Abstract
Perioperative care is complex and involves multiple interconnected subsystems. Delayed starts, prolonged cases and overtime are common. Surgical procedures account for 40–70% of hospital revenues and 30–40% of total costs. Most planning and scheduling in healthcare is done without modern planning tools, which have potential for improving access by assisting in operations planning support. We identified key planning scenarios of interest to perioperative leaders, in order to examine the feasibility of applying combinatorial optimization software solving some of those planning issues in the operative setting. Perioperative leaders desire a broad range of tools for planning and assessing alternate solutions. Our modeled solutions generated feasible solutions that varied as expected, based on resource and policy assumptions and found better utilization of scarce resources. Combinatorial optimization modeling can effectively evaluate alternatives to support key decisions for planning clinical workflow and improving care efficiency and satisfaction.
Introduction
Surgical procedures are often the most intensive and efficacious therapeutic interventions available in modern medicine – these treatments are frequently curative and are sometimes the only recourse for patients. Surgeons and other proceduralists are very highly trained professionals; the technology and resources they employ are typically advanced, expensive, and scarce. Optimization of these limited resources is paramount to the safe, effective, and efficient delivery of healthcare.
The 100 million surgical procedures performed each year in the U.S. account for roughly one-half of total hospital-based care delivered to patients.1,2 In hospitals, these surgical procedures total 40–70% of revenues and 30–40% of total costs. Nearly two-thirds (63%) of all patients discharged from a hospital have had at least one procedure performed during their stay, and hospital stays involving surgery have nearly twice the expenditures of non-surgical inpatient stays, with most expenditures on the day of the surgery.3
Surgical procedures can be divided between elective and non-elective surgeries: most of the operative planning and scheduling literature deals with elective surgery, which can generally be scheduled in advance, and thus can easily benefit from an optimized scheduling approach. These studies find that the average OR starts on schedule just 27% of the time (with the most efficient ORs at 76%); the average turnover time is 31.7 minutes, more than double the recommended best practice of 15 minutes; and the average utilization runs at only 68% capacity.4 Overall, elective surgical caseload is considered the most important factor influencing emergency patient diversions.5 By increasing overall OR utilization and reducing turnover times the occurance of such diversions of emergency patients can be reduced, leading to improved emergency patient care by enhanced utilization of existing resources.
Most U.S. hospitals (87%) have OR suites and are estimated to spend $30B to $90B on their surgical facilities annually – accounting for up to 70% of total hospital expenditures.6 Consequently, ORs are one of the most expensive functional areas in hospitals. Other departments (e.g. intensive care units and general medical-surgical wards) are tightly coupled to the OR and expend significant resources treating surgical patients. Remarkably, while ORs cost between $10 and $40 per minute, and their surgical patients impact hospital-wide efficiency and throughput, relatively little research has focused on optimizing OR financial outcomes.
ORs are similar to many other types of product/service delivery environments that are complex in nature. Root causes of this complexity (in ORs) include: variation in patient comorbidity, severity of illness and needs; provider and patient preferences; staff skill sets; mismatches in patient demand and the capacity of care resources; and the availability, completeness, and accuracy of pertinent information. Fortunately, such levels of complexity can often be managed more effectively through well-designed information management and decision support systems.7–8 However, these systems typically require accurate and timely information about the detailed operational status of the underlying resources and work processes that perform the organization’s functions. Such information (“state” information) is essential for making the best operational decisions regarding priorities. The ad-hoc method of developing OR schedules has been shown to be very poor at planning. In one study, 50% of historical operating lists were under-booked and 37% over-booked.9
In general, healthcare lacks this “state” information, where relatively few hospital managers know which of their rooms are occupied, which are empty, which are in need of cleaning, etc. This makes it very difficult to prioritize admission, surgery, diagnostic procedures, patient transfers, and room cleaning services. As a result, emergency departments, ORs, and PACU areas become congested with patients waiting to be admitted, impacting the ability to deliver timely care. A well-defined system state not only relays current status information, but also helps reduce the level of complexity in the system’s current workload.
Based on current state information, there are many possible future states for an OR suite. The complexity of accurately determining these future states and choosing actions which result in the most desirable states over time arises for three reasons: causality, combinatorics, and uncertainty.
Causality is a simple concept: Tuesday follows Monday, night follows day, etc. However, achieving the goal of providing OR services on time with high surgical team and suite utilization requires that all preparation and precursor steps be completed at the right time. Furthermore, in the real world, a hospital cannot go back to yesterday or last week to do something that has become apparent today as necessary for success.
Combinatorics greatly confounds causality. Currently, hospitals have many different decisions about how they can operate, and their choices set the stage for future success or failure. Consider a hospital making a single decision – should patient A or patient B be treated first. The future consists of two time lines, one in which patient A is satisfied followed by treating patient B, and the other in which the order is reversed. Which of these two time lines is better depends on many factors, such as the uncertainty of outcome. Perhaps a critical piece of equipment is unavailable early in the day, but the surgical team prefers certain procedures earlier to avoid fatigue. Hospitals face many decisions at any given time, and these decisions interact with subsequent decisions. The number of combinations of choices for these decisions means that hospitals must select one of a huge number of timelines on which they must operate. It is difficult to predict which path is best.
