Abstract
Background
Behavioral changes in patients with amyotrophic lateral sclerosis (ALS) mirror those found in frontotemporal dementia (FTD). Considering the high rate of neuropsychiatric symptoms found in ALS patients, this paper examines whether caregiver burden is associated with behavioral changes over and above the physical disability of patients with ALS, and if the presence of caregivers’ depression, anxiety and stress also impacts on caregiver burden.
Methods
140 caregivers of patients with ALS participated in a postal survey investigating patients’ neuropsychiatric symptoms (Cambridge Behaviour Inventory Revised CBI-R), motor function (Amyotrophic Lateral Sclerosis Functional Rating Scale Revised - ALSFRS-R), caregiver burden (Zarit Burden Interview), and caregiver mood (Depression, Anxiety and Stress Scale- DASS21). Seventy four percent of them were caregivers of patients with limb onset and 25.7% were caregivers of patients with bulbar onset.
Results
Moderate to severe behavioral changes were reported in 10-40% of patients with ALS. The levels of depression, anxiety and stress in the caregivers reached 20%. Burden was high in 48% of the caregivers. The strongest predictor of high caregiver burden was ALS patients’ abnormal behavior rather than physical disability, with an odds ratio of 1.4, followed by caregivers’ stress.
Conclusions
Our study has identified that behavioral changes (e.g. disinhibition, impulsivity) and caregiver stress have greater impact on caregiver burden than level and pattern of physical disability.
Keywords: ALS, Behavioral changes, FTD, Caregiver burden
Background
Over the past decade there has been increasing awareness of behavioral changes in patients with amyotrophic lateral sclerosis (ALS), which mirror those found in frontotemporal dementia (FTD) [1,2]. Caregivers of patients with FTD present with higher levels of burden than those caring for Alzheimer’s disease (AD) patients [3,4]. Caregiver burden seems to be closely coupled with the high rate of behavioral changes in FTD, [5-7] although this finding is not universal [8,9].
Caregiver burden is a complex construct involving the caregiver’s feelings about the emotional/physical health, social life and financial status that they suffer as a result of caring for their relatives [10]. Caregiving was shown to have an adverse effect on the physical and psychological health of caregivers [11]. Although advancing ALS undoubtedly causes high levels of caregiver distress, few studies have focused on the contributory factors [12-14]. Caregiver burden, depression and anxiety appear inter-related, and associated with the ALS patients’ physical disability [15]. Also, neurobehavioral symptoms have a negative impact on caregivers’ psychological status [16]. Given the high rate of cognitive deficits and neuropsychiatric symptoms found in ALS patients [2,17,18], it is clearly germane to examine whether caregiver burden is associated with behavioral changes over and above the physical disability of patients with ALS.
The aims of this study were: 1) to assess the impact of ALS patients’ behavior and motor disability on caregiver burden, 2) to assess the frequency of depression, anxiety and stress of the caregivers and possible impact on caregiver burden.
Methods
Caregivers of patients with ALS were contacted through the Motor Neurone Disease Association Australia, who kept their identities anonymous. Of 354 ALS patients registered as members of the association in NSW, 114 of their caregivers (32%) accepted an invitation to participate in a postal survey evaluating neuropsychiatric symptoms and motor function in ALS patients and burden of the caregiver. Additionally, 56 caregivers from other Australian states accepted the invitation through the local MND associations. Of the final one hundred and seventy caregivers who agreed to participate, 30 (17.6%) of them did not continue the study due to patients’ health issues or personal problems. Finally, data from the caregivers of 140 ALS patients was collected (60% from NSW and 40% from other Australian states); 104 (74.3%) of them were caregivers of patients with limb onset, whereas 36 (25.7%) were caregivers of patients with bulbar onset. Ethics approval was obtained from the Human Research Ethics Committee of South Eastern Sydney/Illawarra Area Health Service. Signed consent was obtained from each participant.
Patient - motor function
A self- administered version of the Amyotrophic Lateral Sclerosis Functional Rating Scale Revised (ALSFRS-R) was completed by ALS patients and/or their caregivers. It contains 4 sub scores: bulbar, fine, gross and respiratory function [19,20]. A total score of 48 denotes normal function.
