Abstract
Background
Chronic kidney disease (CKD) is a common disorder with increasing prevalence worldwide. This systematic literature review aims to provide insights specific to Japan regarding the burden and treatment of CKD.
Methods
We reviewed English and Japanese language publications from the last 10 years, reporting economic, clinical, humanistic, and epidemiologic outcomes, as well as treatment patterns and guidelines on CKD in Japan.
Results
This review identified 85 relevant articles. The prevalence of CKD was found to have increased in Japan, attributable to multiple factors, including better survival on dialysis therapy and a growing elderly population. Risk factors for disease progression differed depending on CKD stage, with proteinuria, smoking, hypertension, and low levels of high-density lipoprotein commonly associated with progression in patients with stage 1 and 2 disease. Serum albumin levels and hemoglobin were the most sensitive variables to progression in patients with stage 3 and 5 disease, respectively. Economic data were limited. Increased costs were associated with disease progression, and with peritoneal dialysis as compared with either hemodialysis or combination therapy (hemodialysis + peritoneal dialysis) treatment options. Pharmacological treatments were found potentially to improve quality of life and result in cost savings. We found no reports of treatment patterns in patients with early-stage CKD; however, calcium channel blockers were the most commonly prescribed antihypertensive agents in hemodialysis patients. Treatment guidelines focused on anemia management related to dialysis and recommendations for peritoneal dialysis treatment and preventative measures. Few studies focused on humanistic burden in Japanese patients; Japanese patients reported greater disease burden but better physical functioning compared with US and European patients.
Conclusion
A dearth of evidence regarding the earlier stages of kidney disease presents an incomplete picture of CKD disease burden in Japan. Further research is needed to gain additional insight into CKD in Japan.
Keywords: renal disease, epidemiology, disease progression, treatment patterns
Introduction
Chronic kidney disease (CKD) is a relatively common disorder with an increasing prevalence worldwide generally and specifically in Japan, where the prevalence of CKD has increased significantly over time1 to more than 22% of the general adult population in 2002. CKD is defined by progressive decline in kidney function, documented by serum creatinine and the rate of creatinine clearance as measured by the rate of glomerular filtration.2 Risk factors for the development of CKD include diabetes and hypertension.3 Additional risk for development and progression of CKD may be conferred through lifestyle factors such as smoking or those associated with obesity.4
The five stages of CKD are defined by the increasingly reduced glomerular filtration rate (GFR) and range from stage 1 (least severe) to stage 5 (representing kidney failure). Damage to the kidney, present as early as stage 1, may ultimately progress to stage 5 kidney failure, necessitating dialysis and possibly a kidney transplant.3 CKD is associated with risks of death, hospitalization, and cardiovascular disease.5 It also presents an economic burden, with the medical cost of end-stage renal disease (ESRD) representing approximately 4% of the total health care budget in Japan.6
While there is a significant amount of literature available regarding CKD worldwide, the information is sparser with respect to specific countries. Despite the accumulating literature on CKD in the US, country-specific data on CKD are limited in Japan. The goal of this systematic literature review is to provide insights specific to Japan regarding the burden and treatment of CKD.
Materials and methods
We conducted a systematic literature review of English and Japanese language publications in Medline and Embase, using search algorithms to identify publications with relevant economic, clinical, humanistic, and epidemiologic outcomes, as well as treatment patterns and guidelines on CKD in Japan. The search identified publications on CKD with keywords to identify the indication as well as the geographic location. Included articles featured the keywords in the title and/or abstract of full-length publications pertaining to humans, published in the 10 years preceding the search (ie, June 2001–June 2011). Relevant narrative (nonsystematic) reviews were included if they were published in the last 4 years (ie, July 2007–July 2011). To supplement the search, “gray” literature (ie, material such as meeting abstracts that can be referenced, but is not published in peer-reviewed, indexed medical journals) was also examined.
Abstracts brought in from the search were included when all of the following were true: the study pertained to adults with CKD in Japan with relevant economic, clinical, humanistic, and epidemiologic endpoints evaluated; the study was published in the last 10 years; in a primary experimental study of human subjects, at least 50 patients were enrolled; and 100,000 patients were enrolled in primary observational studies of human subjects.
The review of “gray” literature included information published from 2009 to the present and focused on economic outcomes for CKD patients in Japan. We searched a number of websites associated with professional and scientific organizations, including the Asia-Pacific International Society of Pharmacoeconomics and Outcomes Research, International Society for Quality of Life Research, National Kidney Foundation, World Congress of Nephrology, and American Society of Nephrology.
Results
Search
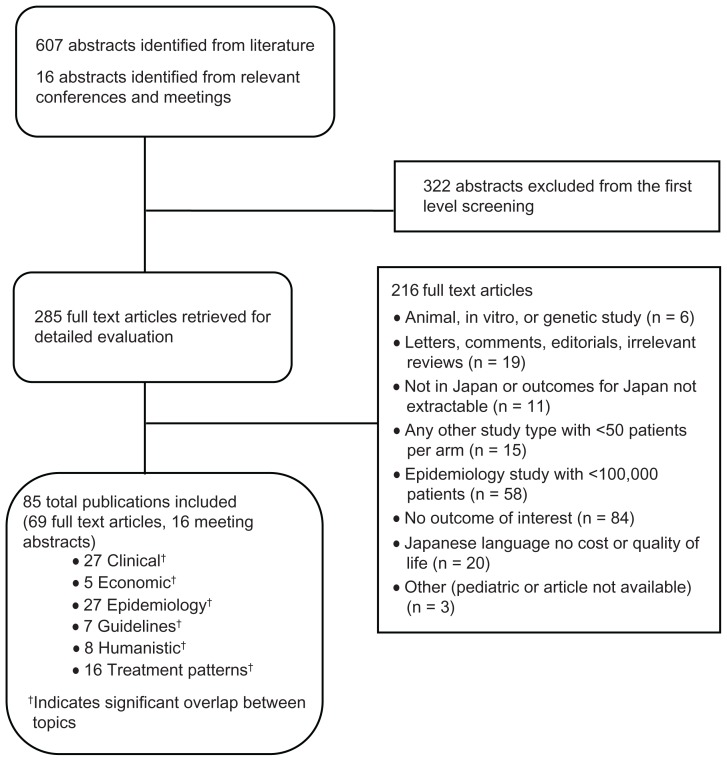
The Medline search identified 490 potentially relevant citations, and the Embase search identified 338 citations. Removing 221 duplicate publications yielded a total of 607 unique citations. Of the 607 abstracts reviewed, 285 articles were included for further review of full text, and 322 were excluded. Figure 1 presents the study attrition and exclusion rationale. Overall, we included 69 articles from Medline and Embase, and 16 articles from the gray literature in this review.
Figure 1.
Study attrition.
Epidemiology
CKD appears to be relatively common in Japan, as it is in other developed areas of the world. Its prevalence is anticipated to increase and may be explained by multiple factors, including better survival on dialysis therapy, greater insurance coverage, and a growing elderly population. Temporal changes in the epidemiological features of both CKD and ESRD in Japan can be seen in terms of demographics and risk factors.
