Abstract
Inadequate organ donation limits transplantation for many in need of a life-saving organ. Race of donor families and requesting coordinators may impact the authorization rate for organ donation.
We evaluated authorization rates for organ donation within the New York Organ Donor Network by race during 2009 and 2010. The donation authorization rate varied considerably according to the race of the donor. The authorization rate was 57% for Hispanic, 53% for Caucasian, 48% for African-American, and 23% for Asian donor families. Fifty-five percent of donor families agreed to donation when there was racial concordance between coordinator and donor. Donation authorization was 49% when a racial mis-match existed. When adjusted for coordinator training and experience, racial discordance had a lesser impact on authorization rates.
Our findings suggest the need for education and communication strategies to overcome racial-associated perception during the organ donation process.
INTRODUCTION
More than 30,000 Americans and more than 1 million persons worldwide die each year from complications of liver failure (1, 2). In the United States alone, the prevalence of liver disease exceeds 20 million and the number of newly diagnosed patients with liver disease has not been decreasing (3). Available treatments are often inadequate and unsuccessful in halting the progressive nature of end-stage liver disease (ESLD), ultimately leading to the need for organ transplantation to prevent death. As of August 2011, there were 16,178 people on the national liver transplant waiting list, whereas approximately only 6,000 liver transplants are performed each year throughout the country (4). This large discrepancy means that nearly two-thirds of these patients continue to be medically managed while awaiting transplantation; approximately 10% of them die each year awaiting this potentially life-saving surgical therapy (4). The considerable disproportion between those requiring liver transplantation and organs available for transplantation directly impacts survival for patients with ESLD. This organ shortage is primarily due to a lack in organ donation. Reasons for the hesitancy to donate are numerous, but likely include the public's general lack of awareness regarding the transplantation process, personal biases, cultural differences, and racial disparities (5, 6, 7). Understanding the issues surrounding this limitation is essential to improving efficient delivery of organs for transplantation and perhaps to increasing the pool of available organs.
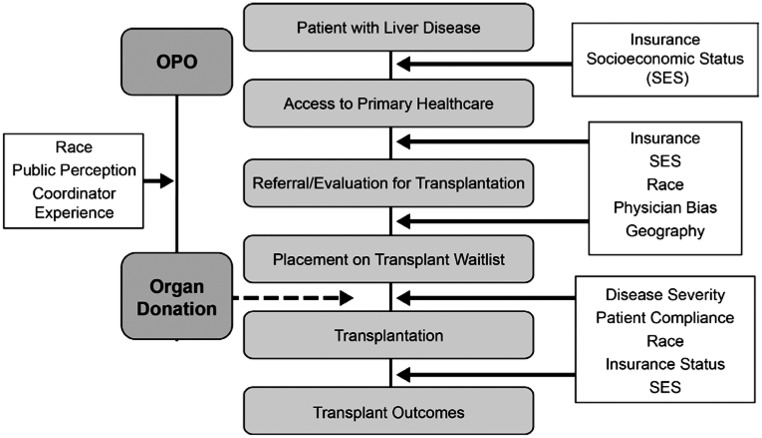
A potential need for organ transplantation begins with the onset of disease and diagnosis by a primary care physician (Figure 1). As disease progresses, patients are referred to specialists who may refer the patient to a transplant center for evaluation for placement on a transplant waitlist. Natural progression of disease, efficiency of diagnostic and therapeutic evaluations, appropriate and timely referral to specialists, and both patient and physician preferences each influence the efficiency of establishing transplant candidacy (8, 9). Once referred to a transplant center, patients undergo an extensive medical and psychosocial evaluation to determine whether or not they will be appropriate candidates for transplantation. Factors examined include social support and financial ability to pay, not only for the transplant itself, but related costs such as medications, transportation, home care, etc. Once a patient meets criteria to be placed on a transplant waitlist, he or she must wait to receive a suitable organ offer at a medically appropriate time. Although the determination of who eventually receives a transplant is highly regulated, the steps leading up to transplantation allow external factors such as financial, geographical, and personal bias of patients and care-givers to enter into the process. Race, socio-economic status, and patient and physician attitudes have all been shown to significantly impact this process (9–12).
Fig. 1.
Factors impacting the organ transplant process (OPO, organ procurement organization).