Patient - behavioral changes
Changes in ALS patients’ behaviour were measured with the Cambridge Behavioural Inventory Revised (CBI-R), a caregiver-based measure of neuropsychiatric symptoms and daily activities, which correlates highly with the Neuropsychiatric Inventory (NPI).
It contains 10 domains: memory, everyday skills, self care, mood, beliefs, sleep, eating habits (e.g. preference for sweet food, increased appetite), abnormal behavior (e.g. disinhibition and impulsivity), stereotypic and/or motor behaviours and lack of motivation (apathy) [21]. The behavioral changes assessed by the CBI-R are independent of motor function and depression [2]. Scores were converted into percentage of impairment: 0-25% was classified as mild, 26-50% as moderate, 51-75% as severe, and > 75% as very severe [2,22].
Caregiver - depression, anxiety and stress scale
Caregivers completed the Depression, Anxiety, Stress scale (DASS 21) [23]. The following cut offs were applied: depression > 9, anxiety > 7 and stress > 14. The degree of severity for all sub-scales was classified as follows: normal, mild, moderate, severe and extremely severe.
Caregiver burden
The Zarit Burden Interview (ZBI) was used to measure caregiver burden by evaluating disease impact on caregivers’ quality of life, psychological suffering and impact on social and family relationships. Caregivers completed a self-administered short version of 12 items, which has shown to have comparable psychometric properties to the full version. The ZBI has a 0–4 point score with a maximum score of 48. A score ≥17 indicates a high burden [10,24,25].
Data analyses
SPSS Statistics 17.0 was used for analysis of results. To examine clinical features reported by caregivers, independent t-tests or Mann Whitney U tests were used where appropriate.
Comparison of behavioral changes across motor onset groups was analysed using Pearson’s X2 tests with Yates’ correction for continuity and Fisher’s exact test. A logistic regression was used to analyse the impact of caregiver’s mood, patients’ motor function, and behavioral changes on caregiver burden.
Results
The caregiver group (n = 140) was predominantly composed by females (69.3%). The mean age was 60.8 ± 12 years. The majority of caregivers were the patient’s spouses (90%), followed by patient’s children (7%); other relatives or friends were occasionally caregivers (3%).
ALS patients’ mean age was 63.5 ± 9 years, with a median of disease duration of 3 years (interquartile range 2–5). The mean ALSFRS-R total score was 30.4 (S.D. 9.7). Distribution of patients by motor onset showed a predominance of limb (73.6%) over bulbar (26.4%) onset. The age range and pattern of disease onset (limb vs. bulbar) mirrors closely that found in large cohorts [26-28].
Motor function
Comparison of ALSFRS-R total scores between patients with limb and bulbar onset showed no significant difference (p > 0.1). As expected, patients with bulbar onset had lower scores on bulbar function than patients with limb onset (limb Md = 9, bulbar Md = 4, U = 411, Z = −6.7, p < 0.001, r = 0.6). Likewise, patients with limb onset had lower scores in fine motor (limb Md = 6, bulbar Md = 9, U = 995.5, Z = −3.8, p < 0.001, r = 0.3) and gross motor function (limb Md = 6, bulbar Md = 8, U = 1171, Z = −2.9, p = 0.004, r = 0.2). No significant difference was found for respiratory function across groups (limb Md = 10, bulbar Md = 9, p > 0.1).
Behavioral changes
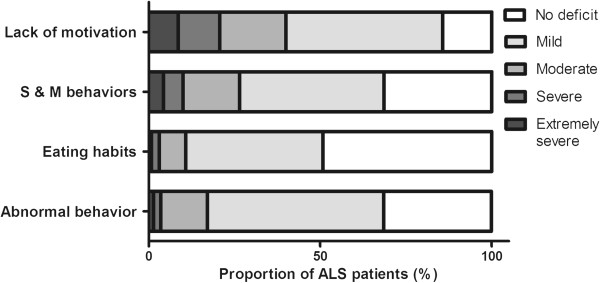
Figure 1 shows that abnormal behavior, stereotypical and motor behaviors and changes in eating habits were reported in more than 50% of the ALS patients, with around 10–30% patients in the moderate-severe category. The most prominent feature was lack of motivation (apathy), reported in more than 80% of the cases, with 40% having moderate-severe apathy.
Figure 1.
Behavioral changes in ALS patients based on CBI-R caregiver reports. (S & M behaviors: stereotypic and motor behaviors).
