Abstract
Care coordination is at the forefront of current health reform efforts, yet most electronic health records (EHRs) lack the functionality needed to facilitate and document care coordination activities. The Integrated Care Coordination Information System (ICCIS) was iteratively developed with user input to meet these needs. Following 16 months of system use, ICCIS users and developers were interviewed about their experiences. These interviews, along with quantitative information about system use, were analyzed using a combination of Linstone’s Multiple Perspective approach and the ABC framework to determine lessons learned about novel system creation. Overall, clinicians saw value in specialized health information technology (HIT) tools for care coordination as long as development focuses on providing user-requested functionality that integrates closely with existing HIT systems and workflows. Close integration between novel HIT and EHRs may increase use by relieving the cited fatigues of duplicative data entry, multiple system logins, and potential data inconsistencies.
INTRODUCTION
Care Management Plus (CMP) is an established model of care coordination, information technology, and quality improvement adopted by primary care clinics to meet the needs of older adults and patients with complex, chronic diseases.1,2 CMP addresses current gaps in care delivery by training dedicated care managers and facilitating the use of health information technology (HIT) to track care plans, monitor and improve quality, and manage the complex coordination tasks prioritized by the patient and care team. Since its inception in 2001, the CMP team, a collaborative group of physicians, care managers, researchers, and project facilitators, has trained more than 208 primary care teams across the U.S., participated in state and national primary care redesign efforts, and partnered with large healthcare organizations to continuously improve their model.
Experience from the dissemination of CMP led to a deep understanding of the unique tracking and population management needs of care coordinators and of the strong desire from clinicians for appropriate HIT support. Subsequently, the CMP team conducted an extensive user-centered development process to reveal and analyze unknown and undeveloped user requirements.3 As a result, the CMP team developed the Integrated Care Coordination Information System (ICCIS) as a novel HIT tool specifically intended to enable primary care clinics to efficiently and effectively conduct care coordination activities. ICCIS integrates data from an electronic health record (EHR) into a supplemental web-based tool intended to provide improved functionality for care planning, population management, and best practice reminders.
The purpose of this paper is to analyze the lessons learned from building and using ICCIS for care coordination. The analysis evaluates the technical, organizational, and personal perspectives relevant to ICCIS by considering the experiences of both the end-users and development team. This analysis may provide valuable information to others for the further development of novel HIT systems to appropriately address the needs for care coordination and improve the quality of patient care. All authors are members of the CMP team.
BACKGROUND
In the United States, over 133 million people – almost half of all Americans – are living with a chronic condition with an expected increase to 157 million by 2020.4 People with chronic conditions account for 83% of all health care spending, while those individuals with 5 or more chronic conditions account for 68% of all Medicare spending.5 These individuals typically require specialized care from multiple care providers and visit up to 16 different physicians each year.6 Care coordination is needed to share information among providers, provide a unified care plan to the patient, and avoid costly adverse events and redundancies in care. The duty of care coordination frequently falls to the patient’s primary care team where the demands associated with care coordination can be daunting. Besides tracking and coordinating care coordination activities, complex alerts are needed to remind clinicians to provide appropriate, evidence-based care to patients in a timely fashion. These fundamental care coordination activities are not adequately addressed in current care delivery models or HIT and are largely not reimbursed by insurers.
