Abstract
Background
All clinical and biological manifestations related to postcardiac arrest (CA) syndrome are attributed to ischemia–reperfusion injury in various organs including brain and heart. Molecular hydrogen (H2) has potential as a novel antioxidant. This study tested the hypothesis that inhalation of H2 gas starting at the beginning of cardiopulmonary resuscitation (CPR) could improve the outcome of CA.
Methods and Results
Ventricular fibrillation was induced by transcutaneous electrical epicardial stimulation in rats. After 5 minutes of the subsequent CA, rats were randomly assigned to 1 of 4 experimental groups at the beginning of CPR: mechanical ventilation (MV) with 2% N2 and 98% O2 under normothermia (37°C), the control group; MV with 2% H2 and 98% O2 under normothermia; MV with 2% N2 and 98% O2 under therapeutic hypothermia (TH), 33°C; and MV with 2% H2 and 98% O2 under TH. Mixed gas inhalation and TH continued until 2 hours after the return of spontaneous circulation (ROSC). H2 gas inhalation yielded better improvement in survival and neurological deficit score (NDS) after ROSC to an extent comparable to TH. H2 gas inhalation, but not TH, prevented a rise in left ventricular end-diastolic pressure and increase in serum IL-6 level after ROSC. The salutary impact of H2 gas was at least partially attributed to the radical-scavenging effects of H2 gas, because both 8-OHdG- and 4-HNE-positive cardiomyocytes were markedly suppressed by H2 gas inhalation after ROSC.
Conclusions
Inhalation of H2 gas is a favorable strategy to mitigate mortality and functional outcome of post-CA syndrome in a rat model, either alone or in combination with TH.
Keywords: cardiac arrest, cardiopulmonary resuscitation, hydrogen gas, therapeutic hypothermia, ventricular fibrillation
Introduction
Despite advances in the management of patients who suffer a nontraumatic cardiac arrest (CA), survival rates remain low, and many survivors are left with neurological and cardiac sequelae.1 Post-CA syndrome, including neurological dysfunction, cardiac damage, and “sepsis-like” systemic inflammation, is likely to contribute to the multisystem organ dysfunction and ultimate demise of many CA victims.2 Therapeutic hypothermia (TH) is widely accepted as the gold-standard method to improve survival and limit neurological outcomes in patients who achieve return of spontaneous circulation (ROSC) after CA. Despite that, it is still underutilized.3 Thus, the development of alternative approaches with or without TH is an unmet medical need in ameliorating the prognosis of post-CA patients.
Molecular hydrogen (H2) has many potential therapeutic applications as a novel antioxidant.4,5 Since the first article reporting H2 effects, in Nature Medicine in 2007,6 the protective effects of H2 have been confirmed in different animal models, including limiting the infarct volume of brain6 and heart7 by reducing ischemia–reperfusion injury without altering hemodynamic parameters and providing protection against multiple-organ damage elicited by generalized inflammation.8 There are also some preliminary clinical data on this topic.9–17
All clinical and biological manifestations related to post-CA syndrome are attributed to ischemia–reperfusion injury in various organs including brain and heart. This study tested the hypothesis that inhalation of H2 gas during hyperoxic resuscitation can improve CA outcome. TH was chosen as the gold standard endorsed by professional societies and backed up by a significant body of evidence.18–25 We subjected rats to 5 minutes of ventricular fibrillation (VF) cardiac arrest (CA), followed by therapeutic hypothermia (TH), H2 treatment, or a combination of both. Controls were subjected to normothermic conditions. All groups were ventilated with 98% O2.
Materials and Methods
Animal Preparation
Fifteen-week-old male Wistar ST rats weighing an average of 373 g were used according to institutional approval by the Animal Ethics Committee. Rats were housed in a rodent facility under a 12-hour light–dark cycle during this study.
For experiments, rats were fasted overnight except for free access to water and then anesthetized with an intraperitoneal injection of pentobarbital sodium (45 mg/kg). The surgical procedures were carried out as previously described.19,20 The tracheas of the animals were intubated through a tracheostomy with a 14-gauge cannula and mechanically ventilated with a tidal volume (TV) of 0.65 mL/100 g, a respiratory rate (RR) of 100/min, and an FiO2 of 0.21 (Ventilator: SN-480-7, Shinano, Japan). Polyethylene catheters (PE50, Natsume, Japan) were inserted into the left femoral artery and vein and flushed intermittently with saline solution containing 2.5 IU/mL bovine heparin. Arterial blood pressure was measured, and an electrocardiogram was recorded by subcutaneous needle electrodes. Core temperature was monitored by a rectal temperature probe (BAT-10, Physitemp Instruments Inc) and maintained by a heating plate (SCP-85, AsOne, Japan) throughout the experiment to ensure appropriate temperature management.
Ventricular Fibrillation and CPR
Ventricular fibrillation (VF) was induced by electrical stimulation via a transthoracic epicardium electrode, as previously described.26 The stimulator (Isostim, World Precision Instrument Inc) was used to perform direct and constant electrical stimulation of the epicardium with crude current, continuous single stimulation, a delay of 100 ms, a wave width of 1 ms, a frequency of 50 Hz, an intensity of 1 mA, and a stimulation duration of 3 minutes. Five minutes after initiation of VF, advanced cardiac life support was started; the rats were ventilated (0.65 mL/100 g, 100 breaths/min), and then chest compressions (200/min) were started by a finger of the same investigator using a metronome assistant. Adrenalin (2 μg/100 g) and 0.1 mL sodium bicarbonate (8.4%) were immediately administered to the rats at the beginning of CPR. Repeated doses were administered at 3-minute intervals as needed. Defibrillation (Nihon Koden, Tokyo, Japan) was performed with direct-current single-phase wave 3 J if the electrocardiogram displayed VF 1 minute after CPR. If the defibrillation failed, CPR was repeated, and defibrillations were again performed 1 minute after CPR. If the spontaneous circulation of the rats was not restored after 10 minutes with the above treatment, CPR was considered a failure.
After ROSC, rats were mechanically ventilated and invasively monitored for 2 hours in maintaining the target temperature. Rats were continuously given 1 mL/h isotonic saline for 2 hours after ROSC. After a recovery period of 2 hours, telemetry probes (Mini mitter, Respironics Inc) were implanted into the inguinal cavities to monitor activity. Rats were then weaned from the ventilator, extubated, and returned to their cages with easily accessible food and water. The survival time after CPR was recorded up to 72 hours.
Experimental Protocol
Rats were randomly assigned to 1 of 4 experimental groups when mechanical ventilation (MV) was resumed at the beginning of CPR: MV with 2% N2 and 98% O2 at normothermia (the control group), MV with 2% H2 and 98% O2 at normothermia (H2 group), MV with 2% N2 and 98% O2 in targeting therapeutic hypothermia (the TH group), and MV with 2% H2 and 98% O2 in targeting TH (the H2+TH group) (Figure 1). The concentration of H2 in the gas mixture was determined using the Breath Gas Analyzer Model TGA-2000 (TERAMECS, Kyoto, Japan).
Figure 1.