Comparison of CBI-R scores across patients with limb and bulbar onset showed no significant association between motor onset and behavioral changes (p > 0.1).
Depression, anxiety and stress
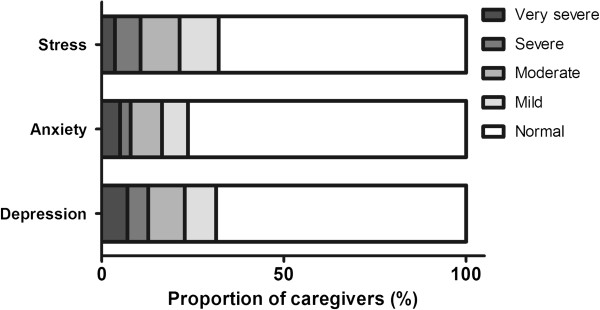
As shown in Figure 2, 69% of the caregivers did not reach the threshold for depression on the DASS. Moderate to very severe depression was present in 23% of the caregivers, and lesser degrees of depression were reported by 9% of caregivers.
Figure 2.
Depression, anxiety and stress based on caregiver self report (DASS21).
The percentage of caregivers with anxiety and stress was lower. Overall, 16% had moderate to extremely severe anxiety and 21% equivalent levels of stress. Comparison of the results between caregivers of patients with limb and bulbar onset showed no significant association between motor onset and presence of depression, anxiety and stress (p > 0.1).
Caregiver burden
The Zarit Burden Interview showed that high levels of burden (score ≥ 17) were reported by 48% of the caregivers. There was no significant difference when comparing caregivers’ burden of patients with limb and bulbar onset (p > 0.1).
Logistic regression was performed to assess the impact of different factors on the likelihood of caregivers in presenting with high burden. The patient related variables considered were motor function (ALSFRS-R sub scores: bulbar, fine motor, gross motor and respiratory function) and behavioral changes (CBI-R domains: abnormal behavior, eating habits, stereotypical and abnormal behavior and apathy). Caregivers’ variables considered were depression, anxiety and stress (DASS 21 sub scales).
The full model containing all predictors was statistically significant, (X2 [11, N = 140] = 74.1 p < 0.001), and explained between 45% (Cox and Snell R Square) and 60% (Nagelkerke R squared) of the variance in caregiver burden scores. Of the caregivers predicted to have high levels of burden, the model correctly classified 83.1%. As shown in Table 1, only two independent variables made statistically significant contributions to the model; abnormal behavior (from the patient) and stress (from the caregiver). The strongest predictor of high burden was abnormal behavior with an odds ratio of 1.4. This indicated that caregivers of ALS patients with abnormal behavior were 1.4 times more likely to report high burden.
Table 1.
Logistic regression: variables predicting likelihood of high burden on caregivers of patients with ALS
| Variable | B | S.E. | Wald | df | p | O.R. |
95% CI for O.R. |
|
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Abnormal behavior (CBI-R) |
0.37 |
0.13 |
8.36 |
1 |
0.004* |
1.44 |
1.13 |
1.85 |
| Eating habits (CBI-R) |
0.02 |
0.17 |
0.02 |
1 |
0.894 |
1.02 |
0.74 |
1.41 |
| Stereotypic & motor behaviors (CBI-R) |
0.10 |
0.11 |
0.79 |
1 |
0.376 |
1.10 |
0.89 |
1.36 |
| Motivation (CBI-R) |
0.04 |
0.06 |
0.34 |
1 |
0.555 |
1.04 |
0.92 |
1.18 |
| Depression (DASS) |
0.06 |
0.06 |
1.36 |
1 |
0.243 |
1.07 |
0.96 |
1.19 |
| Anxiety (DASS) |
−0.08 |
0.04 |
3.88 |
1 |
0.051 |
0.93 |
0.86 |
1.00 |
| Stress (DASS) |
0.12 |
0.052 |
5.10 |
1 |
0.024* |
1.12 |
1.02 |
1.25 |
| Bulbar (ALSFRS-R) |
−0.07 |
0.08 |
0.76 |
1 |
0.384 |
0.93 |
0.79 |
1.1 |
| Fine motor (ALSFRS-R) |
−0.14 |
0.10 |
1.97 |
1 |
0.167 |
0.87 |
0.71 |
1.06 |
| Gross motor (ALSFRS-R) |
0.79 |
0.11 |
0.50 |
1 |
0.478 |
1.08 |
0.87 |
1.35 |
| Respiratory (ALSFRS-R) |
−0.00 |
0.11 |
0.00 |
1 |
0.975 |
0.10 |
0.80 |
1.24 |
| Constant | −2.11 | 1.22 | 2.99 | 1 | 0.84 | 0.121 | ||
The caregiver burden was explained predominantly by the presence of abnormal behavior (in patients) and stress (in caregivers). * = statistically significant.