For seniors with complex needs in 7 primary care clinics in Utah, CMP reduced overall mortality by 20%, hospitalizations by 24%, and complications due to diabetes by 15–25%.1,7 Significant savings were realized from these care improvements – up to $274,000 per clinic for Medicare.1 Providers who referred patients to CMP experienced an 8–12% productivity increase compared to those who did not refer patients.8 While the CMP program demonstrated the benefits of care coordination, clinicians indicated a clear desire for more effective HIT tools that integrated closely with their care coordination workflow. For this reason, an extensive user-centered development process utilized structured surveys and semi-structured interviews of numerous clinicians to determine the most critical and highly desired features in such HIT tools.1
With this knowledge, the core functions of ICCIS were developed to facilitate the care management workflow – to create encounters, record care activities, receive reminders, review patient history, complete assessments, and set goals. The encounter form allows a care manager to create and track any type of encounter, from office visit to email, with the patient, family, or other caregivers. The tickler is a centralized reminder list of tasks and communications that are proactively planned, but incomplete, which allows population-based tasks to be merged with individual encounter tasks into one easy-to-use, actionable list. The patient worksheet summarizes important data a clinician may need to review before seeing a patient, including active diagnoses, medications, patient goals, referrals, appropriate assessments, and recommended care tasks. Advanced reporting is available to review care management activities and assess trends in the health of a clinic’s patient population. A high risk patient list report provides a means to quickly track and enroll high risk clinic patients in care management. ICCIS’s quality measure reports display the clinic’s adherence to 27 quality measures with statistically significant trends and can be run by clinic, by team, or by individual physician. ICCIS is able to track and report on detailed aspects of patient care due to specialized documentation. Current EHRs have difficulty capturing these aspects of patient care in such detail, which is critical in the ability to develop advanced, actionable reports for clinicians. The intended users of ICCIS were primarily physicians and care managers but some functionality could be used by clinic managers as well.
ICCIS was originally implemented in six clinics in Oregon where extensive training in care management was provided by the CMP team. These primary care clinics included over 30 physicians, 17 non-physician clinicians, and approximately 59,000 active patients in practice. The majority of these clinics were rural-based practices, not affiliated with any health systems or academic medical settings. These clinics also played a central role in the initial development process of ICCIS. ICCIS was then utilized to monitor the clinics and study the impact of incentives on care coordination and quality improvement activities within each clinic. The clinics were randomized to receive pay-for-performance incentives for quality improvement or fee-for-service payments for care coordination activities, which may have impacted how each clinic utilized ICCIS. The clinics enrolled 4,043 patients in care management over the sixteen month study period and are able to offer extensive feedback based on their use of ICCIS. Specifically, the clinics were able to provide insight into the implementation, utilization, and maintenance of ICCIS as a specialized HIT tool for care coordination.
METHODS
Extensive research was done to understand methodologies used to systematically analyze the development and implementation of various HIT tools. When evaluating technology, the impact from the technical perspective is typically easier to conceptualize, but understanding the organizational impact is more complex. The desire was to find a methodology that considered both the technical perspective but gave equal consideration to the impact this tool may have on a whole clinic or an individual clinician’s workflow when caring for patients.
Linstone’s Multiple Perspective approach augments the technical perspective with both organizational and personal perspectives. To further understand these distinct perspectives, the technical perspective focuses on structural and functional aspects of a system being analyzed; the organizational perspective on policy, procedure, and interpersonal aspects; and the personal perspective on process and outcomes. Linstone specifically developed this approach “to help the systems practitioner bridge the gap between analysis and action, between model and real world”.9 Each perspective has separate underlying assumptions and is essential to understanding complex technical systems that are meant to interact with a group of people.
A framework to assess and compare information system usage in collaborative care divides necessary functions into three categories of providing Access to information, supporting Best practices, and facilitating Communication (ABC).10 The ABC framework was developed largely due to a lack of support for team-based chronic illness care among previous EHR standards, although nationwide programs, such as the Meaningful Use incentive program and National Committee for Quality Assurance’s patient-centered medical home, have now begun to encourage this functionality within our health system. The ABC framework is based on qualitative expertise in collaborative care, information systems design, and requirements from care managers. Each category of coordinated care functions within the ABC framework was independently evaluated using the Multiple Perspective approach.
