Abstract
Notifying ambulatory providers when their patients visit the hospital is a simple concept but potentially a powerful tool for improving care coordination. A health information exchange (HIE) can provide automatic notifications to its members by building services on top of their existing infrastructure. NYCLIX, Inc., a functioning HIE in New York City, has developed a system that detects hospital admissions, discharges and emergency department visits and notifies their providers. The system has been in use since November 2010. Out of 63,305 patients enrolled 6,913 (11%) had one or more events in the study period and on average there were 238 events per day. While event notifications have a clinical value, their use also involves non-clinical care coordination; new workflows should be designed to incorporate a broader care team in their use. This paper describes the user requirements for the notification system, system design, current status, lessons learned and future directions.
I. Background
Clinical data is a vital tool for taking care of patients whether the caregiver is a physician, nurse, social worker, care manager or other care provider. Ideally, the primary caregiver would know about things happening to their patients outside of their immediate care [1,2]. For example, a primary care physician (PCP) caring for a patient with congestive heart failure should to be informed when her patient visits the emergency department so that she can either provide useful information to the emergency physician or follow-up with the patient to ensure that there is an appropriate treatment plan. If that same patient was being cared for by a visiting nurse, the nurse should be notified that the patient is in the emergency department in order to (a) avoid a costly visit to an empty home and (b) make appropriate changes to the home care plan. A health plan that covers this patient’s care may provide care management services such as care coordination through collaboration with the patient, the PCP, emergency physician and other ancillary providers in response to learning about the emergency department visit.
A regional health information organization (RHIO) often includes the infrastructure needed to detect events of interest and notify the relevant provider. This paper describes the design, development and implementation of an event detection and notification service developed by NYCLIX, Inc., (New York Clinical Information Exchange). This service was developed and piloted with a group of providers because of a belief that the event notifications would help them to improve care and efficiency in health care delivery. We describe the environment in which the system was developed, user requirements for the system, the system architecture, current state (including usage data to data), lessons learned and future directions.
II. Clinical Setting and Overview of the Health Information Exchange
NYCLIX is a network of health care organizations in New York City including major medical centers, primary care physicians, a home health care agency, long-term care facilities and a Medicaid managed care plan. The RHIO establishes an organizational structure for trusted exchange of clinical information and a technical infrastructure that allows the information to be captured and transmitted electronically.
In the NYCLIX RHIO, which began accumulating data in October 2009, there were approximately 4.6 million patients as of December 2011 and 552,133 patients or 11.9% of the total had been to more than one site (Table I).
Table I.
Numbers of patients who have been to more than one NYCLIX participant as of December 2011
| Number of Sites Visited | Number of Patients |
|---|---|
| 2 | 438,024 |
| 3 | 89,022 |
| 4 | 19,465 |
| 5 | 43,66 |
| 6 | 908 |
| 7 | 235 |
| 8 | 73 |
| 9 | 25 |
| 10 | 11 |
| 11 | 3 |
| 12 | 1 |
| Total | 552,133 |
The NYCLIX health information exchange (HIE) uses a federated architecture in which the clinical repository is spread over a collection of “edge servers” that reside in each of the members’ data centers. The edge servers are logically connected by an application that resides at the NYCLIX hub along with a central master patient index (MPI) and record locator service. The edge servers collect registration information, allergies, diagnoses, procedures, lab results, reports (radiology, pathology, cardiology, endoscopy, EKG), medications, discharge summaries, immunizations and vital signs. This information can be viewed by qualified clinical users through a stand-alone portal, which was first piloted in emergency departments (EDs) in late 2009.
There are two components of the NYCLIX system that are prerequisites for the event detection and notification service. The first is the data feeds that all members send to NYCLIX providing details on every patient encounter. These messages (part of a standard HL7 ADT) typically include the patient demographics, visit/discharge dates, diagnosis or reason for visit and the clinician providing treatment. The second component is the MPI which takes the demographic information about patients from different sources and performs a probabilistic match to determine if it is the same person. The specific role of these components in event detection and notification service is described below.
