Abstract
Objective
Mobile technology has the potential to radically improve addiction treatment and continuing care by offering emotional and instrumental support anywhere and just in time. This is particularly important in addiction because timing is critical to preventing relapse. Although most experts consider alcoholism to be a chronic disease, providers do not typically offer ongoing support for relapse prevention after patients complete treatment, even though a central characteristic of alcoholism and other addictive behaviors is their chronically relapsing nature. A-CHESS is a smartphone-based system for preventing relapse to heavy drinking among people leaving active alcohol dependence treatment. A-CHESS is designed to improve competence, social relatedness, and motivation, the three tenets of Self-Determination Theory. This paper reports on the relative impact and use of A-CHESS four months after patients entered the study and discusses implications of the results on treating addiction and chronic diseases generally.
Methods
A total of 349 individuals with alcohol dependence leaving residential treatment were randomly assigned to either receive A-CHESS+Treatment as Usual or Treatment as Usual (standard aftercare). Patients came from two treatment agencies, one in the Midwest and one in the Northeast. Patients assigned to A-CHESS received a smartphone for 8 months and were followed for 12. The authors analyzed use patterns during the first 4 months of use by those receiving A-CHESS.
Results
Participants used A-CHESS heavily and sustained their use over time. Ninety-four percent of A-CHESS participants used the application during the first week after residential treatment. At week 16, almost 80% continued to access A-CHESS. Participants with alcohol and drug-dependence showed higher levels of system use than those with alcohol dependence only. Participants with a mental health diagnosis had slightly lower levels of use at the end of the intervention period (week 16), although more than 70% still accessed the system.
Conclusions
These findings illustrate that patients with alcohol dependence, alcohol and drug dependence, and mental health issues will use smartphone applications such as A-CHESS for ongoing support, resources and information, thus extending patient care if given the opportunity. Further analysis is needed to determine if sustained A-CHESS use improves outcomes.
Keywords: alcohol dependence, eHealth, smartphones, system use analysis, Self Determination Theory, cognitive-behavioral relapse prevention
In 2005, more than 17 million people were classified as having an alcohol use disorder, although fewer than 4 million people received some treatment (Substance Abuse and Mental Health Services Administration [SAMHSA], 2009; Grant & Dawson, 2006).
Despite numerous advances in the treatment of alcoholism, relapse to heavy or uncontrolled use remains common, by some accounts as high as 80% (Bradizza, Stasiewicz, & Paas, 2006; Brownell, Marlatt, Lichtenstein, & Wilson, 1986; Dennis, Scott, & Funk, 2003; Donovan, 1996; Lowman, Allen, & Stout, 1996; McKay & Weiss, 2001; McLellan, 2002; Witkiewitz & Marlatt, 2004; Mueller, Petitjean, Boening, & Wiesbeck, 2007). Abuse of alcohol and other drugs relates to serious public health and safety problems (McLellan, Lewis, O’Brien, &Kleber, 2000); exacts great societal costs, including higher crime (Ettner, 2006); elevates healthcare costs (Ettner, 2006); and reduces productivity (Slaymaker & Owen, 2006; Hoffman, DeHart, & Fulkerson, 1993). The social costs of alcohol abuse and dependence in the U.S. are estimated to exceed $180 billion per year (Harwood, 2000).
Although most experts consider alcoholism to be a chronic disease, providers do not typically offer ongoing support for relapse prevention after patients complete treatment, even though a central characteristic of alcoholism and other addictive behaviors is their chronically relapsing nature. Unlike other chronic diseases, aftercare appointments and ongoing monitoring are rare in the addiction field (McLellan et al., 2000; White, Boyle, & Loveland, 2002). This is true even though most research indicates that prolonged participation in continuing care for alcohol and drug abusers is associated with better outcomes (McLellan, McKay, Forman, Cacciola, & Kemp, 2005; Simpson, 2004; McKay, 2005). This lack of continuing care for relapse prevention arises in part from the current alcohol treatment infrastructure, which is financially overburdened, labor intensive, and unstable (McLellan, Carise, & Kleber, 2003).
One possible solution to the challenge of providing continuing care is the use of technology. Technology has the potential to provide personalized continuing care 24/7, at a fraction of the cost of traditional care. This paper describes a randomized clinical trial of a mobile technology system called A-CHESS (Alcohol – Comprehensive Health Enhancement Support System). A-CHESS was designed to radically improve addiction treatment and continuing care by offering emotional and instrumental support anywhere, at any time (Gustafson et al., 2011). This paper describes how participants assigned to A-CHESS in a randomized trial used the system in the first 4 months after leaving residential treatment.