Prevalence of CKD
Retrospective database analyses gave rise to all the prevalence estimates identified, with six identified publications describing five database analyses. These studies suggest that the prevalence of CKD may be similar to that in the US, and may be rising over time, but that stage-specific prevalence estimates may differ. In a retrospective analysis of two databases from 1993 and 2003, the overall prevalence of CKD was shown to be somewhat similar at 15.7% and 15.1%, respectively.7 However, another such series of analyses documented values of 13.8% in 1993 and 22.4% in 2003,8 suggesting a rising trend in prevalence of CKD.
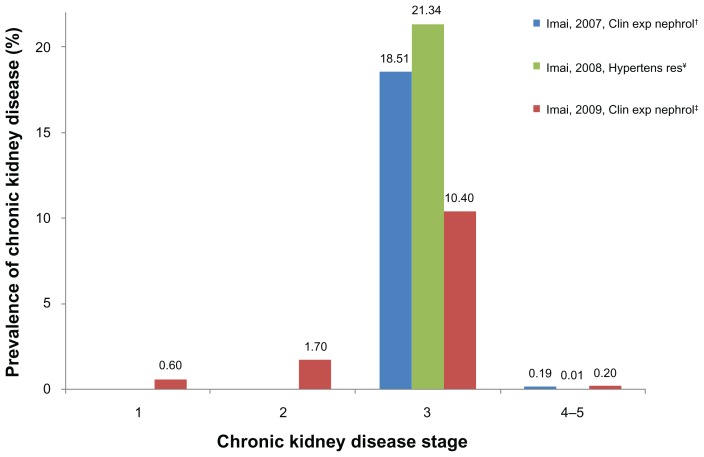
Prevalence estimates among the general population consistently found stage 3 CKD in the highest proportion. In a retrospective database analysis, Imai et al estimated that 19.1 million (18.5%) of those in the general population had stage 3 CKD, while 200,000 (0.2%) had stage 4 or 5 CKD in 2004.9 Data from the same population were used to estimate prevalence rates of CKD stages 1, 2, 3, and 4 + 5, respectively, as 0.6%, 1.7%, 10.4%, and 0.2% (Figure 2).10,11 Another retrospective database analysis produced a higher stage 3 CKD prevalence estimate of 21.3% in participants but a similarly low prevalence estimate of stage 4 + 5 CKD at 0.01% (Figure 2).12 Imai et al document age strata-specific differences in CKD prevalence between the US and Japan,9 suggestive of different epidemiologic patterns in the two countries.
Figure 2.
Prevalence of chronic kidney disease in the general population, by stage; data from retrospective database studies 2007–2009.
Notes:†Estimates based on 527,594 participants aged ≥20 years who participated in an annual health check programs from 2000–2004; ‡based on estimates from the 2005 updated annual health check program, which consisted of individuals aged ≥20 years; ¥based on data from 290,268 individuals aged ≥40 years who participated in an annual health examination program over 10 years (through 2003).
Incidence of CKD
CKD incidence was documented in one study, a retrospective database analysis, in which the incidence of developing CKD in 10 years was 15.5%.8 In contrast, data on the incidence of ESRD or dialysis commencement were found in eight publications.6,13–19 Annual ESRD incidence ranged from 161 to 222 million throughout the 12 regions (including Hokkaido, Tohoku, Kanto, Koshinetsu, Hokuriku, Tokai, Kinki, Chyugoku, Shikoku, Kyushu, and Okinawa) described in publications, but differed significantly across the regions (P < 0.001) in one retrospective analysis.6 These data were similar to those from another retrospective database analysis from 2002 to 2004, which found an ESRD incidence of 191 ± 8 to 348 ± 15 patients per million per year for the 47 prefectures in Japan.13 Similar values were found in a number of other retrospective database analyses16–19 as well as in a cohort study.15
Another retrospective analysis noted gender differences in ESRD incidence, with incidence in men increasing from 99.9 per million population in 1983 to 330.2 per million population in 2002, as compared with an increase among women over the same period from 66.6 per million to 184.9 per million. While this study showed that the incidence of ESRD increased among men compared with women, from 33.3 per million of the population in 1983 to 145.3 per million of the population in 2002,14 when gender ratios and the number of dialysis stations were assessed, no clear relationship emerged, and gender differences were not tested further statistically.
Risk factors for CKD
As noted above, there appear to be gender-related differences in the incidence of ESRD.14 Although a number of studies of Japanese patients have noted specific epidemiologic risk factors, the particular risk factor to which gender might be related has yet to be defined clearly. Japan may well also have geographically differing patterns of risk factors for CKD related to differing causal factors; in both Japan and the US, the main cause of ESRD is diabetes mellitus, but the second most common cause is glomerulonephritis in Japan and hypertension in the US.20 In an observational study of 219,166 dialysis patients from 1983 to 2001, the proportion of patients with chronic glomerulonephritis as the primary disease has tended to decrease year by year, accounting for 28.1% of patients newly introduced to dialysis treatment in 2004 and 60.5% in 1983.21 In a recent review, Uchida described the five major primary diseases in new dialysis patients as being diabetic nephropathy (43.2%), chronic glomerulonephritis (23.0%), nephrosclerosis (10.5%), polycystic kidney disease (2.5%), and rapidly progressive glomerulonephritis (1.2%) as of December 2008.22
Reviews of renal disease outcomes in CKD by Tseki in 2003 and 2010 suggest that important predictors of ESRD include proteinuria, hypertension, hyperglycemia, hyperuricemia, anemia, obesity, metabolic syndrome, and low GFR.16,23 Proteinuria was documented as a risk for ESRD in an observational cohort study of 106,177 patients (odds ratio [OR] 2.71, 95% confidence interval [CI] 2.51–2.92, P < 0.001).24
Metabolic disorders were significantly associated with CKD7,8 and ESRD prevalence.25 Additional study indicates that body mass index is a risk for ESRD in an observational cohort study of 100,753 dialysis patients, with an OR of 1.273 (1.121–1.446, P = 0.0002) for men and 0.950 (0.825–1.094, not significant) for women.25 In another prospective cohort study of 123,764 adults over 40 years of age, baseline-adjusted predictors for developing CKD included age, GFR, hematuria, hypertension, diabetes, serum lipids, obesity, smoking status, and consumption of alcohol.26
In sum, these studies support the concept that while hypertension and diabetes are primary disease risk factors for the development of CKD, metabolic abnormalities also play an important role.
Mortality associated with CKD
A number of observational studies have documented mortality associated with patients undergoing dialysis.18,21,27–30 One study documented overall cumulative survival rates among hemodialysis patients of 56.0%, 35.4%, 23.8%, and 16.5%, at 5-year, 10-year, 15-year, and 20-year periods, respectively.28 Annual mortality rates among dialysis patients were observed in several studies. In an observational study of 260,000 dialysis patients, the annual death rate was 6.1% for peritoneal dialysis patients and 9.7% for hemodialysis patients; the main causes of death were cardiac events, infection, and cerebral stroke.29 Another observational study reflected these estimates; in a cohort of 219,166 dialysis patients from 1983 to 2001, the annual crude mortality rate over the period from 1983 to 2004 ranged from 9.2% to 9.7%.18,30
Disease progression
The literature identified on the clinical burden of CKD patients in Japan mainly focused on late-stage CKD patients, whose disease had progressed to the point where dialysis was required. Twenty-seven studies reporting clinical outcomes were identified, of which eight reported on disease progression. Among these, few documented disease progression in early-stage CKD. While six studies reported progression factors in stage 4 patients who were attempting to delay dialysis, only one reported on patients with early CKD (including stages 1–2), and in one study, the stage was not clear.34 Among studies published in the last 10 years, none were identified that reported rate of disease progression for CKD patients in Japan.
