Abstract
Successful handoffs ensure smooth, efficient and safe patient care transitions. Tools and systems designed for standardization of clinician handoffs often focuses on ensuring the communication activity during transitions, with limited support for preparatory activities such as information seeking and organization. We designed and evaluated a Handoff Intervention Tool (HAND-IT) based on a checklist-inspired, body system format allowing structured information organization, and a problem-case narrative format allowing temporal description of patient care events. Based on a pre-post prospective study using a multi-method analysis we evaluated the effectiveness of HAND-IT as a documentation tool. We found that the use of HAND-IT led to fewer transition breakdowns, greater tool resilience, and likely led to better learning outcomes for less-experienced clinicians when compared to the current tool. We discuss the implications of our results for improving patient safety with a continuity of care-based approach.
Introduction
The Joint Commission defines handoffs as a “contemporaneous, interactive process of passing patient specific information from one caregiver to another for the purpose of ensuring the continuity and safety of patient care” [1]. Handoffs are therefore recognized as a critical clinical activity that occurs at all levels of the hospital starting from an individual level (e.g., between nurses or physicians) to an organizational level (e.g., between hospitals for a patient transfer). A recent study estimated that approximately 1.6 million handoffs occur per year in a typical teaching hospital [2]. This number is likely to increase given the current ACGME (Accreditation Council on Graduate Medical Education) restrictions on resident work hours [3].
Ineffectiveness of handoffs leads to progressive information degradation known as funneling and is characterized by omissions and inaccuracies in the information shared among clinicians [4, 5]. Consequently, they are recognized as a major contributing factor to sentinel events and medical errors [4, 6, 7]. To overcome some of the errors, the Joint Commission [7] has mandated all hospitals in the United States to standardize the communication activity between and among physicians and nurses during transitions by implementing safe handoff protocols and tools. A variety of communication strategies and tools such as mnemonics, checklists and templates have been recommended to support the handoff standardization efforts. However, these solutions are neither strictly being followed nor fully adopted in many hospitals [8]. There still exist significant barriers that affect the implementation, adoption and appropriation of these proposed tools [9].
Part of the challenges of using handoff tools can be traced to the fact that these solutions are designed specifically to support the information exchange activity between clinicians during transitions. Less attention is paid towards supporting the handoff workflow, which is just as critical towards achieving successful information transfer. For example, handoff tools that support the preparatory activities prior to handoffs help in better information management and organization, which consequently results in effective communication during handoffs [10, 11]. With this goal, we designed and evaluated a theoretically-based and empirically-grounded handoff intervention tool, HAND-IT to support physician handoffs in critical care. The tool design was based on content standardization (using a body system-oriented format) and summarization (using a patient-case narrative format) for supporting information organization during pre-handoffs and systematic structuring of communication events during handoffs. In this paper, we report on a pre-post prospective intervention study that was conducted to compare the effectiveness of HAND-IT with a commonly used SOAP handoff note with respect to supporting documentation activities and its impact on the handoff workflow.
Background
There is increasing evidence on handoff failures and its impact on continuity [12], quality, and safety of the patient care process [13–15]. Given its significant impact on clinical workflow, researchers have investigated handoff challenges primarily related to communication behavior, information sharing practices, and human factor issues [16]. For example, Streitenberger et al. [17] explored effects of human factor related issues such as stress, fatigue, interruptions, memory load, multitasking; and communication issues related to differences in training, relationships and professional hierarchies on the quality of handoffs. They found that these factors had a detrimental impact on the accuracy, completeness and timeliness of handoffs. A related study on nursing shift handoffs in a critical care unit identified that most common handoff failures and deviations were related to missing documentation, lack of institutional protocols, limited training on handoff skills, and other interpersonal issues among nurses in the department [18]. In another study, Arora et al. [4] investigated the mediating role of “sign-out” in transfer of care for hospitalized patients between inpatient residents using critical incident interview techniques. The two main challenges that influenced the handoff communication were content omissions either related to medications, treatments, tests, consults or active medical problems; and failure-prone communication processes due to the lack of face-to-face communication, double sign-outs (night floats), and illegible/unclear notes.
To mitigate these handoff challenges, a number of strategies and tools have been developed and studied. Some prevalent ones include the incorporation of a standard checklist, avoiding interruptions by choosing a quiet location for handoffs, limiting use of intermediaries, using a common communication style such as SBAR (Situation, Background, Assessment and Recommendations), implementing a readback/hearback communication process, and also supporting face to face communication with interactive questioning [9, 17, 19, 20].