Liver transplantation makes use of the MELD (Model for End-stage Liver Disease) scoring system to objectify the organ allocation process. All deceased organ allocation in the United States is regulated by the United Network for Organ Sharing (UNOS), and organs are procured by a donor service-area based organ procurement organization (OPO) to facilitate the allocation of organs in a fair and appropriate manner. While on the waitlist, however, many patients become too sick to survive a transplant or die while waiting to receive one, which is where the importance of organ availability plays a central role.
Solid organ transplantation has been constrained by the limited availability of organs. An intervention to overcome this shortage would be aimed at increasing the rate of organ donation. Insights into the reasons individuals, or their families, choose to volunteer for or decline to donate are speculative, but analyzing the donation process may provide insight into methods for optimizing the process of obtaining donation authorization. Minorities have been shown to donate in fewer numbers than Caucasians (13). Individuals who are older than 50 years of age and the chronically ill less often authorize to donate as well (14). Few studies, to date, have specifically investigated the associations between those obtaining authorization and potential donors. Because the dialogue between these two groups delves into sensitive and intensely personal beliefs, developing a better understanding of their relationship may provide beneficial information to better structure the organ donation process. We sought to determine whether coordinator race and race of the potential donor had any effect on donation authorization rates. With the presence of such a link, OPOs may modify their procedures of approaching authorizing individuals to obtain better outcomes. Specific educational initiatives may be used for professionals to better understand cultural beliefs, and alternatively, potential donor families may be approached in an increasingly culturally sensitive manner. Public awareness of the need for organ donation may increasingly address issues of concern related to cultural beliefs. If we understand how to increase organ donation rates, and thereby the number of viable organs available for transplant, we may impact the rate of candidates dying awaiting organ transplantation.
METHODS
Study Population and Procedure
The process of organ donation is typically not organ-specific, and one donor may provide multiple life-saving organs to several recipients. We have the greatest familiarity with the process of liver transplantation, and use this as the example to show specific factors potentially influencing the complex process of organ donation. Certainly any impact on organ donor authorization would have an impact far beyond liver transplantation.
The New York Organ Donor Network (NYODN) is a non-profit, federally designated OPO that serves the greater New York metropolitan area. The organization is the second largest in the country and covers a potential donor population of more than 13 million people, comprising one of the most ethnically diverse populations in the country. The OPO is responsible for the procurement and allocation of organs throughout its geographic donor service area. UNOS, a governmental organization responsible for overseeing and maintaining the transplant waiting list, determines the regulatory elements serving organ allocation. At the time of our study, NYODN employed 60 coordinators who were of varied racial and ethnic backgrounds including Caucasian, African American, Asian, and Hispanic. Beginning in 2007, NYODN established a database to record potential donor characteristics as well as age and racial/ethnic characteristics of the coordinator responsible for the donor cases. Each coordinator is typically assigned to a particular region within the network, and it is his or her responsibility to oversee the authorization for organ donation in that area.
When a potential organ donor is identified, the coordinator is dispatched to the site where they will speak with the family/healthcare proxy regarding organ donation. At times, an immediate decision is made to authorize for organ donation or to decline, but often families wish to further contemplate the decision. In some instances, a different coordinator is sent to the site to complete discussions with the family, thus multiple coordinators may be involved in the authorization process. When this occurs, the encounter is considered to have “multiple approachers,” whereas a case for which only a single coordinator is involved (even if they return at a later time to speak with the family) is considered a “single approacher.” NYODN employs two types of coordinators, Family Service Coordinators (FSCs) and Transplant Coordinators (TCs). FSCs are highly trained coordinators who have extensive experience dealing with families and discussing end-of-life decisions. TCs are also trained to support families during the authorization process, but they are registered nurses who are primarily focused on the medical management of the potential donor. We conducted a retrospective data review of individuals who were referred to NYODN as potential organ donors between January 1, 2009, and December 31, 2010. Potential donors were excluded from our study if they required an approach by more than one coordinator before making the decision to donate or decline, or if their race was unknown. Data was not available regarding the race or ethnicity of the authorized party (i.e., the potential donor's family or health care proxy).
Coordinators collect potential donor data including medical diagnoses, age, and race. Subject race was obtained via hospital intake forms in most circumstances. If that data was not available, the TC determined the designation of donor race. All ages were included in this study. Coordinator race was self-identified by the coordinators themselves.
We sought to define the frequency of authorization for donation by potential donor race. Additionally, we examined the relationship between concordance of coordinator and potential donor race in terms of authorization.
The Beth Israel Medical Center Institutional Review Board reviewed and authorized this study by an exempt review procedure.