Different risk factors contribute to disease progression depending on the stage of CKD. In a cohort study of 485 patients with stage 1 and stage 2 CKD, proteinuria, smoking, hypertension, and low high-density lipoprotein cholesterol were most closely associated with decreasing estimated GFR slope.31 In stage 3, serum albumin level was the variable most sensitive to CKD progression. In stage 5, hemoglobin was the most sensitive variable to CKD progression, as reported by a retrospective cohort study of 624 patients with CKD from January 2007 to December 2009.32 The association of current smoking with adverse outcomes was stronger in patients with lower rather than higher GFR in CKD.33 A recent 10-year cohort study aiming to validate a scoring system to predict renal outcome and estimate risk of ESRD identified several factors associated with increased risk of progression.34
Treatment strategies aimed at reducing albuminuria levels, such as antihypertensive agents, have provided information on predictors of progression in patients with comorbidities. A study of diabetic patients receiving renin-angiotensin system blocking agents found that patients were more likely to have delayed renal failure progression caused by diabetes.35 Based on this result, albuminuria may be an important disease predictor in late-stage CKD patients with diabetes.
Conversely, a cohort study in patients with type 2 diabetes and CKD showed silent cerebral infarction to be a predictor for the development and progression of nephropathy.36 Three hundred and sixty-six patients with type 2 diabetes and either normoalbuminuria or microalbuminuria were evaluated for silent cerebral infarction and for progression to microalbuminuria. Patients with silent cerebral infarction (n = 171) had a greater incidence of reaching the endpoint than those without silent cerebral infarction (n = 195, P = 0.020 by the log-rank test), and a hazard ratio of 2.02 (95% CI 1.09–3.72, P = 0.025) in the multivariate Cox regression model.36 This indicates that patients with cardiovascular disease have a greater risk of albuminuria.
A large-scale cohort study evaluated prognostic indicators and developed a scoring system for estimating risk of developing ESRD.34 The study found that male gender, age younger than 30 years, a family history of chronic renal failure and chronic glomerulonephritis, high systolic blood pressure, severe proteinuria, mild hematuria, hypoalbuminemia, lower GFR, and higher histologic grade were related to increased risk.34
Economics
In the past 10 years, five studies have assessed economic outcomes associated with CKD in Japan. Two of these studies evaluated costs related to dialysis therapy,37,38 whereas the economic benefit of pharmaceutical treatment options was the main focus of two studies,39,40 and one study assessed the impact of CKD on medical expenditure in Japan.41 The findings suggest that progression of CKD is associated with increasing costs.41 Treatment options were also evaluated, and peritoneal dialysis was more costly than either hemodialysis or combination therapy using hemodialysis plus peritoneal dialysis.38 However, dialysis therapy (either peritoneal dialysis or hemodialysis) was not cost-effective when compared with kidney transplantation.37 Finally, use of pharmacological therapy improved quality of life and led to cost savings for patients suffering from CKD.39,40
A summary of costs related to CKD is reported in Table 1. The data presented vary, limiting the ability to make comparisons between studies. Costs were reported in either US dollars ($) or in Japanese yen (¥), and authors rarely reported costing year or discounting. The model perspective was specified in only two studies, and both were from the standpoint of a third-party payer. Indirect costs (ie, caregiver burden, work loss) were not evaluated in this body of literature, and detailed cost components were scarcely reported in any of the publications.
Table 1.
Summary of chronic kidney disease-related costs in the general population
| Reference | Costs | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Home HD | Center/ satellite dialysis | Conventional HD | CAPD | APD | Combination therapy (5 days PD plus one weekly HD treatment) | |
| aKawanishi and Moriishi38 | NR | NR | $2833 per month | $3346 per month | $4649 per month | $2769 per month |
Notes:
Cost reported in United States dollars (USD); costing year and perspective not reported; All costs include laboratory test and management fees.
Abbreviations: APD, automated peritoneal dialysis; CAPD, continuous ambulatory peritoneal dialysis; HD, hemodialysis; NR, not reported; PD, peritoneal dialysis.
Cost of treatment and resource use
Three articles evaluated the cost of treatment and resource use in Japanese patients with CKD, indicating that peritoneal dialysis was associated with higher costs compared with both hemodialysis38 and combination therapy.38 Progression of CKD also led to greater medical expenditure, indicating that preventing progression may result in cost savings.41 Finally, a single study established that pharmacological treatment for hypertension was cost-saving for patients with ESRD.39 Only one study differentiated between mild and moderate kidney dysfunction. The remaining studies defined patient population according to the type of dialysis treatment they were receiving, as opposed to CKD stage. Costs were evaluated at both the patient38,39,41 and national level.41
One study on the cost of dialysis estimated that the cost of combination therapy with both peritoneal dialysis and hemodialysis was either equivalent or less than continuous automated peritoneal dialysis and conventional hemodialysis. 38 Combination therapy was also less expensive than automated peritoneal dialysis. Monthly dialysis costs in Japan (including laboratory test and management fees) were $3346 for continuous ambulatory peritoneal dialysis, $2833 for hemodialysis, $4649 for automated peritoneal dialysis, and $2769 combination therapy with 5 days of peritoneal dialysis and one hemodialysis treatment weekly.38
The progression of CKD is also associated with increasing costs. Higashiyama et al41 analyzed data from the Japanese National Health Insurance claims files (n = 4026 beneficiaries) to assess the effect of CKD on individual and national medical expenditures in Japan, also evaluating the amount of excess cumulative total medical expenditure due to CKD. Patients included were aged 40–74 years, were living in Tanba City in Hyogo Prefecture, Japan, and had undergone a medical examination in 2002. Participants were stratified into three groups based on their kidney function as assessed by GFR (normal kidney function, GFR 90; mild kidney dysfunction 60 ≤ GFR < 90; and moderate kidney dysfunction 30 ≤ GFR < 60). Medical expenditure data were collected from Japanese National Health Insurance after 3 years of follow-up. All costs were presented in Japanese yen. The results show that progression of CKD led to an increase in medical expenditure, with cumulative total medical expenditure per person highest for patients with moderate kidney dysfunction and lowest for patients with normal kidney function (¥536,027 normal, ¥649,865 mild, ¥777,623 moderate). Excess cumulative total medical expenditure was estimated as 11.5% (¥303,947,460) for mild kidney dysfunction (n = 645) and 6.5% (¥171,774,756) for moderate (n = 2670) kidney dysfunction. The authors did not report which cost components contributed to the surplus cost in patients with moderate CKD.41
Adding losartan to conventional therapy in CKD patients with diabetic nephropathy is cost-saving, according to Seng et al, who studied the costs of treatment with losartan plus conventional therapy compared with conventional antihypertensive therapy alone in patients with diabetic nephropathy (n = 96). The study was conducted from the perspective of Japanese National Health Insurance over a time horizon of 3.5 years. Total costs included cost of dialysis therapy (both peritoneal dialysis and hemodialysis) and the cost of losartan therapy. All costs were presented in 2004 USD. The losartan plus conventional therapy regimen led to a cost savings of $4346 over 3.5 years compared with conventional therapy alone ($9023 versus $13,369).39
Cost-effectiveness analyses
There was limited literature describing cost-effectiveness of treatments for CKD in Japan. The findings of these studies revealed that kidney transplant is a cost-effective treatment option compared with dialysis and that intervention with AST-120 (an oral adsorbent that attenuates the progression of CKD) leads to lower costs and greater quality-adjusted survival.37,40 Only one of these studies specified the population evaluated (advanced CKD).