Goldsmith et al. [21] described the design of a web-based nursing handoff tool to improve the standardization of nursing communication. The key functional requirements of this tool included avoiding redundancy, information overload, tool tailoring for specific patient population, and leveraging existing clinician workflow. Some critical data elements included in the tool included patient demographics, code status, allergies, diagnosis, pending tests, safety concerns, and restraints. This study, among many others were focused on designing support for the communication activity between clinicians during handoffs (e.g., [22, 23]). For example, Horwitz et al. [24] tested the effectiveness of a voicemail sign-out system as a handoff method between physicians in an ED and internal medicine department. Pre-post intervention surveys of ED and internal medicine physicians and access logs of the voicemails were evaluated. They found that the asynchronous voicemail sign-out system improved workflow, ease and efficiency of communication. But, it led to reduced interaction between the sending and receiving physicians during handoffs. Furthermore, interestingly the authors found that 30% of the voicemails were not even accessed by the receiving physicians. Consequently, they designed an intervention that included a phone call by the internist to the ED to verify the receipt of the page with the asynchronous voicemail system. There are many others examples of electronic handoff tools that were developed to support communication in hospitals [25], [26].
Despite these various strategies and tools to support handoff standardization, the utilization of these tools in clinical settings is limited [27]. There are two likely reasons for this trend: First, most currently available tools fail to provide integrated support for the clinician’s overall workflow throughout the handoff process. As a result, clinicians have to use different and multiple independent technologies (or tools) to support their preparatory activities in pre-handoff phase (e.g., printed copy of patient record), communication activities in handoff phase (e.g., online handoff form) and patient management activities in post-turnover phase (e.g., post-it and scrap notes). For instance, Van Eaton et al. [28] evaluated a centralized, web-based computerized rounding and sign-out system (UWCores) that automatically downloads patient data (vital signs, lab results) and prints them into rounding, sign-out, and progress note templates. The authors hypothesized that UWCores would positively impact continuity of care and resident workflow by improving team communication involving patient handovers and streamlining inefficiencies in pre-handoff phase. A prospective, randomized, crossover study with fourteen inpatient resident teams at two teaching hospitals was conducted. Frequency of missed patients during handoffs, subjective continuity of care quality and workflow efficiency with and without UWCores, and daily self-reported pre-handoff and handoff times and tasks were evaluated. The authors found that UWCores not only reduced the number of missed patients by half but also reduced the pre-handoff time spent on copying basic data from EMR. This suggests that workflow efficiency and continuity of care can be improved by supporting the pre-handoff activities. Second, some of these proposed handoff tools were rigid and supported a regimented and structured form of communication (e.gs., [7, 20]). While others were highly ambiguous and supported a flexible and open-ended form of communication during handoffs (e.g., [9, 17]). Both of these approaches were often met with skepticism in terms of supporting the handoff process.
To address these issues, we designed a handoff intervention tool, HAND-IT that allowed for an integrated support for the handoff workflow with its structurally-bounded and flexible information organization format [11]. In the subsequent section, we describe the SOAP handoff note and HAND-IT.
Handoff Tools: SOAP and HAND-IT
We compared the effectiveness of two tools for supporting handoffs: SOAP note and HAND-IT (Handoff Intervention Tool). Each of these tools was based on inherently different design rationales. The patient information in the SOAP note is structured based on subjective, objective, assessment and plan of care, therefore followed a problem-based format, commonly used in general medicine-surgery wards [29]. In contrast, we designed HAND-IT grounded on our prior results that showed that content standardization using a body system-oriented format and summarization using a problem-case narrative format would reduce the communication complexity and incidence of transition errors [10]. A brief description of the two paper-based tools and their design rationales are provided below.
SOAP Note
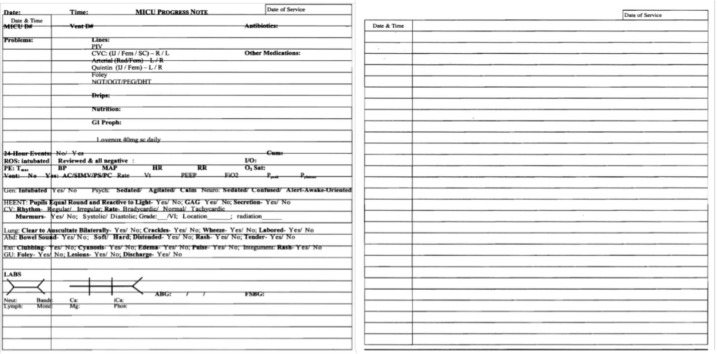
The SOAP note was a generic tool for coordinating patient-care delivery and management process in the MICU. The patient-related information included four components: subjective information (e.g., patient history and chief complaint), objective information (e.g., vital signs, lab results), assessment information (e.g., differential diagnosis) and plan-related information (e.g., medication and lab orders, referrals). SOAP note was originally adopted in the MICU we studied because of its partly structured organization that helped in avoiding information gaps and also in providing a template for residents’ presentation during morning rounds. Furthermore, the billing department found the information organization in the SOAP note easy to comprehend and use for reimbursement and insurance purposes. Prior to the SOAP note, a free-form paper was used for rounds which had limited use during handoffs. A blank SOAP note is provided below in Figure 1.