Experience shows that uncertainty is a fact of life that must be managed by making decisions based on high probabilities of success, regardless of how uncertainty plays out. In addition to different combinations of decision choices, the uncertainty of surgical outcomes presents hospitals with a huge number of possible timelines on which they could operate, some of them with very different outcomes. There are a number of defenses, or insurance, against uncertainty. For example, patients can be sequenced to mitigate uncertainty, a certain amount of buffer time can be built into operating schedules to absorb variability, and certain procedures can be scheduled into time windows to accommodate resource availability.
Multiple investigators have sought to solve the Operating Room (OR) planning problem. Existing approaches include stochastic or linear programming, computer simulation, OR scheduling algorithms, and others. For example, simple linear programming of the sum of individual operation times and a pooled standard deviation of these times generates a probability that the operating list would finish within its scheduled time predicted the correct outcome (under-run or over-run) for 76% of these operating lists.9 Modeling to calculate a surgical suite’s potential reduction in staffing costs are achieved predominantly by reducing allocated OR time.10 Mathematical structures have been developed which could be used to program a computerized surgical services information system to assist in optimizing the sequence of urgent cases.11 OR utilization in such a model was maximized by allocating block time for elective cases based on expected total hours of elective cases, scheduling patients into the first available date provided open block time (available within 4 wk in this case—patients’ desired maximum wait in their survey), and otherwise scheduling patients in “overflow” time outside of the block time. Despite many innovative applications of modeling approaches, there remains a need for advanced planning software for operational decision making.
Advanced Process Combinatorics, Inc. (APC) developed the Virtually Exhaustive Combinatorial System (VirtECS) to help manage resources over a time line. VirtECS provides a highly goal-oriented way of organizing process data. VirtECS was designed for use in manufacturing processes, and uses it in planning industrial and manufacturing plants. VirtECS has capabilities to address the past, present, and future portions of the time line. To do so, VirtECS needs information about process behavior and conditions. VirtECS can interact with a variety of data systems to determine the current state and to compute statistical estimates of cycle times, resource usage, and other basic performance data and publish its predictions. It uses process data to generate a large set of mathematical relationships that incorporate process physics to predict future performance. In fact, VirtECS can very accurately represent behavior over the time line by using Very Large Scale Infinite Dimensional Programming (VLS-IDP) to divide time into infinitesimally small slices. Mathematical relationships are written over each small time slice to enforce real world constraints. VirtECS contains a highly sophisticated technology known as the Extensible Linear Integer Scheduling Engine (ELISE) for simultaneously generating and solving the mathematical relationships. In solving these relationships, ELISE uses company (e.g. hospital) objectives to rate each and every future time line it examines to determine a “very good” time line and the decision choices needed to realize it. ELISE can make a change at an earlier time that is quickly registered at all future times, thus, the ELISE solver can quickly search many alternative time lines to find the best strategy. This mathematical capability was derived from research at Purdue University and over 110 person years of R&D in developing, testing and refining the software.8
In addition to automatically determining a best practice over a single time line, VirtECS can also explore many future time lines that result from process uncertainty.9 VirtECS Simulation-based Optimization (SIM-OPT) provides a means of experiencing a time line the way a hospital might. Initially the ELISE solver is used to generate a plan for the present. The plan is simulated allowing uncertain events to occur. For each time line deviation, the ELISE solver is invoked to determine a new plan that takes into account the realized uncertainty. Many time lines can be generated with different realizations of uncertainty to develop intuition about the range of possibilities that the future might hold. As such, the statistical effect of a certain insurance policy, such as an OR room buffer time, can be quantified. This allows policy decisions to be adjusted rationally to improve overall performance.
We sought to identify key planning scenarios of interest to perioperative leaders and managers, in order to examine the feasibility of solving some of those important planning issues through development of a modeling solution. We identified key determinants of the task flow network, then adapted combinatorial optimization software to the perioperative care setting and assessed the results.
Methods
Needs Assessment
We examined the need for improved planning capabilities for optimizing OR efficiency through key informant interviews and refined the needs identified through an expert consensus approach. We interviewed 11 directors and managers of perioperative service lines at six Midwest hospitals, which represented a range of bedsizes and primary, secondary and tertiary hospitals. We then used a modified Delphi approach to determine big-picture operational and business needs and opportunities.
Key Issues, Metrics, and Desired Services:
Initially, we interviewed six nurse managers (OR Directors) at one academic medical center and three community hospitals with an average of 11 (6–24) operating rooms per site. These OR Directors were responsible for patient care, safety, quality, and satisfaction as well as finance and operations for perioperative services (e.g. preoperative clinics and testing, preoperative units, operating room suites, post anesthesia care units, sterile supplies, and ambulatory surgical centers). We asked these individuals to identify key operational issues of concern, key metrics they used to monitor quality and efficiency, and about what type of services would help them improve work and information flow, as well as operational efficiency.