Although the perspective was not reported, kidney transplant was found to be a cost-favorable treatment option compared with dialysis. In a cost-effectiveness analysis, kidney transplant (either living-related donor or deceased donor) was cost-effective compared with dialysis. All costs were presented in Japanese yen, though the costing year was not specified. Dialysis averted approximately 138,019 disability-adjusted life years (DALY) per year. Living donor-related transplant averted 5740 DALYs per year, and deceased donor transplant averted 1892 DALYs annually. The cost-effectiveness ratio was ¥9,546,000 per DALY for dialysis, ¥1,809,000 per DALY for living donor-related transplant recipients, and ¥2,322,000 per DALY for deceased donor transplant recipients.37
From the perspective of a Japanese reimbursement agency, a cost-effectiveness analysis of AST-120 versus placebo in nondiabetic patients (n = 223) with advanced CKD estimated that AST-120 led to lower costs and greater quality-adjusted survival compared with placebo. AST-120 acts locally within the gastrointestinal tract to remove toxins and, therefore, has the potential to delay disease progression and delay initiation of dialysis. The Markov model used a time horizon of 3 years, and all costs were presented in 2006 Japanese yen as well as USD (using a conversion rate of $1 = ¥117 as of October 2007). Mean total costs per patient at 3 years were estimated to be ¥6.67 million ($56,982) and ¥9.38 million ($80,196) for AST-120 and placebo, respectively. Cumulative mean quality-adjusted life year per patient at 3 years was estimated to be 0.295 (about 3.5 months) greater for patients on AST-120 than for patients on placebo (2.108 versus 1.813, respectively). Sensitivity analyses consistently estimated that AST-120 was associated with lower costs and greater quality-adjusted survival compared with placebo. AST-120 was dominant over placebo in 99.6% of the simulations. Further, 99.6% of the simulations fell below the threshold value of ¥5.85 million ($50,000) per quality-adjusted life year. When the time horizon was extended to 5 and 10 years, AST-120 remained dominant, with 98.9% and 98.7% of the simulations lying below the said threshold, respectively.40
Treatment patterns
In the last decade, 10 articles21,27,29,30,42–47 have examined real-world treatment patterns and resource use associated with CKD patients in Japan. Nearly all the studies evaluated data derived from DOPPS (the Dialysis Outcomes and Practice Patterns Study)42–44,46 or utilized results from a statistical survey conducted annually by the Japanese Society for Dialysis Therapy.21,27,29,30,45 Most publications reported on trends in dialysis treatment and side effects. No studies on treatment patterns in patients with early-stage CKD were identified. The majority of Japanese patients underwent hemodialysis, with only a small proportion receiving peritoneal dialysis for CKD. Changes in management of anemia following a revision of Japan’s health insurance bundling policy in 2006 led to reduced doses of recombinant human erythropoietin, while use of iron increased. In hemodialysis patients in Japan, calcium channel blockers were the most commonly prescribed antihypertensive agents, while data across countries suggest an association between angiotensin receptor blocker use and reduction in all-cause mortality.41
Dialysis
Our review of the recent literature in Japan shows limited information on early-stage CKD treatment patterns; most reported trends related to late-stage or ESRD patients. Dialysis is the predominant nonpharmaceutical therapy recommended for ESRD, with several types of dialysis offered; and hemodialysis is most commonly used in Japan. Hemodialysis removes wastes and water by circulating blood outside the body through an external semipermeable membrane filter, while peritoneal dialysis removes wastes and water from the blood inside the body using the peritoneal membrane as a natural semipermeable membrane.
Hemodialysis
The proportion of patients on dialysis has steadily increased in Japan. The Japanese Society for Dialysis Therapy conducts a yearly survey of individual dialysis facilities that includes a questionnaire on the details of the facility as well as a patient survey. This patient registration system is one of the largest in the world, and the response rate to the questionnaire has consistently been above 95% in recent years. We identified eight publications reporting the annual results of the survey from 2001 and 2008. According to the latest Japanese Society for Dialysis Therapy nationwide review conducted in 2008, the dialysis population rose to 283,421 patients in 2008, the majority of whom underwent daytime hemodialysis (81.7%). The number of patients treated by peritoneal dialysis decreased from 3.4% of patients in 2007 to 3.3% of patients in 2008. The mean duration of dialysis was 4 years or less for half of CKD patients, and less than 10% of patients had been treated with dialysis for 20 years or more. The dynamics of new patients undergoing dialysis in Japan have changed over time, because the average age of patients increased by 15 years between 1983 and 2008 from 51.9 to 67.2 years. Since 1983, the number of patients on dialysis has increased from 443.7 patients per million in 1983 to 2219.6 patients per million in 2008. The dialysis schedule was three times a week for the majority of patients (95.4%), and the average duration of treatment was 3.92 ± 0.53 hours. The average amount of dialyzed solution was 487 ± 33 mL per minute. Native vessel vascular access is most commonly used in dialysis patients. The percentage of patients who used a native vessel arteriovenous fistula for vascular access was 89.7%, while only 7.1% used an artificial vessel arteriovenous fistula, representing an increase over the past 10 years.48
Peritoneal dialysis
Treatment with peritoneal dialysis was less common in CKD patients in Japan, with one article documenting its use. Using results from the Japanese Society for Dialysis Therapy database, in 2006 only 9243 of the 260,000 patients included in the registration system were treated with peritoneal dialysis (3.6%).29 In patients receiving this form of dialysis, CAPD was used in the majority of patients (59.7%). Patients treated with peritoneal dialysis were about 5 years younger than the general CKD patient population. The authors suggest that the detraction for older patients may be related to the additional support needed to perform the daily care and bag exchange associated with peritoneal dialysis.
Treatment guidelines
In the past 10 years, seven guidelines were published on CKD management in Japan.49 The main focus was on anemia management related to dialysis as well as recommendations for peritoneal dialysis treatment and preventative measures.
Anemia
Three guidelines published in the last decade on anemia management in CKD patients undergoing dialysis have recommended use of recombinant human erythropoietin and iron. A 2008 guideline published by the Japanese Society for Dialysis Therapy defined49 the diagnosis threshold of anemia for Japanese patients as a hemoglobin level < 13.5 g/dL (hematocrit level < 40%) in adult males and <11.5 g/dL in adult females (hematocrit level < 35%). When a definite diagnosis of renal anemia is reached, treatment with erythropoiesis-stimulating agents, such as recombinant human erythropoietin, should be started. The recommended dose for intravenous injection of an erythropoiesis-stimulating agent is 1500 IU administered 3 times a week in hemodialysis patients and subcutaneous injection with 6000 IU once a week for peritoneal dialysis patients and nondialysis patients.49 Dose and frequency of administration should be determined by hemoglobin levels. Target hemoglobin levels should range from 10 g/dL to 11 g/dL in hemodialysis patients. Patients with an increased risk for cardiovascular disease or complications should have a dose reduction or interruption of erythropoiesis-stimulating treatment once hemoglobin levels reach 12 g/dL. Treatment with iron preparations required for erythropoiesis should be used concomitantly. Transferrin saturation and serum ferritin levels should be used for evaluation of iron status in CKD patients on erythropoiesis-stimulating therapy. Iron should be used to treat CKD patients with a transferrin saturation ≤ 20% and serum ferritin levels ≤100 ng/mL.