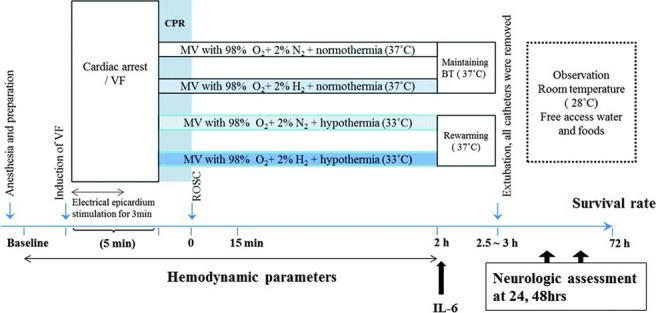
Experimental protocol of CPR and postresuscitation care in VF-induced cardiac arrest model. When mechanical ventilation was resumed (start CPR), rats were assigned to 1 of 4 experimental groups: mechanical ventilation (MV) with 98% O2+2% nitrogen (N2), the control group; MV with 98% O2+2% hydrogen (H2), the H2 group; MV with 98% O2+2% N2+therapeutic hypothermia (TH), the TH group; and MV with 98% O2+2% H2+TH, the H2+TH group. VF indicates ventricular fibrillation; MV, mechanical ventilation; BT, body temperature; and ROSC, return of spontaneous circulation.
Baseline variables (weight, blood pressure, heart rate, body temperature, and preparation time) were the same in the 4 groups (Table 1).
Table 1.
Baseline Physiological Variables
| Control (n=14) | H2 (n=14) | TH (n=14) | H2+TH (n=13) | |
|---|---|---|---|---|
| Weight, g | 373.6±6.1 | 367.5±7.9 | 376.4±8.6 | 375.9±4.8 |
| Preparation time, minutes | 42.4±1.2 | 41.7±0.8 | 40.1±0.8 | 40.1±1.2 |
| HR at baseline, bpm | 398±9 | 377±10 | 399±6 | 361±25 |
| MBP at baseline, mm Hg | 133±3 | 124±5 | 122±5 | 120±5 |
| Temperature at baseline, °C | 36.0±0.0 | 37.0±0.0 | 36.9±0.0 | 36.9±0.0 |
Values expressed as mean±SEM. TH indicates therapeutic hypothermia; HR, heart rate; MBP, mean blood pressure; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
The concentration of 2% H2 was determined on the basis of previous observations7 as an optimal and safe concentration. Rats under ventilation received the respective gases via the tracheal tube until 2 hours after ROSC. In animals assigned to TH, body cooling was initiated coincident with the start of CPR. Rectal temperature was measured with a digital thermometer (BAT-10, Physitemp Instruments Inc) and taken as the body temperature, which was reduced to 33°C within 15 minutes with the aid of ice packs and a cooling plate (SCP-85, AsOne, Japan). Once reached, the target temperature was maintained for 2 hours after CPR and then returned to 37°C over a rewarming period of 30 to 60 minutes. For those animals not subjected to cooling, rectal temperature was maintained at 37°C using a hot plate (SCP-85, AsOne, Japan) for 1 hour after resuscitation. The analytical methods comprised 3 parts. In part 1, rats were divided randomly into 4 groups as described above; their neurological deficits were evaluated 24 and 48 hours after ROSC and their survival rate monitored up to 72 hours after ROSC. Arterial blood for blood gas analysis and peripheral venous blood was obtained at baseline and 10, 60, 90, and 120 minutes after ROSC. In part 2, myocardial functional recovery was monitored during the first 2 hours after ROSC, and then serum samples were obtained to measure cytokines level. In part 3, the sham-operated animals and the resuscitated animals, with or without H2 inhalation, were decapitated 24 hours after ROSC. The same surgical procedures, monitoring, and control of body temperature except for the induction of VF were done for the sham animals. Wet-to-dry weight ratios were measured for lung. Histopathological analyses of heart were performed to evaluate the favorable effect of H2 gas inhalation.
Neurological Deficit Evaluation
Neurological deficit score (NDS) evaluations were performed by a single investigator who was unaware of group assignment. Consciousness and breathing, cranial nerve reflexes, motor function, sensory function, and coordination were scored according to an NDS system (0% to 100% scale; 0 normal, 100 brain death), as described previously.27
Evaluation of Postresuscitation Myocardial Function
A Millar transducer catheter (SPR-320) was placed in the left ventricle (LV) cavity via the right internal carotid artery to monitor LV pressure using the polygraph system (Power Lab, ADInstrument, Castle Hill, Australia) before the induction of VF. LV systolic pressure (LVSP), LV end-diastolic pressure (LVEDP), and peak positive dP/dt and negative dP/dt were monitored during the first 2 hours after ROSC.
Measurement of Serum IL-6 Level
Serum concentrations of IL-6 were measured 2 hours after ROSC in the 4 experimental groups and a sham-operated control group without VF with an ELISA Kit (OptEIA, BD Biosciences) according to the manufacturer's instructions.
Lung Water Content Determined by Wet–Dry Method
Twenty-four hours after ROSC, the right lower lobes of the lungs were removed in a standard fashion, weighed immediately after removal, and then placed in a laboratory oven (60°C) for slow evaporation over 72 hours. The dried samples were weighed, and the water content (%) was calculated as (wet weight−dry weight)/(wet weight)×100%.
Histopathological Analysis
Twenty-four hours after ROSC, the rats were decapitated. The hearts were quickly removed and fixed with Zamboni's solution. Coronal tissue slices (6-μm thickness) of the hearts (at the level of the left ventricle papillary muscle) were stained with hematoxylin and eosin and/or Azan–Mallory for histological evaluation.
For immunohistochemistry, the fixed sections were immunostained overnight at 4°C using a mouse monoclonal antibody against 4-hydroxy-2-nonenal (4-HNE; Japan Institute for the Control of Aging, NIKKEN SEIL Co, Ltd) to assess lipid peroxidation or a mouse monoclonal antibody against 8-hydroxy-deoxyguanosine (8-OHdG; Japan Institute for the Control of Aging, NIKKEN SEIL Co, Ltd) to detect the extent of nucleic acid oxidation.
In each Azan–Mallory-, 4-HNE-, and 8-OHdG-stained section, 4 slide fields were randomly examined using a defined rectangular field area (0.14 mm2). Images of Azan and 4-HNE staining were analyzed using Adobe Photoshop CS 5.1, and data of each staining section are reported as fibrotic tissue area stained blue (%) and 4-HNE relative intensity area (%) using automated counting software (Image J 1.46r, National Institute of Health). The 8-OHdG-positive cells were counted using automated counting software (Image J 1.46r, National Institute of Health), and the data were represented as the number of 8-OHdG-positive cells per field. A fluorescence microscope (Biorevo BZ-9000, Keyence, Osaka, Japan) was used for imaging.
Statistical Analysis
Continuous variables are expressed as mean±SEM. Normally distributed data were analyzed by 1-way analysis of variance (ANOVA) with Bonferroni correction for post hoc comparisons between multiple experimental groups. NDSs were analyzed by Kruskal–Wallis with Mann–Whitney U analyses between multiple groups because the values are categorical variables. Kaplan–Meier analysis and the log-rank test were used to calculate survival rates. Hemodynamic and laboratory data were examined by a mixed-effects model for repeated-measures analyses, followed by ANOVA with Bonferroni correction for post hoc comparisons. The mixed-effects model for repeated-measures analysis contained treatment group, time, and treatment-by-time interaction as factors and random intercept for each subject. Significance was considered at the level of P<0.05. The Bonferroni-adjusted P value was defined such that the raw P value multiplies the number of comparisons. Statistical analyses were performed using SPSS software (SPSS Inc, Chicago, IL).