Theoretical Foundation
A-CHESS is based on Self-Determination Theory and cognitive-behavioral relapse prevention. Self-Determination Theory posits that satisfying three fundamental needs contributes to adaptive functioning: perceived competence, a feeling of relatedness (feeling connected to others), and autonomous motivation (feeling internally motivated and not coerced in one’s actions) (Ryan & Deci, 2006). Ryan and Deci (2000) argue that quality of life increases when the three basic psychological needs for competence, relatedness, and autonomy are met.
The three psychological needs relate to determinants of relapse in Marlatt and George’s (1984) cognitive-behavioral relapse prevention model, usually referred to as Marlatt’s model. This model suggests that both immediate determinants (high-risk situations, lack of coping response, decreased self-efficacy, and abstinence violation effects) and covert antecedents (lifestyle imbalances, urges, and cravings) can lead to relapse. The model includes interventions that address each of the determinants of relapse, suggesting both specific strategies (e.g., identifying high-risk situations, managing lapses) and more global ones (e.g., balancing lifestyle, pursuing positive and rewarding activities).
Both Self-Determination Theory and Marlatt’s model build on a rich tradition of social sciences research related to behavior change (Bandura, 1977), social learning (Rhodes, Fishbein, & Reis, 1997), persuasive communication (Hovland, Janis, & Kelley, 1964), motivational interviewing (Miller & Rollnick, 1991), behavioral intent (Ajzen & Fishbein, 1977), and stages of change (Prochaska & DiClemente, 1983). A-CHESS employs these concepts in the following ways to prevent relapse: (1) Offer resources to cope with pressures to relapse, e.g., cravings, withdrawal symptoms, high-risk situations (competence); (2) provide opportunities to give and receive social support to persevere (relatedness); and (3) develop and maintain autonomous motivation to prevent relapse (autonomy).
Figure 1 shows how A-CHESS fits within both Self-Determination Theory and Marlatt’s model (Larimer, Palmer, & Marlatt, 1999; Witkiewitz & Marlatt, 2004). The bottom row of boxes lists Marlatt’s stages preceding relapse. The row above lists the stage-appropriate-change methods, again from Marlatt’s model. The arrows between those two rows show how the change methods could be applied to the stages preceding relapse. The rest of Figure 1 is built on the three elements of Self-Determination Theory — competence, relatedness, and autonomy. Every A-CHESS service listed has a corresponding change method and Self-Determination Theory construct. The relationships shown are examples of how A-CHESS addresses the interventions suggested by Marlatt’s model, but do not include all possible examples.
Figure 1.
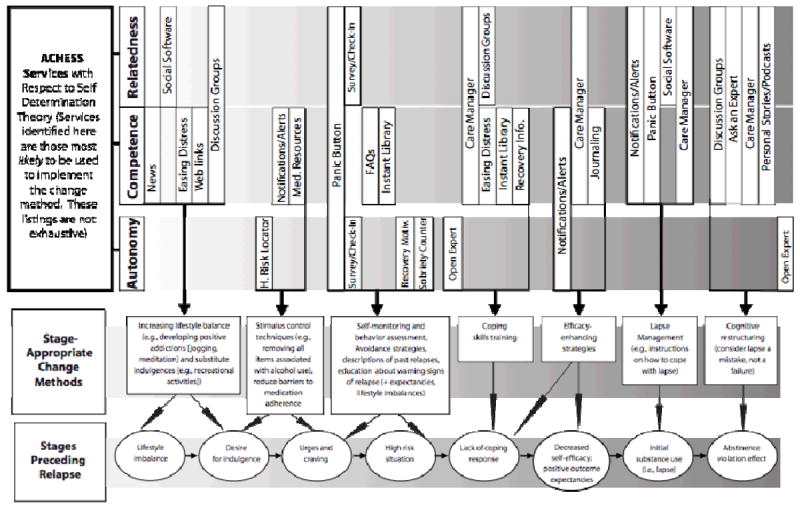
A-CHESS relationship with Self-Determination Theory and Marlatt’s Model
METHODS
Participants
The current clinical trial (Developing and Testing a Computer-based Alcohol Use Disorder Recovery System) included 349 adults who met the criteria for current DSM-IV alcohol dependence at the time they entered treatment at two residential treatment sites, one in the Midwest and one on the East Coast. Participants had to be at least 18 years of age, willing to be randomized (the control group received standard care; the experimental group received standard care plus a smartphone with A-CHESS access for 8 months), and willing to identify two people who could provide contact information about their location for the next year. Exclusionary criteria included patients with a psychiatric or medical condition that precluded participating in the study (a history of suicidality, a significant developmental or cognitive impairment that would limit the ability to understand A-CHESS material, or vision problems). Patients who appeared eligible for the study based on the treatment center’s analysis of their administrative database were approached by the onsite project coordinator approximately two weeks before leaving residential treatment. The project coordinator had a complete discussion of the study, explained the study procedures, the benefits and risks of participation, participant responsibilities, and data collected. Written informed consent was obtained after this discussion. The study was conducted in accordance with the Declaration of Helsinki in compliance with the policies of the Institutional Review Board of the University of Wisconsin – Madison, who approved and monitored the study. If participants agreed to be on study, they signed a written consent and completed a pretest. The study also included three posttest interviews at 4, 8, and 12 months. Those randomized to A-CHESS would also have their use of A-CHESS automatically collected. Participants were recruited between February 2010 through June 2011.