Discussion
Our study has identified that behavioral changes (e.g. disinhibition, impulsivity) and caregivers’ level of stress have greater impact on caregiver burden than any other patient variables, including level and pattern of physical disability.
Behavioral symptoms, as measured by the Frontal Systems Behavioral Scale (FrSBe), have previously been reported to be associated to higher caregiver burden, [16,18] although only one study has considered variables related to caregivers [16]. We have confirmed this association using the Cambridge Behavioural Inventory - Revised and, importantly, found that the strongest predictor of caregiver burden was the patient’s abnormal behavior. It should be noted that, as in other studies, apathy was the most common behavioral change [2,18,29], but this factor did not enter the model of caregiver burden. Stereotypical behaviors were also reported at similar levels to abnormal behavior, but again, this factor did not explain caregiver burden. Specific changes in behavior, notably disinhibition and impulsivity, are particularly distressing for caregivers. We suspect that many clinicians involved in the management of ALS patients are unaware of the high rate of these changes and their impact on family relationships. Specific interventions targeting carers and developing their coping skills have been shown to be successful in FTD [30] and may have a successful place in the management of ALS dyads.
A number of studies have shown that caregivers of patients with ALS report high levels of burden, anxiety and depression in association with the patient’s loss of physical functions [14,15]. In our study, somewhat surprisingly, burden was not associated with changes in physical function, as measured by the ALSFRS-R. One possible explanation for this lack of association may be that behavioral changes which overshadow the lesser influence of physical disability in a log regression model. Moderate or worse depressive symptoms were present in 23% of caregivers, with similar rates of stress. These symptoms did not, however, enter the model explaining caregiver burden. The reported rate of caregiver depression in caregivers of people with ALS has varied from 11 to 61% [31,32] which almost certainly reflects the use of different instruments, the threshold used to determine depression and the level of disability of patients in the cohorts. It is interesting that caregiver depression had lesser role in the genesis of caregiver burden than seen in pure FTD, despite the overlap in behavioral symptoms between bvFTD and ALS [12,13].
The levels of anxiety and stress (around 20%) in our caregivers were lower than reported previously [33,34]. Again, the variability probably reflects the use of different instruments. Caregivers’ state anxiety has been previously related to their trait anxiety more than external factors [34]. Stress rather than depression and anxiety was the main psychological caregiver variable contributing to caregiver burden. This is clearly relevant to management since can be addressed in MND clinics and are potentially amenable to intervention.
A longitudinal study identified that, initially, caregiver distress was best predicted by the psychosocial impact of ALS symptoms and emotional lability. Later, caregiver distress related to satisfaction with social relationships and social support [13] rather than behavioral changes, although these were limited to dysexecutive symptoms rather than the FTD-like features explored by the CBI. Future longitudinal studies should investigate the role of specific behavioral changes, caregiver variables, and disease progression especially given the fact that caregiver burden seems to increase over time. A limitation of this study was the nature of the survey via the MND Association, where carers who responded to the invitation to the research study were likely to be those willing to respond the questionnaires. Still, our results corroborated those published previously, and the patients’ characteristics mirrored those in large cohorts.
The fact that ALS patients presented similar behavioural symptoms to patients with FTD has been reinforced by a recent genetic discovery. The presence of a hexanucleotide repeats in the intron of C90RF72 in almost a quarter of cases with familial ALS and 12% of the cases with familial FTD [35,36] support strongly the idea of the continuum between ALS and FTD.
Conclusions
In summary, behavioral changes appear to lead to considerable caregiver burden, highlighting the importance to screen for neuropsychiatric symptoms in MND Clinics. Importantly, these symptoms could be modified by psychological or pharmaceutical therapies in an attempt to reduce caregiver burden. Caregivers’ emotional state also affects burden, with stress (but not depression or anxiety) playing major roles. Professionals involved with the care of ALS patients should be aware of these specific caregivers’ needs, which once addressed, are also likely to benefit the wellbeing of the patients.