Peritoneal dialysis
A 2009 guideline created by the Japanese Society for Dialysis Therapy recommended combination therapy of peritoneal dialysis and hemodialysis as part of integrated renal replacement therapy for ESRD. Initiation of dialysis should be considered in stage 5 CKD patients with GFR < 15.0 mL/min/1.73 m2 body surface area if they have signs or symptoms of uremia resistant to medical treatment. Additionally, initiation of dialysis was recommended before the GFR reaches 6.0 mL/min/1.73 m2 body surface area. During treatment, the adequacy of peritoneal dialysis must be evaluated regularly and the efficacy of peritoneal dialysis should be evaluated according to the weekly Kt/Vurea (target 1.7). In order to avoid fluid overload, an appropriate volume of ultrafiltration must be set, monitored, and maintained. Peritoneal dialysis patients are at increased risk for development of malnutrition. Therefore, patient nutritional status should be assessed routinely, and patients should also be monitored for signs or symptoms of uremia or malnutrition, the appearance of which warrants reassessment of the prescribed treatment. The guideline also recommends regular evaluation of peritoneal membrane function using the peritoneal equilibrium test and either the standard or simplified method.
Preventative measures
A recent review of CKD in Japan recommended preventative measures to delay disease progression in patients, including weight loss and AHA treatment,6 while a second study50 emphasized the importance of urinalysis screening to aid in early diagnosis and prevent early disease progression. There is evidence of a protective effect of weight loss on CKD progression when it occurs prior to appearance of late-stage disease. However, a higher body mass index can have a beneficial effect on survival in ESRD patients. Based on this, weight loss may be an important tool to delay progression but not management of ESRD. Renin-angiotensin system inhibitors are suggested to prevent progression of CKD. Angiotensin receptor blockers, angiotensin-converting enzyme inhibitors, or their combination, and calcium channel blockers have been effective in reducing proteinuria and progression of CKD.6
Proteinuria is known to be an accurate predictor of reduced renal function. A recent review emphasized the early detection and management benefits resulting from a simple urine screen for proteinuria50 that could reduce disease progression in some patients. The positive rate of proteinuria is high in the general Japanese population, especially in patients without hypertension or diabetes. Because many patients are asymptomatic and the incidence of glomerulonephritis, especially IgA nephropathy, is high in the Japanese and Asian races, universal screening could lead to early detection whereby treatment to reduce progression can be optimized.
Patient-reported outcomes
Our review identified seven studies documenting patient-reported outcomes, two of which were related publications. Of the six independent studies, four documented health-related quality of life outcomes, one documented symptoms (depression), while another documented functional outcomes. Of those studies documenting health-related quality of life, two used the Short Form-36 (SF-36), one used the Kidney Disease Quality of Life Short Form (KDQOL-SF), and one used the EuroQol 5D (EQ-5D). The results of these studies are summarized in Table 2.
Table 2.
Studies documenting health-related quality of life information in Japanese patients with chronic kidney disease
| HRQoL instrument | Description of instrument | Results cited |
|---|---|---|
| Kidney Disease Quality of Life Short Form56 | 80 items, kidney disease-specific (SF-36 is the generic core) 19 scales | DOPPS study51
|
| Short Form-3657 | 36 items, generic, 8 health concepts | Fukuhara et al58
|
| EuroQoL 5D (EQ-5D)59 | 5 items + 1 visual scale generic | Tajima et al54
|
Abbreviations: DOPPS, Dialysis Outcomes and Practice Patterns Study; HRQoL, health-related quality of life; CKD, chronic kidney disease.
While the humanistic burden of CKD has been the subject of much study, there are relatively few studies specific to Japanese populations, or comparing those populations with those from other countries. The ongoing DOPPS provides a powerful means to answer such questions. In a study by Fukuhara et al using cross-sectional data from administration of the KDQOL-SF instrument to the DOPPS population, Japanese hemodialysis patients reported significantly greater burden of kidney disease than did patients in the US or Europe.51
However, in contrast with the subjective feeling of disease burden, DOPPS data indicate that Japanese hemodialysis patients reported better physical functioning as measured using the KDQOL scale, compared with hemodialysis patients from other continents.51 The authors suggest that socioeconomic factors and major comorbid conditions could not account for this discrepancy, and that other factors, including quality of dialysis and other CKD-related health care, may be playing a role, suggesting further study is warranted.51
The humanistic burden of CKD was supported by a 48-week comparative longitudinal study of 471 predialysis patients with CKD and 4500 members of the general population, with additional observation of associations with physiologic parameters, notably hematocrit and serum creatinine.52 The authors used the generic SF-36, documenting overall and domain-specific score changes. This study documented significantly greater one-year decreases among CKD patients compared with the general population in all domains of the SF-36, except role-emotional.52 The authors also found that anemia was associated with a decrease in the vitality domain of the SF-36, with a 10% decline in hematocrit being associated with a decline in the vitality score of 4.5 points (P = 0.003). Further, increases in serum creatinine from baseline were associated with decrements in health-related quality of life, specifically in the domains of physical function (−1.2, P = 0.004), role-physical (−1.9, P = 0.035), and mental health (−1.0, P = 0.008).