Figure 1.
SOAP Handoff Note
Handoff Intervention Tool (HAND-IT)
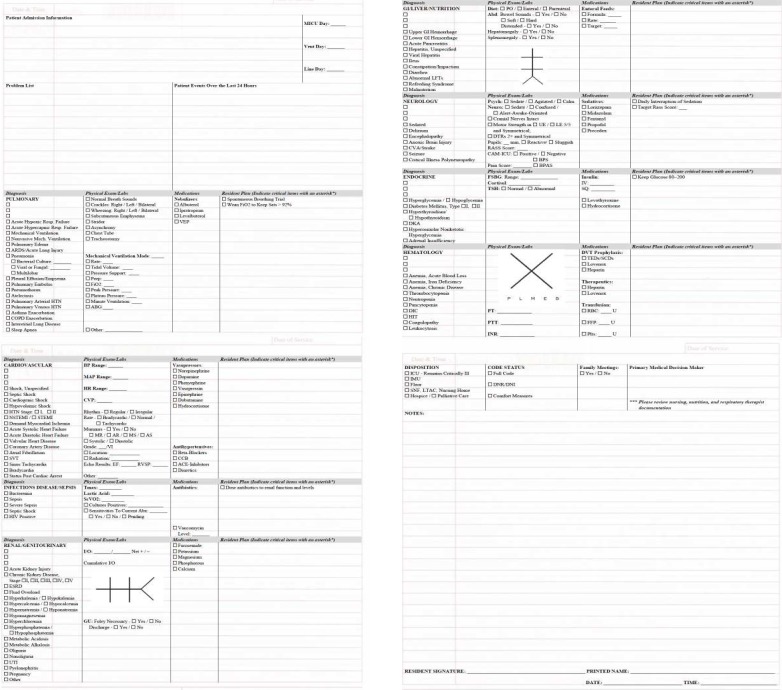
HAND-IT is a simple, cost-effective and paper-based tool developed based on a hybrid body system-oriented and problem case-narrative format. It can be considered as an upgraded version of the SOAP note with its design features influenced by prior empirical work. The goal of HAND-IT is two-fold: facilitate handoff communication in a consistent and effective manner and to support coordination of information seeking and organization activities in preparation for handoffs. The design of HAND-IT involved (1) requirements gathering (2) design (3) tool development and (4) evaluation. The design requirements were primarily gathered in phase 1 of the study based on an extensive evaluation of handoff processes, communication during handoffs, and information and decision breakdowns during handoffs (detailed descriptions can be found in [10, 27]).
The new tool design was based on two fundamental design requirements: content standardization (using a body system-oriented format) and content summarization (using a problem-case narrative format) for standardizing information sharing during handoffs. These design requirements were selected as they have been reported to minimize information breakdowns and support effective clinical decision-making [17, 30]. Additionally, based on the Society of Critical Care Medicine (SCCM) guidelines [31], we also incorporated evidence-based concepts related to standard critical care management that can improve patient outcomes including identification of delirium, sedation practices, prophylaxis and feeding information. Based on these functional requirements, the basic format and content of the tool were decided by the design team consisting of two (2) ICU attending physicians (which include the MICU director and a quality officer), one MICU clinical fellow, and one researcher (first author) [See Figure 2 for the final design of the HAND-IT tool].
Figure 2.
Handoff Intervention Tool: HAND-IT
Content standardization was achieved through a checklist-based body system-oriented format. Checklists have been shown to be particularly effective in organizing complex clinical information and tasks and helps in avoiding critical errors and breakdowns [32]. Using the checklist format, we organized information within each body system into fundamental categories including (a) diagnosis, (b) physical exam and labs, (c) medications, and (d) resident plan (for that particular body-system). Such an organization of body system-based information supports the reasoning process behind assessment and plan of care and also allows for identifying interactions between the different body systems [30]. In addition to content standardization, we incorporated a summarization feature through free-text fields for the physicians to add patient-case related narrative summaries. Their summaries could be included into the: (a) patient admission information, (b) problem list, (c) patient events over the last 24-hour period and finally, (d) resident notes. Such a narrative helps in effectively reasoning about the case and leads to better sense-making, problem analysis and also assists in developing a temporal re-construction of the patient care events [10]. HAND-IT was pilot tested with two (2) residents and a clinical fellow in the MICU. Iterative modifications were made based on their feedback and suggestions. For instance, a resident suggested that a patient problem list was an important component that was missing in a previous iteration of HAND-IT.
Method
In this section, we describe the study setting, participants, study design, data collection, and the measures used for analysis. This study was part of a larger longitudinal study that involved the detailed evaluation of HAND-IT using extensive observations, physician shadowing, audio recording of morning rounds, interviews with the clinical team and evaluation of handoff documentation during multi-professional rounds. Here we focus on the evaluation and analysis of handoff documentation during multi-professional rounds. The institutional review board (IRB) of the hospital approved the study.