Statistical Analysis
Data were analyzed using the SAS/STAT software, version 9.2, SAS Institute, Inc., Cary, NC.
Descriptive statistics included counts and percentages for categorical variables and means and standard deviations for normally distributed continuous variables. Bivariate analysis was conducted using chi-square and Fisher's exact tests for categorical variables. P values of <0.05 were considered statistically significant. All analyses conducted are considered exploratory and hypothesis generating.
For all cases in which race of both donor and coordinator was available, we determined race concordance between donor and coordinator. Chi-Square statistics were conducted to assess the association between race concordance and authorization rates of potential donors.
RESULTS
The characteristics of potential donors as well as those of NYODN TCs and FSCs employed at the time of this study are reported in Table 1. Half of the coordinators were Caucasian and most of the remaining coordinators were African American or Hispanic, also reflecting the population of potential donors.
TABLE 1.
Characteristics of Coordinators and Potential Donors
| Race | Age | |
|---|---|---|
| Characteristic | n (%) | Mean ± SD |
| Coordinators (n) | 60 | |
| Asian | 4 (6.67) | 33.66 ± 3.92 |
| African-American | 13 (21.67) | 40.35 ± 7.31 |
| Caucasian | 30 (50) | 42.72 ± 5.84 |
| Hispanic | 13 (21.67) | 38.12 ± 9.83 |
| Potential Donors (n) | 907 | |
| Asian | 57 (6.28) | 57.61 ± 16.22 |
| African-American | 271 (29.88) | 52.16 ± 17.45 |
| Caucasian | 375 (41.35) | 54.51 ± 17.8 |
| Hispanic | 204 (22.49) | 50.19 ± 19.27 |
From January 1, 2009, through December 31, 2010, 1,244 cases were referred to the New York Organ Donor Network. The vast majority of these cases (98.3%) involved NYODN coordinators obtaining authorization, whereas 15 cases were either family initiated or hospital personnel approaches. To study the relationship between race concordance and the agreement to authorize donation, we selected only those records for which families authorized donation through a single coordinator.
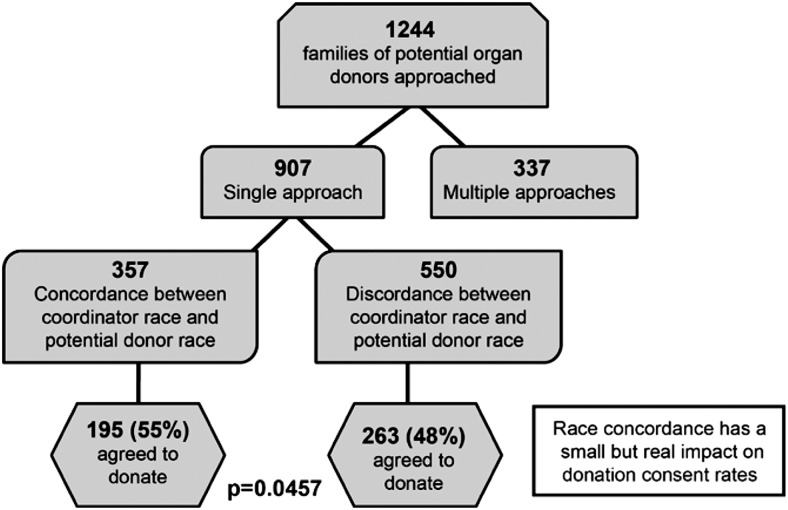
Of the 1,244 cases available for analysis, 907 (72.9%) were approached by a single coordinator, were family initiated, or were hospital approaches, whereas 337 (27.1%) cases had multiple coordinators involved before a decision was made to donate or decline. Among the sample of 907, for 15 (1.7%), either the race of the approacher was not available or the family initiated authorization.
If we assume race discordance for the 15 cases in which coordinator data was not available, 357 cases (39%) had a concordance between the coordinator race and the potential donor race and discordance was found in 550 (60.6%) cases. For the cases in which concordance existed, 195 (54.6%) authorized donation, whereas in the group without concordance between races, 263 (47.8%) agreed to donate (P =0.046). These results show a small but significant difference in authorization rate based on concordance of race (Figure 2).
Fig. 2.
Potential donors assessed in the analysis of rates of donation authorization by concordance versus discordance of race. Refer to the text for additional analyses excluding cases of uncertain concordance.