Results
Inhalation of H2 Gas Improved Early Post-ROSC Survival After Cardiac Arrest With Ventricular Fibrillation
First, we compared inhaled H2 gas with TH for the effect on early post-ROSC survival after VF-induced CA. Post-CA rats were assigned to the control group, H2 group, TH group, or H2+TH group at the time of CPR. There was no significant difference in terms of procedures for performing CPR, including CPR time to ROSC, dose of epinephrine, and number of defibrillations (Table 2). The resuscitation rates were 92.4% (13 survivors of 14 rats) in the control group, 92.4% (13 survivors of 14 rats) in the H2 group, 92.4% (13 survivors of 14 rats) in the TH group, and 100% (13 survivors of 13 rats) in the H2+TH group, respectively.
Table 2.
Physiological Variables and Therapies During Cardiopulmonary Resuscitation
| Control (n=14) | H2 (n=14) | TH (n=14) | H2+TH (n=13) | |
|---|---|---|---|---|
| CPR time to ROSC, seconds | 117±20 | 99±18 | 109±11 | 106±18 |
| Total dose of epinephrine, μg | 8.5±1.0 | 8.0±0.8 | 8.0±0.0 | 8.5±0.5 |
| Total administration of defibrillation | 1.0±0.2 | 0.9±0.2 | 1.2±0.2 | 1.0±0.1 |
| ROSC rate, n (%) | 13 (92.9) | 13 (92.9) | 13 (92.9) | 13 (100) |
| Temperature at the end of 2-hour protocol, °C | 36.9±0.0 | 36.9±0.0 | 33.0±0.0*† | 32.8±0.0*† |
Values expressed as mean±SEM. TH indicates therapeutic hypothermia; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
P<0.001 compared with the control group.
P<0.001 compared with the H2 group.
Arterial oxygen partial pressure (PaO2) was higher in the TH group compared with the controlled normothermia group, whereas serum potassium levels 60 and 120 minutes after ROSC were lower in the TH group compared with the controlled normothermia group. These results were consistent with evidence that hypothermia reduces oxygen consumption by 6% to 10% per degree Celsius23 and could potentially induce electrolyte loss.23 The groups did not differ in terms of partial pressure of carbon dioxide (PaCO2), pH, base excess, hematocrit, or lactate (Table 3).
Table 3.
Group Arterial Blood Gas Analyses and Lactate Concentration Before Cardiac Arrest and in 2 Hours After Return of Spontaneous Circulation
| After ROSC | ||||
|---|---|---|---|---|
| Baseline | 10 Minutes | 60 Minutes | 120 Minutes | |
| pH | ||||
| Control | 7.48±0.03 | 7.18±0.02 | 7.37±0.02 | 7.36±0.03 |
| H2 | 7.53±0.02 | 7.20±0.01 | 7.38±0.01 | 7.38±0.01 |
| TH | 7.51±0.01 | 7.19±0.01 | 7.35±0.01 | 7.31±0.01 |
| H2+TH | 7.53±0.01 | 7.18±0.01 | 7.36±0.00 | 7.34±0.00 |
| PaO2, mm Hg** | ||||
| Control | 86±3 | 314±51 | 438±35 | 480±19 |
| H2 | 92±7 | 319±41 | 364±27 | 481±21 |
| TH | 84±3 | 513±38#† | 575±19##†† | 582±21##†† |
| H2+TH | 92±4 | 433±41 | 534±22†† | 571±19#† |
| PaCO2, mm Hg | ||||
| Control | 29.9±1.3 | 41.3±2.6 | 38.7±2.7 | 38.8±3.9 |
| H2 | 28.9±1.7 | 42.5±1.8 | 36.9±2.2 | 38.1±1.9 |
| TH | 30.9±1.3 | 43.1±3.1 | 39.5±2.2 | 42.8±2.5 |
| H2+TH | 28.9±0.7 | 46.8±2.1 | 38.0±1.1 | 42.3±1.2 |
| Na, mmol/L | ||||
| Control | 139.8±0.5 | 140.7±1.0 | 140.3±0.6 | 139.5±0.5 |
| H2 | 139.4±0.6 | 141.2±0.7 | 139.3±0.7 | 139.6±0.6 |
| TH | 140.8±0.6 | 141.3±0.7 | 140.2±0.8 | 141.3±0.7 |
| H2+TH | 139.6±0.4 | 142.8±0.6 | 141.9±0.8 | 140.2±0.7 |
| K, mmol/L* | ||||
| Control | 3.8±0.0 | 3.9±0.2 | 3.8±0.1 | 4.2±0.1 |
| H2 | 3.9±0.0 | 3.8±0.2 | 3.8±0.1 | 4.2±0.1 |
| TH | 3.9±0.0 | 3.4±0.2 | 3.4±0.0#† | 3.7±0.1#† |
| H2+TH | 4.0±0.0 | 3.4±0.1 | 3.2±0.5#† | 3.5±0.0#† |
| SaO2, % | ||||
| Control | 97.5±0.3 | 99.0±0.6 | 99.9±0.0 | 100±0.0 |
| H2 | 97.4±0.4 | 99.6±0.1 | 100±0.0 | 100±0.0 |
| TH | 97.2±0.3 | 99.9±0.0 | 100±0.0 | 100±0.0 |
| H2+TH | 97.6±0.4 | 99.9±0.0 | 100±0.0 | 100±0.0 |
| Glucose, mg/dL** | ||||
| Control | 196±8 | 238±22 | 293±15 | 269±20 |
| H2 | 185±11 | 264±25 | 328±22 | 319±20 |
| TH | 193±16 | 258±24 | 339±21 | 338 ±38 |
| H2+TH | 178±10 | 205±18 | 304±10 | 337±17 |
| Hematocrit, % | ||||
| Control | 48.6±0.9 | 52.5±1.3 | 51.3±1.1 | 49.5±1.2 |
| H2 | 48.1±1.1 | 54.0±0.9 | 50.3±0.8 | 49.0±0.8 |
| TH | 49.8±0.9 | 53.3±1.1 | 51.3±0.7 | 51.3±0.9 |
| H2+TH | 49.2±0.8 | 54.2±0.6 | 52.0±0.6 | 50.0±0.6 |
| Lactate, mg/dL | ||||
| Control | 1.4±0.1 | 8.9±0.7 | 2.3±0.3 | 2.0±0.2 |
| H2 | 1.3±0.1 | 8.5±0.7 | 2.4±0.2 | 1.9±0.1 |
| TH | 1.7±0.2 | 8.9±0.7 | 3.1±0.6 | 2.8±0.9 |
| H2+TH | 1.4±0.1 | 8.4±0.4 | 3.0±0.2 | 1.9±0.2 |
| Base excess, mmol/L | ||||
| Control | 1.1±0.6 | −12.7±1.2 | −2.8±0.9 | −3.5±0.9 |
| H2 | 1.3±0.7 | −11.1±0.8 | −3.0±0.7 | −3.1±0.8 |
| TH | 1.6±0.6 | −11.7±1.0 | −3.8±1.0 | −4.1±1.4 |
| H2+TH | 1.6±0.6 | −8.4±2.0 | −3.7±0.7 | −2.3±0.7 |
Values expressed as mean±SEM. Resuscitated animal were analyzed (n=13 for each group). TH indicates therapeutic hypothermia; ROSC, return of spontaneous circulation.
P<0.05;
P<0.01, statistically significant differences for treatment by time between 4 groups by mixed-effects model for repeated-measures analyses.
P<0.05;
P<0.01 vs the control group.
P<0.05;
P<0.01 vs the H2 group.