Study Setting
This study was conducted in a large academic hospital in the Gulf Coast that had over 33,000 admissions in 2011. We focused on resident handoffs in a 16-bed, closed MICU that was managed by intensivists. We selected the MICU, as their patients typically stay longer than a single clinician shift and hence required care transitions (or handoffs) across shifts [33]. We chose resident handoffs because the newly implemented working hour restrictions increased the number of resident sign-outs [3]. In the MICU we studied, resident handoffs were an example of team handoffs, where the team comprised of outgoing resident and intern (i.e., post-call), an attending physician (i.e., on-call), a clinical fellow (i.e., on-call), and incoming resident and intern (i.e., on-call), patient nurse, a pharmacist and a respiratory therapist.
The handoff process in the MICU comprised of three interdependent phases with distinct goals (detailed descriptions can be found in [27]): a pre-turnover phase that focused on coordination activities (e.g., information seeking and organization); a handoff phase that focused on exchange of communication events related to patient-care between outgoing and incoming team members; and the post-turnover phase that focused on execution of patient-care delivery activities [27]. Previously, for each patient case, the MICU outgoing team used a SOAP (subjective, objective, assessment and plan) note to seek and organize information for presentation and communication with the oncoming team in the handoff phase. The whole study was conducted over a six-month period from April to October 2011. As previously described, this paper reports on the analysis of a smaller, but relevant aspect of the effectiveness in the use of two handoff tools by the MICU residents and interns over a two-month period.
Participants
The participants in the study included the attending physician, clinical fellow, internal medicine residents, interns, respiratory therapist, a pharmacist and nurses. Each resident and intern were responsible for a total of sixteen (16) patients, with each assigned up to eight (8) patients during a shift. The team handoffs occurred daily in the morning and took approximately 4 hours to complete. At the MICU we studied, there was a set of three (3) residents and three (3) interns who rotated for a period of 1 month although their specific roles varied during different shifts (e.g., on-call, post-call or short-call). Thus, in our study for a two-month period, there were six (6) residents and six (6) interns. The specific roles and responsibilities of the MICU team are provided in Table 1.
Table 1.
MICU Roles and Responsibilities
| Role | Responsibilities |
|---|---|
| Attending | Intensivist supervisor for all MICU team patient care decisions. |
| Fellow | Intensivist in training, second in command supervising over all MICU team patient care decisions, care, and procedures in the attending’s absence. The fellow also keeps the attending informed of daily MICU activities. |
| Resident | A physician in their second or third year of internal medicine residency training in charge of daily patient care activities working under the direction and supervision of the attending and fellow. |
| Intern | A physician in their first year of internal medicine residency training tasked with implementing daily patient care activities under the direction and supervision of the attending, fellow, and other residents. |
Materials and Design
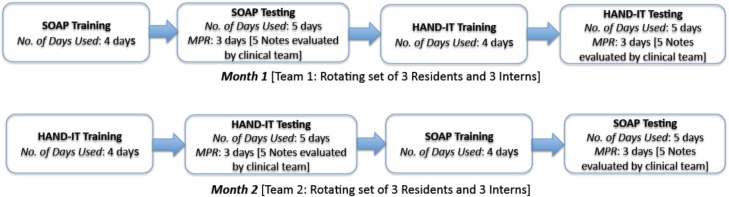
SOAP note and HAND-IT were evaluated for their effectiveness as tools for supporting documentation for the handoff process. We used a longitudinal pre-post prospective intervention study where two sets of residents and interns used SOAP and HAND-IT in a two-month period (See Figure 3 for the organization of the study). The effectiveness of documentation using both tools was measured using multi-professional rounds conducted by the director of the MICU and the on-call care team (see details in the next section).
Figure 3.
Study Design and Procedure
Multi-Professional Rounds
Multi-professional round (MPR) is a mechanism by which teams of clinical professionals perform joint evaluation. For example, such multi-professional teams are often convened to evaluate quality and decision-making initiatives [34]. In our study, the MICU director convened MPRs to evaluate the quality and completeness of the handoff note (either SOAP or HAND-IT). These MPR’s were conducted immediately after the morning rounds and were organized only for research purposes, as it was not part of the typical MICU workflow. These collaborative sessions were attended by MICU Director, on-call attending physician, on-call resident and intern, patients’ nurses, a pharmacist, a respiratory therapist and the first author.
