Abstract
Mindfulness-based stress reduction (MBSR) is thought to reduce emotional reactivity and enhance emotion regulation in patients with social anxiety disorder (SAD). The goal of this study was to examine the neural correlates of deploying attention to regulate responses to negative self-beliefs using functional magnetic resonance imaging. Participants were 56 patients with generalized SAD in a randomized controlled trial who were assigned to MBSR or a comparison aerobic exercise (AE) stress reduction program. Compared to AE, MBSR yielded greater (i) reductions in negative emotion when implementing regulation and (ii) increases in attention-related parietal cortical regions. Meditation practice was associated with decreases in negative emotion and social anxiety symptom severity, and increases in attention-related parietal cortex neural responses when implementing attention regulation of negative self-beliefs. Changes in attention regulation during MBSR may be an important psychological factor that helps to explain how mindfulness meditation training benefits patients with anxiety disorders.
Keywords: social anxiety, emotion regulation, mindfulness, fMRI, attention
INTRODUCTION
Mindfulness meditation is a form of mental training that has existed for more than two and a half millennia in the East and has recently become integrated into Western health care approaches (Chiesa and Serretti, 2011). Mindfulness-Based Stress Reduction (MBSR; Kabat-Zinn, 1990), the format of mindfulness training that has received the most empirical investigation, has been shown to reduce symptoms of stress, depression and anxiety (Hofmann et al., 2010). MBSR has been applied as an alternative clinical intervention for a variety of psychological [e.g. anxiety and depression disorders (Allen et al., 2006; Carmody, 2009; Chiesa and Serretti, 2009)] and chronic medical problems (Merkes, 2010).
Recently, researchers have begun to examine the mechanisms of action underlying MBSR. One candidate mechanism is emotion regulation, a key feature of mood and anxiety disorders and a popular target of many psychosocial clinical interventions (Campbell-Sills and Barlow, 2007). Recent studies have found that emotion regulation may (i) be related to dispositional mindfulness (Modinos et al., 2010) and (ii) enhanced with MBSR (Goldin and Gross, 2010). In the present study, we used functional magnetic resonance imaging (fMRI) to investigate changes in the neural bases of emotion regulation in a randomized controlled trial (RCT) of MBSR and aerobic exercise (AE) for adults diagnosed with generalized social anxiety disorder (SAD).
Mechanisms underlying MBSR
MBSR is associated with decreases in the habitual tendency to emotionally react to and ruminate about transitory thoughts and physical sensations (Teasdale et al., 2000; Ramel et al., 2004), stress, depression and anxiety symptoms (Segal et al., 2002; Evans et al., 2008; Chiesa and Serretti, 2009) and distorted self-view (Goldin et al., 2009c). MBSR is also associated with increases in behavioral self-regulation (Lykins and Baer, 2009), volitional orienting of attention (Jha et al., 2007) and emotion regulation (Goldin and Gross, 2010; Modinos et al., 2010).
There are a variety of emotion regulation strategies (Gross, 2007) with distinct neural circuitry and temporal features (Goldin et al., 2008). However, little is known about how MBSR influences emotion regulation abilities (Chambers et al., 2009). Preliminary evidence suggests that MBSR may influence the ability to exert cognitive control over negative rumination (Ramel et al., 2004), self-referential processes (Goldin et al., 2009c) and attention allocation and regulation (Slagter et al., 2008). Importantly, MBSR may be related to greater ability to disengage attention from aversive emotional stimuli (Lutz et al., 2008); thereby reducing emotional reactivity and enhancing the ability to implement emotion regulation strategies.
MBSR and SAD
One clinical context for examining the effects of MBSR on emotion regulation is SAD. SAD is a common, chronic and insidious psychiatric condition characterized by intense fear of evaluation and avoidance of social or performance situations (Stein and Stein, 2008). SAD involves a distorted attentional focus on internal cues (e.g. negative thoughts and self-imagery) and external cues (e.g. other’s facial expressions) during social situations (Schultz and Heimberg, 2008), which maintains social anxiety symptoms by interfering with natural habituation processes that lead to corrective learning (Heimberg and Becker, 2002).
Studies of patients with SAD have reported abnormal attentional processes consisting of early hypervigilance followed by attentional avoidance (i.e. reduced visual processing) of social threat (Mueller et al., 2008). Imaging studies with patients with SAD have begun to identify specific neural patterns related to these abnormal attentional processes. Findings include hyperactivity in brain regions related to immediate emotional reactivity (amygdala, insula) (Stein et al., 2007) and insufficient recruitment of brain networks implicated in cognitive reappraisal [dorsolateral prefrontal cortex (dlPFC), dorsomedial prefrontal cortex (dmPFC), dorsal anterior cingulate cortex (dACC)] and attention regulation [posterior cingulate (PC)/precuneus, inferior parietal lobe (IPL), supramarginal gyrus] when modulating responses to social threat (Goldin et al., 2009b) and negative self-beliefs (Goldin et al., 2009a).
Although effective cognitive–behavioral and pharmacological treatments have been developed for adults (Heimberg and Becker, 2002), investigating alternative approaches to help 30–40% of the patients who do not respond to traditional interventions is warranted (Stein and Stein, 2008). Preliminary evidence suggests that MBSR may be helpful for patients with SAD. MBSR has been found to improve mood, functionality and quality of life in patients with SAD (Koszycki et al., 2007). MBSR-related changes in self-referential processing and attention regulation have also been observed in patients with SAD (Goldin et al., 2009c; Goldin and Gross, 2010). More specifically, during attention regulation, increased recruitment of posterior (parietal and occipital) cortical attention-related brain regions from pre- to post-MBSR was related to decreased anxiety in patients with SAD (Goldin and Gross, 2010). While these initial studies are promising, little is known about how MBSR impacts emotion regulation, how it influences the neural bases of emotion regulation and how it compares in the context of an RCT to other alternative and effective interventions that have been shown to reduce stress and anxiety such as AE.
