the fact I had it [tracked data] for day after day after day and I could show her what was going on.”
HW-P23 also thought tracking would be beneficial for supporting communication with her doctor, especially because her clinic visits were often weeks apart, and without a tool, she could not accurately answer her doctor’s questions about how she had been doing. In addition, HW-P18 pointed out that having access to HealthWeaver on the mobile phone was particularly valuable to her during clinic visits. This access increased her confidence that she could answer any question the clinician might ask because she could easily look up the information she was asked about.
In summary, HealthWeaver’s tracking system supported communication with clinicians in three ways: enabling patients to keep accurate and concrete data about their symptoms, helping them preserve symptom history over long periods of time, and giving patients confidence that they can accurately answer clinicians’ questions during appointments even if they had not prepared the needed information in advance.
4.4.3. Patients take psychosocial comfort in regular tracking
Finally, even when patients are not looking to resolve specific health issues, they still seem to derive psychosocial benefits from using tracking tools. HW-P17 described herself as uninterested in technology, to the point of being the last person she knew to get a cell phone and email address. Yet, HW-P17 found tracking in HealthWeaver helpful for her emotional wellbeing, specifically by reminding herself that she still had positive moments when things were going poorly. She relayed the benefit she saw in tracking:
“This might be really goofy, but adding something good that happened, any good news, might be helpful to go back and remember that there have been improvements [good things happening]. I usually summarize, so you can look over the last couple of weeks ad see how things are going…Day to day it doesn’t look like much has changed but then you look back after a couple of weeks and you see, ‘oh cool, there has actually been an improvement, or even it’s getting worse, you know you need to push it. Being encouraged to log every day and be able to see a summary of those logs isn’t the part I would have thought would be the coolest, but really has been the part I relied on the most.”
HW-P23 also found herself relying on HealthWeaver’s tracking features to capture how she was feeling. She liked the journal and used it to track her exercise as well as to record experiences—the “ups and downs” of cancer:
“If I had it for the whole year, it would have been really useful. It was a roller coaster, overwhelming at times, from the beginning. Tracking helps with that, with the ups and downs.”
Cancer treatment is a psychologically difficult experience, and one benefit of tracking could be to just make visible the positive moments interspersed with their challenging moments. For patients dealing with a life threatening illness, this awareness of the good aspects of their lives could serve as an important source of comfort.
5. Discussion
As a technology probe, HealthWeaver exposed how patients’ tracking behaviors differed when they did or did not have access to a real-time tracking tool. Our research team designed HealthWeaver with a minimal preconception of how the tracking feature should work, yet use of HealthWeaver overcame natural barriers that patients encountered trying to track symptoms on their own. Almost all HealthWeaver users were motivated enough to engage in more self-tracking than required, which helped uncover benefits they had not discovered before. No participants said that tracking constantly reminded them of cancer, as the ovarian cancer patients did after being alerted to log metrics with an EMA tool.11
Our findings suggest that while tracking is very difficult to initiate and undertake on one’s own, doing so with a well-designed tool could be more beneficial than expected. Designing real-time tracking tools for patients with cancer comes with its own set of challenges. Even though HealthWeaver was engaging, it still required a great deal of effort for users to track. HealthWeaver users were also limited in the scales that they could use and were more likely to enter check-ins on a daily basis rather than in real time as symptoms occur. Tracking symptoms in the moment, or even on a daily basis, requires patients to decide what to track from the many symptoms they experience while also being engaged enough with the tool to follow through with tracking symptoms as they occur. Ideally, real-time tracking tools would capture the following: variability of symptoms, mood states, or behaviors over time; cyclical patterns; and co-occurrence of symptoms, environmental conditions, and psychological states.11
Given our knowledge of what real-time tracking tools could capture and our understanding of HealthWeaver use among patients with breast cancer, we suggest the following 5 implications for the design of future tracking tools:.
Pre-seed metrics based on diagnosis and treatment. Without access to HealthWeaver, participants received little guidance on what to track. Profiling individual patients based on their diagnosis and treatment plan would provide some guidance to patients who do not know what symptoms to look for during cancer treatment. Personalized default symptom metrics—based on diagnosis and treatment profile—could be supplemented with optional metrics from a list that covers the breadth of symptoms that patients experience.