A total of 380 patients were approached to join study. Thirteen patients were deemed ineligible for study and 18 patients declined. The primary reasons patients declined were (1) not interested, (2) did not want to use a smartphone with GPS, and (3) did not come to their scheduled intake meeting.
Of the 349 patients who joined the study, 179 were randomized to the control group and 170 to the experimental group. No matching or stratification was used. All subjects gave written consented prior to randomization.
The average age of the study participants was 38.3 years (SD = 10.4), the majority of participants were male (60.6%), and 82.9% were Caucasian. About a quarter of participants (22.3%) did not complete high school. Self-report survey data indicated that 62.7% abused other drugs besides alcohol when they entered treatment, 47.1% had mental health problems (e.g., depression, bipolar), and 53.4% had a history of emotional or physical trauma that continues to affect them. Approximately a third (34.9%) were planning to live in a halfway house or shelter when they left treatment.
The Intervention
Those randomized to the experimental group received access to A-CHESS for 8 months. A-CHESS was designed for people in recovery being discharged from residential care, and has digital voice services, text messaging, Web access, GPS, voice recognition, and video capabilities. The system transfers data from the phone to a computer accessible by the patient’s counselor or care manager. It has sufficient memory to store static content and a global positioning system (GPS) that provides location-detection services.
Each study participant has a unique log-in allowing us to automatically collect A-CHESS use data in server log files for later analysis. The server tracks date and time a participant entered A-CHESS, the service selected, how long they used each service, pages viewed, and whether the participant sent or received messages. Table 1 has a brief description of some of the services in A-CHESS.
Table 1.
A-CHESS Services
| Discussion Groups | Participants can anonymously exchange emotional support and information with other A-CHESS users via online bulletin-board support groups. |
| Ask an Expert | Allows A-CHESS users to receive personal responses to their questions from experts in addiction within 48 hours. |
| Open Expert | Responses to questions sent to Ask an Expert that are of general interest are rendered anonymous and made available for all users to view. |
| Personal Stories | Professionally produced text and video accounts of recovery experiences based on interviews of patients and family members. Stories focus on ways to overcome barriers to addiction management as well as how to make different choices and cope with challenges. |
| Instant Library | Detailed summaries of articles, chapters, and manuals on addiction management. |
| Medication Resource | Information about addiction pharmacotherapies, side effects, and ways to reduce barriers to adherence (e.g., forgetting to take medications, daily techniques to remember to take medications). |
| Frequently Asked Questions | Brief answers to frequently asked questions about addiction, such as “Why do some people become addicted to drugs, while others don’t?” and “How do I deal with cravings for alcohol?” Links to additional CHESS services offering more detailed information and support are also provided. |
| Web Links | Patients access approved addiction-related web sites (and specific pages within sites). |
| Easing Distress | A computerized cognitive-behavior therapy program designed to help people cope with harmful thoughts that can stymie efforts to prevent relapse. It helps assess logical errors, attributional style, and the tendency to exaggerate distress, and offers practical exercises to improve cognitive problem-solving skills. |
| Healthy Events Newsletter | Alerts the person in recovery about healthy drug- and alcohol-free events taking place in their city. |
| High-Risk Patient Locator | Global positioning system (GPS) technology tracks when participants approach an area where they traditionally obtained or consumed alcohol so they can receive “just-in-time” support to work through what might be a high-risk situation for relapse. To activate, individuals voluntarily register places where they regularly obtained or consumed alcohol in the past and now designate as a high-risk locations for relapse. |
| Daily Thoughts | Motivational quotes (usually about sobriety) sent via text messaging each morning to A-CHESS participants. |
| Sobriety Counter | Appears on the home page of A-CHESS to remind participants of how many days they have been sober. |
| Panic Button | Provides immediate help to avoid an imminent relapse (e.g., if urges and cravings become severe and help is desired). By pressing the PANIC BUTTON an intervention (set up during training) would start, including automated reminders to the patient (personal motivations for not drinking), computer-generated alerts to key people (e.g., counselor, sponsor, counselor, family) who may reach out to the patient via phone or in person, and specific tools for dealing with urges. |
| Weekly Check-In | Brief survey (Brief Alcohol Monitoring Index) to obtain patient data on negative affect, lifestyle balance, and recent substance use. Check-in information is used by A-CHESS for triage and feedback. Patients’ care managers are automatically notified if a participant score exceeds a predetermined threshold. The care manager can view a summary report of Check-in data if they wish. |
While still in the residential treatment facility, study participants randomized to A-CHESS learned and practiced using A-CHESS services under counselor guidance. Before leaving residential treatment, participants were required to demonstrate a minimal understanding of the smartphone before getting it (i.e., they had the ability to set up their Profile and use the Discussion Board and texting features, and had entered a minimum of two people who would receive a text message if they pressed the panic button). Participants were given a wallet size card that included a toll-free number to call if they had any questions about the study or using the A-CHESS phone as well as the dates of their follow-up telephone surveys.