The present study
The goal of the present study was to investigate the differential effects of MBSR vs AE (an alternative stress reduction intervention) in the context of an RCT on the neural bases of emotion regulation of negative self-beliefs in patients with generalized SAD. To do this, we obtained behavioral and neural measures of emotion regulation during an fMRI experiment in patients with generalized SAD at baseline and again after being randomly assigned to MBSR or AE.
We chose AE as an alternative intervention for several reasons. Like MBSR, AE has been shown to improve both physical and mental health (Penedo and Dahn, 2005), especially symptoms of stress, depression and anxiety (Petruzzello et al., 1991; Stich, 1998; Ströhle, 2009) in clinical samples of mixed anxiety (e.g. Merom et al., 2007), panic disorder (e.g. Broocks et al., 1998; Dratcu, 2001) and generalized anxiety disorder (e.g. Steptoe et al., 1989; McEntee and Halgin, 1999). Similar to MBSR, it is a low-cost intervention that is readily available in the community. Furthermore, as implemented in this study, individual and group practice for both MBSR and AE were easy to match and control. In patients with SAD, the effects of AE on the neural bases of emotion regulation have not been examined or compared to MBSR in an RCT.
Compared to AE, we expected MBSR to be associated with greater (i) reduction of negative emotion and (ii) recruitment of posterior cortical attention-related brain regions during attention regulation. In the MBSR group, we expected meditation practice to be associated with decreased negative emotion and increased brain responses in attention-related posterior cortical regions from baseline to post-MBSR.
METHODS
Participants
Participants were patients seeking treatment for SAD and who met DSM-IV (Association, 1994) criteria for primary generalized SAD based on the Anxiety Disorders Interview Schedule for the DSM-IV-Lifetime version (DiNardo et al., 1994). Of the 316 individuals assessed for eligibility, 260 were excluded due to not meeting study criteria (173), other reasons (66) or declined to participate (21). The remaining 56 participants were randomly assigned to either MBSR (n = 31) or AE (n = 25) (Figure 1). Groups did not differ in gender, age, ethnicity or education (Table 1). Complete fMRI assessments at both baseline and post-intervention were available for 23 MBSR and 19 AE participants.
Fig. 1.
Consolidated standards of reporting trials (CONSORTs) diagram for a RCT of MBSR vs AE.
Table 1.
Demographic characteristics for patients randomized to MBSR or AE
| MBSR n = 31 | AE n = 25 | t-test or χ2 | |
|---|---|---|---|
| Females, n (%) | 19 (61.3) | 10 (40) | χ2 = 2.88 |
| Age (M ± SD) (years) | 32.87 ± 8.83 | 32.88 ± 7.97 | t = 0.42 |
| Ethnicity, n (%) | χ2 = 0.43 | ||
| Caucasian | 13 (41.9) | 10 (40) | |
| Asian | 14 (45.2) | 11 (44) | |
| Hispanic | 3 (9.7) | 1 (4) | |
| Multiracial | 1 (3.2) | 3 (12) | |
| Education (M ± SD) (years) | 16.40 ± 2.00 | 16.84 ± 2.64 | t = 0.34 |
| Current axis-I comorbidity | χ2 = 0.88 | ||
| Generalized anxiety disorder | 10 | 8 | |
| Major depressive disorder | 5 | 6 | |
| Dysthymia | 2 | 3 | |
| Specific phobia | 3 | 2 | |
| Panic disorder | 2 | 2 | |
| Agoraphobia | 1 | 2 | |
| Obsessive–compulsive disorder | 1 | 0 | |
| Past axis-I comorbidity | χ2 = 1.49 | ||
| Major depressive disorder | 9 | 2 | |
| Dysthymia | 1 | 0 | |
| Panic disorder | 1 | 0 | |
| Obsessive–compulsive disorder | 0 | 1 | |
| Substance abuse | 0 | 1 | |
| Eating disorder | 3 | 1 | |
| Past psychotherapy | 15 | 9 | χ2 = 1.84 |
| Past pharmacotherapy | 7 | 5 | χ2 = 1.56 |
Note. MBSR = Mindfulness-Based Stress Reduction, AE = aerobic exercise.
Participants passed an MRI safety screen and were excluded if they had current pharmacotherapy or psychotherapy, history of medical disorders or head trauma, or current psychiatric disorders other than SAD, generalized anxiety disorder, major depressive disorder, obsessive compulsive disorder, agoraphobia without a history of panic attacks or specific phobia. Participants were excluded if they had previously completed an MBSR course or if they had a regular meditation practice or AE regime (defined for our purposes as three or more times per week, for >2 months).
In MBSR participants, current Axis I comorbidity included 10 with generalized anxiety disorder, 5 with major depressive disorder, 3 with specific phobia, 2 with dysthymia, 2 with panic disorder, 1 with agoraphobia and 1 with obsessive–compulsive disorder. Past Axis I comorbidity included nine with major depressive disorder, three with eating disorders, one with panic disorder and one with dysthymia. Fifteen participants reported past, non-cognitive–behavioral psychotherapy and seven reported past pharmacotherapy.