Our second round of interviews added five new OR Directors at two additional health systems. Questions were based on findings from the first round of interviews and assessed technical capabilities. This round of interviews focused on preferred business case scenarios with questions related to priority, and users of the information and decision support tools. Following completion of the initial qualitative phase of data collection, we analyzed the data to identify key themes of capabilities and features that were desirable. These findings were used to create a survey of 40 potential system features, with items rated on Likert-type scales. Interviewees completed this survey face-to-face with interviewers in order to prioritize challenges, key metrics and top features.
Defining the Task Flow Network
Modeling resource interactions, identifying key system constraints, and building a realistic simulation of an OR required several key subtasks: analysis of historical data; observation of live perioperative systems: categorizing subsystems, actors, key tasks, and data; and creating task flow networks.
Analysis of Historical Data:
Data from (i) a large Midwest tertiary referral hospital (involving complex surgeries across 18 ORs) and (ii) a large city-county safety-net hospital (involving general, trauma, and specialty surgeries across 10 ORs) included 12 months of executed OR schedules for on-time starts, surgery durations (by procedure), and turnover and sterilization times. Discrete event durations were used as input for our scheduling model. Key hospital personnel and subject matter experts helped identify information gaps and/or inconsistencies during observational studies.
We identified a set of performance measures for the perioperative system through literature review, previous work, and expert opinion. These metrics included OR utilization, on-time starts, workload leveling, patient waiting time, and turnover time between cases.
Observations of the Operating Suite:
We observed the perioperative settings at our partner hospitals and mapped out the flow process for each, using rapid ethnography with opportunistic interviews. To configure the simulation model, data and parameters were hybridized from electronic OR schedule data, observational studies, mathematical modeling, and expert review. We focused on key personnel performing critical tasks that often cause changes in the planned OR schedule.10 Lastly, we collected multiple informational artifacts that represented key “State” information including staff schedules, case schedules, equipment lists (case carts), lunch schedules, and work lists.
Discrete Event Network Simulation Model:
We used data from key informant interviews, observations, historical data and artifacts to identify multiple subsystems, data sources, actors, tasks, processes, and constraints within the perioperative system.11 Our task flow network model includes these critical elements and processes and describes key tasks (and their sequences and interdependencies), staff and resource requirements/ availability (e.g. surgeons, anesthesiologists, nurses, equipment, and beds), and supporting elements.12
A discrete event simulation model was developed in AnyLogic to represent patient and workflow in the perioperative system. Different models were created to represent the two different health systems within which we worked. These models were reviewed with senior surgical, anesthesia and perioperative nursing managers and clinicians, to assess the validity of the representations and assumptions. Note: due to space limitations, we present only a small subset. We also conducted a series of financial models to calculate potential return on investment for investment in a new system with the capabilities desired.
Based on these task flow processes, we developed a discrete-event simulation model of perioperative workflow at our partner hospitals. The model considers factors such as patient arrival, registration, beds and staffing in POCU, OR, PACU or ICU, and exit. It can be configured to model a variety of operational and financial outcomes.
Combinatorial Optimization Model
Our goal for this phase of the project was to apply advanced scheduling techniques to the modern operating room (OR) suite, to demonstrate the feasibility of using the software to assist in planning scenarios to consider policy alternatives being considered to improve the efficiency of OR operations. Specifically, we sought to: (i) adapt the VirtECS Scheduling engine for the purpose of scheduling OR suites; (ii) perform scenario analyses; and (iii) compare model solutions to actual scheduling data.
Adapting the VirtECS® Scheduling Engine for the OR
We created a Resource Task Network (RTN) specifically for the OR to formulate a perioperative VirtECS model. OR activities were modeled as a series of related tasks, including staff interaction with patients in the preoperative care unit (POCU), operating room (OR), post-ambulatory care unit (PACU), and intensive care unit (ICU). Surgeons and equipment requirements and availability for each surgery were defined. The scheduling engine was able to produce a quality schedule (albeit a rudimentary one compared to our plans for subsequent development) where all surgeries were completed on the day requested (or as soon as possible). Several modeling features had to be newly developed for OR scheduling. One key concept was that of “block times” which specify a set of ORs, which can only be scheduled within a certain date range for a single type of surgical unit (e.g. neurosurgery). In practice these blocks would be “released” at some time interval prior to surgery so that the set of unused, restricted ORs becomes open to having new surgeries scheduled from any surgical group. Another key implementation issue was the allocation of key personnel, like staff anesthesiologists, at specific points in the surgery (e.g. first and last half-hour). Another issue to consider is whether it would be possible to schedule a group of patients in batches, in order to create a more optimal schedule to meet a specific operational outcome, such as OR utilization, or minimizing overtime.