When the 15 cases of uncertain racial concordance (1.7% of 907) are removed from the analysis, 892 remain, of which 357 cases (40%) had a concordance between the coordinator and the potential donor's race and 535 (60%) did not. In the concordant group, 195 (54.6%) authorized donation as compared to 260 (48.6%) in the discordant group (P =0.078).
Both analyses are consistent with a modest difference of 6% to 7% in authorization rates of agreement to donate between the racially concordant and discordant groups. A larger sample would be needed to have sufficient power to detect a difference of 6% between the concordant and the discordant groups.
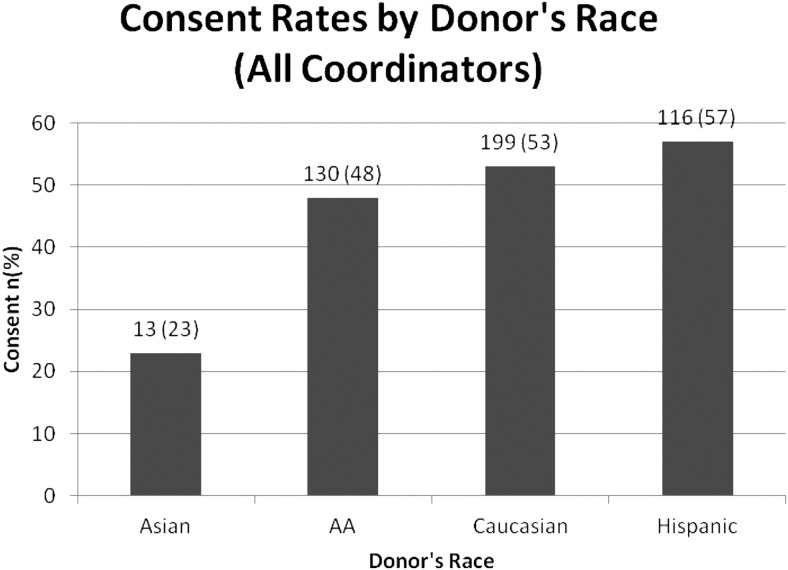
To explore the association between potential donor's race and agreement to donate we analyzed data on all 1,244 cases available. We found that families representing Asian potential donors had a lower consent rate (23%) than did African Americans (48%), Caucasians (53%) and Hispanics (57%) (P <0.0001) (Figure 3).
Fig. 3.
Donation authorization rates of all coordinators by potential donor race. Numbers on columns indicate number of potential donors, and (n) indicates authorization to donate rate.
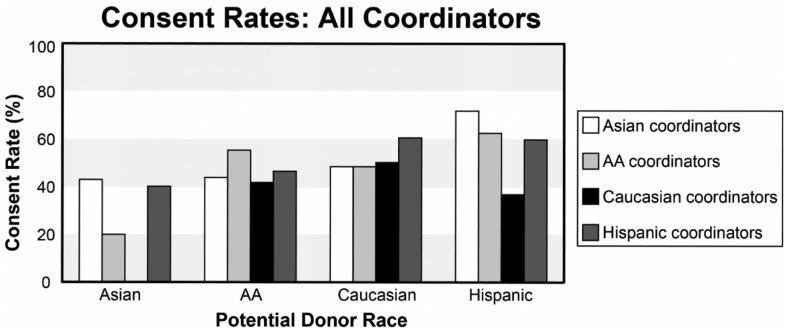
We further stratified our data by race/ethnicity of authorized representative and also by FSC. We assessed the success of coordinators of a particular race in obtaining organ donation consent from authorized persons. This analysis is shown in Figure 4. Asian potential donors consent the best to the Asian coordinators (43% consent rate), followed by Hispanic coordinators (40%), and these are significantly different from the 0% consent rate by Caucasian coordinators. African American potential donors consent the best to African American coordinators. Caucasian potential donors consent the best to Hispanic coordinators. Hispanic potential donors consent the best to Asian and African American coordinators.
Fig. 4.
Donation authorization rates of all coordinators by coordinator race and potential donor race.