In AE participants, current Axis I comorbidity included eight with generalized anxiety disorder, six with major depressive disorder, three with dysthymia, two with specific phobia, two with panic disorder and two with agoraphobia, Past Axis I comorbidity included two with major depressive disorder, one with substance abuse, one with eating disorder, 1 with obsessive–compulsive disorder and one with panic disorder. Nine participants reported past, non-cognitive behavioral psychotherapy and five reported past pharmacotherapy.
Procedure
All participants were recruited through web-based community listings and referrals from mental health providers. Participants were told on the phone that the study involved random assignment to two stress reduction programs. After passing a telephone screening, potential participants were administered the ADIS-IV-L (Di Nardo et al., 1994) by a clinical psychologist (P.G. or M.Z.). We enrolled patients with a principal diagnosis of generalized SAD (operationalized as moderate or higher severity (≥4 on a scale of 0–8) on the ADIS-IV-L (i) Clinician’s Severity Rating for SAD and (ii) social fear for five or more distinct social or performance situations in the SAD section. All participants provided informed consent in accordance with Stanford University Human Subjects Committee rules.
Participants were randomly assigned to 8 weeks of either MBSR or AE using Efron’s biased coin randomization procedure (Efron, 1971), which entails higher probability of allocation to the under-represented treatment group throughout the duration of the clinical trial. Randomization was done only after all baseline assessments (including fMRI) were completed.
Participants were administered self-report clinical and well-being measures (Jazaieri et al., 2012) and fMRI scanning assessments before and after MBSR and AE.
Interventions
Mindfulness-based stress reduction
We administered the standard MBSR program consisting of eight, weekly 2.5 h group classes, a 1-day meditation retreat and daily home practice. Participants were trained in formal meditation (i.e. breath-focus, body scan, open monitoring), informal practice and Hatha yoga. Daily logs were collected each week to measure group and individual meditation and yoga practice. Participants attended MBSR courses offered by seven different teachers in eight health care settings throughout the San Francisco Bay Area. MBSR instructors had 15.7 years (SD = 4.1 years, range = 10–20 years) of MBSR teaching experience. MBSR was offered at no-cost.
Aerobic exercise
We provided at no cost 2-month gym memberships to participants randomized to AE. To match the individual and group components of MSBR, participants in the AE intervention were required to complete at least two individual AE sessions and one group AE session (other than meditation or yoga) each week during the 8-week intervention.
Experimental task
A version of this task focused on cognitive reappraisal has been published (Goldin et al., 2009a). The version used here implemented a meta-cognitive attention regulation cued with a single word ‘observe’. The task consisted of five situations. The first was an experimenter-composed neutral situation about washing a car that was used to obtain baseline emotion ratings and fMRI BOLD signals for reading neutral statements. Then, four participant-generated autobiographical social anxiety situations characterized by social anxiety, humiliation and embarrassment were presented. For each situation, participants composed a paragraph describing the events, thoughts and feelings and five negative self-beliefs (NSBs) (e.g. I am incompetent; others think I am not normal). Participants indicated their age at the time of each situation and provided ratings, on a scales of 1 (not at all) to 9 (very much), of the vividness of the memory, their experience of shame at the time of the situation, as well as current shame, disturbance, avoidance and frequency of talking about the situation.
Five situations were presented in a single run lasting 15 min and 27 s. The sequence of instructions for the five situations was fixed: neutral, react NSB, regulate NSB, react NSB and regulate NSB. Each situation consisted of (i) an instruction to ‘react’ or ‘observe’ (6 s), (ii) 16 sentences (3 s each) in white font against a black background describing the situation, (iii) 10 NSBs (9 s each) embedded in the unfolding story in uppercase letters that flashed nine times (850 ms on and 150 ms off) and (iv) a negative emotion rating after each NSB (3 s) from 1 = not at all to 3 = moderately to 5 = extremely negative (Figure 2). Negative self-beliefs were flashed to maintain attention and appeared in white font for neutral and react trials and green for reappraisal trials. The task was programmed in Eprime (Psychology Software Tools, Inc) with a button response pad positioned in the participant’s right hand inside the magnet. Participants were trained prior to the baseline scan to react to NSBs by reflecting on how the NSB represents something that is true about the participant. Observing NSBs consisted of cultivating a present moment, meta-cognitive attentional perspective that focused on just noticing any thought, memory, emotion or sensation as it appeared and dissolved of its own accord without grasping at or rejecting any experience of body or mind.
Fig. 2.
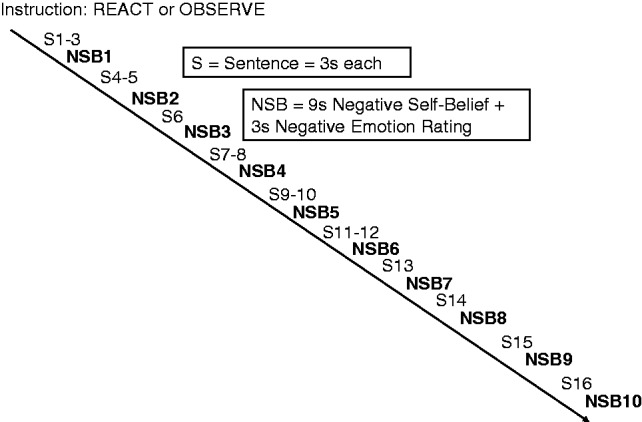
Structure of one autobiographical social situation block with 10 trials embedded.