Also documenting the association of anemia and health-related quality of life was a single-arm trial of darbepoetin alfa in the treatment of anemia in 487 hemodialysis patients by Fukuhara et al; this study documented increases in all eight SF-36 subscales over 14 weeks of treatment.53 All increases were signficant except that on the social function subscale; the largest increases were in role functioning and vitality.53 The authors evaluated the role of anemia in change in health-related quality of life and found that only the subscale of vitality was associated with hemoglobin concentration. This is consistent with a previous study by Fukuhara et al in which a 10% decline in hematocrit was significantly associated with a decline in the vitality subscale of the SF-36.52
In a cross-sectional survey of 588 outpatients with CKD and on hemodialysis, Tajima et al used the EQ-5D instrument to document health-related quality of life.54 The presence of all five stages of CKD in the sample allowed for weights to be calculated for each stage relative to the standard weight of 1 (perfect health). Overall, CKD patients had a quality-adjusted weight of 0.885 (95% CI 0.871–0.898). The authors documented that the quality-adjusted weights associated with each CKD stage 1 through 5 decreased from 0.940 (95% CI 0.915–0.965), 0.918 (0.896–0.940), 0.883 (0.857–0.909), 0.839 (0.794–0.884), to 0.798 (0.757–0.839), respectively; the decreasing trend associated with progressive CKD stage was statistically signficant (analysis of variance P < 0.0001).54 Further, the authors documented the role of comorbidities in the decrease of these quality-adjusted weights. Hypertension significantly (P = 0.03) lowered the weight overall from 0.910 (0.885–0.936) to 0.874 (0.858–0.891), diabetes significantly (P = 0.0001) reduced the weight overall from 0.901 (0.886–0.917) to 0.840 (0.811–0.869), and cardiovascular disease significantly (P = 0.002) reduced the weight overall from 0.892 (0.878–0.906) to 0.783 (0.718–0.848). In this way, the authors were able to document the role of these comorbidities in the reduction of health-related quality of life concomitant with that seen among all CKD patients.54
Few studies documenting specific CKD symptoms were noted. One study examined the presence of both depression and bodily pain among patients with CKD. In this longitudinal study of 531 patients from the Japan DOPPS cohort, the authors used the Center for Epidemiological Studies Depression Screening Index (CES-D) to document the association between depression and development of severe bodily pain as assessed using a 6-point Likert scale.55 At baseline, the study documented an association between the proportion of patients reporting severe bodily pain and their baseline CES-D score, with an OR of 2.53 (95% CI 1.96–3.26, P < 0.0001).55 This observation suggests an association between the two symptoms, but not necessarily a temporal one. The baseline CES-D scores were subsequently shown to be associated with severe bodily pain symptoms at the second data collection point, occurring between 0.5 to 2.5 years after the first, among those ESRD patients with no severe symptoms at baseline, with an OR of 2.13 (95% CI 1.36–3.33, P = 0.001).55 Depressive symptoms among ESRD patients may predict the risk of development of severe bodily pain.
Discussion
While this review identified a substantial body of literature on CKD in Japan, there were limitations in all areas, suggesting a currently incomplete picture of CKD burden in Japan. Few data on disease progression in Japanese populations were available; no publication documented progression rates from one stage to the next, and few documented progression from early-stage to late-stage CKD. With respect to information on treatment patterns, only that regarding dialysis was available, as well as management of anemia and cardiovascular disease in the context of CKD. This situation was mirrored by the economic literature identified, which also focused on dialysis, with no information available on indirect costs incurred, eg, by caregiver burden. A substantial number of publications documented the epidemiology of CKD in Japan; however, a large proportion focused on later stages of CKD, ie, incidence, prevalence, risk factors, and mortality of dialysis or ESRD. Finally, with respect to patient-reported outcomes, several important publications were based on the DOPPS study, a prospective, observational, international study of hemodialysis patients, which provides the potential for powerful insight into the experience of CKD on three continents. However, among many papers describing results from the DOPPS study, our review found that relatively few of them described results in a manner allowing differentiation of CKD in Japan compared with the other continents incorporated into the DOPPS (US and Europe). Conclusions drawn from the longitudinal health-related quality of life studies identified in this review must also be tempered by the fact that common comorbidities associated with CKD may affect health outcomes, thereby confounding the results of such observational studies, and few studies accounted for such potential confounding.
It is clear that further study is warranted in all these areas, particularly in the early stages. There are suggestions that the experience of CKD patients in Japan may differ from that of patients in other areas of the world in important ways, potentially associated with different environmental and socioeconomic factors, access to and use of health care resources, and humanistic burden.
The dearth of information around the costs associated with the early stages of this chronic disease makes it difficult to place potential treatments in economic context in comparison with other pharmacologic or nonpharmacologic interventions. Further analysis of costs incurred by CKD patients would be an important step towards providing economic evidence. Economic studies piggy-backed onto head-to-head clinical trials or observational studies, retrospective database analysis, or chart reviews in Japan should be considered for this purpose. The choice of study design needs to ensure that all data possible can be collected for further economic analysis, such as cost-effectiveness models.
Data regarding real-world resource utilization by CKD patients in Japan are limited. Given the chronic nature of this disease, as well as comorbidities, estimation of such resource use is challenging. Retrospective studies of claims databases, if available, may serve to fill this gap, identifying patterns of resource use by patients diagnosed with early stages of CKD. The costs of the use of such resources can also be estimated and provide data relevant to the estimation of the potential economic impact of the treatment of early CKD.
With a similar scarcity of real-world treatment patterns, a series of interviews with key opinion leaders may help to define real-world treatment patterns. Additionally, reviews of claims databases may serve to document treatment patterns specific to early CKD.