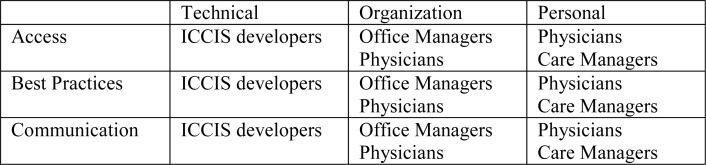
Key stakeholders were identified in the ICCIS project and structured surveys as well as semi-structured interviews were conducted after implementation of ICCIS with these individuals. Over 12 hours of semi-structured interviews were conducted with clinicians, clinic managers, and team developers. Interviews were sought from all clinic members and ICCIS team developers. Overall, 25 individuals were interviewed – 11 care managers, 7 physicians, 3 office managers, and 4 ICCIS team developers. Figure 1 is a data matrix that displays how the majority of key informants’ comments were coded as technical, organization, or personal and then aligned with one category of the ABC model. The previously mentioned definitions of Linstone’s multiple perspectives and the categories within the ABC model were considered when coding specific comments. Figure 1 provided a tool to associate comments from key stakeholders with categories of functions important to the ICCIS system and development of other HIT tools for care coordination.
Figure 1.
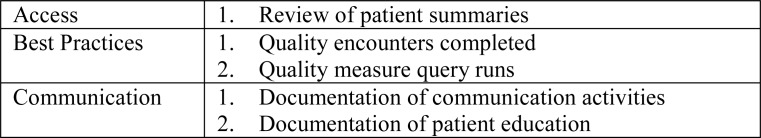
The interviews provided substantial qualitative evidence, but quantitative metrics were identified to provide further context and identify how often clinicians were using each category of functions within ICCIS. Metrics for access to information include the number of times a patient summary was reviewed by a clinician. To evaluate the support of best practices, the number of quality encounters completed and the number of quality measure query runs were utilized as metrics. Quality encounters are reminders generated by ICCIS to facilitate the delivery of evidence-based care and this metric quantifies the total number of those encounters completed. Clinicians were also able to run quality measure queries to determine their performance on specific quality measures and identify patients in which they could improve care. Finally, documentation of other care activities, such as assessment, goal-setting, education, and communication, were utilized as metrics to assess the use of the communication features within ICCIS. These specific metrics are included in Figure 2 below. All quantitative metrics were identified as appropriate for use because they were inherently calculated within ICCIS and could be associated with a specific category in the ABC framework.
Figure 2.
RESULTS
Access
ICCIS integrates complex patient data found in multiple locations within the EHR into meaningful summaries that clinicians can review. Clinicians reviewed 819 patient summaries during the sixteen month trial in which 4,043 patients were enrolled.
Technical Perspective
Initially, obtaining the data to import into ICCIS was difficult, especially in clinics that lacked or could not identify an individual who had the necessary knowledge to access this raw data. An ICCIS developer identified one of the greatest challenges in the initial implementation of ICCIS was “identifying the technical players [to] work with… so we could get [the data]” and further stated, “Everyone has data but no one has the resources to get it out.” Appropriate clinic IT personnel had to be identified and presented with specific data element requirements to facilitate this process. Deciding which information from the EHR is most important to clinicians and how to display it appropriately and consistently throughout the system also proved challenging. The amount of data related to each patient can be vast, especially for patients with multiple chronic conditions and frequent appointments. Every clinician has different beliefs about what information requires review at each patient visit, making it difficult to develop a tool that is satisfactory to all clinicians.
Organizational Perspective
Care team members, other than the care managers, did not use ICCIS frequently to access and review patient information, since this functionality was already inherent in the EHR. Multiple physicians from one clinic stated they were not required to review patient information in ICCIS so they never did. The expectation in all clinics was for the care manager to be the predominant user of ICCIS. Although some physicians agreed ICCIS summarized patient information better than their EHR, it was still perceived as burdensome to log into a separate system to review this information. Unfortunately, in certain clinics, even care managers resisted accessing patient information via ICCIS, because much of the information existed in the EHR which they were required to use by their clinic.