Enable customization for symptoms. HealthWeaver allowed participants to customize which symptoms to track and name the symptom terms themselves. Users could define new symptoms that they have a personal interest in monitoring instead of just choosing among the many already provided in HealthWeaver. This feature allowed patients to further personalize the tracking tool to meet their own needs. For example, HW-P17, the patient with hip pain, could track that symptom, even though it is not a typical symptom of patients with breast cancer.
Maximize benefits for patients by supporting reflection and communication with clinicians. In HealthWeaver, users have the ability to choose metrics to overlay in graphs and see co-occurrences of symptoms or other patterns. We found evidence that patients prefer tools that support this type of functionality. Previous focus group findings from Norway suggest that patients wish to engage in reflection upon the data that they enter in PRO tools available to them at home.0 Supporting reflection by patients, and not just clinicians, is one step closer to personal informatics tools that provide individuals with transparent ways to use the data that they collect. Patients need to be able to understand what the data collected means to find use of a tracking tool worthwhile, especially if clinicians are not always reviewing the tracked data. Patients also need the option to review the data with clinicians when it is hard to determine what action should be taken on one’s own.
-
Create intuitive multimodal interfaces. Participants found value in accessing tracking data along with the calendar and notes in one place, which made their cancer-related information less fragmented. The positive aesthetic of the interface combined with the usefulness of HealthWeaver features likely made the tool engaging enough to drive consistent tracking even with the effort required to enter check-in entries and log medications.
To decrease the effort tracking takes, future tools should take a multimodal approach. HealthWeaver’s mobile interface facilitated convenient data entry in the moment. Future mobile applications could also enable voice-based data entry with voice recognition to allow patients to record symptoms or annotate individual check-ins with more detailed contextual information.
Give patients ownership over tracking data. Patients valued ownership over their data in HealthWeaver since they had greater freedom to express what mattered to them. They did not necessarily need or want to share everything with clinicians or caregivers. Some patients, such as HW-P17, specified sharing was helpful but not necessary to find value in tracking. With control over who could see what data, patients could record sensitive issues, but only share selected issues. In contrast, for most PRO tools or interactive tailored patient assessments, the clinic or research team—not the patient—drives PRO tool use and clinicians see all the data.
In summary, patients need to remain engaged and aware to manage symptoms that emerge during outpatient treatment. Real-time tracking is a self-care activity that could engage patients in becoming aware of what they need to manage symptoms at home and how to communicate their needs to clinicians.
6. Conclusion
People with cancer experience a broad range of symptoms during treatment, yet they do not always see the benefits of real-time tracking. In the wild, participants rarely invested time in the tracking process, and those who did typically made do with fragmented and sporadic self-devised systems. All but one participant were not aware of the benefits of self-tracking prior to participating in the study using HealthWeaver. With HealthWeaver, participants augmented their memories, supported communication with clinicians, and derived psychosocial comfort from tracking. We found that HealthWeaver motivated our participants sufficiently to take the effort to track symptoms due to its customizable metrics and opportunities it provided patients for reflection—with and without clinicians. Further investigation into the cancer diagnoses, stages, and treatments that can best be served by real-time tracking—and how to ensure that well-designed tools are accessible and used—will help patients realize their full benefit during cancer treatment. When carefully designed, such tools could help patients to better manage their treatment, communicate with their providers, and maintain control over their care and their lives.
Table 2.