RESULTS
This paper focuses on how the A-CHESS study participants (n=170) used the intervention in the first four months after they left residential treatment. All data were collected automatically on the server to track the use of the A-CHESS application on the smartphone. Data on participant use during training were removed from the analysis. Of those randomized to A-CHESS, 93.5% accessed the system during the first week after leaving treatment. At the end of 4 months, 78.2% were still actively using the system. The A-CHESS services used by the greatest percent of participants included Discussions, My Messages, My Team, and Weekly Surveys. The least used services were Instant Library, Frequently Asked Questions, and Weblinks.
As discussed previously, A-CHESS was built on Self-Determination Theory and Marlatt’s stages-of-relapse model. Therefore we measured use of A-CHESS services around the three tenets of Self-Determination Theory (competence, relatedness, and autonomy). These tenets are not mutually exclusive. For example, Discussions fit under relatedness but, because information exchange often occurs within messages, also contributes to competence. Thus, use of Discussions is counted in both categories.
A-CHESS services related to competence include: Notifications, Panic Button, Discussions, Ask an Expert, News, Easing Distress, Instant Library, Recovery Information, Open Expert, Frequently Asked Questions, Weblinks, Tutorials, Our Stories, and Recovery Podcasts. Services associated with relatedness include: Panic Button, Weekly Survey, Daily Check-In, Discussions, Ask an Expert, Events and Meeting Planner, My Friends, My Messages, My Profile, My Team, and Team Feed. Services related to autonomy include: High-Risk Locator, Notifications, Recovery Motivation, Panic Button, Weekly Survey, Daily Check-In, Sobriety Date Counter, Our Stories, and Recovery Podcasts.
In week 1, 80% of A-CHESS participants used services related to competence, 91% used services associated with relatedness, and 84% used services related to autonomous motivation. By week 16, only 39% used services related to competence while 76% used services associated with relatedness, and 66% used services related to autonomous motivation (see Figure 3).
Figure 3.
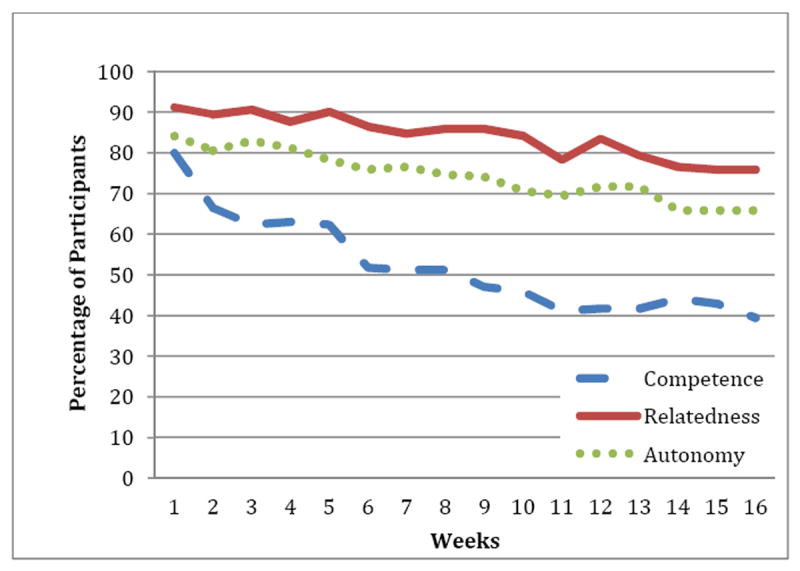
Percentage of participants viewing content by Self-Determination Theory tenets/week (color figure available online).