The selection of specific patient handoff notes for evaluation during MPR (in either the SOAP or HAND-IT condition) was made after a brief discussion between the MICU director, the on-call attending physician and the first author of the paper. These decisions were based to ensure maximum selection variability across patient cases, patient status and patient condition complexity. After the patient cases were selected, the MICU team (including the patient’s nurse) convened to jointly evaluate the information documented (by the outgoing) on the tool with respect to the accuracy and completeness of patient-care information. During the MPR session, the handoff note (either SOAP or HAND-IT) was read loudly to the team. Then the on-call team members were asked individually to identify any breakdowns in patient-care information and patient-care decisions. For instance, the nurse was asked whether there were any omissions with respect to a nursing standpoint for the particular patient. In addition, they were also asked if the handoff note was up-to-date and accurate. Based on their collective content analysis of the handoff note, the team characterized the breakdowns into omissions, inaccuracies, and modifications to the originally written plan of care and missed problem lists of patients. During MPRs, the lead author made meticulous notes on the team analysis of the case in addition to the audio recording of the MPRs. In addition, de-identified photocopies of the evaluated SOAP and HAND-IT tools (with prior IRB approval) were collected for detailed analysis. Informal interviews with the participants (about the tool use and limitations) were also conducted after the MPR.
Procedure
The experimental implementation consisted of multiple stages in each month over a two-month period (See Figure 3). In the first month, participants first used the SOAP note for a period of four (4) days as part of their training. This was followed by the experimental stage where they used the SOAP note for five (5) days. During days seven, eight and nine (last three days of experimental evaluation), MPRs were conducted after the morning rounds. Following this period, participants were provided introductory training with the HAND-IT tool. They used HAND-IT for handoffs for the next four (4) days. This helped in acclimatizing them to different features with respect to content, function and format of the tool. In the last stage, we started the experimental evaluation of the use HAND-IT tool for a period of five (5) days. As with the SOAP condition, MPRs were conducted over the last three days of the experimental sessions. A total of five (5) notes each was evaluated during the MPRs in the SOAP and HAND-IT condition: two each on days one and two, and one on day three. The same procedure was repeated in the second month with a new MICU on-call team. During the second month, the order in which the participants used the two tools was counter-balanced with the previous month. In other words, the participants started with the HAND-IT training for four (4) days followed by testing for a period of five (5) days. As in the previous month, a total of five (5) notes from each condition were selected for evaluation during the MPRs. As described in the previous section on MPRs, the handoff tool was then evaluated for missed information, incorrect entries, missed problem list items and changes to plan of care.
Measures
We used three measures to evaluate the efficiency of handoff documentation using the two tools: number of information breakdowns, decision-making breakdowns and expertise of the clinicians. Each of these is described below.
Information Breakdowns:
We characterized information breakdowns as the failure to appropriately gather the necessary information regarding a patient or gap in information flow. Two variables were used to represent the information-breakdowns: number of missed information and number of incorrect information on the handoff tool (either SOAP or HAND-IT).
Decision-Making Breakdowns:
We characterized decision-making breakdowns as modifications (including additions/deletions) that were made by the attending to the decision-related information documented by the outgoing team (resident or intern) on the handoff tool during the MICU morning rounds. Two variables were used to represent the decision-making breakdowns: number of changes to plan of care and number of missed problem list items.
Expertise Differences:
Patient care responsibility in the MICU was divided between an intern (a first year trainee resident) and senior resident (third year trainee resident). We characterized the efficacy in the use of the handoff tools based on their year of residency training.
Data Analysis
We used the audio-recorded data, researcher notes from the MPR evaluation, and photocopies of the selected SOAP and HAND-IT tools for our two-staged analysis. First, a qualitative analysis of the information on the tools was coded based on information gaps. The frequencies of missed and incorrect information, missed problem list items, and changes to plan of care were tabulated based on the MPR recordings. Data was organized according to handoff tool type (SOAP, HAND-IT) and expertise (resident, intern). Then comparative analysis using student t-tests were performed. After this, we evaluated the causal determinants of decision-making (i.e., number of missed problem list items and number of changes to plan of care) while using the SOAP and HAND-IT tools. For this, we developed the best-fit zero-inflated Poisson regression model using the following variables: expertise differences (resident, intern) and information breakdowns (number of missed information, number of incorrect information). These variables were considered as there was no association between expertise and information breakdowns based on Chi-square tests (χ2 = 0.0899, df =1, p =0.76). For information breakdowns, an aggregate value of the number of missed information and number of incorrect information was used for the analysis. For expertise differences, we used the categorized notes created by the residents and interns.
Results and Discussion
Information Breakdowns
We found that significantly more information was missed using the SOAP note than with HAND-IT [MSOAP= 12.5, MHAND-IT= 2.8; t(18)=5.98, p <0.0001]. Additionally, more incorrect information was recorded using the SOAP note than with HAND-IT [MSOAP= 1.8, MHAND-IT= 0.9; t(18)=2.1, p <0.05]. In other words, our new intervention tool, HAND-IT improved the information seeking and organization activities of residents and interns during the pre-turnover phase and consequently led to fewer missed and incorrect information.