Personal Perspective
Both clinicians and ICCIS developers appreciate the difficulty in displaying complex patient information, but some stated the interface used to access patient information lacked consistency and found it difficult to predict where to find certain details of a patient’s information within ICCIS. Clinicians identified some difficulties initially accessing information in ICCIS, such as the web tool being slow or unresponsive, but many stated improvements were recognized once feedback was relayed to developers. Nevertheless, some users desired a more intuitive interface with descriptive links to information. One clinician described she had “difficulty deciding which tab or headline was the one she actually want[ed]” because it was unclear what action was triggered by certain labels in the ICCIS interface.
Best Practices
ICCIS focused on supporting best practices by providing advanced reporting and the tickler list for care action reminders. 4,440 quality encounters were completed during the study period, which is greater than one encounter per patient enrolled in care management on average. 1,203 quality measure queries were run across the clinics, which indicate an average of greater than 12 quality query runs were performed per month per clinic.
Technical Perspective
Quality metrics typically have detailed technical specifications and ICCIS incorporated over 25 metrics in its quality reporting. While implementing these metrics in one clinic is difficult, the ICCIS team successfully adapted these metrics to be flexible enough to accommodate multiple clinics’ complex data structures. The technical complexity of these metrics typically was not realized by clinicians who actually appreciated the simplicity in determining their compliance with a multitude of quality measures and the recent trends in the quality of their care. Clinicians enjoyed the ability to “easily see performance markers then drill down across different teams [or providers] within [the] clinic [and pull] lists of patients at goal or not.” Additionally, customizable population-based reporting was developed within ICCIS for clinics to find high risk patients or patients by any combination of condition, medication, and demographic information.
Organizational Perspective
Clinics were most willingly to adopt this collaborative care functionality, because it was the most novel compared to the existing functionality offered in their EHRs. Reports were developed to provide clinic summaries of completed care coordination activities and quality metric adherence, which are difficult to capture and report within standard EHRs. Many physicians endorsed frequently using the advanced reporting to identify gaps in care delivery within their patient cohort. One physician stated that she routinely “used ICCIS to identify a sub-population of patients… such as all patients with hypertension on [certain] medications or not and [how well their blood pressure] was controlled… to identify any trends.” ICCIS enabled physicians to run quality reports on their patient lists to determine if they were compliant with certain evidence-based practices, such as obtaining a HgbA1c every 6 months in patients with diabetes, or simply identifying all patients with diabetes under a certain physician’s care.
Personal Perspective
Many care managers reported enjoying being able to use the tickler in ICCIS when they previously described using stray sticky notes or an excel spreadsheet to track care management activities. Care managers stated this new organizational tool provided the desired structure to list the necessary care tasks for each patient and track their completion in a timely fashion. By using the tickler, clinics could more easily track the completion of care coordination activities as well. Care managers appreciated the automated alerts in the tickler to perform such tasks as calling a patient to follow up after a recent emergency room visit.
Communication
To facilitate communication among care team members, ICCIS provides specialized documentation to record encounters, assessments, and patient goals. Clinicians completed 3,820 communication encounters and 2,925 education encounters over the study period across all the patients enrolled in care management.
Technical Perspective
Two-way communication between ICCIS and the EHR was impossible at many clinics for a majority of the study period. A few clinicians resisted the use of ICCIS in clinic, specifically stating that it slowed down the care managers because they were forced to “double document” both in the EHR and ICCIS. The lack of interoperability between ICCIS and the EHR was, by far, the most common complaint in the interviews with users and recognized by the ICCIS developers. Many EHRs don’t support the importing of patient data from another information system, such as ICCIS, and in other settings clinics didn’t have the appropriate support to build the necessary connection for two-way communication. Eventually, the ICCIS developers were able to provide some clinics with this uniformly desired functionality.