Summary of key findings and related implications
| Summarized findings | Implication from HealthWeaver tracking feature use |
|---|---|
| In-the-wild: barriers to tracking | |
| Limited clinical guidance | Pre-populated metrics helped patients decide what to track. |
| Fragmentation of data | Patient preferred unified information on cancer care in one system. |
| Time & energy burden | Multimodal data entry. |
|
| |
| With HealthWeaver: benefits to tracking | |
| Augmented memory | Patients did their own reflection and customized metrics to remember trends. |
| Psychosocial comfort | Patients owned the tracking process and took comfort in routine. |
| Communication support with clinicians | Patients could show tracking data to clinicians and help prioritize symptoms. |
Acknowledgments
We would like to thank all participants and funding sources (NLM #5T15LM007442-09, NIH #R01LM009143)
References
- 1.Newell S, Sanson-Fisher RW, Girgis A, et al. How well do medical oncologists’ perceptions reflect their patients’ reported physical and psychosocial problems? Data from a survey of five oncologists. Cancer. 1998;83:1640e51. [PubMed] [Google Scholar]
- 2.Meuser T, Pietruck C, Radbruch L, Stute P, Lehmann KA, Grond S. Symptoms during cancer pain treatment following WHO-guidelines: a longitudinal follow-up study of symptom prevalence, severity and etiology. Pain. 2001;93:246–57. doi: 10.1016/S0304-3959(01)00324-4. [DOI] [PubMed] [Google Scholar]
- 3.Barsevick AM, Dudley WN, Beck SL. Cancer-related fatigue, depressive symptoms, and functional status: a mediation model. Nurs Res. 2006;55:366–72. doi: 10.1097/00006199-200609000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Jacobsen R, Liubarskene Z, Moeldrup C, Christrup L, Sjugren P, Samsanaviciene J. Barriers to cancer pain management: a review of empirical research. Medicina. 2009;45(6):427–33. [PubMed] [Google Scholar]
- 5.Hutchinson H, Mackay W, Westerlund B, Bederson BB, Druin A, Plaisant C, et al. Technology probes: inspiring design for and with families. Proc of CHI ’03. 2003:17–24. [Google Scholar]
- 6.Wilde MH, Garvin S. A concept analysis of self-monitoring. J Adv Nurs. 2007;57(3):339–50. doi: 10.1111/j.1365-2648.2006.04089.x. [DOI] [PubMed] [Google Scholar]
- 7.Basch E, Iasonos A, Barz A, Culkin A, Kris MG, Artz D, et al. Long-term toxicity monitoring via electronic patient-reported outcomes in patients receiving chemotherapy. J Clin Oncol. 2007b;25(34):5374–80. doi: 10.1200/JCO.2007.11.2243. [DOI] [PubMed] [Google Scholar]
- 8.Berry DL, Blumenstein BA, Halpenny B, Wolpin S, Fann JR, Austin-Seymour M, et al. Enhancing patient-provider communication with the Electronic Self-report Assessment for Cancer: A randomized trial. J Clin Oncol. 2011;2011;29(8):1029–35. doi: 10.1200/JCO.2010.30.3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruland CM, Jeneson A, Andersen, Andersen R, Slaughter L, Schjoedt-Osmo B, et al. AMIA Annu Symp Proc; 2007. pp. 635–639. [PMC free article] [PubMed] [Google Scholar]
- 10.Abernethy AP, Zafar SY, Uronis H, Wheeler JL, Coan A, Rowe K, et al. Validation of the Patient Care Monitor 2.0: a review of system assessment instrument for cancer patients. J Pain Symptom Manage. 2010;40(4):545–58. doi: 10.1016/j.jpainsymman.2010.01.017. [DOI] [PubMed] [Google Scholar]
- 11.Stone AA, Shiffman S, Atienza AA, Nebeling L. The science of real-time data capture. New York: Oxford University Press; 2007. [Google Scholar]
- 12.Redelmeier DA, Kahneman A. Patients’ memories of painful medical treatments: real-time and retrospective evaluations of two minimally invasive procedures. Pain. 1996;66(1):3–8. doi: 10.1016/0304-3959(96)02994-6. [DOI] [PubMed] [Google Scholar]
- 13.Boykoff N, Moieni M, Subramanian SK. Confronting chemo brain: an in-depth look at survivors’ reports of impact on work, social networks, and health care response. J Cancer Surviv. 2009;3(4):223–32. doi: 10.1007/s11764-009-0098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li I, Dey A, Forlizzi J. A stage-based model of personal informatics systems. Proc of ACM Computer-Human Interaction Conference ‘10; 2010. pp. 557–66. [Google Scholar]
- 15.Hermansen-Kobulnicky CJ. Symptom-monitoring behaviors of rural cancer patients and survivors. Support Care Cancer. 2009;17(6):617–26. doi: 10.1007/s00520-008-0552-8. [DOI] [PubMed] [Google Scholar]
- 16.Klasnja P, Hartzler A, Powell C, Phan G, Pratt W. HealthWeaver Mobile: Designing a mobile tool for managing personal health information during cancer care. AMIA Annu Symp Proc; 2010. pp. 392–6. [PMC free article] [PubMed] [Google Scholar]
- 17.Strauss A, Corbin J. Basics of Qualitative Research. 2nd Ed. London: Sage Publications; 1998. [Google Scholar]
- 18.Ruland CM, Jeneson A, Andersen, Andersen R, Slaughter L, Schjoedt-Osmo B, et al. Designing tailored Internet support to assist cancer patients in illness management. AMIA Annu Symp Proc; 2007. pp. 635–9. [PMC free article] [PubMed] [Google Scholar]