When use is measured by mean number of pages viewed per Self-Determination Theory tenet, a similar but different picture emerges. The mean number of relatedness pages viewed was 164.2 pages during week 1, compared to 35.97 competence pages and 19.32 autonomous motivation pages. By week 16, a mean of 52.3 relatedness pages, 14.24 competence pages, and 11.17 autonomous motivation pages were viewed (Figure 4).
Figure 4.
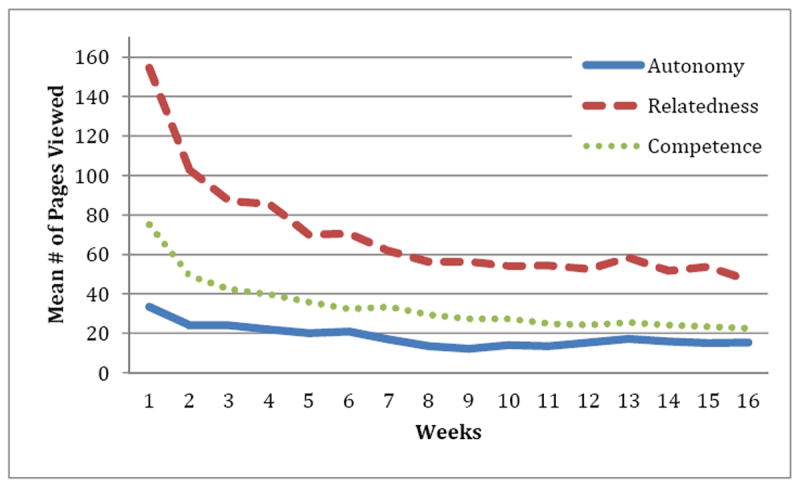
Mean number of A-CHESS pages viewed per Self-Determination Theory tenets (color figure available online).
We also looked at whether A-CHESS use was different if the participant had a self-reported mental health disorder in addition to alcohol or drug dependence. More than 90% of those who self-reported mental health issues used A-CHESS through week 4. By week 16, approximately 74% of those with self-reported mental health issues were still using A-CHESS compared to 83% of those with no self-report mental health issues.
All subjects in this study met criteria for current DSM-IV alcohol dependence at the time they entered treatment. According to the National Institute on Drug Abuse (NIDA, 2011), 23.1% of admissions to publically funded treatment centers in 2008 were for alcohol abuse only, whereas 18.3% were for alcohol and other drugs. As part of the pretest survey, study participants self-reported other drug abuse besides alcohol. The 2001 DASIS Report (Substance Abuse and Mental Health Services Administration) stated that “many believe that successful treatment of polydrug use may be more difficult” than single drug treatment. Looking at A-CHESS use by individuals with drug as well as alcohol dependence (n=105) versus those with alcohol dependence alone (n=65), we found that the percentage of overall use of A-CHESS by each group was essentially the same through week 8 (approximately 90% of participants in each group were using A-CHESS), but by week 16, 82% of those with alcohol and drug dependence used A-CHESS compared to 72% of those with alcohol dependence alone. Including only those who used A-CHESS each week, there was no difference between groups in mean number of pages viewed per week.
Additionally we looked at the mean number of pages viewed per Self-Determination Theory tenet (relatedness, competence and autonomous motivation) and found no difference between groups. However, use of two services within the relatedness tenet were significantly different. Participants with alcohol and drug dependence used the My Messages service significant less than those with alcohol dependence only [t(160)=2.139, p=.034] but had significantly more use of My Team service [t(157)=3.071, p=.003]. There was no significant difference in the use of any A-CHESS services found for individuals who self-reported other mental health issues. While we have not looked at outcomes in this paper, it is encouraging that individuals with alcohol and drug dependence as well as people with dual diagnosis (self-reported mental health issues in addition to alcohol or drug dependence) have sustained use of A-CHESS over time.
We then looked to see if there were differences in use by gender and age. When comparing number of weeks of use of A-CHESS by age we found no significant difference of A-CHESS by age group. However we did find that females had significantly higher weekly use of the A-CHESS services clustered in the competence tenet of the Self-Determination Theory than males [t(168)=-2.814, p=.005]. The mean number of weeks that females viewed services related to competence was 9.63 compared to 7.48 for males. Additionally females viewed significantly more pages (M=219.13) than males (M=128.15) within the competence tenet [t(164)=-2.803, p=.006)].