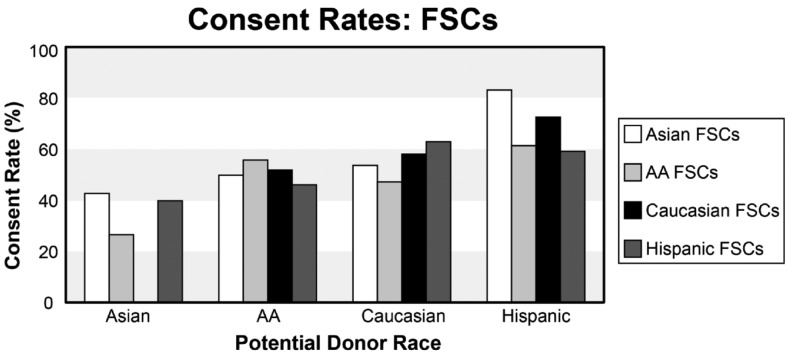
Finally, we wanted to determine whether coordinator training might impact the role of race in the authorization process. FSCs undergo extensive training in communication and have a wealth of experience in this regard. Thus, we analyzed the subgroup of FSCs by potential donor's race (Figure 5). Our findings suggest less variability in authorization rates of FSCs when stratifying by potential donor's race, suggesting that coordinator training might alter the relationship between race and agreement to authorize donation.
Fig. 5.
Donation authorization rates by Family Service Coordinator (FSC) race and potential donor race.
DISCUSSION
Our results suggest that racial concordance plays a role in the rate of authorization for organ donation. Our data is consistent with variability in rates of agreement to donate among the various racial groups. Our data also suggest that training and experience of transplant coordinators can minimize the impact of race and maximize organ donation rates. Organ donation is an extremely complex process, addressing sensitive issues and values. Understanding racial and cultural attitudes towards the donation of organs may help to increase authorization for donation and close the gap between organ need and availability.
The fact that race plays a significant role in organ donation rates is not surprising given the impact that race and culture have shown to exhibit at every stage of the transplant process from etiology and prevalence of disease (15) through time spent on a waitlist (16) and post-transplantation outcomes (17). Being of African American descent is associated with a decreased likelihood of being referred to a transplant center (9) and being listed for transplantation, but it is also associated with a greater likelihood of refusing to donate an organ (18). These findings should not be considered unconnected. African Americans present to transplant centers with more advanced disease and at younger ages than their Caucasian counterparts. This comes at a great detriment to African Americans, as they have less opportunity for conservative medical management and the possibility to undergo transplantation at the most opportune time. The Milan criteria provides an established set of parameters in which patients with hepatocellular carcinoma may be eligible for transplantation early in the course of their disease with the intent of curative intervention (19). African Americans present to transplant centers with disease exceeding the Milan criteria at rates greater than similar Caucasian patients (10). This tendency to present at a later stage of disease may be explained by lack of access to primary care, but may also reflect variability in health care practices, socio-economic factors, and personal preferences on the part of patients. African Americans are less likely to be referred to transplant centers and may have worse outcomes after transplantation (9, 17). Possessing only public insurance was also associated with presenting for transplant with a higher MELD score and decreased likelihood of receiving a transplant (8, 11, 20). Minorities are less likely to purchase private insurance and the prohibitive cost surrounding a transplant may discourage physicians from referring their patients. As African Americans perceive that they are not full participants in receiving transplants, they may be less willing to donate organs. African Americans are likely not to know that, as a group, they have a greater need for transplanted organs (18).
Barriers to organ donation vary between individuals, as personal experiences, biases, and knowledge base are central to the decision-making process. A general lack of awareness of transplantation is a major hurdle to familiarizing people with the concept of organ donation. A surprising study found that a majority of patients obtained information regarding organ transplantation from the Department of Motor Vehicles rather than health care providers (21). In that same study, 89% of participants stated they would be more comfortable discussing matters regarding organ donation with their primary physician than with a government employee. Limited time available during primary care office visits may, in part, explain the lack of discussion of organ donation. Some physicians may also have a lack of knowledge regarding the transplant process based on their medical training or personal experience.
Lack of knowledge regarding transplantation was specifically found among minority groups, particularly African Americans (22), which may explain our finding of lower authorization rates among this population. African Americans have been found to have little knowledge regarding the various organs able to be transplanted and were less likely to know about the existence of organ donation cards. Educational programs should be targeted to these specific populations to enhance the process of organ donation and promote the benefits of giving an organ. Donation rates are also increased when conversations regarding potential wishes were discussed before a devastating event. Discussion with family members about wishes to donate is less frequent among African American, Asian American, and Latino American families than European Americans (23). In our study, however, we found that Hispanics had the highest authorization rates. This may be a reflection on the quality of the coordinators and their ability to resonate with this population.