The survival rate 24 hours after ROSC was 43% (6/13) in the control group, 92% (12/13) in the H2 group, 77% (10/13) in the TH group, and 100% (13/13) in the H2+TH group, whereas 72-hour survival rates were 31% (4/13), 69% (9/13), 69% (9/13), and 77% (10/13), respectively (Figure 2). These results indicated that inhalation of H2 gas during CPR and during the first 2 hours after ROSC significantly improved survival rate, comparable to those of hypothermia.
Figure 2.
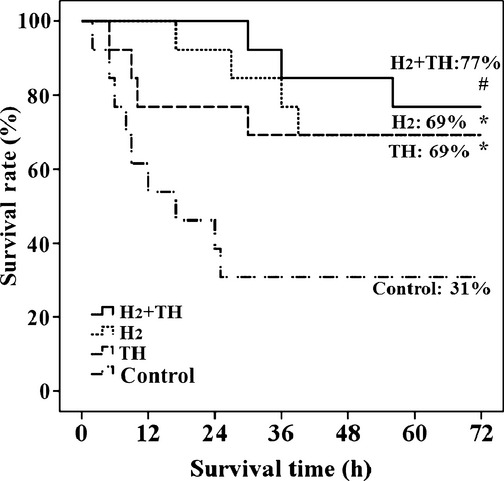
Kaplan–Meier analyses of cumulative survival at 72 hours. Statistically significant differences: #P<0.01 compared with the control group; *P<0.05 compared with the control group. TH indicates therapeutic hypothermia.
Inhalation of H2 Gas Improved NDS in Postarrest State
Interestingly, appearance was the most obvious difference between these groups of post-CA animals (Figure 3A). The typical sick-rat appearance of a hunched back and unkempt hair was often seen in post-CA control rats, whereas post-CA rats treated with H2 gas appeared healthy. All animals were evaluated for neurological function based on their NDS (100=worst NDS; 0=best NDS) 24 and 48 hours after ROSC. NDS 24 hours after ROSC was significantly lower in the H2 group (25.7±7.7%), TH group (38.0±10.7%), and H2+TH group (8.0±2.5%) compared with the control group (77.1±8.6%) (Figure 3B). The H2+TH group showed significantly better NDS 24 hours after ROSC compared with the H2 and TH groups. NDS 48 hours after ROSC was significantly better in the H2 group (41.9±11.7%), TH group (36.0±12.4%), and H2+TH group (18.5±10.0%) than in the control group (82.6±9.2%), with the H2+TH group showing a significantly better NDS 48 hours after ROSC than the H2 group (Figure 3C). These results indicated that functional outcome was improved by inhalation of H2 gas during CPR to an extent comparable to TH in post-CA rats. Inhalation of H2 gas plus TH had additive effect on NDS 24 hours after ROSC, but not 48 hours after ROSC, in the rat model of CA with ventricular fibrillation.
Figure 3.
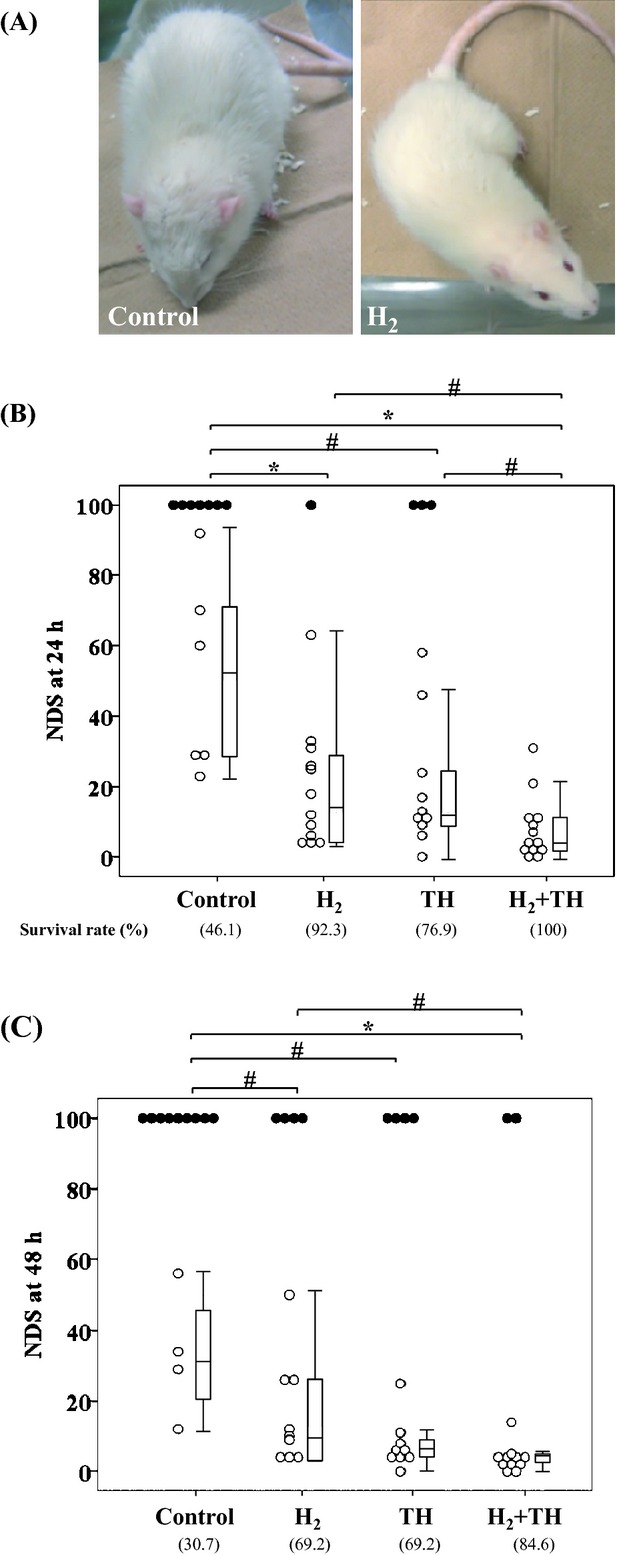
A, Representative photographs of rat appearance 24 hours after ROSC in the control group (left) and in the H2 group (right). Survival rate and neurological deficit scores (NDSs) 24 hours (B) and 48 hours (C) after ROSC. Dead rats (indicated by score=100) are indicated by closed circles. Box plots indicate NDS of survivors 24 hours and 48 hours after ROSC. TH indicates therapeutic hypothermia. Statistically significant differences: #P<0.05 between groups; *P<0.001 between groups.
Inhalation of H2 Gas Significantly Suppressed Elevations of IL-6 After Cardiac Arrest and Cardiopulmonary Resuscitation
Serum IL-6 levels 2 hours after ROSC markedly increased in post-CA rats of the controlled normothermia group (2239.9±440.8 pg/mL) compared with sham-operated rats (27.4±13.3 pg/mL), but were almost equal in post-CA rats of the TH (2431.2±634.7 pg/mL) and controlled normothermia groups, indicating that TH has little effect on the systemic inflammatory response at this point.
Serum IL-6 levels 2 hours after ROSC were not significantly increased in post-CA rats of the H2 group (848.9±257.0 pg/mL) or H2+TH group (933.3±339.0 pg/mL) compared with sham-operated rats, but in the H2+TH group, serum IL-6 levels were suppressed to the same degree as that of post-CA rats receiving only H2 gas. These results indicated that the elevation of IL-6 2 hours after ROSC was markedly suppressed by H2 gas inhalation (Figure 4).