Image acquisition
Imaging was performed on a General Electric 3-T Signa magnet with a T2*-weighted gradient echo spiral-in/out pulse sequence (Glover and Law, 2001) and a custom-built quadrature ‘dome’ elliptical bird cage head-coil (GE Healthcare, Milwaukee, WI, USA). Head movement was minimized using a bite-bar and foam padding. Across a single functional run, 618 functional volumes were obtained from 22 sequential axial slices (repetition time = 1500 ms, echo time = 30 ms, flip angle = 60°, field of view = 22 cm, matrix = 64 × 64, single-shot, resolution = 3.438 mm2 × 4.5 mm; voxel volume = 53.2 mm3). 3D high-resolution anatomical scans were acquired using fast spin-echo spoiled gradient recall (0.85942 × 1.5 mm; field of view = 22 cm, frequency encoding = 256).
fMRI data preprocessing
Analysis of functional neuroimages (AFNI) software (Cox, 1996) was used for preprocessing and statistical analysis. The functional run was subjected to preprocessing steps to maximize signal-to-noise contrast. This included an analysis of potential outliers, volume registration to a base image, motion correction, 4 mm3 isotropic Gaussian spatial smoothing, masking non-brain voxels, high-pass filtering (.011 Hz), linear detrending and conversion into BOLD signal percentage change in each voxel. No volumes demonstrated motion in the x, y or z directions in excess of ±0.8 mm. There was no evidence of stimulus-correlated motion, as assessed by correlations between condition-specific reference functions and x, y, z motion correction parameters (all P’s > 0.48).
fMRI statistical analysis
Multiple-regression was implemented with AFNI 3dDeconvolve and included baseline parameters to remove mean, linear and quadratic trends and motion-related variance in the BOLD signal. Regressors for the react NSBs, regulate NSBs and read neutral statements were convolved with the gamma variate model (Cohen, 1997) of the hemodynamic response function. Functional MRI BOLD signal intensity was computed as percentage of signal change [(MR signal per voxel per time point/mean MR signal in that voxel for the entire functional run) × 100].
Individual brain maps were converted to Talairach atlas space (Talairach and Tournoux, 1988) and second-level group statistical parametric maps were produced according to a random-effects model. To investigate interaction effects, a 2 Group (MBSR, AE) × 2 Time (pre, post) repeated-measures ANOVA (3dANOVA3 in AFNI) was implemented for regulate vs react NSBs. Follow-up t-tests examined within- and between-group effects.
To correct for multiple comparisons, we used 3dFWHMx to calculate the intrinsic smoothness of the noise (i.e. residual in the BOLD signal time series) for each subject. We then computed the group mean FWHM (5.44151) and entered this value into 3dClustSim with a gray matter mask generated by 3dAutomask. For a voxel-wise P = 0.004, 7.0 original size voxels (3.44 × 3.44 × 4.5 mm) are required to achieve a cluster-wise P-value of P = 0.05.
To examine the association of practice (meditation in MBSR and exercise in AE) and whole-brain BOLD responses for the contrast of regulate vs react NSB, we used AFNI 3dRegAna with the same thresholding procedure noted above.
RESULTS
Preliminary analyses
Of the 31 participants, 5(16%) dropped from MSBR, and of the 25, 2 (8%) participants dropped during AE, a non-significant difference, χ2 (1, N = 56) = 0.84, P = 0.36. Between-group t-tests showed that the average amount of practice time each week in the MBSR (M = 212, SD = 104 min) and AE (M = 196, SD = 86 min) groups did not differ [t(45) = 0.60, P > 0.55].
Below, we report the differential effects of MBSR vs AE on negative emotion ratings and neural responses when reacting to and regulating negative self-beliefs. Within MBSR and AE groups, separately, we report the association of practice (meditation or AE) with negative emotion ratings during emotion regulation and with thresholded whole-brain responses for the contrast of regulate vs react NSBs. The effects of MBSR and AE on clinical and well-being measures in patients with SAD is reported elsewhere (Jazaieri et al., 2012).
Emotional reactivity
Negative emotion
A 2 Group (MBSR, AE) × 2 Time (baseline, post) repeated-measures ANOVA for the negative emotion ratings yielded no interaction of group by time for negative emotion when reacting to NSBs [F(2,37) = 1.24, P > 0.27]. There was a main effect of time [F(2,37) = 24.48, P < 0.001, partial η2 ( ) = 0.40] and no effect of group [F(2,37) = 0.80, P = 0.38] (Figure 3). To rule out story effects, a paired t-test showed that there were no differential negative emotion responses to NSBs in all 56 participants during baseline react situation 1 vs 2 [t(55) = 1.45, P = 0.15].
) = 0.40] and no effect of group [F(2,37) = 0.80, P = 0.38] (Figure 3). To rule out story effects, a paired t-test showed that there were no differential negative emotion responses to NSBs in all 56 participants during baseline react situation 1 vs 2 [t(55) = 1.45, P = 0.15].
Fig. 3.

The effect of MBSR and AE on negative emotion ratings when reading neutral statements, reacting and regulating negative self-beliefs. *P < 0.05, **P < 0.005. Error bars = standard error of the mean.
Neural responses
A 2 Group (MBSR, AE) × 2 Time (baseline, post) repeated-measures ANOVA on BOLD responses for the contrast of react NSBs vs neutral statements resulted in interactions of group by time in one region: right ventrolateral PFC (Table 2). This effect was characterized by baseline to post-intervention BOLD response decrease for MBSR [% BOLD change = −0.07 %; t(22) = 2.90, P = 0.008] and increase for AE [% BOLD change = 0.06%; t(18) = 4.01, P = 0.001] groups. This suggests that both groups had a similar pattern of change in brain responses with only one brain dissociation in the prefrontal cortex.