Organizational Perspective
Since other team members were not using ICCIS to access documentation, care managers had to document within the EHR to ensure others were aware of a patient’s progress related to care management. A physician stated she “never used ICCIS for documentation or reviewed documentation in ICCIS.” Although specific templates were created to speed up documentation of certain activities and make documentation of data elements structured and accessible by ICCIS for monitoring and tracking purposes, this category of functions was not well received by clinicians because it duplicated a number of existing features already found in their current EHR products. At least one clinic developed a workaround for care managers to document on paper slips, which were later entered en masse into ICCIS by a dedicated individual.
Personal Perspective
Many clinicians failed to achieve or recognize the benefits of documenting in ICCIS for quality assurance monitoring because of the burdens of duplicative data entry. Care managers in these clinics would complete only minimal documentation within ICCIS which limited the information ICCIS had available to provide additional support of best practices. ICCIS team developers stated it was a “challenge to encourage detailed documentation required for analysis… while avoiding redundancy.” It is evident that clinicians who were involved in the development of ICCIS felt more ownership and used the tool more appropriately and frequently. Other care managers lacked an understanding of the potential benefits associated with documenting in ICCIS compared to the EHR.
DISCUSSION
The Multiple Perspective approach in conjunction with the ABC framework provided an adequate structure for organizing the results of analysis of structured surveys and semi-structured interviews with 25 key stakeholders involved with the ICCIS project. In the development of a novel HIT tool, it is critical to provide users clear requirements and expectations for its proper use. Communicating this information to the user can help predict potential barriers to the implementation of this tool. Most HIT tools require iterative improvements to continue to meet evolving user needs. Thus, users must be aware how to best provide regular feedback. Developers must collect this feedback and prioritize it into future changes within the tool. Delivering novel HIT functionality is ideal to ensure adequate adoption of the tool into a clinic’s workflow.
Challenges
Clinicians expect access to patient information to be quick and reliable. Even though EHR data was integrated into ICCIS, it is clear most clinicians were discouraged by having to log into a separate system to review this information, despite ICCIS’s additional features. Physicians have limited time during a patient visit and found the cost of time spent logging into ICCIS outweighed the benefit of system use in many situations. Furthermore, since care managers were the predominant users of ICCIS, other care team members did not typically take the time to review documentation within ICCIS. For most clinics, the care coordination documentation was not transferred back to the EHR; although ICCIS provided many benefits, it failed to increase communication among care team members.
Successes
Although many challenges were identified, successes were still apparent in the implementation of ICCIS. Developing a structured process to assess user needs is very valuable when developing a novel product. Using a foundation of identified user needs provides a clear purpose to the developers and ensures users will obtain an initial benefit from using the HIT tool if it includes the desired features. Developing technical data specifications helped to facilitate clinics’ discussions about adopting a new HIT tool and to determine their readiness for adoption. Many clinics supported using ICCIS for quality reporting and started initiatives to improve care delivered to their cohort of patients that rely on the ability to monitor quality trends. It is clear that many clinics find value in using this care management tool as it is now implemented in over 20 clinics across the Western United States.
Recommendations
Although user interviews tended to focus on major challenges or barriers to use, the quantitative metrics clearly show ICCIS was regularly used across multiple categories of functionality. Supplemental HIT tools, such as ICCIS, are developed because current EHRs still lack specific features desired by clinicians. Many clinicians have already adjusted their clinical workflows to accommodate the use of EHRs, thus it is important that supplemental HIT tools augment this workflow rather than disrupt it. For instance, the functions of ICCIS could be further integrated in various EHRs, or the link between the tools made seamless. A simple link with integrated security access within the EHR may appease most clinicians, and ideally all clinics could establish a two-way transfer of data between the EHR and ICCIS. Some individuals doubt the continued need for supplemental HIT tools as EHR vendors improve their products to address specific gaps in functionality, but health systems, even providers that utilize a single EHR product such as Kaiser Permanente Northwest region, continue to utilize supplemental HIT tools because they have proven to provide significant performance gains in patient care.13 Motivating clinicians to monitor and improve the quality of care delivered to patients in their use of ICCIS was promising. Overall, it is clear clinicians see value in developing specialized HIT tools for care coordination, whether inherent or supplemental, and future developments must focus on providing novel functionality that can be closely integrated with and support their workflow to provide the best possible patient care.