A. Privacy Considerations
In New York State, the Department of Health has created privacy recommendation for RHIOs. Under these recommendations, a provider organization is allowed to access a patient’s data via a RHIO only if the patient has given written affirmative consent. However, a RHIO may be used to transmit clinical data between organizations without the patient’s affirmative consent if the transmission is a “one-to-one” communication that would be allowed under existing state and federal privacy law (e.g. a request for a referral between two individual providers). Notifications about hospital visits and discharges are communicated to a relevant caregiver under the one-to-one provision. Notification messages provide the patients name, date of service and location but do not contain other clinical data.
Once a caregiver has received a notification from NYCLIX about an encounter, he or she may want to learn more about the details of the encounter so that they can take appropriate action. A patient’s affirmative consent is required before the provider can obtain additional clinical data through the NYCLIX portal.
III. Requirements / Use Cases
The event detection and notification service was developed in response to requests from NYCLIX participants. All of the use cases are focused on informing certain NYCLIX members about hospital ED visits, inpatient admissions and discharges. These notifications allow recipients to consult with patients and collaborate with colleagues to improve coordination. In each case the requests were made with the belief that these notifications would allow caregivers to improve the quality and efficiency of the care that they provide.
A. Deliver notifications to PCPs when their patients are admitted to or discharged from the hospital
The Institute for Family Health (IFH) is a Federally Qualified Health Center (FQHC) operating approximately 22 clinics in New York City and the Hudson Valley. IFH has received Level 3 Patient Centered Medical Home (PCMH) certification and has several programs designed to improve care coordination.[3]
From a workflow perspective, the primary care physicians at IFH asked to receive a notification in the form of a message in their electronic medical record (EMR) when one of their patients visits the ED or is admitted or discharged from an area hospital. Clinicians at IFH asked for the notification to include the patient name and ID, the type of encounter, name of the hospital and the date. For convenience, clinicians also asked for a link to the NYCLIX portal in the notification so that the PCP can more easily access the information and learn about the details of the encounter.
B. Deliver notifications to home health service when active patients are admitted to or discharged from the hospital
The Visiting Nurse Service of New York (VNSNY), the largest home health agency in the country, provides a diversity of home health care services throughout New York City, Long Island and Westchester County. VNSNY strives to leverage technology for effective and efficient care delivery: for example, nurses in the field are able to communicate with the central office using tablet computers and supporting applications.
VNSNY has chosen to implement The NYCLIX event detection and notification service as another application of technology to improve the efficiency and quality of care. Visiting nurses wish to be informed in the event that their patient has been taken to the ED in order to avoid a wasted trip to an empty home. In addition, VNSNY needs to know when their patients are discharged to better enable them to coordinate care with the hospital and avoid an unnecessary re-admission. VNSNY has asked that all notifications be sent to their Customer Care Center which takes care of routing the message to the appropriate care team. The care team then receives an alert in the EMR on their tablet and can access the notification directly. Anyone on the team can update the alert to indicate that it has been read. The notification becomes a permanent part of the chart documentation.
C. Deliver notifications to health plan when active members are admitted to or discharged from the hospital
SelectHealth is a Medicaid Special Needs Plan (SNP) focused on managing the care of people living with HIV and AIDS. SelectHealth’s mission is to increase member access to high quality sub-specialty care while effectively managing HIV through specialist PCPs with the goal of improving the health of its members, providing a better care experience and controlling per capita costs.
SelectHealth has loaded notifications into their member management system to send alerts to their Medical Director and nursing staff. SelectHealth works closely with their members’ PCPs and uses these notifications as a new tool to improve the coordination of care. For example, a SelectHealth nurse care manager may receive a notification of an ED visit by one of their members and contact the PCP who may not have otherwise been aware of the encounter. This allows timely follow-up and could prevent readmissions or other complications.