Results
Our phase-I interviews with OR administrators and managers consistently identified advanced strategic planning and operational decision-making tools as essential, yet unavailable, for optimizing OR efficiency. Specific, high-priority objectives necessary to drive efficiency included: increasing utilization of OR during core hours and decreasing over-utilization (e.g. overtime) during other times; leveling workload (e.g. balancing surgical schedules and staffing with anticipated demand); identifying opportunities for improving workflow; and assessing need and future return on investment (ROI) for additional key resources (e.g. adding anesthesiologists or surgical nurses).
The most critical issues identified by OR Directors included: (1) utilization (to increase the number of cases or new services/specialties); (2) workload leveling (to decrease day-to-day and throughout shift variation in rooms running); and (3) efficiency and workflow (to better use existing staff and resources). Their key performance indicators were similar, and performance metrics were obtained when available, otherwise respondents reported recent estimates. Across all sites, OR utilization (proportion of ORs with cases running during day shift) averaged 60% (30–70%), workload ranged from zero rooms running to maximum capacity (widely variable at all sites), on-time starts averaged 57% (20–80%), and the mean turn-over time was 25.3 minutes (21–30 min.).
Overall highest priorities (Table 1) included: (1) tools to support and/or balance patient and staff scheduling and (2) decision support and analytics for planning perioperative services.
Table 1.
Highest rated planning capabilities needed for improving operative efficiency.
| User | Feature Description |
|---|---|
| OR Director | Ability to identify policy (block scheduling) or process issues impacting utilization/ efficiency |
| OR Director | Ability to identify resource constraints impacting utilization/ efficiency |
| OR Director | Ability to model and perform “What-If?” scenarios |
| Scheduler | Decision support for when and where to best schedule a patient/ case |
| OR Charge | Decision support to schedule staff against forecasted need (demand) |
A model of typical patient flow logic on the day of surgery was developed in our discrete event simulation model. is the model was refined to be more complex, considering the outpatient evaluation, referral patterns, preoperative evaluation, as well as the intrahospital flow, which typically includes a post-anesthesia care unit (PACU), may include intensive care unit and telemetry or general ward stays, prior to discharge and scheduled follow-up. The patient flow also varied, depending upon the type and duration of surgery, the surgical specialty, use of specific implants or devices, intraoperative imaging, pathology and any complications.
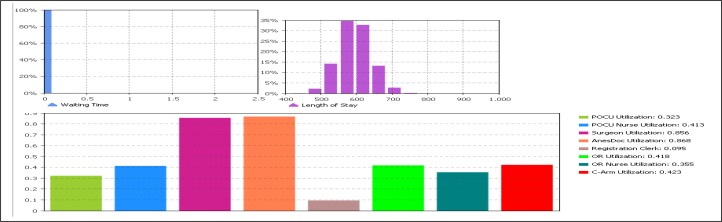
The discrete-event simulation model also displays system performance measures (Figure 1). The first bar chart on the top-left shows the percentage of patients waiting to begin the process. The bar chart (top-right) shows the percentage of patients waiting. The bottom bar chart shows the mean utilization of each critical staff and resource. In this specific snap shot (only one of many modeling scenarios considered), surgeons and anesthesiologists are highly utilized when assigned to OR, while the operating rooms in this scenario had a relatively low utilization (0.42). This increases dramatically as the assumptions are varied and assignment of staff, such as anesthesiologists increase. We were able to explore the impact of various blocking or staffing policies on OR utilization, such as freeing up blocks of time at different intervals before surgery, in order to explore the model’s potential role as a planning, scheduling and policy tool. We found significant increases in OR utilization with variation in policies related to blocking, timing in releasing the blocks, scheduling in batches and based on providing key staffing. Our models confirmed that modest gains in OR efficiency (e.g. optimizing utilization, streamlining patient flow, and redesigning surgical care processes) could significantly increase revenue generation, cost savings, and likely staff and patient satisfaction. These results clearly demonstrated the need for and feasibility of developing and commercializing a set of perioperative optimization tools. Figures 2 and 3 demonstrate combinatorial optimization modeling, using the VirtECS engine for scheduling and scenario analysis (batch scheduling, modified block times, increased staffing), and calculation of metrics of interest to administrators.
Figure 1.
Sample perioperative system performance measures of patient waiting time, length of stay, and staff/resource utilization, according to the discrete event simulation models.
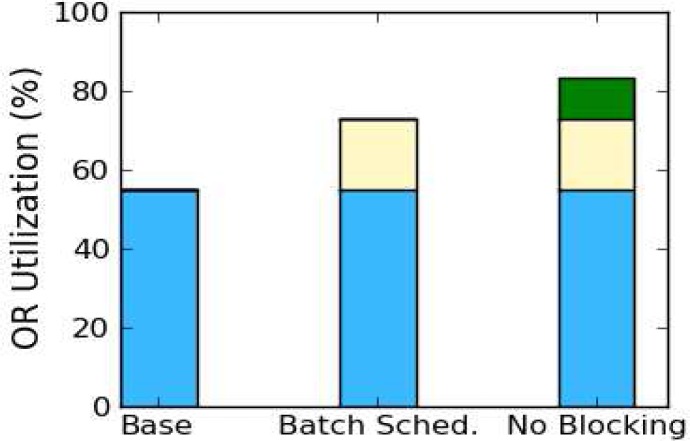
Figure 2.