To further understand use of the smartphone applications, we compared A-CHESS use to two other smartphone applications: (1) the use by teenagers of Asthma-CHESS and (2) the use by adult patients with colon cancer of Survivor-CHESS. The mean age of the teens was 14.1 years (SD = 1.8). The colon cancer survivors’ mean age was 58 years (SD = 13.3). As might be expected, the mean number of pages viewed by teens was much greater than the pages viewed by participants with alcohol dependence or colon cancer survivors (950 pages versus 225 pages versus 179, respectively).
To compare changes in use patterns over time among different populations, we recorded the number of mean pages viewed in week 1 (the highest use period) as 100% and compared each week thereafter to week 1. For example, if mean pages viewed in week 1 was 50 pages, week 1 is 100% and the pages viewed each week after is a fraction of the maximum use (e.g., 25 pages is 50% use). Asthma-CHESS had a mean of 950 pages viewed in week one (100% or maximum use), but quickly dropped to 30% of maximum use (or 292 pages viewed) by week 3 and stayed at that level every week but one. In contrast, Alcohol-CHESS users dropped to approximately 56% of maximum use by week 3 (127 compared 225 pages viewed) and remained above the 30% level throughout week 16. Colon cancer survivors dropped to 40% of maximum use by week 3 and remained below 20% from week 10 on (see Figure 5).
Figure 5.

Percentage of pages viewed by week (color figure available online).
Using the percentage of users viewing pages per week rather than the mean number of pages viewed, approximately 93% of Alcohol-CHESS participants used the smartphone application during the first week they left residential treatment. At week 16, almost 80% continued to access Alcohol-CHESS. All of the teens (100%) used Asthma-CHESS during week 1; by week 6, approximately 75% used it; and by week 16, 65% were still viewing content. Survivors of colon cancer used the application least through the 16-week period, with a high of 65% of participants using it in week 1 and only 35% using it at week 16 (see Figure 6).
Figure 6.

Percentage of participants using application by week (color figure available online).
Both Alcohol-CHESS and Asthma-CHESS had high levels of sustained use of the system, higher than what we typically observed in our earlier clinical trials using laptops. In a previous study of 231 low-income women (mean age of 51) diagnosed with breast cancer, 84% of participants used the Breast Cancer CHESS program on laptops in the first week. By week 16, only 31% were still participating. In a second breast cancer study, the percentage of women using the system in week 1 was 74% and declined to 30% by week 16. Other CHESS studies of patients with HIV and prostate cancer using laptops show similar patterns of declined use over time.
DISCUSSION
Research2Guidance co-founder Ralf-Gordon Jahns estimates that there are currently more than 40,000 mobile health apps on the market (Cohn, 2012). Jahns expects the number of apps to double as the number of smartphone users, the sophistication of the apps, and the marketing muscle behind the apps all increase. He estimates that close to 250 million people will download health apps in 2012. Despite this growth, very little research has been done on the efficacy of smartphone apps, let alone standard ways of measuring their use. Our initial analysis of A-CHESS use is a step in this direction, and begins to provide a richer sense of how these sorts of applications can be used to treat chronic disease generally and alcohol addiction and associated issues specifically.
Our analysis focused on two distinct types of use: entry into the system and exposure to specific content. Entry is defined as how often someone chooses to access an application. In the case of A-CHESS, entry is measured the first time during a session that the person gets to the A-CHESS homepage. The number of entries was examined at various points during the study period. To understand sustained use, we looked at the number of weeks a participant entered the system over time. An online survey by Consumer Health Information Corporation (2011) found that only 26% of health apps downloaded are used more than once. As reported earlier, 93% of those given access to A-CHESS used it in the first week. By week 16, 73% were still actively accessing the system. Previous CHESS studies of women with breast cancer using laptops showed that 80% of participants entered the system in the first two weeks; this dropped to approximately 30% of participants at week 16. The sustained high use of the A-CHESS application may relate to the platform used, age of participants, familiarity with the device, or perhaps the chronic and addictive nature of alcohol and drug abuse. Understanding what sustains ongoing entry into e-health systems such as A-CHESS is critical for designing applications, for without entry into such systems, the benefits of their use are unavailable.
Participants reporting other drug dependence or mental health issues had similar patterns of sustained A-CHESS use as those with alcohol dependence only. By week 16, those with alcohol and drug dependence had higher sustained use (82%) than those with alcohol dependence only (72%). In addition, 74% of participants with mental health issues continued to use A-CHESS at week 16. This pattern of sustained entry into A-CHESS by those with alcohol and drug dependence, as well as those with dual diagnosis over time is encouraging because it indicates that a wide range of patients in recovery programs found the systems useful. This is especially significant because research indicates that prolonged participation in continuing care is associated with better outcomes (McLellan et al., 2005; Simpson, 2004; McKay, 2005).