Figure 4.
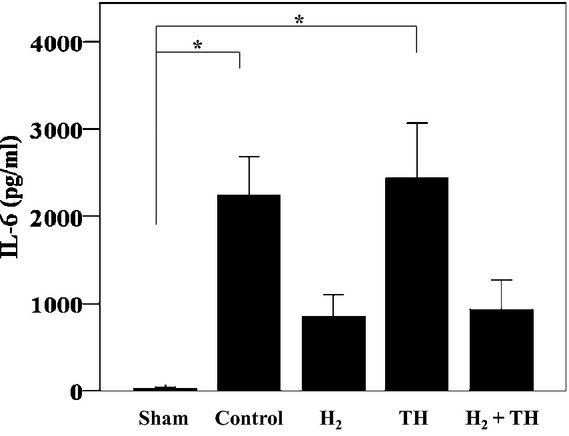
Serum IL-6 concentrations 2 hours after ROSC in the experimental and sham-operated groups. Bars represent the mean and standard error. *P<0.01 compared with the sham-operated group. ROSC indicates return of spontaneous circulation; TH, therapeutic hypothermia.
Inhalation of H2 Gas Kept LVEDP Low During the First 2 Hours After ROSC
We examined the impact of H2 gas inhalation on left ventricular functional recovery during the post-CA reperfusion period in comparison with TH. Hemodynamic parameters prior to induction of CA did not differ among the control, H2, TH, and H2+TH groups. Mean blood pressure was also not different among the 4 groups during the first 2 hours after ROSC; however, heart rate was significantly lower in the TH group compared with the control and H2 groups.
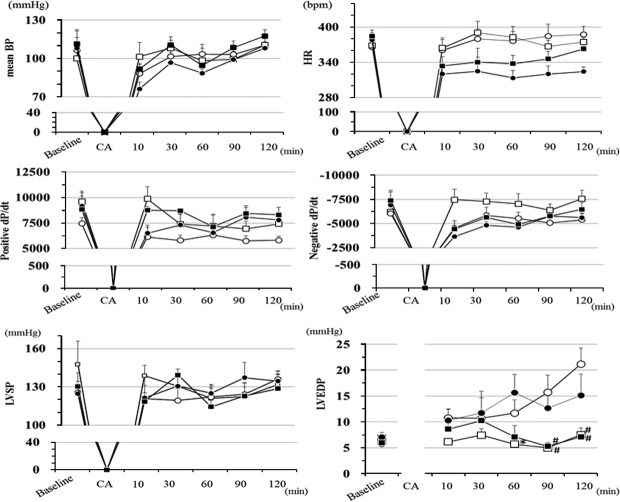
Recovery of dP/dt max, an indicator of left ventricular systolic function, after 10 minutes of ROSC was significantly higher in the H2 and H2+TH groups than in the control and TH groups. Recovery of negative dP/dt max, an indicator of left ventricular diastolic function, after 10 minutes of ROSC was significantly superior in the H2 group compared with the other groups. This superiority conferred by H2 gas inhalation tended to continue during the first 2 hours after ROSC, and left ventricular systolic pressure was recovered after CA and ROSC to pre-CA levels. There was no difference in terms of left ventricular systolic pressure among the 4 groups during the first 2 hours after ROSC. By contrast, there was a striking difference with respect to left ventricular end-diastolic pressure (LVEDP), which gradually increased to ≥20 mm Hg 2 hours after ROSC in the control group. Remarkably, H2 gas inhalation kept LVEDP at pre-CA levels during the first 2 hours after ROSC (Figure 5), and this protective effect was observed both under controlled normothermia and under TH conditions.
Figure 5.
Changes in mean blood pressure (MBP), heart rate (HR), and LV peak positive, negative dP/dt and LV systolic pressure (LVSP), LV diastolic pressure (LVEDP), n=5 to 6; #P<0.05 compared with the control group; *P<0.05 compared with the TH group.
Inhaled Hydrogen Gas Attenuated Cardiomyocyte Degeneration and Necrosis, Inflammatory Cell Infiltration, Reactive Fibrosis, and Oxidative Stress in the Postcardiac Arrest Heart
A favorable effect of inhaled H2 gas during CPR and during the first 2 hours after ROSC on functional recovery of the heart in rats after CA with VF prompted us to examine the pathohistological changes 24 hours after ROSC between control and H2 gas–treated rats. Consistent with the continuous elevation of LVEDP in post-CA rats of the control group, water content of the lung, an indicator of lung edema, tended to be higher in controls than in sham-operated rats, although lung water content was similar between post-CA H2 and sham rats (Figure 6).
Figure 6.
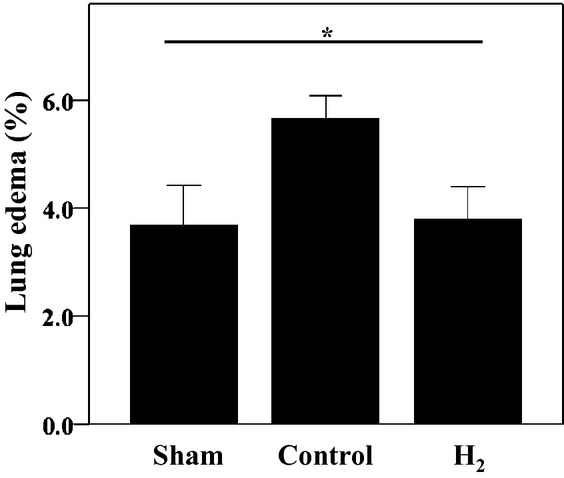
Effects of hydrogen on lung edema. Lung edema 24 hours after ROSC (n=3 to 6); *P<0.05 for analysis of variance between groups. Bars represent the standard error. ROSC indicates return of spontaneous circulation.
Azan–Mallory-stained gross sections of whole heart also revealed that perivascular and interstitial fibrosis on the endocardial side of the myocardium emerged in the post-CA control rats 24 hours after ROSC but that this reactive fibrosis was less severe in the post-CA rats administered H2 gas (Figure 7).
Figure 7.
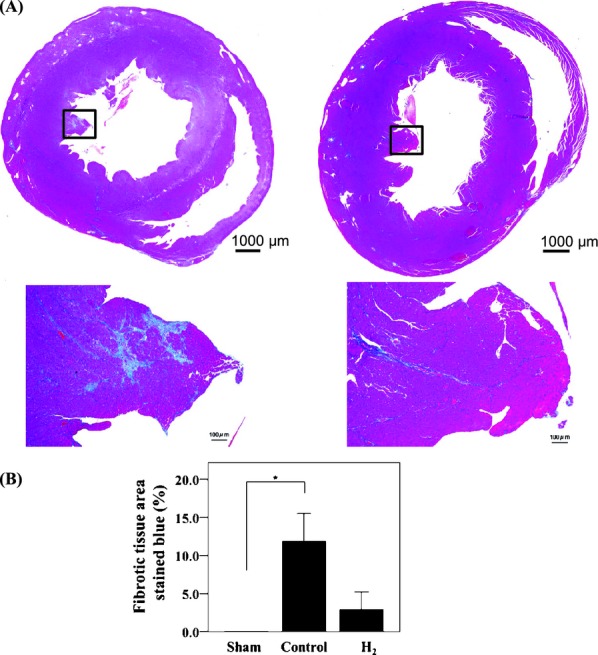
A, Representative photographs of Azan–Mallory staining of heart sections obtained 24 hours after ROSC in the absence (right) or presence (left) of H2 inhalation. B, Fibrotic tissue area stained blue (%) in sham and rats 24 hours after ROSC with or without H2 inhalation. Bars represent the standard error (n=4 to 6); *P<0.05 between groups. ROSC indicates return of spontaneous circulation.