Table 2.
BOLD Responses for interaction of Group (MBSR, AE) × Time (pre, post) for react negative self-beliefs vs read neutral statements and regulate vs react negative self-beliefs
| Brain regions (Cluster #) | BA | xa | ya | za | Vol (mm3) | F-value |
|---|---|---|---|---|---|---|
| React NSBs > read neutral | ||||||
| R ventrolateral prefrontal cortex | 10 | 21 | 45 | 5 | 529 | 15.8 |
| Read neutral > react NSBs | none | |||||
| Regulate > react NSBs | ||||||
| Parietal lobes | ||||||
| R SPL 3 | 7 | 24 | −72 | 53 | 426 | 8.2 |
| R IPL 2 | 40 | 52 | −58 | 50 | 479 | 10.5 |
| R IPL 5 | 40 | 58 | −41 | 46 | 372 | 13.7 |
| Occipital lobes | ||||||
| L lingual gyrus 4 | 18 | −21 | −68 | −2 | 372 | 9.3 |
| Cerebellum | ||||||
| Culmen 1 | 0 | −37 | −9 | 745 | 8.0 | |
| React > regulate NSBs | none |
aTalairach coordinates for voxel with peak BOLD % signal change.
F ≥ 7.66, voxel P < 0.004, minimum cluster volume threshold ≥372 mm3 (7 voxels × 3.438 mm2 × 4.5 mm), cluster-wise P < 0.05.
BA = Brodmann Area, BOLD = blood oxygen dependent, L = left, NSBs = negative self-beliefs, R = right, Vol = volume. The Cluster # after each brain region refers to Figure 5.
Emotion regulation
Negative emotion
To assess the effect of MBSR vs AE on emotion regulation of NSBs, we conducted 2 Group (MBSR, AE) × 2 Time (baseline, post) repeated-measures ANOVA on percent reduction of negative emotion when regulating NSBs. This analysis yielded an interaction of group by time [F(2,37) = 4.99, P = 0.03,  = 0.12], a main effect of group [F(1,37) = 4.10, P = 0.05,
= 0.12], a main effect of group [F(1,37) = 4.10, P = 0.05,  = 0.10] and no effect of time (P > 0.25). Follow-up t-tests revealed a significant increase in percent reduction of negative emotion from baseline to post-training for MBSR [t(20) = 2.13, P < 0.05,
= 0.10] and no effect of time (P > 0.25). Follow-up t-tests revealed a significant increase in percent reduction of negative emotion from baseline to post-training for MBSR [t(20) = 2.13, P < 0.05,  = 0.19], but not AE [t(17) = 0.98, P > 0.34] (Figure 3). To rule out story effects, a paired t-test showed that there were no differential negative emotion responses to NSBs in all 56 participants during baseline regulate situation 1 vs 2 [t(55) = 0.89, P = 0.37].
= 0.19], but not AE [t(17) = 0.98, P > 0.34] (Figure 3). To rule out story effects, a paired t-test showed that there were no differential negative emotion responses to NSBs in all 56 participants during baseline regulate situation 1 vs 2 [t(55) = 0.89, P = 0.37].
Among MBSR participants, total meditation practice was associated with greater percent reduction of negative emotion when implementing emotion regulation at post-MBSR [r(22) = 0.48, P = 0.02]. Among AE participants, there was no association of AE practice with percent reduction of negative emotion during emotion regulation (P > 0.69).
Neural responses
A 2 Group (MBSR, AE) × 2 Time (baseline, post) repeated-measures ANOVA on whole-brain BOLD responses for the contrast of regulate vs react NSBs yielded five significant interactions, including right superior parietal lobule (SPL), two regions within the right IPL, left lingual gyrus and cerebellar culmen (Table 2 and Figure 5). Follow-up t-tests in these interaction brain regions revealed baseline to post-MBSR BOLD response decreases in right posterior superior temporal gyrus (STG), and bilateral lingual gyrus, and increases in left IPL, right anterior IPL, right posterior IPL and right SPL. From baseline to post-AE, paired t-tests showed BOLD response decreases in right SPL and bilateral IPL and increases in right lingual gyrus.
Fig. 5.
BOLD responses for interaction of Group (MBSR, AE) × Time (Pre, Post) for regulate vs react negative self-beliefs contrast. Percent signal change = Change in BOLD signal from pre- to post-intervention. Interaction of Group by Time: F(2,40) ≥ 7.66, P = 0.004, Error bars = standard error of the mean. 1 = Culmen, 2 = Right IPL, 3 = Right SPL, 4 = Left Lingual Gyrus, 5 = Right IPL.
Among MBSR participants, total amount of meditation practice was associated with increased BOLD responses during regulate (vs react NSBs) after MBSR training in MPFC, left IPL, left middle occipital gyrus) (Table 3). There were no associations between meditation practice and react (vs regulate NSBs). Among AE participants, there were no associations between amount of AE and BOLD responses for regulate vs react NSBs or react vs regulate NSBs (all P’s >0.10).
Fig. 4.

Percent reduction in negative emotion during emotion regulation of negative self-beliefs at baseline and post-MBSR and AE. Interaction of Group by Time: F(2,37) = 4.99, P = 0.03,  = 0.12. Error bars = standard error of the mean. *P < 0.05
= 0.12. Error bars = standard error of the mean. *P < 0.05
Table 3.