The second measure of use we examined was exposure. Exposure can be defined as the number of pages viewed or total minutes that a participant is exposed to a particular type of content. In this study, we relied on page views as an indicator of exposure to different sorts of content. For pages containing rich content, such as lengthy videos or detailed narrative accounts, total minutes might be a more appropriate indicator of exposure. Nonetheless, a goal of this study was to map the use of A-CHESS services to the three tenets of Self-Determination Theory: competence, relatedness, and autonomy. This is important because Self-Determination Theory suggests that all three elements improve quality of life. At the most basic level, we found that participants choose to expose themselves to content aligned with relatedness and autonomy more than competence, especially in the later weeks of the study period. Gustafson et al. (2001) found that information and support must be relevant and timely, meeting patient’s needs as they arise, for system use to be effective. Certainly smartphone applications have the potential to provide timely and relevant information, just in time. It may be that the tools linked to relatedness and autonomy were seen as more relevant and timely.
Despite these differences, exposure to content geared toward competence, relatedness, and autonomy was largely sustained throughout the study period. Previous research by Han et al. (2009) demonstrated that patients with improved quality of life showed consistency and continuity in their use of an interactive healthcare system. This bodes well for the sustained use of A-CHESS participants in this study. Smaglik et al. (1998) found that simply measuring the amount of use of a particular service was not a good predictor of improved quality of life. They reported that users who exclusively used a bulletin discussion group feature benefitted little, if at all, while those who used multiple services to systematically pursue a topic over time improved the most. These insights, when combined with our findings, provide further reassurance.
As with past CHESS studies using laptops, we found that the social media services within our A-CHESS smartphone application (such as Discussions and TeamFeed) were much more heavily used than the services related to competence and autonomous motivation. It should be noted, however, that while fewer competence- and autonomy-related pages were viewed, by week 16, 66% of participants were still viewing autonomy-related pages and 39% were viewing competence-related pages. This may support Smaglik’s (1998) and Han’s (2009) findings that use of multiple services over an extended period of time is associated with better outcomes. Further, combining a page-views approach with a time-spent approach may show how balanced or imbalanced was the use of various components of A-CHESS in relation to one another.
Another common measure of use is engagement, which refers to actions by the participant--what he or she does with the content. While engagement was beyond the scope of this present analysis, combining use data with outcome data will be important in determining which features in A-CHESS have the greatest effect and whether smartphones can engage participants more than other technologies. For example, the number of messages posted or read by a participant or a participant’s ongoing use of a decision-aid or other interactive system would provide a better sense of engagement with the capabilities the system provides. Past research shows that these indicators of engagement predict improved coping and quality of life in other chronic disease settings (Han et al., 2011; Namkoong et al., 2010).
While there are certainly many other ways use can be measured and defined, measuring use by entry and exposure to A-CHESS sets the foundation for more complex use and outcome analysis in the future. It also allows for comparison across other studies, as we did with comparable data from patients with asthma and colon cancer. Future analysis of the A-CHESS use data should include machine learning in order to recognize complex patterns and develop algorithms that will predict the likelihood of a participant’s using alcohol or drugs before actually doing it. By instantly analyzing data gathered by built-in sensors (such as GPS and accelerometers) and combining it with A-CHESS use patterns, smartphone interventions have the capability of providing just-in-time interventions. This suggests the potential for much richer entry and exposure measures, which will provide insights into the use and effects of mobile e-health systems for the treatment of chronic disease.
Limitations
Several limitations should be considered. As previously explained, A-CHESS services were categorized according to the three tenets of Self-Determination Theory (competence, relatedness, and autonomy), but the categories are not mutually exclusive. While conceptually sound, this raises the potential problem of double counting or inflating use counts. Additionally, we measured exposure to content by number of pages viewed, which treats all pages as equal. For example, a 3-sentence message in Discussions and a 45-minute podcast in Recovery Podcasts are both considered one viewed page. A more complete understanding of use might consider the percentage of people using a service and the amount of time spent viewing a page as well as the number of pages viewed.
It should also be noted that A-CHESS was designed for individuals with alcohol dependence. As A-CHESS matures and develops, more content should be added for individuals dealing with alcohol and drug dependence and/or mental health issues given the high percentage of participants dealing with these issues.
Figure 2.