IV. System Design
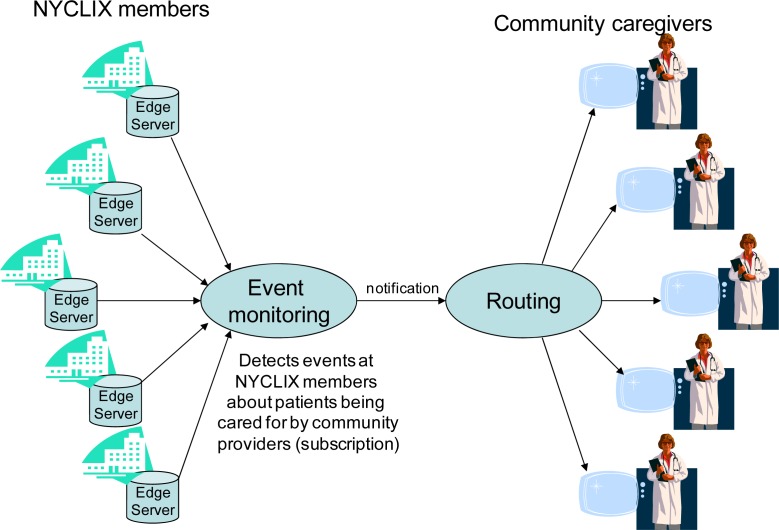
The event detection and notification service consists of two major functions: event monitoring and routing. Event monitoring detects the occurrence of a hospital visit, admission or discharge for a set of patients (“subscriptions”). Routing delivers a notification about that encounter to the appropriate provider (“subscriber”).
A. Event monitoring
Event monitoring consists of two components: subscriptions and detection. Subscriptions identify what patients are to be monitored in the system. The criteria for subscriptions varies with each use case. Examples may include:
Patients in a diabetes registry
Patients who have been seen by a given PCP (subscriber) at a primary care clinic within the past year
Patients who are actively receiving home care
Patients who are active members of a managed care plan
Patients manually chosen by a provider (subscriber)
Subscriptions are stored in a database table that contains the patients’ RHIO enterprise ID (EID) from the MPI and the subscriber. The EID enables the system to match the patient in the subscription to an encounter at any facility in the RHIO. Events are detected by using the subscriptions to check each ED visit, hospital admission or discharge to determine if there is a match in the table. When an event has been detected, a simple notification message is prepared. The notification message contains the patient name and medical record number at the subscribing organization, the location and type of encounter (ED visit, inpatient admission or discharge), date and time of the event, the patient’s consent status and a link to the NYCLIX Clinical Portal for additional clinical history and details about the encounter.
B. Routing
Once an event has been detected and a notification message has been created it must be delivered securely to the subscriber. In all instances the notification is sent in the form of an HL7 message via a secure virtual private network (VPN) established between NYCLIX and the subscribing organization. There are several approaches to delivering the notification to the appropriate provider once it has reached the subscribing organization.
NYCLIX routes to a specific provider – The notification message may contain the provider’s ID which can be used by the subscribing organization’s EMR to route the message to their secure inbox. This approach requires the subscribing organization or the individual subscribers to maintain an accurate and up-to-date patient-provider relationship in their subscriptions with NYCLIX.
NYCLIX routes to the organization – The patient MRN in the notification message is used by the subscribing organization to determine the appropriate provider to receive the message at the time the message is received. This approach allows the subscriber to leverage an existing internal record of patient-provider relationships. In some situations, such as home care, the patient-provider relationship can change frequently and it is most practical for the organization to take responsibility for routing messages to the appropriate provider.
Notification is stored as an encounter in the EMR – In one case, the subscribing organization used the notification to create an encounter in the patient’s record in addition to routing the message to the provider. This approach enables other providers in the organization who do not receive the notification to see a record of these hospital visits in their encounter history. This also quickly highlights patterns such as frequent ED use.
V. Data Analysis
For this study, the application was used to create subscriptions and detect events at all three facilities between November 1, 2010 and April 30, 2011. As described in the System Design section above, subscriptions are created based on various criteria and compared with visit data from each of the hospitals to detect events (ED visits, inpatient admissions and discharges). The event data captured includes the patient ID, the facility visited, the date-time of the event and the type of encounter (emergency, inpatient admission or discharge). These data were used to perform the following analyses:
Number of events by category and site
Total and average events per day over the six-month study period
Frequency of events types: emergency, inpatient admissions and discharges
Incidence of a single patient visiting multiple sites (and specifically EDs)
Incidence of patients transferring from ED to inpatient as part of a single encounter
A. Event Rates
A total of 63,305 patients were enrolled in the service during the study period, November 2010 thru April 2011, and a total of 42,918 events were detected. On average 238 events were reported per day across the three facilities.