Competing interests
Dr Lillo is supported by a CONICYT scholarship (Government of Chile) and Faculty of Medicine, University of Chile.
Dr. Mioshi serves on the editorial board of Dementia and Geriatric Cognitive Disorders and is a recipient of a National Health and Medical Research Council of Australia Early Career Fellowship and an Motor Neurone Disease Research Institute of Australia Grant.
Prof Hodges is funded by the Australian Research Council Federation Fellowship, FF0776229.
Prof. Hodges serves on editorial boards of Aphasiology, Cognitive Neuropsychiatry, and Cognitive Neuropsychology; receives royalties from publication of Cognitive Assessment for Clinicians (Oxford University Press, 2007) and Frontotemporal Dementia Syndromes (Cambridge University Press, 2007); and receives fellowship support from the Australian Research Council Federation.
Authors’ contributions
In order to give appropriate credit to each author of a paper, the individual contributions of authors to the manuscript should be specified in this section. PL: 1) have made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; 2) have been involved in drafting the manuscript and revising it critically for important intellectual content; and 3) have given final approval of the version to be published. EM: 1) have made substantial contributions to conception and design, analysis and interpretation of data; 2) have been involved in revising it critically for important intellectual content; and 3) have given final approval of the version to be published. JRH: 1) have made substantial contributions to conception and design, analysis and interpretation of data; 2) have been involved in revising it critically for important intellectual content; and 3) have given final approval of the version to be published.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Patricia Lillo, Email: pclz@uchile.cl.
Eneida Mioshi, Email: e.mioshi@neura.edu.au.
John R Hodges, Email: j.hodges@neura.edu.au.
Acknowledgements
We are extremely grateful to all our patients with ALS and caregivers who participated in this study. We also would like to thank to Prof. Matthew Kiernan, A/Prof Steve Vucic, the Multidisciplinary teams of Motor Neuron Disease clinics (Prince of Wales Hospital and St Joseph’s Hospital, Sydney) and The Motor Neurone Disease Association of New South Wales (MND NSW) and MND Australia.
References
- Merrilees J, Klapper J, Murphy J, Lomen-Hoerth C, Miller BL. Cognitive and behavioral challenges in caring for patients with frontotemporal dementia and amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2010;11(3):298–302. doi: 10.3109/17482961003605788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lillo P, Mioshi E, Zoing MC, Kiernan MC, Hodges JR. How common are behavioural changes in amyotrophic lateral sclerosis? Amyotroph Lateral Scler. 2011;12(1):45–51. doi: 10.3109/17482968.2010.520718. [DOI] [PubMed] [Google Scholar]
- Riedijk SR, De Vugt ME, Duivenvoorden HJ, Niermeijer MF, Van Swieten JC, Verhey FR, Tibben A. Caregiver burden, health-related quality of life and coping in dementia caregivers: a comparison of frontotemporal dementia and Alzheimer’s disease. Dement Geriatr Cogn Disord. 2006;22(5–6):405–412. doi: 10.1159/000095750. [DOI] [PubMed] [Google Scholar]
- Kaiser S, Panegyres PK. The psychosocial impact of young onset dementia on spouses. Am J Alzheimers Dis Other Demen. 2006;21(6):398–402. doi: 10.1177/1533317506293259. [DOI] [PubMed] [Google Scholar]
- Mourik JC, Rosso SM, Niermeijer MF, Duivenvoorden HJ, Van Swieten JC, Tibben A. Frontotemporal dementia: behavioral symptoms and caregiver distress. Dement Geriatr Cogn Disord. 2004;18(3–4):299–306. doi: 10.1159/000080123. [DOI] [PubMed] [Google Scholar]