Language and cultural understanding are important tools for communication. Respecting the cultural nuances and expectations of individual groups is critical in this context given the sensitive nature of these encounters. Transplant coordinators receive extensive training on how to approach end-of-life issues with a grieving family while stressing the importance of organ donation. An untrained individual may inadvertently not address specific concerns held by certain cultures, possibly leading to misunderstandings and misinterpretations among some groups. Our data support the importance of experience, training, and cultural sensitivity relating to this issue.
Misconceptions regarding the transplant process are also a major deterrent to interest in organ donation. Some individuals fear that they or their loved ones will not receive proper care if their organs are designated for donation. Other fears include the premature determination of death or that the patient will actually experience the pain of organ procurement (24). There is a widespread perception that the organ distribution system is unfair and that organs primarily go to the wealthy and white (25, 26). The MELD scoring system, for example, was instituted in February 2002 to establish a more objective criteria in predicting mortality from liver failure and to identify those patients who would most benefit from a liver transplantation. Criteria for MELD include measurements of International Normalized Ratio, serum creatinine, and bilirubin. Before the introduction of MELD, African American race was associated with a lower rate of being listed for transplantation. African Americans, once listed, were also found to be more likely than Caucasians to die on the waitlist. After the implementation of the MELD scoring system, African American ethnicity was no longer associated with an increased risk of mortality or of dying on the waitlist (16, 27). Strong efforts have been made to identify and correct these disparities. The presence of bias may disillusion minorities from trusting in the medical establishment. Higher concordance of authorization with coordinators of the same race may be a manifestation of this mistrust, which is overcome by identifying with a coordinator of a similar background.
Our study has several limitations. We relied on retrospective data, we focused on single approachers, and, most importantly, our race variable reflects race of donor, not that of the authorized party. Although an assumption can be made that the race of the authorized party is the same as the potential donor, we could not, with certainty, determine whether or not this was the case. Furthermore, the determination of race was made by the coordinator, or as indicated on hospital intake forms and one assumes variability in the way these data were obtained. As race may not have been self-identified by the potential donor, we cannot be certain that the recorded race was that which the potential donor might have self-identified.
Our analyses are considered exploratory and hypothesis generating. Further analysis is needed to understand the relationship between coordinator's race and that of the potential donor families and how this might influence agreement to authorize organ donation. We also need to explore the influence of confounding variables. Future studies need to explore the role of training as well as control for the role of phone contacts, as well as age and gender differences. Prospective data collection may help to more precisely understand the role of a coordinator's race in a family's decision to donate.
Increasing awareness of transplantation and the importance of donation is a crucial factor in increasing the availability of viable organs. While education should be aimed at the general public and specifically to minority communities, open dialogue should also be fostered among healthcare professionals to emphasize the importance of referral, education, and discussion of these sensitive issues with patients. Adjusting OPO protocols to maximize the effect on donation rates may be a powerful initial step. By intervening, increasing awareness, and perhaps modifying our strategies to approaching patients, we can overcome the rate-limiting step of lack of organs and increase organs available for transplantation.
Race impacts personal behavior including authorization for organ donation and must be addressed in managing organ transplantation. All involved should effectively participate in the organ donation process so as to make it fair and equitable and to increase the numbers of organs available for transplant. Understating the limitations of our knowledge of the decisions to authorize donation of organs may allow us to alter our approach to most effectively increase organ donation rates.
ACKNOWLEDGMENTS
The authors acknowledge the collaboration of the leadership of the NYODN on this project. We are particularly grateful for the support of Helen Irving, Elaine Berg, and Harvey Lerner.
Footnotes
Potential Conflicts of Interest: None disclosed.
DISCUSSION
Makowiak, Baltimore: You mentioned socio-economic status sort of at the end of your talk. I didn't notice that you had controlled for that in your analysis. Obviously, it raises a complicated issue about how individuals choose to declare and assign themselves to a particular race when they are of a mixed background. Some people would suggest that really the types of differences that you observed here are totally socio-economic. I was wondering what happens if you reanalyze your data controlling for socio-economic status?
Bodenheimer, New York: We are in the process of extending our observations. There are additional studies in the literature pertaining to the impact of socio-economic status and transplantation. Our analyses in the future may look at zip code to the extent that this information is available. Acquisition of data is limited by the context of seeking consent for organ donation at the time of a loved one's death. Observations by others have looked at this and found that socio-economic status does have a significant impact on access to transplantation, and it appears to be independent from race. One additional question that we explored was not only consent for donation by race, but also the concordance or discordance of race between the coordinator asking for donation and the potential donor. This analysis has not been looked at stratified by socio-economic status of the potential donor, partly due to smaller numbers of observations available for analysis as data are subdivided.