The volume of events varied significantly across use cases. SelectHealth with an enrollment of 3,748 patients generated an average of 13 notifications per day while VNSNY with an enrollment of 19,255 generated an average of 143 notifications per day.
But size does not account for the only variation between the sites. IFH has the most patients enrolled in the service 40,302 but VNSNY with half the enrollment had about 1¾ times the number of events.
B. Events per Patient
Of the 63,305 patients enrolled 6,913 had one or more events reported ranging from 1,879 patients with a single event to 623 patients with 10 or more events reported. Of the patients who had an event 37.7% had 4 or more events with a maximum of 96 events reported for a single patient. The average number of events per patient among patients who had events was 7.7 and among all patients enrolled was 0.7.
C. Event Patterns
A substantial number of the patients admitted to hospital start in the ED and are transferred to inpatient on the same or next day (see Table V below). At IFH and SelectHealth approximately a quarter of the patients with events visited the ED and were subsequently admitted to inpatient. At VNSNY it was closer to half.
Table V.
Patients transferring from ED to inpatient and visiting multiple sites
| Indicator | IFH | VNSNY | SelectHealth | |||
|---|---|---|---|---|---|---|
| Patients with events | 2,905 | 3,585 | 458 | |||
| Admitted to inpatient from ED | 1,336 | 24.6% | 4,360 | 51.4% | 225 | 26.9% |
| Visits to multiple sites | 67 | 4.3% | 95 | 4.1% | 9 | 4.2% |
| Visits to multiple EDs | 143 | 3.1% | 147 | 1.9% | 25 | 2.8% |
There are a small but substantial number of patients who visited multiple hospitals and, in particular, multiple EDs in the study period.
VI. Discussion and Lessons Learned
Although IFH, which generally serves a primary care population, had a much higher number of patients enrolled than the other sites, they had fewer events and a lower rate of events per patient than VNSNY, which tends to serve an older, sicker population, and a lower rate of events per patient than SelectHealth, which serves a population living with HIV and AIDS. Also of interest was the observation that VNSNY patients who visited the ED were admitted about twice as often as patients from the other two programs. This may have been due to the fact that the VNSNY patients are referred to the ED after the VNSNY nurse determines a need for hospital services, while patients from SelectHealth and IFH most often self-refer to the ED.
Establishing a health information exchange is an expensive endeavor. Event notifications are a useful extension of his technology that provide additional clinical value from the information that is already being collected with little additional investment. The event notifications provide information to providers about their patients that they may not have otherwise known. This could lead to more timely follow-up visits, consults with other care team members or gathering of additional information about the encounter. Given the volume of notifications and the schedules of many providers it may not be practical to send all notifications directly to a PCP. A more practical workflow might include sending these to a dedicated care manager who can “triage” and involve the PCP as needed. The event detection and notification service provides new and valuable information but also adds a new task to the provider organization’s workflow. Accountable care and the NYS Medicaid Health Homes programs have recognized the value of care coordination and are promoting additional investment in these types of activities.
We have developed and piloted a notification service that extends the capabilities of a functioning health information exchange and increases its value. The notification service detects admissions and ED visits at hospitals in the exchange and notifies physicians and other staff at an ambulatory care organization, a home health agency and a Medicaid managed care organization. Data collected in the over a six-month period present the numbers and types of events detected and illustrate some of the potential utility of such a service.
Event notifications enhance the ability to do care coordination but the addition of this new information service does not account for the additional work that it generates or the appropriate staff to act on these notifications. While it is critical for PCPs to be engaged in coordinating the patients care, managing the new workflow these notifications require may be more appropriate for a care manager or care navigator. A more sensible workflow may have the care manager receiving notifications, gathering additional information and consulting with the PCP as needed. Determining the right timing (urgency) for notifying the PCP of an event is something that will vary and will require the PCP and care managers to develop protocols that take into account clinical and non-clinical circumstances.