Scenario Analysis for Utilization
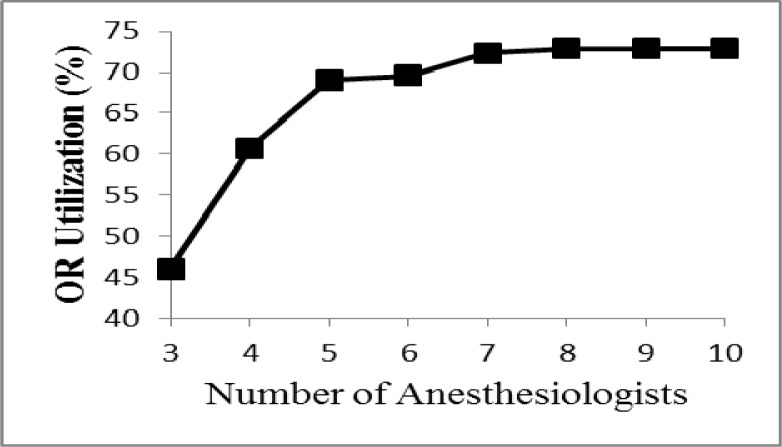
Figure 3.
Utilization vs. Anesthesiologist count
Comparison of VirtECS generated OR schedules to historical schedules
Real schedule data for a two-week period of operations in two separate hospitals were analyzed. The initial models generated similar schedules to those in actual use, when the model was generated with the most restrictive conditions (surgeries scheduled on the requested date, block times in-place, etc.) Review of these schedules by content experts confirmed content validity. Based on our discussions with surgical and anesthesia leadership, the VirtECS model was generated for multiple different case studies (choosing different input values and system constraints), to examine the capability of the software to solve high priority scheduling challenges. This was done to test the ability of the scheduling software to provide quality schedules under a variety of input conditions, and to explore how much improvement might be possible in OR utilization, leveling the operative schedule, and minimizing overtime. Three scheduling scenarios and one planning scenario study are described.
Scenario 1 – Restrictive block times in place, with surgeries scheduled exactly on the date requested by the clinic
This ‘baseline’ case study is closest to the actual approach taken for scheduling the OR at present. Block times are setup, which constrain the use of approximately 75% of the ORs. These blocks correspond to specific ORs set aside for use by units such as Obstetrics, Orthopedics, etc. For these case studies the blocks were always honored.
Scenario 2 – Surgeries batch-scheduled with blocking in place
This scenario considers the impact of rescheduling while keeping the block times in place. A VirtECS model was generated in which surgeries were performed on or before the desired date. The restriction on the scheduled surgery date is lifted so that the improved efficiency of an optimized schedule can be realized. The real data utilized for this study was originally scheduled without the benefit of optimization, and restricting the optimized schedule to recreate the original schedule would yield no benefit in terms of daily OR utilization. However, because the total number of surgeries performed over the two week period modeled is constant, this increased utilization results in the model beginning to run out of surgeries to perform during the seventh day of the schedule. This results in a sudden decrease in apparent OR utilization late in the schedule because the ORs sit idle due to having no additional surgeries available to perform. In practice, utilization would remain high and more procedures could be performed over the period than were during the same two weeks of the base case scenario.
Scenario 3 – Block times removed, surgeries batch-scheduled
This scenario is similar to Scenario 2, except that the Block Time restrictions are lifted. The purpose of this study is to provide an example of the type of analysis that can be performed with the VirtECS Scheduling tool to determine how different schedule approaches may effect OR utilization and patient care. In this case the effect of Schedule Blocking on OR utilization is investigated.
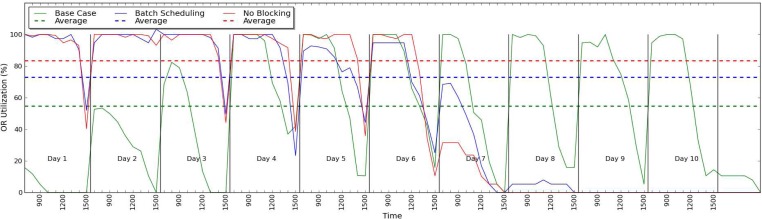
The results of these first three related case studies are shown in Figures 2 and 3. Figure 2 shows the overall OR Utilization measured over the course of their respective schedules. The improvement in overall OR Utilization can be observed for each case of decreasing restrictions on the scheduler, which allows for greater optimization of the schedule. This demonstrates how OR Utilization could be improved with an optimization-oriented approach, and similarly, how analysis of the effect of certain decisions (for example, how to schedule Blocks), could be improved.