Association between total amount of meditation and whole-brain BOLD signal for observe vs react NSBs at post-MBSR in 23 patients with SAD
| Brain regions | BA | x y za | Vol (mm3) | t-value | R2 |
|---|---|---|---|---|---|
| Observe > react | |||||
| Frontal lobes | |||||
| L medial prefrontal cortex | 6 | −10 −10 50 | 729 | 3.95 | 0.43 |
| Parietal lobes | |||||
| L IPL | 40 | −52 −37 39 | 1000 | 4.89 | 0.53 |
| Occipital lobes | |||||
| L Middle occipital gyrus | 19/31 | −28 −68 22 | 891 | 4.10 | 0.44 |
| React > observe–none |
aTalairach coordinates for voxel with peak t-value.
t-value threshold ≥ 3.14, voxel P < 0.005, minimum cluster volume threshold ≥ 372 mm3 (7 voxels × 4.5 mm× 3.438 mm2), cluster P < 0.05. BA = Brodmann area, x, y, z = Talairach and Tournoux coordinates, R2 = variance explained.
DISCUSSION
The goal of this study was to investigate how mindfulness meditation and AE stress reduction training programs differentially influence behavioral and neural outcomes in the context of emotion regulation. The target was present moment focused meta-cognitive attention regulation in patients with generalized SAD when they interacted with their own negative self-beliefs embedded in autobiographical social anxiety related situations.
Emotional reactivity
MBSR and AE resulted in equivalent reduction of self-reported negative emotional reactivity to NSBs. This converges with a prior study showing MBSR-related reduction in negative emotional reactivity to NSBs in patients with SAD (Goldin and Gross, 2010). This is the first study to demonstrate that AE reduces emotional reactivity to NSBs in patients with SAD.
The contrast of react NSBs vs read neutral statements yielded an interaction in the right ventrolateral PFC, characterized by baseline to post-intervention BOLD signal decrease for MBSR and increase for AE. Right ventrolateral PFC has been implicated in cognitive control processes including cognitive reappraisal of emotion (Ochsner and Gross, 2005), response inhibition (Aron et al., 2004) and expressive suppression (Goldin et al., 2008). This pattern of brain activity changes may be related to lesser automatic cognitive control of emotion experience while reacting to NSBs in MBSR.
Emotion regulation
MBSR, but not AE, resulted in a significant reduction in negative emotion to NSBs when implementing the attentional emotion regulation strategy deployed in the experimental task. This converges with prior findings of MBSR-related reduction in negative emotion when implementing breath-focused attention regulation of NSBs in patients with SAD (Goldin and Gross, 2010). The attention regulation strategy used here is a meta-cognitive attentional focus referred to as ‘open monitoring’ or ‘receptive awareness’ in various contemplative traditions. The degree of reduction in negative emotional reactivity with attentional emotion regulation at post-MBSR is similar to what has been reported during cognitive reappraisal of NSBs in patients with SAD (Goldin et al., 2009a). This suggests that distinct emotion regulation strategies are effective in patients with SAD.
Practice dose effects were observed for MBSR, but not AE. Meditation practice during MBSR was associated with lesser negative emotion during regulation of NSBs. The set of mindfulness meditation skills taught in MBSR may impact core features of SAD, namely, social fear, behavioral avoidance and exaggerated emotional reactivity by promoting a more flexible and adaptive attentional engagement with core negative self-beliefs. This is likely a result of the extensive training in recognizing habitual patterns of thinking and interpreting in conjunction with flexible implementation of meta-cognitive attention regulation. The absence of a practice effect in the AE group suggests that improvement in clinical and well-being measures with AE in patients with SAD (Jazaieri et al., 2012) is likely related to mechanisms other than meta-cognitive attention regulation, such as reduction in autonomic reactivity or anxiety sensitivity. However, this has yet to be investigated in the context of SAD.
Brain responses from the contrast of regulate vs react NSBs provide evidence for the role of posterior parietal attention-related brain regions in elucidating how MBSR trains attention processes in patients with SAD. The brain response interactions revealed a dissociation characterized by MBSR increases and AE decreases in three posterior parietal attention-related brain regions: right anterior IPL, right posterior IPL and right SPL. These brain regions have been implicated in attentional alerting to a stimulus (Fan et al., 2005). Enhanced recruitment of these brain regions following MBSR may reflect greater attentional engagement (rather than avoidance or distraction) with the emotional probe. MBSR-related increased activation in similar parietal cortex regions has been reported with breath-focused attention vs distraction in patients with SAD (Goldin and Gross, 2010).
Of note, similar to the pattern with self-reported negative emotion, there were practice dose effects on brain responses for MBSR, but not AE, specifically for the observe emotion regulation condition. Greater amount of meditation practice was related to greater BOLD responses for regulate vs react NSBs in brain regions implicated in cognitive (MPFC) and visual attention (IPL, middle occipital gyrus). This pattern of association suggests that MBSR enhancement of psychological flexibility may depend on the amount of meditation practice and functional integration of somatic–attention–cognitive control brain systems.
Implications
While MBSR has been shown to reduce symptoms of stress, anxiety and depression, this RCT of MBSR vs AE provides evidence that changes in attention regulation may be related to well-established beneficial effects of mindfulness meditation. Specifically, MBSR, but not AE, was associated with increased ability to downregulate negative emotional reactivity to their own NSBs during the observe condition during which participants were attempting to implement one type of meta-cognitive attention regulation. Importantly, this indicates that specific emotion regulation strategies with distinct neural architectures can be effective in the same clinical sample. For example, increases in cognitive reappraisal, which involves logical reasoning, linguistic processing and modification of meaning, has been shown to mediate reduction of SAD symptoms (Goldin et al., 2012). This study shows that a meta-cognitive attention regulation strategy, which does not rely on logical reasoning, linguistic processing and modification of meaning, may also be effective in SAD patients.