Histological analysis with hematoxylin/eosin staining exhibited contraction band necrosis, coagulation necrosis with cytoplasmic eosinophilia, loss of nuclei, and vacuolar degeneration surrounded by inflammatory cell infiltration in the myocardium of the post-CA rats of the control group. These pathohistological changes were less severe in rats administered H2 gas (Figure 8).
Figure 8.
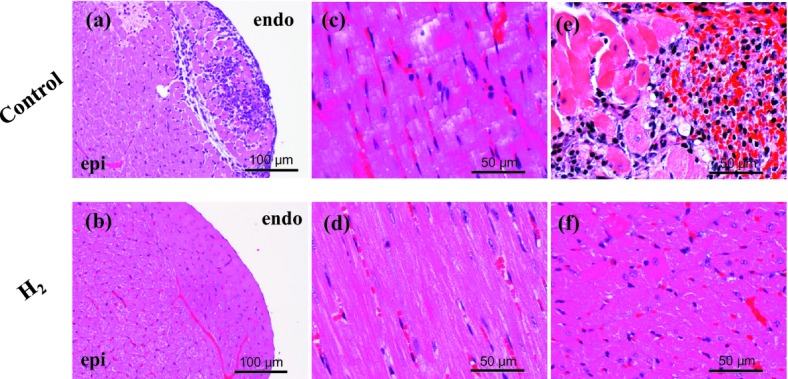
Hematoxylin and eosin staining of transverse sections of rat heart in the presence or absence of H2 inhalation. Shown is a microscopic view of inflammatory cell infiltration (a), contraction band necrosis (c), cytoplasmic eosinophilia (e), loss of nuclei (e), and vacuolar degeneration (e) in the left ventricle. These observations were reduced by inhalation of H2 (b, d, f).
Immunohistochemistry for 8-OH-dG (which is an index of oxidative DNA damage) and 4-HNE (which is the end product of lipid peroxidation) was carried out to investigate oxidative stress in myocardium obtained from the post-CA rats 24 hours after ROSC. The 8-OHdG-positive cells and 4-HNE-positive cardiomyocytes were distributed throughout the myocardium, particularly on the endocardial side of the myocardium. Notably, there were fewer 8-OHdG- positive cells and 4-HNE-positive cardiomyocytes obtained from the post-CA rats administered H2 gas (Figure 9). These results indicated that inhalation of H2 gas ameliorated oxidative myocardial injury during CPA and after ROSC.
Figure 9.
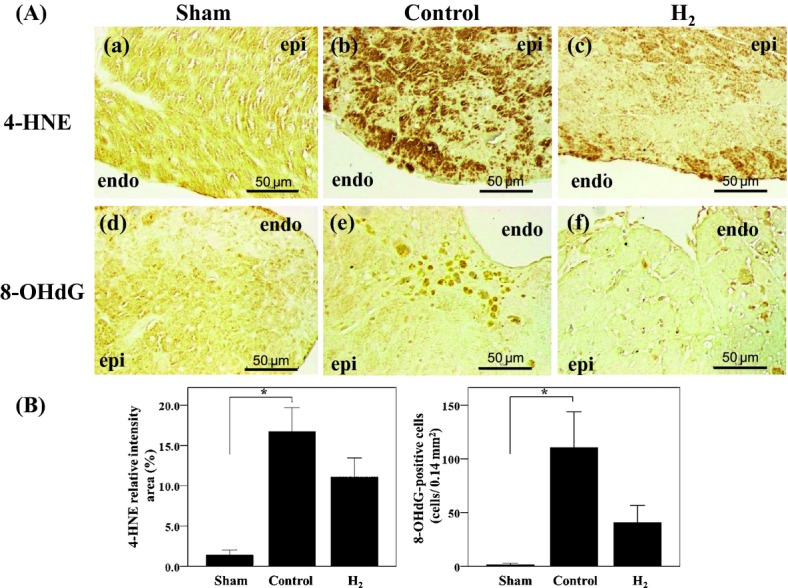
A, Immunohistochemical staining with antibodies against 4-HNE and 8-OHdG in transverse sections of sham and rats 24 hours after ROSC with or without H2 inhalation. H2 decreased levels of 4-HNE (b, c) and 8-OHdG (e, f). B, 4-HNE relative intensity area (%) and 8-OHdG-positive cells (cells/0.14) in sham and rats 24 hours after ROSC with or without H2 inhalation. Bars represent the standard error (n=4 to 6); *P<0.05 between groups.
Discussion
Molecular hydrogen (H2) is a novel antioxidant with the following unique properties: (1) H2 is permeable to cell membranes and can target organelles, including mitochondria and nuclei; (2) H2 specifically quenches detrimental ROS such as •OH and peroxynitrite (ONOO−) while maintaining the metabolic oxidation–reduction reaction and other less potent ROS, such as O2−•, H2O2, and nitric oxide (NO•)4,5; and (3) inhaled H2 gas is rapidly transported and thus can reach “at-risk” ischemic organs including the brain in a timely fashion.5
We hypothesized that H2 therapy may improve outcomes of post-CA syndrome characterized by systemic ischemia–reperfusion injury and “sepsis-like” systemic inflammation because H2 treatment by oral, intravenous administration, or inhalation has demonstrated extended effectiveness in various situations, such as in brain ischemia–reperfusion injury,6 myocardial ischemia–reperfusion injury,7 sepsis,28 diabetes,9,29 intestinal grafts,30 hemodialysis,11 liver injury,31 and spinal cord injury32 and in animal models of Parkinson's disease33 and Alzheimer's disease.34 The present study demonstrated for the first time that inhalation of 2% H2 gas starting at the beginning of CPR and given for 2 hours after ROSC significantly improves the functional status of the brain (based on NDS) and heart and suppresses the systemic inflammatory response, thereby improving survival rate in a rat model of CA with VF. The salutary impact of H2 gas could be at least partially attributed to its radical-scavenging effect in the heart, because both 8-OHdG- and 4-HNE-positive cardiomyocytes obtained from the post-CA rats 24 hours after ROSC were markedly suppressed by H2 gas inhalation. The improved appearance in the H2 group relative to control animals could be at least in part a consequence of better cardiovascular performance, because lung edema tended to been diminished in the H2 group compared with the controls. Because the neurological assessment was based only on the NDS in this study, we do not have compelling evidence that the benefits were mediated via attenuation of brain injury in the present study.
We found that H2 inhalation had protective and, in some aspects, superior effects, comparable to those of hypothermia. The results are surprising, because TH is believed to confer protection against reperfusion injury by multiple mechanisms,23 including the suppression of free radicals, enzymes, and excitatory and inflammatory reactions, in addition to the direct physical protection of membranes, whereas the cornerstone of H2 therapy is selective ROS attenuation, which is only 1 facet of TH therapy. All groups were ventilated with 98% O2, and increased reperfusion damage due to hyperoxia could have improved the chance of detecting the H2 protective effect. If H2 protects only from the harmful effects of hyperoxia, then avoiding hyperoxia/targeting normoxia might have the same benefit. Slow rewarming is also considered important in avoiding harmful systemic responses, including vasodilation, hypotension, and rebound cerebral edema. The optimal rate of warming is not known, but the consensus is currently about 0.25°C to 0.5°C of warming per hour.35 Rewarming speed after hypothermia in a rodent model of CA was variable among different TH protocols in previous research.19,24,36 Here, we chose 60 minutes of rewarming based on the high metabolic rate of rats compared with humans. However, a rapid rewarming speed after hypothermia might reduce the protective effects of cooling. Consistent with previous observations,37 blood lactate increased while the base excess decreased in post-CA rats, peaking 10 minutes after ROSC and returning to near baseline levels 60 minutes after ROSC. Although the prognostic value of these measures38 after CA have been reported in clinical studies, we could not detect any difference in the time course of blood lactate levels and base excess after ROSC among the control, H2, TH, and H2+TH groups.