Including disease-specific health-related quality of life instruments, such as the KDQOL, in future clinical trial protocols will allow for a time-effective and cost-effective method of quantifying the impact of CKD on health-related quality of life in patients and confirming the association of CKD with decrements in health-related quality of life as documented by observational studies. The choice of instrument should be made carefully to ensure that its psychometric properties are appropriate for potentially reading out from a clinical trial and that it has been validated for use in this patient population. Selection of an instrument that can be converted to health state utilities would also be valuable for future health economics and modeling efforts. Patient preference studies, of which none were identified in the current review, would also be of use in order to capture the effects of this disease and potential treatments on the lives of CKD patients even more fully.
Conclusion
The recent literature on the burden of illness and treatment of CKD in Japan primarily evaluated ESRD patients undergoing dialysis. As a result, the dearth of evidence for the earlier stages of kidney disease led to an incomplete picture of disease burden. Further research is needed to gain additional insight into CKD in Japan.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nagata M, Ninomiya T, Doi Y, et al. Trends in the prevalence of chronic kidney disease and its risk factors in a general Japanese population: the Hisayama Study. Nephrol Dial Transplant. 2010;25(8):2557–2564. doi: 10.1093/ndt/gfq062. [DOI] [PubMed] [Google Scholar]
- 2.Eknoyan G, Lameire N, Barsoum R, et al. The burden of kidney disease: improving global outcomes. Kidney Int. 2004;66(4):1310–1314. doi: 10.1111/j.1523-1755.2004.00894.x. [DOI] [PubMed] [Google Scholar]
- 3.Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2005;67(6):2089–2100. doi: 10.1111/j.1523-1755.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- 4.Tozawa M, Iseki K, Iseki C, Oshiro S, Ikemiya Y, Takishita S. Influence of smoking and obesity on the development of proteinuria. Kidney Int. 2002;62(3):956–962. doi: 10.1046/j.1523-1755.2002.00506.x. [DOI] [PubMed] [Google Scholar]
- 5.Tsukamoto Y, Wang H, Becker G, et al. Report of the Asian Forum of Chronic Kidney Disease Initiative (AFCKDI) 2007. “Current status and perspective of CKD in Asia”: diversity and specificity among Asian countries. Clin Exp Nephrol. 2009;13(3):249–256. doi: 10.1007/s10157-009-0156-8. [DOI] [PubMed] [Google Scholar]
- 6.Iseki K. Chronic kidney disease in Japan. Intern Med. 2008;47(8):681–689. doi: 10.2169/internalmedicine.47.0906. [DOI] [PubMed] [Google Scholar]
- 7.Iseki K, Kohagura K, Sakima A, et al. Changes in the demographics and prevalence of chronic kidney disease in Okinawa, Japan (1993 to 2003) Hypertens Res. 2007;30(1):55–62. doi: 10.1291/hypres.30.55. [DOI] [PubMed] [Google Scholar]
- 8.Tokashiki K, Tozawa M, Iseki C, et al. Decreased body mass index as an independent risk factor for developing chronic kidney disease. Clin Exp Nephrol. 2009;13(1):55–60. doi: 10.1007/s10157-008-0085-y. [DOI] [PubMed] [Google Scholar]
- 9.Imai E, Horio M, Iseki K, et al. Prevalence of chronic kidney disease (CKD) in the Japanese general population predicted by the MDRD equation modified by a Japanese coefficient. Clin Exp Nephrol. 2007;11(2):156–163. doi: 10.1007/s10157-007-0463-x. [DOI] [PubMed] [Google Scholar]
- 10.Imai E, Horio M, Watanabe T, et al. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol. 2009;13(6):621–630. doi: 10.1007/s10157-009-0199-x. [DOI] [PubMed] [Google Scholar]
- 11.Iseki K, Horio M, Imai E, Matsuo S, Yamagata K. Geographic difference in the prevalence of chronic kidney disease among Japanese screened subjects: Ibaraki versus Okinawa. Clin Exp Nephrol. 2009;13(1):44–49. doi: 10.1007/s10157-008-0080-3. [DOI] [PubMed] [Google Scholar]
- 12.Imai E, Horio M, Yamagata K, et al. Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res. 2008;31(3):433–441. doi: 10.1291/hypres.31.433. [DOI] [PubMed] [Google Scholar]
- 13.Furumatsu Y, Nagasawa Y, Hamano T, et al. Integrated therapies including erythropoietin decrease the incidence of dialysis: lessons from mapping the incidence of end-stage renal disease in Japan. Nephrol Dial Transplant. 2008;23(3):984–990. doi: 10.1093/ndt/gfm705. [DOI] [PubMed] [Google Scholar]
- 14.Iseki K, Nakai S, Shinzato T, Nagura Y, Akiba T. Increasing gender difference in the incidence of chronic dialysis therapy in Japan. Ther Apher Dial. 2005;9(5):407–411. doi: 10.1111/j.1744-9987.2005.00318.x. [DOI] [PubMed] [Google Scholar]
- 15.Iseki K, Tozawa M, Ikemiya Y, Kinjo K, Iseki C, Takishita S. Relationship between dyslipidemia and the risk of developing end-stage renal disease in a screened cohort. Clin Exp Nephrol. 2005;9(1):46–52. doi: 10.1007/s10157-004-0332-9. [DOI] [PubMed] [Google Scholar]
- 16.Iseki K. The Okinawa screening program. J Am Soc Nephrol. 2003;14(7 Suppl 2):S127–S130. doi: 10.1097/01.asn.0000070153.91733.09. [DOI] [PubMed] [Google Scholar]
- 17.Kato N, Usami T, Fukuda M, et al. Different regional dynamics of end-stage renal disease in Japan by different causes. Nephrology (Carlton) 2005;10(4):400–404. doi: 10.1111/j.1440-1797.2005.00404.x. [DOI] [PubMed] [Google Scholar]
- 18.The current state of chronic dialysis treatment in Japan (as of December 31, 2000) Ther Apher Dial. 2003;7(1):3–35. [PubMed] [Google Scholar]
- 19.Wakai K, Nakai S, Kikuchi K, et al. Trends in incidence of end-stage renal disease in Japan, 1983–2000: age-adjusted and age-specific rates by gender and cause. Nephrol Dial Transplant. 2004;19(8):2044–2052. doi: 10.1093/ndt/gfh317. [DOI] [PubMed] [Google Scholar]
- 20.Iseki K. Chronic kidney disease in Japan from early predictions to current facts. Nephron Clin Pract. 2008;110(4):c268–c272. doi: 10.1159/000170094. [DOI] [PubMed] [Google Scholar]
- 21.Nakai S, Wada A, Kitaoka T, et al. An overview of regular dialysis treatment in Japan (as of December 31, 2004) Ther Apher Dial. 2006;10(6):476–497. doi: 10.1111/j.1744-9987.2006.00440.x. [DOI] [PubMed] [Google Scholar]
- 22.Uchida S. Differential diagnosis of chronic kidney disease (CKD): by primary diseases. Japan Medical Association Journal. 2011;54(1):22–26. [Google Scholar]
- 23.Iseki K. Renal outcomes in chronic kidney disease. Nephrology (Carlton) 2010;15(Suppl 2):27–30. doi: 10.1111/j.1440-1797.2010.01308.x. [DOI] [PubMed] [Google Scholar]
- 24.Iseki K, Ikemiya Y, Iseki C, Takishita S. Proteinuria and the risk of developing end-stage renal disease. Kidney Int. 2003;63(4):1468–1474. doi: 10.1046/j.1523-1755.2003.00868.x. [DOI] [PubMed] [Google Scholar]
- 25.Iseki K, Ikemiya Y, Kinjo K, Inoue T, Iseki C, Takishita S. Body mass index and the risk of development of end-stage renal disease in a screened cohort. Kidney Int. 2004;65(5):1870–1876. doi: 10.1111/j.1523-1755.2004.00582.x. [DOI] [PubMed] [Google Scholar]
- 26.Yamagata K, Ishida K, Sairenchi T, et al. Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int. 2007;71(2):159–166. doi: 10.1038/sj.ki.5002017. [DOI] [PubMed] [Google Scholar]
- 27.Nakai S, Shinzato T, Nagura Y, et al. An overview of regular dialysis treatment in Japan (as of December 31, 2001) Ther Apher Dial. 2004;8(1):3–32. doi: 10.1111/j.1526-0968.2004.00109.x. [DOI] [PubMed] [Google Scholar]
- 28.Furumatsu Y, Nagasawa Y, Yamamoto R, et al. Specialist care and improved long-term survival of dialysis patients. Nephrol Dial Transplant. 2010;25(6):1930–1935. doi: 10.1093/ndt/gfp738. [DOI] [PubMed] [Google Scholar]