Weir, Baltimore: Interesting presentation. I was wondering: have you adjusted your data for renal function? Because this really does make such a powerful impact on liver transplantation since we do have alleles for ABL1, in particular in African heritage patients, which clearly predispose to increasing problems with kidney function over time.
Bodenheimer, New York: You are talking about success following transplant?
Weir, Baltimore: Right.
Bodenheimer, New York: To my knowledge, the observations of the success of liver transplantation by race were not controlled for renal function. Separate investigators have controlled for hepatitis C and found that in the non-hepatitis C transplant population, they were not able to demonstrate a difference in outcomes by race in liver transplantation. This observation implies that a major component of liver graft failure in African Americans versus whites post-transplant may be related to racial disparity in the natural history or management of hepatitis C.
Weir, Baltimore: Yeah, and the other thing may very well be the heritage of the liver donor in the sense that we now have data showing that, in fact, the liver donor, if they are of African heritage, actually makes circulating proteins and there may be some concern that this could have influence subsequently on the kidney function of the recipient. So, again, that may be one other confounding variable to look at within your data set.
Bodenheimer, New York: Those are valuable observations. Individuals have looked at really two questions in terms of race and the actual transplant process. One was: does concordance or discordance of race in the donor-recipient match make a difference? And second: does any organ of a particular race behave less well? The data in this regard are actually conflicting. There are papers on both sides saying whether that has a significant impact. There was a series of papers showing that discordance of donor-recipient race might have a deleterious effect on graft survival, but this observation was not confirmed by other studies.
Glass, Bethesda: Interesting presentation. The ability to ask people and convince them to donate is probably as variable as the people who ask, whether it's for donations of livers or donations for raising funds. You didn't present any data on the numbers of people who are asking or the variability to see if some people are the Babe Ruth's of asking and other people are the minor leagues. Is there anything you can see from that variability because that might be quite important in understand this data.
Bodenheimer, New York: Yes. We are looking at that to see the impact of individual training and success. We will analyze our data assessing coordinator training. The hiring and tenure of the coordinators was quite variable among the four races that we measured in the organ procurement organization that we are working with. There is experience in other organ procurement organizations looking at the impact of educational training programs demonstrating an increase in the efficiency of organ donation. Personal ability certainly has an impact on the efficiency of obtaining consent for organ donation.
REFERENCES
- 1.World Health Organization. Geneva, Switzerland: Health Statistics and Informatics Department; 2011. [Accessed January, 2011]. Global Burden of Disease. Available at: http://www.who.int/evidence/bod. [Google Scholar]
- 2.Miniño A, Xu J, Kochanek K. Centers for Disease Control and Prevention. Deaths: preliminary data for 2008. National Vital Statistics Reports. 2010;59:1–5. [PubMed] [Google Scholar]
- 3.Bell BP, Manos MM, Zaman A, et al. The epidemiology of newly diagnosed chronic liver disease in gastroenterology practices in the United States: results from population-based surveillance. Am J Gastroenterol. 2008;103:2727–36. doi: 10.1111/j.1572-0241.2008.02071.x. [DOI] [PubMed] [Google Scholar]
- 4.Liver Transplants Performed Yearly. Organ Procurement and Transplantation Network Database. [Accessed: August, 2011]. Available at: http://optn.transplant.hrsa.gov/latestData/rptData.asp.