Limitations
The current study is limited to inferences about a single emotion regulation strategy, (present moment, meta-cognitive attention regulation) for only one type of SAD-related emotional probe (NSBs). A direct comparison of multiple emotion regulation strategies for different anxiety-inducing probes will be important to consider in future studies. This study used a fixed order of only four autobiographical situations. Future studies may benefit from using a random sequence of many more types of autobiographical life situations.
In the present study, the AE active comparison training was useful for matching both individual and group practice components of MBSR. However, given that MBSR provides multiple tools for learning the skill of mindfulness, it may be helpful to add an active training program that also teaches a new non-meditative mental skill, for example, visualization as a tool for enhancing memory ability. Future studies will also benefit from adding a waitlist control group.
While this study investigated brain changes before and after MBSR, to address the issue of optimal treatment matching, future analyses should determine if behavioral and neural signals during emotion regulation at baseline can predict who will maximally benefit from MBSR or AE (i.e. moderator analysis). To better understand how MBSR and AE work, an analysis of underlying mechanisms might investigate whether changes in BOLD responses from baseline to post-intervention predict longer term clinical status (i.e. mediator analysis). Specifically, future studies may consider investigating whether and how changes in emotion regulation strategy during treatment are related to clinical outcomes.
Funding
National Center for Complimentary and Alternative Medicine Institutes of Health awarded to James Gross [Grant AT003644].
Conflict of Interest
None declared.
Acknowledgments
The authors of this manuscript do not have any direct or indirect conflicts of interest, financial or personal relationships or affiliations to disclose. This work was supported by the National Center for Complimentary and Alternative Medicine Institutes of Health awarded to James Gross [Grant AT003644].
REFERENCES
- Allen NB, Chambers R, Knight W. Mindfulness-based psychotherapies: a review of conceptual foundations, empirical evidence and practical considerations. Australian & New Zealand Journal of Psychiatry. 2006;40:285–94. doi: 10.1080/j.1440-1614.2006.01794.x. [DOI] [PubMed] [Google Scholar]
- Aron AR, Robbins TW, Poldrack RA. Inhibition and the right inferior frontal cortex. Trends in Cognitive Science. 2004;8:170–7. doi: 10.1016/j.tics.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Association AP. Diagnostic and Statistical Manual of Mental Disorders. 4 edn. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Broocks A, Bandelow B, Pekrun G, et al. Comparison of aerobic exercise, clomipramine, and placebo in the treatment of panic disorder. American Journal of Psychiatry. 1998;155:603–9. doi: 10.1176/ajp.155.5.603. [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Barlow DH. Incorporating emotion regulation into conceptualizations and treatments of anxiety and mood disorders. In: Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford; 2007. pp. 542–59. [Google Scholar]
- Carmody J. Evolving conceptions of mindfulness in clinical settings. Journal of Cognitive Psychotherapy. 2009;23:270. [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: an integrative review. Clinical Psychology Review. 2009;29:56072. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. Journal of Alternative and Complementary Medicine. 2009;15:593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Research. 2011;187:441–53. doi: 10.1016/j.psychres.2010.08.011. [DOI] [PubMed] [Google Scholar]
- Cohen MS. Parametric analysis of fMRI data using linear systems methods. Neuroimage. 1997;6:93–103. doi: 10.1006/nimg.1997.0278. [DOI] [PubMed] [Google Scholar]
- Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research. 1996;29:162–73. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L) San Antonio, TX: Psychological Corporation; 1994. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Dratcu L. Physical exercise: an adjunctive treatment for panic disorder? European Psychiatry. 2001;16:372–4. doi: 10.1016/s0924-9338(01)00593-4. [DOI] [PubMed] [Google Scholar]
- Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403. [Google Scholar]
- Evans S, Ferrando S, Findler M, Stowell C, Smart C, Haglin D. Mindfulness-based cognitive therapy for generalized anxiety disorder. Journal of Anxiety Disorders. 2008;22:716–21. doi: 10.1016/j.janxdis.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Fan J, McCandliss BD, Fossella J, Flombaum JI, Posner MI. The activation of attentional networks. Neuroimage. 2005;26:471–9. doi: 10.1016/j.neuroimage.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Glover GH, Law CS. Spiral-in/out BOLD fMRI for increased SNR and reduced susceptibility artifacts. Magnetic Resonance in Medicine. 2001;46:515–22. doi: 10.1002/mrm.1222. [DOI] [PubMed] [Google Scholar]