Figure 3 shows OR utilization as a function of time over the course of each day of the two week schedules for scenarios 1–3. The utilization of the ORs in the first schedule is strongly limited by the original schedule that serves as the base for this scenario, since the tool is prevented from scheduling surgeries on an earlier day to make more efficient use of available resources.
Figure 2. Summarizes the differences in OR utilization, based on several alternate strategies for scheduling. The first scenario is the baseline, where cases are scheduled no earlier than the day that the surgery occurred in the actual data, and the availability of their time in specific blocks (ie specific days reserved for specific specialties). The second scenario shows the impact of optimizing the schedule, while still honoring the schedule blocks. Tthe third scenario optimizes the schedule, eliminating blocking and scheduling patients in batches, in order to further increase OR Utilization.
Figure 3. The impact of increasing a scarce human resource, number of anesthesiologists, to the point where their availability no longer becomes the limiting factor in a given OR suite, and other factors become limiting.
Scenario 4 – Effect of Additional Anesthesiologists
This is another example of the type of scenario analysis that can be performed with VirtECS. A second site used in this work, but distinct from the case studies above, discussed the constraint placed on their schedules by the availability of Anesthesiologists—VirtECS is capable of handling a wide variety of constraints, and a case study was assembled to measure the effect of the number of available anesthesiologists on the utilization of the ORs. The model used in this case covered a four week period of time, and the surgeries were allowed to be performed as early as possible during the course of scheduling (in order to allow the schedule to be optimized). An Anesthesiologist was required for the first and final half hours of any surgery. The number of anesthesiologists was varied from 3 to 10 while keeping the model otherwise identical and the OR Utilization was calculated for each case.
The results of this study are shown in Figure 4. As expected, OR Utilization increases as a function of the number of Anesthesiologists available but the increase is uneven and remains steady at 73% with 8–10 Anesthesiologists available. Other constraints such as the availability of nurses, PACU, POCU, and ICU units could be explored similarly by VirtECS helping to provide additional information for management decisions.
Figure 4.
Efficiency Metric, based on combinatorial optimization models, using VirtECS. Here OR Utilization (proportion of day between 7:30am–3:30 pm where the OR is occupied with an ongoing case), as a function of time.
Although this software is an early version, it finds optimal solutions within a few seconds. Whereas the scenarios we tested were relatively simple, the optimized schedules are considerably different from existing schedules, in that there is both greater use of operating rooms and key personnel, as well as overall utilization of the OR suite. The schedules developed under different assumptions of resource availability and policy changes put into place were reviewed by content experts in surgery, anesthesia and OR nursing. These experts confirmed that the schedule solutions were both practical and modeled utilization varied as expected, based on expected relationships between resources and efficiency. These findings showed face and content validity.
Discussion
Perioperative leaders desire a broad range of decision support tools for planning and decision support. Our study identified a series of subsystems within the perioperative system, each with its own key determinants and constraints. Furthermore, this study demonstrated the feasibility of applying combinatorial optimization modeling to evaluate policy and practice alternatives to support key decisions to improve care efficiency. These findings demonstrate that the tool has obvious benefits both for tactical decision making (e.g. making up a more efficient schedule from the perspectives of the hospital, patients and providers), as well as in strategic decision-making (as open versus block scheduling, number of nursing and anesthesia staff to be scheduled, etc). Our research confirms and expands the work of Testi and Tànfani who used linear programming and combinatorial optimization, focused on perioperative “outcome” from a societal perspective (health improving or preventing from worsening) rather than on “output” (delivered procedures).15
Optimizing operating room (OR) efficiency has the distinct potential to level care demand and normalize workload, resulting in less overtime, fewer cancelled shifts, less resource strain, and increased staff satisfaction. Furthermore, leveling surgical demand should enable better coordination and allocation of limited human and technical resources for delivery of safe and effective care. Our financial analyses demonstrated an expected significant impact on hospital financial outcomes from optimizing OR scheduling. Additionally, an optimized OR should create a patient-centered environment, where special needs and preferences can be addressed for individual patients.
Apart from financial gains, optimizing OR efficiency minimizes waits, delays, and scheduling inefficiencies that improve overall patient and staff satisfaction. Surgical personnel who are not overworked are less likely to change jobs; patients who are not left in waiting rooms or perioperative areas are more satisfied and less likely to change providers. Hospitals and their communities benefit from improved staff and patient satisfaction because healthcare providers stay and patients continue to call on them. Furthermore, optimized OR efficiency will have a significant impact on improving mortality, morbidity, and quality of life – all major indicators of quality healthcare.
The initial hospital scheduling model (and underlying algorithm) developed here needs to be refined for deployment within a live OR environment. There are three primary refinements needed for this: Staffing and room constraints must be applied within the model. There are hard limits on the suitability of certain rooms for specific surgery types when a dedicated piece of equipment (e.g. DaVinci machine) is required. In addition, staffing requirements are very important, especially anesthesiologists, nursing staff, and surgeons. The OR availability of individual surgeons must be considered for realistic scheduling.