- 5.Bratton C, Chavin K, Baliga P. Racial disparities in organ donation and why. Curr Opin Organ Transplant. 2011;2:243–9. doi: 10.1097/MOT.0b013e3283447b1c. [DOI] [PubMed] [Google Scholar]
- 6.Anker AE, Feeley TH. Why families decline donation: the perspective of organ procurement coordinators. Prog Transpl. 2010;20:239–46. doi: 10.1177/152692481002000307. [DOI] [PubMed] [Google Scholar]
- 7.Lee E, Midodizi W, Gourishankar S. Attitudes and opinions on organ donation: an opportunity to educate in a Canadian city. Clin Transpl. 2010;24:E223–9. doi: 10.1111/j.1399-0012.2010.01260.x. [DOI] [PubMed] [Google Scholar]
- 8.Bryce CL, Angus DC, Arnold RM, et al. Sociodemographic differences in early access to liver transplantation services. Am J Transpl. 2009;9:2092–101. doi: 10.1111/j.1600-6143.2009.02737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Julapalli VR, Kramer JR, El-Serag HB. Evaluation for liver transplantation: adherence to AASLD referral guidelines in a large Veterans Affairs center. Liver Transpl. 2005;11:1370–8. doi: 10.1002/lt.20434. [DOI] [PubMed] [Google Scholar]
- 10.Kemmer N, Neff G, Secic M, Zacharias V, Kaiser T, Buell J. Ethnic differences in hepatocellular carcinoma: implications for liver transplantation. Dig Dis Sci. 2008;53:551–5. doi: 10.1007/s10620-007-9872-7. [DOI] [PubMed] [Google Scholar]
- 11.Yu JC, Neugut AI, Wang S, et al. Racial and insurance disparities in the receipt of transplant among patients with hepatocellular carcinoma. Cancer. 2010;116:1801–9. doi: 10.1002/cncr.24936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navaneethan SD, Singh S. A systematic review of barriers in access to renal transplantation among African Americans in the United States. Clin Transpl. 2006;20:769–75. doi: 10.1111/j.1399-0012.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- 13.Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transpl. 2006;6:190–8. doi: 10.1111/j.1600-6143.2005.01130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown CV, Foulkrod KH, Dworaczyk S, et al. Barriers to obtaining family consent for potential organ donors. J Trauma. 2010;68:447–51. doi: 10.1097/TA.0b013e3181caab8f. [DOI] [PubMed] [Google Scholar]
- 15.Liver disease by race. Organ Procurement and Transplantation Network Database. [Accessed: January, 2011]. Available at: http://optn.transplant.hrsa.gov/latestData/rptData.asp.
- 16.Reid AE, Resnick M, Chang Y, Buerstatte N, Weissman JS. Disparity in use of orthotopic liver transplantation among blacks and whites. Liver Transpl. 2004;10:834–41. doi: 10.1002/lt.20174. [DOI] [PubMed] [Google Scholar]
- 17.Ananthakrishnan AN, Saeian K. Racial differences in liver transplantation outcomes in the MELD era. Am J Gastroenterol. 2008;103:901–10. doi: 10.1111/j.1572-0241.2008.01809.x. [DOI] [PubMed] [Google Scholar]
- 18.Siminoff LA, Burant CJ, Ibrahim SA. Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med. 2006;21:995–1000. doi: 10.1111/j.1525-1497.2006.00516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–99. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 20.Kemmer N, Zacharias V, Kaiser TE, Neff GW. Access to liver transplantation in the MELD era: role of ethnicity and insurance. Dig Dis Sci. 2009;54:1794–7. doi: 10.1007/s10620-008-0567-5. [DOI] [PubMed] [Google Scholar]
- 21.Sander SL, Miller BK. Public knowledge and attitudes regarding organ and tissue donation: an analysis of the northwest Ohio community. Patient Education and Counseling. 2005;58:154–63. doi: 10.1016/j.pec.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Yuen CC, Burton W, Chiraseveenuprapund P, et al. Attitudes and beliefs about organ donation among different racial groups. J Nat Med Assoc. 1998;90:13–8. [PMC free article] [PubMed] [Google Scholar]
- 23.Morgan S. The power of talk: African Americans' communication with family members about organ donation and its impact on the willingness to donate organs. J Social Personal Relationships. 2004;21:112–24. [Google Scholar]
- 24.Morgan M, Hooper R, Mayblin M, Jones R. Attitudes to kidney donation and registering as a donor among ethnic groups in the UK. J Publ Health. 2006;28:226–34. doi: 10.1093/pubmed/fdl045. [DOI] [PubMed] [Google Scholar]
- 25.Boulware LE, Troll MU, Wang NY, Powe NR. Perceived transparency and fairness of the organ allocation system and willingness to donate organs: a national study. Am J Transpl. 2007;7:1778–87. doi: 10.1111/j.1600-6143.2007.01848.x. [DOI] [PubMed] [Google Scholar]
- 26.Morgen S, Cannon T. African Americans' knowledge about organ donation: closing the gap with more effective persuasive message strategies. J Nat Med Assoc. 2003;95:1066–71. [PMC free article] [PubMed] [Google Scholar]
- 27.Moylan CA, Brady CW, Johnson JL, Smith AD, Tuttle-Newhall JE, Muir AJ. Disparities in liver transplantation before and after introduction of the MELD score. JAMA. 2008;300:2371–8. doi: 10.1001/jama.2008.720. [DOI] [PMC free article] [PubMed] [Google Scholar]