Finally, we observed that TH did not affect IL-6 levels 2 hours after ROSC, whereas inhaled H2 gas did, although we did not aim to refute the anti-inflammatory effect of TH. Rather, we should emphasize the anti-inflammatory effect of H2. Previous in vitro studies and observations in patients with traumatic brain injury also demonstrated the effects of hypothermia on IL-6 levels.39–41 In addition, H2 gas inhalation significantly improved the survival rate and organ damage of septic mice with cecal ligation and puncture, and that favorable effect was accompanied by a reduction in serum and tissue proinflammatory cytokine levels.28
Conclusions
This study provided novel evidence that H2 inhalation administered at the beginning of CPR and continued for 2 hours after ROSC markedly improves NDS, myocardial outcome, and 72-hour survival rate in rats after CA to an extent comparable to TH.
Limitation of the Study
We could not conclude that whether H2 inhalation has the same beneficial outcome as TH because of the small sample size and low statistical power. Because neurological outcome was assessed on the basis of the NDS only, further studies are clearly needed to determine whether H2 directly confers neuroprotection in post-CA status. Whether H2 gas must be applied at the beginning of CPR or if a delayed application could have similar effect was also not tested in this study, and indeed, hypothermia could be applied in a delayed fashion. The use of H2 remains in its infancy, and further studies are necessary to delineate the enigmatic effect of H2 beyond that of a simple antioxidant.
Acknowledgments
The authors thank Y. Miyake (Keio University School of Medicine) and S. Kotoda (Bioresearch Center) for technical assistance. Dr Sano is a core member of the Global Center of Excellence (GCOE) for Human Metabolomics Systems Biology at MEXT.
Sources of Funding
This work was supported by a Grant-in-Aid for Scientific Research (KAKENHI; to S.H.), the Marumo Research Foundation of the Japanese Society of Acute Medicine (to K.H.), the Research Foundation of the General Insurance Association of Japan (to K.H.), and Graduate School Doctoral Student Aid Program, Keio University (to K.H.).
Disclosures
None.
References
- 1.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, Ford E, Furie K, Go A, Greenlund K, Haase N, Hailpern S, Ho M, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott M, Meigs J, Mozaffarian D, Nichol G, O'Donnell C, Roger V, Rosamond W, Sacco R, Sorlie P, Stafford R, Steinberger J, Thom T, Wasserthiel-Smoller S, Wong N, Wylie-Rosett J, Hong Y. Heart disease and stroke statistics – 2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21-e181. [DOI] [PubMed] [Google Scholar]
- 2.Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Bottiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT, Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452-2483. [DOI] [PubMed] [Google Scholar]
- 3.Merchant RM, Soar J, Skrifvars MB, Silfvast T, Edelson DP, Ahmad F, Huang KN, Khan M, Vanden Hoek TL, Becker LB, Abella BS. Therapeutic hypothermia utilization among physicians after resuscitation from cardiac arrest. Crit Care Med. 2006;34:1935-1940. [DOI] [PubMed] [Google Scholar]
- 4.Ohta S. Recent progress toward hydrogen medicine: potential of molecular hydrogen for preventive and therapeutic applications. Curr Pharm Des. 2011;17:2241-2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ohta S. Molecular hydrogen is a novel antioxidant to efficiently reduce oxidative stress with potential for the improvement of mitochondrial diseases. Biochim Biophys Acta. 2012;1820:586-594. [DOI] [PubMed] [Google Scholar]
- 6.Ohsawa I, Ishikawa M, Takahashi K, Watanabe M, Nishimaki K, Yamagata K, Katsura K, Katayama Y, Asoh S, Ohta S. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med. 2007;13:688-694. [DOI] [PubMed] [Google Scholar]
- 7.Hayashida K, Sano M, Ohsawa I, Shinmura K, Tamaki K, Kimura K, Endo J, Katayama T, Kawamura A, Kohsaka S, Makino S, Ohta S, Ogawa S, Fukuda K. Inhalation of hydrogen gas reduces infarct size in the rat model of myocardial ischemia-reperfusion injury. Biochem Biophys Res Commun. 2008;373:30-35. [DOI] [PubMed] [Google Scholar]
- 8.Xie K, Yu Y, Zhang Z, Liu W, Pei Y, Xiong L, Hou L, Wang G. Hydrogen gas improves survival rate and organ damage in zymosan-induced generalized inflammation model. Shock. 2010;34:495-501. [DOI] [PubMed] [Google Scholar]
- 9.Kajiyama S, Hasegawa G, Asano M, Hosoda H, Fukui M, Nakamura N, Kitawaki J, Imai S, Nakano K, Ohta M, Adachi T, Obayashi H, Yoshikawa T. Supplementation of hydrogen-rich water improves lipid and glucose metabolism in patients with type 2 diabetes or impaired glucose tolerance. Nutr Res. 2008;28:137-143. [DOI] [PubMed] [Google Scholar]
- 10.Nakao A, Toyoda Y, Sharma P, Evans M, Guthrie N. Effectiveness of hydrogen rich water on antioxidant status of subjects with potential metabolic syndrome – an open label pilot study. J Clin Biochem Nutr. 2010;46:140-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama M, Nakano H, Hamada H, Itami N, Nakazawa R, Ito S. A novel bioactive haemodialysis system using dissolved dihydrogen (H2) produced by water electrolysis: a clinical trial. Nephrol Dial Transplant. 2010;25:3026-3033. [DOI] [PubMed] [Google Scholar]
- 12.Shimouchi A, Nose K, Shirai M, Kondo T. Estimation of molecular hydrogen consumption in the human whole body after the ingestion of hydrogen-rich water. Adv Exp Med Biol. 2012;737:245-250. [DOI] [PubMed] [Google Scholar]