A disproportionate number of the events detected came from patients with a high frequency of visits to the ED a significant number of these patients also visited multiple hospitals. It is likely that these patients have the most complex issues and the greatest medical costs [4]. The event detection and notification service could be enhanced to identify patients with these patterns and highlight these individuals and their visit patterns when sending notifications to providers. There are emerging on health care reform programs such as the New York State Medicaid Health Homes that focus on the ability detect patients with high-utilization of the hospital and emergency department services in support of programs designed to intervene in these cases to provide more appropriate, efficient and high quality care. Notifications about individuals with these encounter patterns may be given a higher priority in care coordination activities.
VII. Next Steps
Despite the workflow issues cited above, with the launch of Accountable Care Organizations (ACOs) [5], Patient Centered Medical Homes [6], and Medicaid Health Homes in New York State [7], event notification services are being increasingly requested. Under these programs, most notifications are more likely to be sent first to care managers who will have primary responsibility for reviewing and “triaging” the notifications and then involving PCPs as appropriate.
Other enhancements to under consideration include:
Sending “tickler” notifications to pagers or cell phones (via text message) to prompt recipients to log into the HIE or their EMR for the full message.
Subscription to other events such as selected lab results, prescription fills and appointments
Establishing groups at the receiving end so that notifications can be picked up by multiple subscribers
Including more information in the notification about the encounter such as the admitting diagnosis and patterns of encounters to help identify the high-risk high-utilizer patients
The service will be improved in general by increasing the size of the network to include more providers. The service can only provide notifications on encounters at sites that are part of NYCLIX.
VIII. Conclusion
NYCLIX has leveraged its HIE infrastructure to provide a notification service that alerts primary care doctors, visiting nurses and care managers when their patients have been to the hospital. Primary care doctors have been using the service since November 2010. The service detects about 237 events per day across three participating organizations: ambulatory care clinics, home health agency and Medicaid managed care plan. This paper has described the characteristics of these events over a six month period and may help in planning the infrastructure and workflows required for similar services being developed elsewhere.
Table II.
Events (November 1, 2010 to April 30, 2011)
| Site | Patients Enrolled | ED Visits | Admissions | Discharges | Total Events | Events per day | Events per patient |
|---|---|---|---|---|---|---|---|
| VNS | 19,255 | 7,202 (27.8%) | 13,920 (53.4%) | 4,741 (18.3%) | 25,863 (100%) | 143 | 1.3 |
| IFH | 40,302 | 5,886 (39.8%) | 7,725 (52.2%) | 1,168 (7.9%) | 14,779 (100%) | 82 | 0.4 |
| SelectHealth | 3,748 | 818 (35.9%) | 1,194 (52.5%) | 264 (11.6%) | 2,276 (100%) | 13 | 2.0 |
| Total | 63,305 | 13,906 | 22,839 | 6,173 | 42,918 | 238 | 0.7 |
References
- 1.Brailer DJ. Interoperability: The Key To The Future Health Care System. Health Affairs. 2005:W5.195.21. doi: 10.1377/hlthaff.w5.19. [DOI] [PubMed] [Google Scholar]
- 2.Bourgeois FC, Olson KL, Mandl KD. Patients Treated at Multiple Acute Health Care Facilities. Archives of Internal Medicine. 2010:1989–1995. doi: 10.1001/archinternmed.2010.439. [DOI] [PubMed] [Google Scholar]
- 3.Sinsky CA. The Patient-Centered Medical Home Neighbor: A Primary Care Physician’s View. Annals of Internal Medicine. 2011:61–62. doi: 10.7326/0003-4819-154-1-201101040-00010. [DOI] [PubMed] [Google Scholar]
- 4.Robinson JC, Yegian JM. Medical Management After Managed Care. Health Affairs. 2004:W4.269–W4.280. doi: 10.1377/hlthaff.w4.269. [DOI] [PubMed] [Google Scholar]
- 5.McClellan M, McKethan AN, Lewis JL, et al. A National Strategy to put Accountable Care into Practice. Health Affairs. 2010;29(5):982–990. doi: 10.1377/hlthaff.2010.0194. [DOI] [PubMed] [Google Scholar]
- 6.Rittenhouse DR, Shortell SM. The Patient-Centered Medical Home: Will it Stand the Test of Health Reform? JAMA. 2009;301(19):2038–2040. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
- 7.http://www.health.ny.gov/health_care/medicaid/program/medicaid_health_homes/. Accessed March 14, 2012.