Block times for departments are also an important consideration. Currently each individual unit (e.g. neurosurgery) has specific blocks of time in one or more OR rooms, which are not free to be requested by other units until a specific ‘release time’ (e.g. one week before the date of surgery). Block times have been used historically to manage the complexity of scheduling, but reduce the efficiency of the schedule. During phase I, a basic approach to managing block times was developed, but this needs to be refined to be more flexible and realistic.
The scheduling process involves more than just the software application – it is the set of all procedures and policies (formal and informal) used by agreement of the hospital OR scheduler and the individual surgery groups. Currently, a clinic may call to request a specific surgery on a given date and a slot is assigned if there is room within that unit’s block time, or if there is a free room available. These times are assigned on a first-come-first-served basis. This approach to scheduling, while natural, does not result in an efficient or high utilization schedule. In Phase-II, we will work with managers and clinicians to develop a scheduling process acceptable to the hospital, patients and staff, which allows for rescheduling and optimization. Another task will be to progress from generating schedules from blank slates to a dynamic rescheduling process, where requests for new surgeries (and cancellations) are occurring on a frequent basis. This tool should be useful in a range of tactical decisions that need to be made daily. From a tactical perspective, it should help with issues such as optimal sequencing of urgent cases to enhance patient safety, reduce surgeons’ complaints, and increase patient satisfaction with surgery timeliness.
The second important practical application of our software package is planning and scenario analysis. From a strategic viewpoint, it may help with determining issues, such as the appropriate amount of block time to allocate to surgeons and selecting the days on which to schedule elective cases can maximize operating room (OR) use. The software is used here to answer questions, such as: What would be the effect of adding one anesthesiologist (or an additional on-call team) to the roster? What impact would an alternate method of reducing ‘block time’ have on OR utilization? Addressing variability is also important, as the hospital will want to insure quality control when they make a policy change. Monte Carlo simulation will be used to consider variance in surgery duration to answer questions, such as: How often will long duration surgeries lead to an end-of-day cancellation for a patient (or staff overtime)? These are very important issues for hospital leaders to consider. There is great value in obtaining reliable answers to such questions and maintaining some excess staff capacity to handle worse case scenarios (e.g. emergency cases).
Successful implementation of our software is dependent upon the availability and accuracy of specific input data regarding surgery attributes, resource availability, room constraints, and other process variables. Our standard approach to VirtECS solutions involves the development of a ‘model manager’ which combines a data viewer/editor as well as database (back end) for storage and data management. Since we will ultimately be pulling in data from several different sources (as each hospital will have several systems), we will transform data into a standardized VirtECS model format. Our program interfaces with a number of data management systems, such as SAP. Based on our experience with the software in other settings considering multiple complex variables, run time is not expected to be a significant factor impacting its use.
One major practical consideration for deployment of a software package for use in hospital planning and scheduling is the need to develop a graphical user interface (GUI) that is specifically designed to address hospital-scheduling procedures. VirtECS scheduling projects have been developed for manufacturing applications. Some aspects of the current GUI are unnecessary in hospital scheduling, while certain necessary controls are lacking. For example, in early iterations, it will likely not be necessary to track inventory of materials in OR scheduling (although we expect, eventually, to track supplies of surgical inserts and devices), but a dedicated panel is required to manage the blocking schedule. Design of a GUI will be completed, while working in concert with Engineering Healthcare Solutions and hospital staff in live environments – tailored to the needs of individual users, whether for daily scheduling or long term planning. The GUI must also deal with unforeseeable needs (e.g. emergency and transplant procedures).
Validation is crucial for the commercialization of our software package because hospital decision makers must have confidence in the schedules and planning recommendations made by our tool. We plan further validation through a combination of the following: (i) creating a “test suite” of scenarios, which updated versions of the Scheduler must pass; (ii) developing through iterative models to ensure that all real-world constraints are accurately modeled and considered within the solution algorithm; and (iii) comparing model-generated schedules to actual schedules.
Conclusions
Perioperative care is complex and involves multiple interconnected subsystems which are a microcosm of the hospital. Delayed starts, prolonged cases and overtime are common. Surgical procedures are major drivers of patient morbidity, mortality, satisfaction, and overall hospital costs and profitability. We sought to determine key planning scenarios of interest to perioperative leaders, in order to examine the feasibility of solving some of those important planning issues by applying combinatorial optimization software to the operative setting. Perioperative leaders desire a broad range of decision support tools for tactical and strategic planning.
This study demonstrated combinatorial optimization modeling can effectively evaluate planning alternatives to support key policy and practice decisions. Successful implementation will depend upon the availability and accuracy of specific input data regarding surgery attributes, resource availability, room constraints, and other process variables, development of a useful GUI, as well as successful tests of its capabilities in the real world OR environment. Our study demonstrates the value of modeling to evaluate policy and practice alternatives to support key decisions to improve planning, clinical workflow, improving care efficiency and satisfaction.