- 13.Ono H, Nishijima Y, Adachi N, Sakamoto M, Kudo Y, Nakazawa J, Kaneko K. Hydrogen(H2) treatment for acute erythymatous skin diseases. A report of 4 patients with safety data and a non-controlled feasibility study with H2 concentration measurement on two volunteers. Med Gas Res. 2012;2:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aoki K, Nakao A, Adachi T, Matsui Y, Miyakawa S. Pilot study: effects of drinking hydrogen-rich water on muscle fatigue caused by acute exercise in elite athletes. Med Gas Res. 2012;2:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ito M, Ibi T, Sahashi K, Ichihara M, Ohno K. Open-label trial and randomized, double-blind, placebo-controlled, crossover trial of hydrogen-enriched water for mitochondrial and inflammatory myopathies. Med Gas Res. 2011;1:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ono H, Nishijima Y, Adachi N, Tachibana S, Chitoku S, Mukaihara S, Sakamoto M, Kudo Y, Nakazawa J, Kaneko K, Nawashiro H. Improved brain MRI indices in the acute brain stem infarct sites treated with hydroxyl radical scavengers, Edaravone and hydrogen, as compared to Edaravone alone. A non-controlled study. Med Gas Res. 2011;1:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kang KM, Kang YN, Choi IB, Gu Y, Kawamura T, Toyoda Y, Nakao A. Effects of drinking hydrogen-rich water on the quality of life of patients treated with radiotherapy for liver tumors. Med Gas Res. 2011;1:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colbourne F, Corbett D. Delayed and prolonged post-ischemic hypothermia is neuroprotective in the gerbil. Brain Res. 1994;654:265-272. [DOI] [PubMed] [Google Scholar]
- 19.Ye S, Weng Y, Sun S, Chen W, Wu X, Li Z, Weil MH, Tang W. Comparison of the durations of mild therapeutic hypothermia on outcome after cardiopulmonary resuscitation in the rat. Circulation. 2012;125:123-129. [DOI] [PubMed] [Google Scholar]
- 20.Schneider A, Teschendorf P, Vogel P, Russ N, Knapp J, Bottiger BW, Popp E. Facilitation of hypothermia by quinpirole and 8-OH-DPAT in a rat model of cardiac arrest. Resuscitation. 2012;83:232-237. [DOI] [PubMed] [Google Scholar]
- 21.Hickey RW, Ferimer H, Alexander HL, Garman RH, Callaway CW, Hicks S, Safar P, Graham SH, Kochanek PM. Delayed, spontaneous hypothermia reduces neuronal damage after asphyxial cardiac arrest in rats. Crit Care Med. 2000;28:3511-3516. [DOI] [PubMed] [Google Scholar]
- 22.Callaway CW, Rittenberger JC, Logue ES, McMichael MJ. Hypothermia after cardiac arrest does not alter serum inflammatory markers. Crit Care Med. 2008;36:2607-2612. [DOI] [PubMed] [Google Scholar]
- 23.Polderman KH. Mechanisms of action, physiological effects, and complications of hypothermia. Crit Care Med. 2009;37:S186-S202. [DOI] [PubMed] [Google Scholar]
- 24.Abella BS, Zhao D, Alvarado J, Hamann K, Vanden Hoek TL, Becker LB. Intra-arrest cooling improves outcomes in a murine cardiac arrest model. Circulation. 2004;109:2786-2791. [DOI] [PubMed] [Google Scholar]
- 25.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL. Part 9: Post-cardiac arrest care: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S768-S786. [DOI] [PubMed] [Google Scholar]
- 26.Lin JY, Liao XX, Li H, Wei HY, Liu R, Hu CL, Huang GQ, Dai G, Li X. Model of cardiac arrest in rats by transcutaneous electrical epicardium stimulation. Resuscitation. 2010;81:1197-1204. [DOI] [PubMed] [Google Scholar]
- 27.Neumar RW, Bircher NG, Sim KM, Xiao F, Zadach KS, Radovsky A, Katz L, Ebmeyer E, Safar P. Epinephrine and sodium bicarbonate during CPR following asphyxial cardiac arrest in rats. Resuscitation. 1995;29:249-263. [DOI] [PubMed] [Google Scholar]
- 28.Xie K, Yu Y, Pei Y, Hou L, Chen S, Xiong L, Wang G. Protective effects of hydrogen gas on murine polymicrobial sepsis via reducing oxidative stress and HMGB1 release. Shock. 2010;34:90-97. [DOI] [PubMed] [Google Scholar]
- 29.Kamimura N, Nishimaki K, Ohsawa I, Ohta S. Molecular hydrogen improves obesity and diabetes by inducing hepatic FGF21 and stimulating energy metabolism in db/db mice. Obesity (Silver Spring). 2011;19:1396-1403. [DOI] [PubMed] [Google Scholar]
- 30.Buchholz BM, Kaczorowski DJ, Sugimoto R, Yang R, Wang Y, Billiar TR, McCurry KR, Bauer AJ, Nakao A. Hydrogen inhalation ameliorates oxidative stress in transplantation induced intestinal graft injury. Am J Transplant. 2008;8:2015-2024. [DOI] [PubMed] [Google Scholar]
- 31.Liu Q, Shen WF, Sun HY, Fan DF, Nakao A, Cai JM, Yan G, Zhou WP, Shen RX, Yang JM, Sun XJ. Hydrogen-rich saline protects against liver injury in rats with obstructive jaundice. Liver Int. 2010;30:958-968. [DOI] [PubMed] [Google Scholar]
- 32.Chen C, Chen Q, Mao Y, Xu S, Xia C, Shi X, Zhang JH, Yuan H, Sun X. Hydrogen-rich saline protects against spinal cord injury in rats. Neurochem Res. 2010;35:1111-1118. [DOI] [PubMed] [Google Scholar]
- 33.Fujita K, Seike T, Yutsudo N, Ohno M, Yamada H, Yamaguchi H, Sakumi K, Yamakawa Y, Kido MA, Takaki A, Katafuchi T, Tanaka Y, Nakabeppu Y, Noda M. Hydrogen in drinking water reduces dopaminergic neuronal loss in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson's disease. PLoS One. 2009;4:e7247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li J, Wang C, Zhang JH, Cai JM, Cao YP, Sun XJ. Hydrogen-rich saline improves memory function in a rat model of amyloid-beta-induced Alzheimer's disease by reduction of oxidative stress. Brain Res. 2010;1328:152-161. [DOI] [PubMed] [Google Scholar]
- 35.Che D, Li L, Kopil CM, Liu Z, Guo W, Neumar RW. Impact of therapeutic hypothermia onset and duration on survival, neurologic function, and neurodegeneration after cardiac arrest. Crit Care Med. 2011;39:1423-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Walters JH, Morley PT, Nolan JP. The role of hypothermia in post-cardiac arrest patients with return of spontaneous circulation: a systematic review. Resuscitation. 2011;82:508-516. [DOI] [PubMed] [Google Scholar]
- 37.von Planta I, Weil MH, von Planta M, Bisera J, Bruno S, Gazmuri RJ, Rackow EC. Cardiopulmonary resuscitation in the rat. J Appl Physiol. 1988;65:2641-2647. [DOI] [PubMed] [Google Scholar]
- 38.Carden DL, Martin GB, Nowak RM, Foreback CC, Tomlanovich MC. Lactic acidosis during closed-chest CPR in dogs. Ann Emerg Med. 1987;16:1317-1320. [DOI] [PubMed] [Google Scholar]
- 39.Aibiki M, Maekawa S, Ogura S, Kinoshita Y, Kawai N, Yokono S. Effect of moderate hypothermia on systemic and internal jugular plasma IL-6 levels after traumatic brain injury in humans. J Neurotrauma. 1999;16:225-232. [DOI] [PubMed] [Google Scholar]
- 40.Kimura A, Sakurada S, Ohkuni H, Todome Y, Kurata K. Moderate hypothermia delays proinflammatory cytokine production of human peripheral blood mononuclear cells. Crit Care Med. 2002;30:1499-1502. [DOI] [PubMed] [Google Scholar]
- 41.Suehiro E, Fujisawa H, Akimura T, Ishihara H, Kajiwara K, Kato S, Fujii M, Yamashita S, Maekawa T, Suzuki M. Increased matrix metalloproteinase-9 in blood in association with activation of interleukin-6 after traumatic brain injury: influence of hypothermic therapy. J Neurotrauma. 2004;21:1706-1711. [DOI] [PubMed] [Google Scholar]