Acknowledgments
This study was funded by AHRQ grant 5R18HS017832-03 Enhancing Complex Care through an Integrated Care Coordination Information System and by the John A. Hartford Foundation.
Additional information about Care Management Plus and the Integrated Care Coordination Information System can be found online at: www.caremanagementplus.org
REFERENCES
- 1.Dorr D, Wilcox A, Brunker C, Burdon R, Donnelly S. The effect of technology-supported, multidisease care management on the mortality and hospitalization of seniors. J Am Geriatr Soc. 2008 Dec;56(12):2195–2202. doi: 10.1111/j.1532-5415.2008.02005.x. [DOI] [PubMed] [Google Scholar]
- 2.Dorr D, Wilcox A, Burns L, Brunker C, Narus S, Clayton P. Implementing a multidisease chronic care model in primary care using people and technology. Dis Manag. 2006 Feb;9(1):1–15. doi: 10.1089/dis.2006.9.1. [DOI] [PubMed] [Google Scholar]
- 3.Behkami N, Dorr D. User centered design in complex healthcare workflows: the case of care coordination and care management redesign. AMIA Annu Symp Proc. 2009 Nov 14;2009:39–43. [PMC free article] [PubMed] [Google Scholar]
- 4.Robert Wood Johnson Foundation . Partnership for Solutions, Johns Hopkins University. Sep, 2004. Chronic Conditions: Making the Case for Ongoing Care. [Google Scholar]
- 5.Agency of Healthcare Research and Quality Medical Expenditure Panel Survey Household Component. MEPS HC-059A. 2004 Feb; 2001. [Google Scholar]
- 6.McDonald KM, Sundaram V, Bravata DM, et al. Care coordination Vol 7. In: Shojania KG, McDonald KM, Wachter RM, Owens DK, editors. Closing the quality gap: a critical analysis of quality improvement strategies. Stanford, CA: Stanford University-UCSF Evidence-based Practice Center, Agency for Healthcare Research and Quality; 2007. [PubMed] [Google Scholar]
- 7.Dorr D, Wilcox A, Donnelly S, Burns L, Clayton P. Impact of generalist care managers on patients with diabetes. Health Serv Res. 2005 Oct;40(5 Pt 1):1400–21. doi: 10.1111/j.1475-6773.2005.00423.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dorr D, Wilcox A, McConnell K, Burns L, Brunker C. Productivity enhancement for primary care providers using multicondition care management. Am J Manag Care. 2007 Jan;13(1):22–28. [PubMed] [Google Scholar]
- 9.Linstone H. Multiple Perspectives: Concept, Applications, and User Guidelines. Systems Practice. 1989;2(3):307–331. [Google Scholar]
- 10.Dorr D, Jones S, Wilcox A. A framework for information system usage in collaborative care. Journal of Biomedical Informatics. 2007;40:282–287. doi: 10.1016/j.jbi.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodenheimer T. Coordinating Care – A Perilous Journey through the Health Care System. The New England Journal of Medicine. 2008 Mar;10:1064–1071. doi: 10.1056/NEJMhpr0706165. 358. [DOI] [PubMed] [Google Scholar]
- 12.Ash J, Gorman P, Lavelle M, Lyman J. Multiple Perspectives on Physician Order Entry. Proc AMIA Symp. 2000:27–31. [PMC free article] [PubMed] [Google Scholar]
- 13.Zhou Y, Unitan R, Wang J, et al. Improving Population Care with an Integrated Electronic Panel Support Tool. Popul Health Manag. 2011 Feb;14(1):3–9. doi: 10.1089/pop.2010.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]