- Knutson KM, Zamboni G, Tierney MC, Grafman J. Neural correlates of caregiver burden in cortical basal syndrome and frontotemporal dementia. Dement Geriatr Cogn Disord. 2008;26(5):467–474. doi: 10.1159/000167268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutoleau-Bretonniere C, Vercelletto M, Volteau C, Renou P, Lamy E. Zarit burden inventory and activities of daily living in the behavioral variant of frontotemporal dementia. Dement Geriatr Cogn Disord. 2008;25(3):272–277. doi: 10.1159/000117394. [DOI] [PubMed] [Google Scholar]
- Riedijk S, Duivenvoorden H, Rosso S, Van Swieten J, Niermeijer M, Tibben A. Frontotemporal dementia: change of familial caregiver burden and partner relation in a Dutch cohort of 63 patients. Dement Geriatr Cogn Disord. 2008;26(5):398–406. doi: 10.1159/000164276. [DOI] [PubMed] [Google Scholar]
- Mioshi E, Bristow M, Cook R, Hodges JR. Factors underlying caregiver stress in frontotemporal dementia and Alzheimer’s disease. Dement Geriatr Cogn Disord. 2009;27(1):76–81. doi: 10.1159/000193626. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontologist. 1980;20(6):649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- Dunkin JJ, Anderson-Hanley C. Dementia caregiver burden. Neurology. 1998;51(1 Suppl 1):S53–S60. doi: 10.1212/wnl.51.1_suppl_1.s53. [DOI] [PubMed] [Google Scholar]
- Gauthier A, Vignola A, Calvo A, Cavallo E, Moglia C, Sellitti L, Mutani R, Chio A. A longitudinal study on quality of life and depression in ALS patient-caregiver couples. Neurology. 2007;68(12):923–926. doi: 10.1212/01.wnl.0000257093.53430.a8. [DOI] [PubMed] [Google Scholar]
- Goldstein LH, Atkins L, Landau S, Brown R, Leigh PN. Predictors of psychological distress in carers of people with amyotrophic lateral sclerosis: a longitudinal study. Psychol Med. 2006;36(6):865–875. doi: 10.1017/S0033291706007124. [DOI] [PubMed] [Google Scholar]
- Nakagawa Y, Uozumi T, Tsuji S. [Quality of life and burden in caregivers for ALS patients in Japan] Rinsho Shinkeigaku. 2010;50(6):412–414. doi: 10.5692/clinicalneurol.50.412. [DOI] [PubMed] [Google Scholar]
- Pagnini F, Rossi G, Lunetta C, Banfi P, Castelnuovo G, Corbo M, Molinari E. Burden, depression, and anxiety in caregivers of people with amyotrophic lateral sclerosis. Psychol Health Med. 2010;15(6):685–693. doi: 10.1080/13548506.2010.507773. [DOI] [PubMed] [Google Scholar]
- Chio A, Vignola A, Mastro E, Giudici AD, Iazzolino B, Calvo A, Moglia C, Montuschi A. Neurobehavioral symptoms in ALS are negatively related to caregivers’ burden and quality of life. Eur J Neurol. 2010;17(10):1298–1303. doi: 10.1111/j.1468-1331.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- Ringholz GM, Appel SH, Bradshaw M, Cooke NA, Mosnik DM, Schulz PE. Prevalence and patterns of cognitive impairment in sporadic ALS. Neurology. 2005;65(4):586–590. doi: 10.1212/01.wnl.0000172911.39167.b6. [DOI] [PubMed] [Google Scholar]
- Witgert M, Salamone AR, Strutt AM, Jawaid A, Massman PJ, Bradshaw M, Mosnik D, Appel SH, Schulz PE. Frontal-lobe mediated behavioral dysfunction in amyotrophic lateral sclerosis. Eur J Neurol. 2010;17(1):103–110. doi: 10.1111/j.1468-1331.2009.02801.x. [DOI] [PubMed] [Google Scholar]
- Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, Nakanishi A. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. J Neurol Sci. 1999;169(1–2):13–21. doi: 10.1016/s0022-510x(99)00210-5. [DOI] [PubMed] [Google Scholar]
- Montes J, Levy G, Albert S, Kaufmann P, Buchsbaum R, Gordon PH, Mitsumoto H. Development and evaluation of a self-administered version of the ALSFRS-R. Neurology. 2006;67(7):1294–1296. doi: 10.1212/01.wnl.0000238505.22066.fc. [DOI] [PubMed] [Google Scholar]