This shows the effectiveness of HAND-IT in supporting the information organization activities in preparation for handoffs, resulting in fewer information breakdowns and errors. This was achieved through (a) supporting a logical and systematic arrangement of information in a standardized checklist format that helps with cognitive and time constraints in busy settings, (b) affording the recognition of inconsistencies between discrete pieces of information with the ordering of most important life-sustaining body systems (such as pulmonary and cardio-vascular) followed by commonly addressed critical illnesses in ICUs (such as renal, GI), (c) providing a coherent coverage of all patient body system information (with related parameters explicitly stated) and, (d) supporting a comprehensive arrangement of all aspects (such as problems, therapy, medications, labs etc.) pertaining to each body system displayed in a format that is user-friendly with respect to writing and reading.
Decision Making Breakdowns
We also found differences in the number of changes to plan of care that were made: significantly more attending changes to plan of care were made with the SOAP note than with HAND-IT [MSOAP = 4.0, MHAND-IT = 0.8; t(18)=3.7, p <0.001]. Also, the differences in number of problem list items that were missed between the two tools was nearly significant, with more problem list items being missed in the SOAP note than with HAND-IT [MSOAP = 2.1, MHAND-IT = 0.8; t(18)= 1.93, p =0.051].
This shows that HAND-IT led to fewer changes to plan of care created by the outgoing team and lesser omissions of patient diagnoses (i.e., problem lists). The juxtaposed organization and grouping of related body system information in checklist and narrative formats (a) allowed for cuing of relevant information that the physician should consider, recall for making diagnostic and therapeutic decisions, (b) allowed for specific inferences to be drawn (relevant to patient problem) because the assessment and corresponding plan are formulated for each of the different body systems and, (c) provided cognitive support that affords their reasoning process.
Handoff Tool Resilience
Resilience was based on a Poisson regression that evaluated the decision-making effectiveness variables (number of missed problem lists and number of changes to plan of care) in terms of information breakdowns and expertise of the participants (residents, interns). Based on the analysis, we found that for the SOAP note, the increase in the aggregate number of breakdowns was directly proportional to the number of missed problem list items. In other words, unit increase in the missed problem list led to a unit increase in the total breakdowns. In contrast, unit increase in the missed problem list required an increase of 11.92 breakdowns. For the number of changes in plan of care, there was no statistically significant model that described the effects.
Based on the results on the number of missed problem list items, we conclude that HAND-IT was more resilient, requiring significantly more breakdowns before it resulted in a missed problem list. This is especially encouraging considering that one of the oft-described characteristics of a good handoff tool is its resilience to errors [12, 35]. Though HAND-IT was not designed with an explicit goal of resilience towards breakdowns, this serendipitous outcome was likely a result of our design goals (i.e., systematization of content in a checklist format and summarization). These features provided (a) transparency within the clinician’s thought process helping in identifying and avoiding errors (through checklist format) and, (b) supported the process of crosschecking clinicians’ assumptions using a fresh perspective (through the narrative).
Effects of Expertise
Based on the regression model, we also evaluated the decision-making effectiveness based on the expertise of the physicians who used the two tools. We found that residents’ usage of the SOAP note led to 0.32 fewer number of missed problem list items than interns. In contrast, residents’ usage of HAND-IT led to 2.92 more number of missed problem list items than interns. This shows that interns’, who had lesser experience and expertise than senior residents, performance was improved by the better information organizational capabilities of HAND-IT.
This improvement in performance by interns may have been supported by the layering (display) of information that prompted interns to attend to appropriate (and relevant) information relevant for decision-making. This allowed for a focused perspective without being concerned about the significant amount of available information. Additionally, such an organization may have helped less-experienced interns whose medical knowledge schema are less developed [36]. In other words, a structured, checklist style presentation provided a training wheels type of interface that is more likely to have helped in progressive learning and not having to deal with a deluge of patient information. In contrast, residents who have much more developed knowledge schemas found difficulty in re-adjusting their mental models to a new tool. This likely led to a higher number of breakdowns. More detailed empirical evaluation is necessary to identify the causal reasons for that led to these differences in documentation effectiveness between residents and interns.
Conclusion and Future Work
HAND-IT demonstrated several desirable characteristics of handoff tools such as support for error detection and recovery (i.e., avoiding information and decision-making breakdowns) [24], resilience to breakdowns [35] and support for education and learning [37]. Additionally, HAND-IT, by its very design purpose supported coordination of information flow and decision-making, which inherently helps in ensuring continuity of care that emphasizes the importance of capturing an “uninterrupted and coordinated succession” of patient events to meet their care needs [38]. In other words, mitigating the information and decision-making breakdowns improves timeliness of care delivery, reduces work duplication, minimizes patient length of stay and most importantly, enhances patient safety and quality.