- Goldin P, Ziv M, Jazaieri H, Werner K, Kraemer H, Heimberg RG, Gross JJ. Cognitive Reappraisal Self-Efficacy Mediates the Effects of Individual Cognitive-Behavioral Therapy for Social Anxiety Disorder. Journal of Consulting and Clinical Psychology. 2012 doi: 10.1037/a0028555. May 14, 2012, No Pagination Specified. doi:10.1037/a0028555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. 2010;10:83. doi: 10.1037/a0018441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Manber-Ball T, Werner K, Heimberg R, Gross JJ. Neural mechanisms of cognitive reappraisal of negative self-beliefs in social anxiety disorder. Biological Psychiatry. 2009a;66:1091–9. doi: 10.1016/j.biopsych.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Manber T, Hakimi S, Canli T, Gross JJ. Neural bases of social anxiety disorder: emotional reactivity and cognitive regulation during social and physical threat. Archives of General Psychiatry. 2009b;66:170–80. doi: 10.1001/archgenpsychiatry.2008.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, McRae K, Ramel W, Gross JJ. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biological Psychiatry. 2008;63:577–86. doi: 10.1016/j.biopsych.2007.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ramel W, Gross JJ. Mindfulness meditation training and self-referential processing in social anxiety disorder: behavioral and neural effects. Journal of Cognitive Psychotherapy. 2009c;23:242–56. doi: 10.1891/0889-8391.23.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross, J.J., editor. (2007). The Handbook of Emotion Regulation. New York, NY: Guilford Press. [Google Scholar]
- Heimberg RG, Becker RE. Cognitive-Behavioral Group therapy for Social Phobia: Basic Mechanisms and Clinical Strategies. New York: Guilford Press; 2002. [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78:169. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jazaieri H, Goldin P, Werner K, Ziv M, Heimberg R, Gross JJ. A randomized clinical trial of mindfulness-based stress reduction versus aerobic exercise for social anxiety disorder. Journal of Clinical Psychology. 2012;68:715–731. doi: 10.1002/jclp.21863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AP, Krompinger J, Baime MJ. Mindfulness training modifies subsystems of attention. Cognitive Affective and Behavioral Neuroscience. 2007;7:109–19. doi: 10.3758/cabn.7.2.109. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Dell Publishing; 1990. [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behavior Research and Therapy. 2007;45:2518–26. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends in Cognitive Sciences. 2008;12:163–9. doi: 10.1016/j.tics.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lykins ELB, Baer RA. Psychological functioning in a sample of long-term practitioners of mindfulness meditation. Journal of Cognitive Psychotherapy. 2009;23:226. [Google Scholar]
- McEntee DJ, Halgin RP. Cognitive group therapy and aerobic exercise in the treatment of anxiety. Journal of College Student Psychotherapy. 1999;13:39–58. [Google Scholar]
- Merkes M. Mindfulness-based stress reduction for people with chronic diseases. Australian Journal of Primary Health. 2010;16:200–10. doi: 10.1071/PY09063. [DOI] [PubMed] [Google Scholar]
- Merom D, Phongsavan P, Wagner R, et al. Promoting walking as an adjunct intervention to group cognitive behavioral therapy for anxiety disorders: a pilot group randomized trial. Journal of Anxiety Disorders. 2007;22:959–68. doi: 10.1016/j.janxdis.2007.09.010. [DOI] [PubMed] [Google Scholar]
- Modinos G, Ormel J, Aleman A. Individual differences in dispositional mindfulness and brain activity involved in reappraisal of emotion. Social Cognitive and Affective Neuroscience. 2010;5:369–77. doi: 10.1093/scan/nsq006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller EM, Hofmann SG, Santesso DL, Meuret AE, Bitran S, Pizzagalli DA. Electrophysiological evidence of attentional biases in social anxiety disorder. Psychological Medicine. 2008;39:1141–1152. doi: 10.1017/S0033291708004820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochsner KN, Gross JJ. The cognitive control of emotion. Trends in Cognitive Science. 2005;9:242–9. doi: 10.1016/j.tics.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Current Opinion in Psychiatry. 2005;18:189–93. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- Petruzzello SJ, Landers AC, Hatfield BD, Kubitz KA, Salazar W. A meta-analysis on the anxiety-reducing effect of acute and chronic exercise: outcomes and mechanisms. Sports Medicine. 1991;11:143–82. doi: 10.2165/00007256-199111030-00002. [DOI] [PubMed] [Google Scholar]
- Ramel W, Goldin PR, Carmona PE, McQuaid JR. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cognitive Therapy and Research. 2004;28:433. [Google Scholar]
- Schultz LT, Heimberg RG. Attentional focus in social anxiety disorder: potential for interactive processes. Clinical Psychology Review. 2008;28:1206–21. doi: 10.1016/j.cpr.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guildford Press; 2002. [Google Scholar]
- Slagter HA, Lutz A, Greischar LL, Nieuwenhuis S, Davidson RJ. Theta phase synchrony and conscious target perception: impact of intensive mental training. Journal of Cognitive Neuroscience. 2008;21:1536–49. doi: 10.1162/jocn.2009.21125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Simmons AN, Feinstein JS, Paulus MP. Increased amygdala and insula activation during emotion processing in anxiety-prone subjects. American Journal of Psychiatry. 2007;164:318–27. doi: 10.1176/ajp.2007.164.2.318. [DOI] [PubMed] [Google Scholar]
- Stein MB, Stein DJ. Social anxiety disorder. Lancet. 2008;371:1115–25. doi: 10.1016/S0140-6736(08)60488-2. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Edwards S, Moses J, Mathews A. The effects of exercise training on mood and perceived coping ability in anxious adults from the general population. Journal of Psychosomatic Research. 1989;33:537–47. doi: 10.1016/0022-3999(89)90061-5. [DOI] [PubMed] [Google Scholar]
- Stich FA. A meta-analysis of physical exercise as a treatment for symptoms of anxiety adults from the general population. Psychosomatic Research. 1998;33:537–47. [Google Scholar]
- Ströhle A. Physical activity, exercise, depression and anxiety disorders. Journal of Neural Transmission. 2009;116:777–84. doi: 10.1007/s00702-008-0092-x. [DOI] [PubMed] [Google Scholar]
- Talairach J, Tournoux P. Co-planar Stereotaxic Atlas of the Human Brain. New York: Thieme; 1988. [Google Scholar]
- Teasdale JT, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology. 2000;68:615–23. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]