- 29.Masakane I, Tsubakihara Y, Akiba T, Watanabe Y, Iseki K. The most recent trends of peritoneal dialysis in Japan. Perit Dial Int. 2008;28(Suppl 3):S27–S31. [PubMed] [Google Scholar]
- 30.Patient Registration Committee, Japanese Society for Dialysis Therapy. An overview of regular dialysis treatment in Japan (as of December 31, 2002) Ther Apher Dial. 2004;8(5):358–382. doi: 10.1111/j.1526-0968.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 31.Yoshida T, Takei T, Shirota S, et al. Risk factors for progression in patients with early-stage chronic kidney disease in the Japanese population. Intern Med. 2008;47(21):1859–1864. doi: 10.2169/internalmedicine.47.1171. [DOI] [PubMed] [Google Scholar]
- 32.Iwamoto S, Iimori S, Yokotani A, et al. Analysis of risk factors associated with the progression of CKD in Japan. World Conference on Nephrology. 2011:Abstr SU282. [Google Scholar]
- 33.Yamamoto R, Nagasawa Y, Shoji T, et al. Cigarette smoking and progression of IgA nephropathy. Am J Kidney Dis. 2010;56(2):313–324. doi: 10.1053/j.ajkd.2010.02.351. [DOI] [PubMed] [Google Scholar]
- 34.Goto M, Wakai K, Kawamura T, Ando M, Endoh M, Tomino Y. A scoring system to predict renal outcome in IgA nephropathy: a nationwide 10-year prospective cohort study. Nephrol Dial Transplant. 2009;24(10):3068–3074. doi: 10.1093/ndt/gfp273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fujiwara A, Hirawa N, Yasuda G, Umemura S. Use of renin-angiotensin system blocking agents and retarded progression of end-stage renal failure: a retrospective study. Renal Week. 2010:Abstr F-PO1951. [Google Scholar]
- 36.Bouchi R, Babazono T, Yoshida N, et al. Silent cerebral infarction is associated with the development and progression of nephropathy in patients with type 2 diabetes. Hypertens Res. 2010;33(10):1000–1003. doi: 10.1038/hr.2010.122. [DOI] [PubMed] [Google Scholar]
- 37.Kaminota M. Cost-effectiveness analysis of dialysis and kidney transplants in Japan. Keio J Med. 2001;50(2):100–108. doi: 10.2302/kjm.50.100. [DOI] [PubMed] [Google Scholar]
- 38.Kawanishi H, Moriishi M. Clinical effects of combined therapy with peritoneal dialysis and hemodialysis. Perit Dial Int. 2007;27(Suppl 2):S126–S129. [PubMed] [Google Scholar]
- 39.Seng WK, Hwang SJ, Han DC, et al. Losartan reduces the costs of diabetic end-stage renal disease: an Asian perspective. Nephrology (Carlton) 2005;10(5):520–524. doi: 10.1111/j.1440-1797.2005.00472.x. [DOI] [PubMed] [Google Scholar]
- 40.Takahashi T, Reed SD, Schulman KA. Cost-effectiveness of the oral adsorbent AST-120 versus placebo for chronic kidney disease. Nephrology (Carlton) 2008;13(5):419–427. doi: 10.1111/j.1440-1797.2008.00960.x. [DOI] [PubMed] [Google Scholar]
- 41.Higashiyama A, Okamura T, Watanabe M, et al. Effect of chronic kidney disease on individual and population medical expenditures in the Japanese population. Hypertens Res. 2009;32(6):450–454. doi: 10.1038/hr.2009.51. [DOI] [PubMed] [Google Scholar]
- 42.Hasegawa T, Bragg-Gresham JL, Pisoni RL, et al. Changes in anemia management and hemoglobin levels following revision of a bundling policy to incorporate recombinant human erythropoietin. Kidney Int. 2011;79(3):340–346. doi: 10.1038/ki.2010.382. [DOI] [PubMed] [Google Scholar]
- 43.Lopes AA, Bragg-Gresham JL, Ramirez SP, et al. Prescription of antihypertensive agents to haemodialysis patients: time trends and associations with patient characteristics, country and survival in the DOPPS. Nephrol Dial Transplant. 2009;24(9):2809–2816. doi: 10.1093/ndt/gfp212. [DOI] [PubMed] [Google Scholar]
- 44.Mason NA, Bailie GR, Satayathum S, et al. HMG-coenzyme a reductase inhibitor use is associated with mortality reduction in hemodialysis patients. Am J Kidney Dis. 2005;45(1):119–126. doi: 10.1053/j.ajkd.2004.09.025. [DOI] [PubMed] [Google Scholar]
- 45.Nakahara N, Morita N, Uchida M, Kishimoto T, Miura K. Nursing care for dialysis patients in Japan. EDTNA ERCA J. 2004;30(4):217–221. doi: 10.1111/j.1755-6686.2004.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 46.Sood MM, Thumma JR, Tentori F, et al. Oral anticoagulants (OAC): prescription patterns and outcomes in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Renal Week. 2010:Abstr TH-PO510. [Google Scholar]
- 47.Tozawa M, Iseki K, Iseki C, et al. Analysis of drug prescription in chronic haemodialysis patients. Nephrol Dial Transplant. 2002;17(10):1819–1824. doi: 10.1093/ndt/17.10.1819. [DOI] [PubMed] [Google Scholar]
- 48.Nakai S, Suzuki K, Masakane I, et al. Overview of regular dialysis treatment in Japan (as of December 31, 2008) Ther Apher Dial. 2010;14(6):505–540. doi: 10.1111/j.1744-9987.2010.00893.x. [DOI] [PubMed] [Google Scholar]
- 49.Tsubakihara Y, Nishi S, Akiba T, et al. 2008 Japanese Society for Dialysis Therapy: guidelines for renal anemia in chronic kidney disease. Ther Apher Dial. 2010;14(3):240–275. doi: 10.1111/j.1744-9987.2010.00836.x. [DOI] [PubMed] [Google Scholar]
- 50.Yamagata K, Iseki K, Nitta K, et al. Chronic kidney disease perspectives in Japan and the importance of urinalysis screening. Clin Exp Nephrol. 2008;12(1):1–8. doi: 10.1007/s10157-007-0010-9. [DOI] [PubMed] [Google Scholar]
- 51.Fukuhara S, Lopes AA, Bragg-Gresham JL, et al. Health-related quality of life among dialysis patients on three continents: the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2003;64(5):1903–1910. doi: 10.1046/j.1523-1755.2003.00289.x. [DOI] [PubMed] [Google Scholar]
- 52.Fukuhara S, Yamazaki S, Marumo F, et al. Health-related quality of life of predialysis patients with chronic renal failure. Nephron Clin Pract. 2007;105(1):c1–c8. doi: 10.1159/000096802. [DOI] [PubMed] [Google Scholar]
- 53.Fukuhara S, Akizawa T, Morita S, Koshikawa S. Quality of life improvements in dialysis patients receiving darbepoetin alfa. Ther Apher Dial. 2007;12(1):72–77. doi: 10.1111/j.1744-9987.2007.00544.x. [DOI] [PubMed] [Google Scholar]
- 54.Tajima R, Kondo M, Kai H, et al. Measurement of health-related quality of life in patients with chronic kidney disease in Japan with EuroQol (EQ-5D) Clin Exp Nephrol. 2010;14(4):340–348. doi: 10.1007/s10157-010-0304-1. [DOI] [PubMed] [Google Scholar]
- 55.Yamamoto Y, Hayashino Y, Akiba T, et al. Depressive symptoms predict the subsequent risk of bodily pain in dialysis patients: Japan Dialysis Outcomes and Practice Patterns Study. Pain Med. 2009;10(5):883–889. doi: 10.1111/j.1526-4637.2009.00661.x. [DOI] [PubMed] [Google Scholar]
- 56.Hays RD, Kallich JD, Mapes DL, Coons SJ, Carter WB. Development of the kidney disease quality of life (KDQOL) instrument. Qual Life Res. 1994;3(5):329–338. doi: 10.1007/BF00451725. [DOI] [PubMed] [Google Scholar]
- 57.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 58.Fukuhara S, Yamazaki C, Hayashino Y, et al. The organization and financing of end-stage renal disease treatment in Japan. Int J Health Care Finance Econ. 2007;7(2–3):217–231. doi: 10.1007/s10754-007-9017-8. [DOI] [PubMed] [Google Scholar]
- 59.Gusi N, Badia X, Herdman M, Olivares PR. Translation and cultural adaptation of the Spanish version of EQ-5D-Y questionnaire for children and adolescents. Aten Primaria. 2009;41(1):19–23. doi: 10.1016/j.aprim.2008.04.005. Spanish. [DOI] [PMC free article] [PubMed] [Google Scholar]