Optimal care delivery in the modern ICU requires consistent coordination among multiple disciplines and services, such as sub-specialty consultants and supportive healthcare personnel. For example, in addition to the critical care team service, a septic patient with multi-organ failure may require consultations from infectious disease and nephrology specialists to help manage the infection and acute renal failure respectively. However, other services such nutrition, physical therapy, and social work often contribute to the general plan of care for these complex patients. From our MICU observations and informal interviews with nurses and consults, we found that the HAND-IT tool improved overall continuity of patient care not just between clinicians during transitions but also across clinicians from different services. The tool was viewed as a “coordination artifact” that helped in managing information and task interdependencies between multiple clinicians involved in a single patient care process.
Limitations:
We would like to acknowledge the study limitations. The evaluation of HAND-IT was conducted at a single MICU setting. While some of the specific findings may not be transferrable to other ICUs and care settings, the design of our intervention tool (inherent structure and function) is based on a traditional medical school education format. The general features of the tool can therefore be applied to care transitions in other settings. Nevertheless, other clinical settings will need to refine the tool based on their local clinical workflows. Additionally, we did not report on the several unintended workflow effects as a result of the use of HAND-IT tool such as the increased time and effort involved in seeking complete information from multiple data sources and switching between information tasks. Our primary focus of this paper is to highlight the effectiveness of the handoff tools with respect to documentation accuracy and completeness. A true measure of the success of HAND-IT can be made only after a complete evaluation and assessment of these parameters.
Acknowledgments
This research was supported by Grant No. 220020152 by James S McDonnell Foundation (JSMF) for Cognitive Complexity and Error in Critical Care to Vimla L. Patel. We would especially like to thank Mark Warner, MD for his assistance during HAND-IT tool development. We are also greatly obliged to the study participants including nurses and physicians.
References
- [1].NPS National Patient Safety Goals. 2008. [cited 2012 March 15]
- [2].Vidyarthi A. Triple Handoff. Hospital Medicine. 2006.
- [3].Accreditation Council for Graduate Medical Education, A. Report of the Work Group on Resident Duty Hours and the Learning Environment. 2002. [Google Scholar]
- [4].Arora V, et al. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health. 2005;14:401–407. doi: 10.1136/qshc.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Anthony MK, Preuss G. Models of care: The influence of nurse communication on patient safety. Nursing Economics. 2002;20(5):209–215. [PubMed] [Google Scholar]
- [6].Singh H, et al. Medical Errors Involving Trainees: A Study of Closed Malpractice Claims From 5 Insurers. Archives of Internal Medicine. 2007;167(19):2030–2036. doi: 10.1001/archinte.167.19.2030. [DOI] [PubMed] [Google Scholar]
- [7].Arora V, Johnson J. A model for building a standardized hand-off protocol. Joint Commission Journal on Quality and Patient Safety. 2006;32(11):646–655. doi: 10.1016/s1553-7250(06)32084-3. [DOI] [PubMed] [Google Scholar]
- [8].Kitch B, et al. Handoffs causing patient harm: a survey of medical and surgical house staff. Joint Commission Journal on Quality and Patient Safety. 2008;34(10):563–570. doi: 10.1016/s1553-7250(08)34071-9. [DOI] [PubMed] [Google Scholar]
- [9].Patterson E, et al. Handoff strategies in settings with consequences for failure: lessons for health care operations. International Journal for Quality in Health Care. 2004;16:125–132. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- [10].Abraham J, et al. American Medical Informatics Association (AMIA) Washington, DC: 2011. Falling Through the Cracks: Information Breakdowns in Critical Care Handoff Communication. [PMC free article] [PubMed] [Google Scholar]
- [11].Abraham J, et al. Minimizing Communication Breakdowns: An Empirical Evaluation of A Handoff Intervention Tool. Critical Care Medicine. 2011;39(12):152. [Google Scholar]
- [12].Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Quality and Safety in Health Care. 2010;19(6):493–497. doi: 10.1136/qshc.2009.033480. [DOI] [PubMed] [Google Scholar]
- [13].Coutsouvelis J, et al. Implementation of a pharmacist-initiated pharmaceutical handover for oncology and haematology patients being transferred to critical care units. Supportive Care in Cancer. 2009 doi: 10.1007/s00520-009-0713-4. [DOI] [PubMed] [Google Scholar]