- Wedderburn C, Wear H, Brown J, Mason SJ, Barker RA, Hodges J, Williams-Gray C. The utility of the Cambridge behavioural inventory in neurodegenerative disease. J Neurol Neurosurg Psychiatry. 2008;79(5):500–503. doi: 10.1136/jnnp.2007.122028. [DOI] [PubMed] [Google Scholar]
- Bozeat S, Gregory CA, Ralph MAL, Hodges JR. Which neuropsychiatric and behavioural features distinguish frontal and temporal variants of frontotemporal dementia from Alzheimer’s disease? J Neurol Neurosurg Psychiatry. 2000;69(2):178–186. doi: 10.1136/jnnp.69.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Orr N, Zarit JM. The hidden victims of Alzheimer’s disease: families under stress. New York: New York University Press; 1985. [Google Scholar]
- Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M. The zarit burden interview. Gerontologist. 2001;41(5):652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- Gundersen MD, Yaseen R, Midgard R. Incidence and clinical features of amyotrophic lateral sclerosis in More and Romsdal County, Norway. Neuroepidemiology. 2011;37(1):58–63. doi: 10.1159/000329523. [DOI] [PubMed] [Google Scholar]
- Huisman MH, de Jong SW, van Doormaal PT, Weinreich SS, Schelhaas HJ, van der Kooi AJ, de Visser M, Veldink JH, van den Berg LH. Population based epidemiology of amyotrophic lateral sclerosis using capture-recapture methodology. J Neurol Neurosurg Psychiatry. 2011;82(10):1165–1170. doi: 10.1136/jnnp.2011.244939. [DOI] [PubMed] [Google Scholar]
- Logroscino G, Traynor BJ, Hardiman O, Chio A, Mitchell D, Swingler RJ, Millul A, Benn E, Beghi E. Incidence of amyotrophic lateral sclerosis in Europe. J Neurol Neurosurg Psychiatry. 2010;81(4):385–390. doi: 10.1136/jnnp.2009.183525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbons ZC, Richardson A, Neary D, Snowden JS. Behaviour in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis. 2008;9(2):67–74. doi: 10.1080/17482960701642437. [DOI] [PubMed] [Google Scholar]
- Mioshi E, McKinnon C, Savage S, O’Connor CM, Hodges JR. Improving burden and coping skills in frontotemporal dementia caregivers: a pilot study. Alzheimer Dis Assoc Disord. 2012. Epub ahead of print. [DOI] [PubMed]
- Trail M, Nelson ND, Van JN, Appel SH, Lai EC. A study comparing patients with amyotrophic lateral sclerosis and their caregivers on measures of quality of life, depression, and their attitudes toward treatment options. J Neurol Sci. 2003;209(1–2):79–85. doi: 10.1016/s0022-510x(03)00003-0. [DOI] [PubMed] [Google Scholar]
- Miyashita M, Narita Y, Sakamoto A, Kawada N, Akiyama M, Kayama M, Suzukamo Y, Fukuhara S. Care burden and depression in caregivers caring for patients with intractable neurological diseases at home in Japan. J Neurol Sci. 2009;276(1–2):148–152. doi: 10.1016/j.jns.2008.09.022. [DOI] [PubMed] [Google Scholar]
- Goldstein LH, Adamson M, Jeffrey L, Down K, Barby T, Wilson C, Leigh PN. The psychological impact of MND on patients and carers. J Neurol Sci. 1998;160(Suppl 1):S114–121. doi: 10.1016/s0022-510x(98)00209-3. [DOI] [PubMed] [Google Scholar]
- Vignola A, Guzzo A, Calvo A, Moglia C, Pessia A, Cavallo E, Cammarosano S, Giacone S, Ghiglione P, Chio A. Anxiety undermines quality of life in ALS patients and caregivers. Eur J Neurol. 2008;15(11):1231–1236. doi: 10.1111/j.1468-1331.2008.02303.x. [DOI] [PubMed] [Google Scholar]
- Renton AE, Majounie E, Waite A, Simon-Sanchez J, Rollinson S, Gibbs JR, Schymick JC, Laaksovirta H, van Swieten JC, Myllykangas L. et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron. 2011;72(2):257–268. doi: 10.1016/j.neuron.2011.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeJesus-Hernandez M, Mackenzie IR, Boeve BF, Boxer AL, Baker M, Rutherford NJ, Nicholson AM, Finch NA, Flynn H, Adamson J. et al. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron. 2011;72(2):245–256. doi: 10.1016/j.neuron.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]