Table 2.
Examples of key model components (subsystems of the perioperative system), key data elements, and sources of the data. Note: this table is considerably simplified for ease of presentation.
| Model Component | Data element | Source |
|---|---|---|
| Patient arrival to OR | OR schedules | OR scheduling system |
| Scheduling process | Observation and interview of OR schedulers | |
| Peri-op overall process | Process flow | Interview of leadership, observation |
| Resource arrangement | Staffing (surgeon, anesthesiologist, nurse, technicians) | Interview of key staff members |
| Equipment | Interview of key staff members, observation | |
| Beds | Interview of key staff members, observation | |
| Peri-op physical layout | Peri-op facility layout design | Peri-op leadership |
| Service rate | Tasks and time for tasks | Observation |
| Surgery time | Surgery duration | Historical OR schedules |
Acknowledgments
This work was supported by the National Institute of Health (NIH) Small Business Technology Transfer Research (STTR) phase-I funding. We appreciate the input of our patients, surgeons, anesthesiologists, nurses and other staff.
References
- 1.Services, Office of Information. Inpatient surgery. [Online] 2007 http://www.cdc.gov/nchs/fastats/insurg.htm.
- 2.Cullen KA, Hall MJ, Golosinskiy A, Division of Health Care Statistics National Health Statistics Reports, #11, Revised September 4, 2009. US Outpatient surgeries on the rise [Online] CDC National Center for Health Statistics, Office of Communication, 2009. http://www.cdc.gov/nchs/pressroom/09newsreleases/outpatientsurgeries.htm.
- 3.(AHRQ), Agency for Healthcare Research Quality 2004. Statistical Brief #164. Medical Expenditure Panel Survey. [Online] www.meps.ahrq.gov/mepsweb/data_files/publications/st164/stat164.pdf.
- 4.Premier, Inc., Charlotte, N.C. HBS International, Bellevue, WA . Surgical services reform Executive Briefing for Clinical Leaders. Washington, D.C.: Clinical Advisory Board; 2001. [Google Scholar]
- 5.Litvak E, Long MC, Cooper A, McManus M. Emergency department diversions: Causes and solutions. Academic Emergency Medicine. 2001;8:1108–1110. [PubMed] [Google Scholar]
- 6.Vargas LG, May JH, Spangler W, Stanciu A, Strum DP. Operating room scheduling and capacity planning. In: Rushkin J, Stonemetz K, editors. Anesthesia Informatics. sl. Springer; 2008. p. 19. [Google Scholar]
- 7.Davenport TH, Short JE. The new industrial engineering: Information technology and business process redesign. Slogan Management Review. 1990. pp. 11–27.
- 8.Pekny Joseph F. Algorithm architectures to support large scale process systems engineering applications involving combinatorics, uncertainty, and risk management. Computers and Chemical Engineering. 2002;26:239–267. [Google Scholar]
- 9.Pandit JJ, Tavare A. Using mean duration and variation of procedure times to plan a list of surgical operations to fit into the scheduled list time. Eur J Anaesthesiol. 2011 Jul;28(7):493–501. doi: 10.1097/EJA.0b013e3283446b9c. [DOI] [PubMed] [Google Scholar]
- 10.Dexter F, Macario A, Traub RD. Optimal sequencing of urgent surgical cases. Scheduling cases using operating room information systems. J Clin Monit Comput. 1999 May;15(3–4):153–62. doi: 10.1023/a:1009941214632. [DOI] [PubMed] [Google Scholar]
- 11.Dexter F, Macario A, Traub RD, Hopwood M, Lubarsky DA. An operating room scheduling strategy to maximize the use of operating room block time: computer simulation of patient scheduling and survey of patients’ preferences for surgical waiting time. Anesth Analg. 1999 Jul;89(1):7–20. doi: 10.1097/00000539-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Miller DL, Schertz D, Stevens C, Pekny JF. Mathematical programming for the design and analysis of a biologics facility: The use of mathematical programming methods for automated schedule generation. BioPharm International. 2012;23:654416. [Google Scholar]
- 13.Burton MM, De-Laurentis PC, Wiebke E, Ekbia HR, Lawley M, Doebbeling BN. Clinical workflow: A systems lifecycle approach. Rochester, MN: Mayo Clinic Conference on Systems Engineering and Operations Research in Health Care; 2010. [Google Scholar]
- 14.Burton MM, Doebbeling BN. Understanding how we care for patients: Information needs and best practices for capturing clinical workflow. Washington, DC: AMIA Annu Symp Proc; 2010. [Google Scholar]
- 15.Testi A, Tànfani E. Tactical and operational decisions for operating room planning: efficiency and welfare implications. Health Care Manag Sci. 2009 Dec;12(4):363–73. doi: 10.1007/s10729-008-9093-4. [DOI] [PubMed] [Google Scholar]