- [14].Donchin Y, et al. A look into the nature and causes of human errors in the intensive care unit. Quality and Safety in Health Care. 2003;12(2):143–147. doi: 10.1136/qhc.12.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mistry KP, et al. Using Six Sigma® Methodology to Improve Handoff Communication in High-Risk Patients. Advances in Patient Safety: From Research to Implementation. 2008:3. [PubMed] [Google Scholar]
- [16].Riesenberg LA, Leitzsch J, Little B. Systematic Review of Handoff Mnemonics Literature. American Journal of Medical Quality. 2009;24(3):196–204. doi: 10.1177/1062860609332512. [DOI] [PubMed] [Google Scholar]
- [17].Streitenberger K, Breen-Reid K, Harris C. Handoffs in Care--Can We Make Them Safer? Pediatric Clinics of North America. 2006;53(6):1185–1195. doi: 10.1016/j.pcl.2006.09.010. [DOI] [PubMed] [Google Scholar]
- [18].Berkenstadt H, et al. Improving Handoff Communications in Critical Care*. Chest. 2008;134(1):158–162. doi: 10.1378/chest.08-0914. [DOI] [PubMed] [Google Scholar]
- [19].Arora V, et al. A theoretical framework and competency-based approach to improving handoffs. Quality and Safety in Health Care. 2008;17:11–14. doi: 10.1136/qshc.2006.018952. [DOI] [PubMed] [Google Scholar]
- [20].Haig K, Sutton S, Whittington J. SBAR: A shared mental model for improving communication between clinicians. Jt Comm J Qual Patient Saf. 2006;32:167–175. doi: 10.1016/s1553-7250(06)32022-3. [DOI] [PubMed] [Google Scholar]
- [21].Goldsmith D, et al. Development of a Nursing Handoff Tool: A Web-Based Application to Enhance Patient Safety. AMIA Annual Symposium. 2010:256–260. [PMC free article] [PubMed] [Google Scholar]
- [22].Anderson J, et al. The Veterans Affairs shift change physician-to-physician handoff project. Joint Commission Journal on Quality and Patient Safety. 2010;36(2):62–71. doi: 10.1016/s1553-7250(10)36012-0. [DOI] [PubMed] [Google Scholar]
- [23].Wayne J, et al. Simple Standardized Patient Handoff System that Increases Accuracy and Completeness. Journal of Surgical Education. 2008;65(6):476–485. doi: 10.1016/j.jsurg.2008.06.011. [DOI] [PubMed] [Google Scholar]
- [24].Horwitz L, et al. Dropping the Baton: A Qualitative Analysis of Failures During the Transition From Emergency Department to Inpatient Care. Annals of Emergency Medicine. 2009;53(6):701–710. doi: 10.1016/j.annemergmed.2008.05.007. [DOI] [PubMed] [Google Scholar]
- [25].Flanagan ME, et al. Evaluation of a Physician Informatics Tool to Improve Patient Handoffs. Journal of the American Medical Informatics Association. 2009;16(4):509–515. doi: 10.1197/jamia.M2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Stein D, et al. Signout: a collaborative document with implications for the future of clinical information systems. AMIA Annual Symposium Proceedings; 2007. pp. 696–700. [PMC free article] [PubMed] [Google Scholar]
- [27].Abraham J, Kannampallil T, Patel VL. Bridging gaps in handoffs: A continuity of care approach. Journal of Biomedical Informatics. 2012;45(2):240–254. doi: 10.1016/j.jbi.2011.10.011. [DOI] [PubMed] [Google Scholar]
- [28].Van Eaton EG, Horvath KD, Lober William B, Rossini Anthony J, Pellegrini Carlos A. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. Journal of the American College of Surgeons. 2005;200(4):538–545. doi: 10.1016/j.jamcollsurg.2004.11.009. [DOI] [PubMed] [Google Scholar]
- [29].Weed LL. Medical terminology records, medical education, and patient care. The problem-oriented record as a basic tool. Cleveland, OH: Case Western Reserve University; 1969. [Google Scholar]
- [30].Varon J, Acosta P, editors. Handbook of Critical and Intensive Care Medicine. Second ed. S.S.B. Media; 2010. [Google Scholar]
- [31].Jacobi J, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Critical Care Medicine. 2002;30(1):119–141. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- [32].Gawande A. The Checklist Manifesto: How to Get Things Right. New York, NY: Metropolitan Books; 2009. [Google Scholar]
- [33].Nemeth C, et al. Creating resilient IT: how the sign-out sheet shows clinicians make healthcare work. 2006. [PMC free article] [PubMed] [Google Scholar]
- [34].Gurses AP, Xiao Y. A Systematic Review of the Literature on Multidisciplinary Rounds to Design Information Technology. Journal of the American Medical Informatics Association. 2006;13(3):267–276. doi: 10.1197/jamia.M1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Cheung DS, et al. Improving Handoffs in the Emergency Department. Annals of Emergency Medicine. 2009;55(2):171–180. doi: 10.1016/j.annemergmed.2009.07.016. [DOI] [PubMed] [Google Scholar]
- [36].Patel VL, Arocha JF, Kaufman DR. Diagnostic reasoning and medical expertise. Psychology of Learning and Motivation - Advances in Research and Theory, Vol 31. 1994;31:187–252. [Google Scholar]
- [37].Lally S. An investigation into the functions of nurses’ communication at the inter-shift handover. Journal of Nursing Management. 1999;7(1):29–36. doi: 10.1046/j.1365-2834.1999.00095.x. [DOI] [PubMed] [Google Scholar]
- [38].Harvey CM, et al. Human Factors of Transition of Care. 2006:233–248. [Google Scholar]