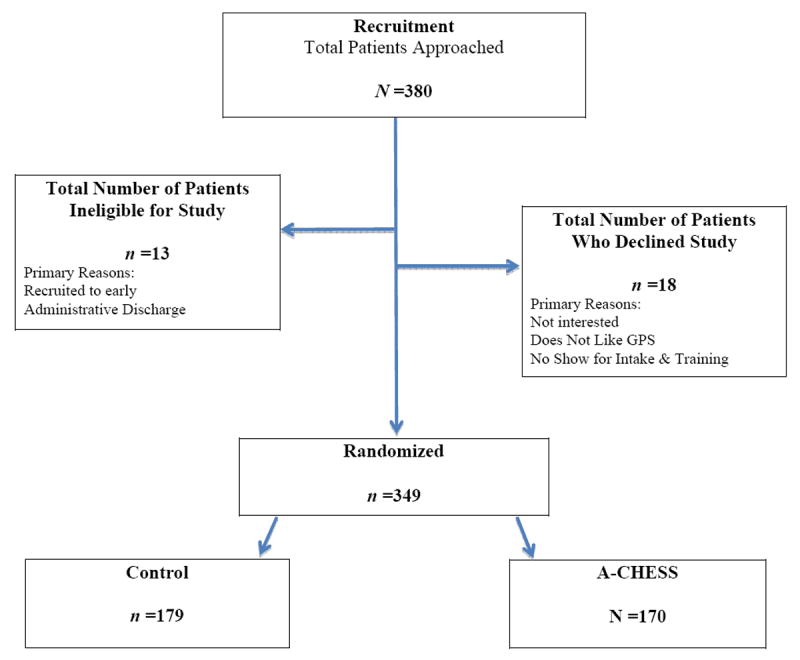
Consort diagram (color figure available online).
Acknowledgments
This research is being supported by a grant from the National Institute of Alcohol Abuse and Alcoholism (Grant number: R01 AA017192).
Footnotes
DISCLOSURES
The authors of this manuscript report no financial relationships with commercial interests.
Contributor Information
Fiona M. McTavish, University of Wisconsin-Madison.
Ming-Yuan Chih, University of Wisconsin-Madison.
Dhavan Shah, University of Wisconsin-Madison.
David H. Gustafson, University of Wisconsin-Madison.
References
- Ajzen I, Fishbein M. Attitude-behavior relations: A theoretical analysis and review of empirical research. Psychological Bulletin. 1977;84(5):888–918. doi: 10.1037/0033-2909.84.5.888. [DOI] [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavior change. Psychological Review. 1977;84(2):191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance abuse disorders: A review. Clinical Psychology Review. 2006;26(2):162–178. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Brownell KD, Marlatt GA, Lichtenstein E, Wilson GT. Understanding and preventing relapse. American Psychologist. 1986;41(7):765–782. doi: 10.1037/0003-066X.41.7.765. [DOI] [PubMed] [Google Scholar]
- Cohn M. Hopkins researchers aim to uncover which mobile health applications work. The Baltimore Sun. 2012 Mar 14; Retrieved from http://articles.baltimoresun.com/2012-03-14/health/bs-hs-mobile-health-apps-20120314_1_health-apps-mhealth-mobile-health.
- Consumer Health Information Corporation. Motivating patients to use smartphone health apps. 2011 Apr 21; Retrieved from http://www.consumer-health.com/press/2008/NewsReleaseSmartPhoneApps.php.
- Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management check-ups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26(3):339–352. doi: 10.1016/S0149-7189(03) 00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan D. Assessment issues and domains in the prediction of relapse. Addiction. 1996;91(12, Supp. 1):29–36. doi: 10.1046/j. 1360-0443.91.12s1.14.x. [DOI] [PubMed] [Google Scholar]
- Ettner SL. Does treatment ‘pay for itself’? Looking at the economic argument for addiction treatment. Behavioral Healthcare. 2006;26(5):32–34. [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research & Health. 2006;29(2):74–78. [Google Scholar]
- Gustafson DH, Hawkins R, Pingree S, McTavish F, Arora NK, Mendenhall J, Salner A, et al. Effect of computer support on younger women with breast cancer. Journal of General Internal Medicine. 2001;16(7):435–445. doi: 10.1046/j.1525-1497.2001.016007435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, Shaw BR, Isham A, Baker T, Boyle MG, Levy M. Explicating an evidence-based, theoretically informed, mobile technology-based system to improve outcomes for people in recovery for alcohol dependence. Substance Use and Misuse. 2011;46(1):96–111. doi: 10.3109/10826084.2011.521413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han JY, Hawkins RP, Shaw BR, Pingree S, McTavish F, Gustafson DH. Unraveling uses and effects of an interactive health communication system. Journal of Broadcasting & Electronic Media. 2009;53(1):112–133. doi: 10.1080/08838150802643787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han JY, Shah DV, Kim E, Namkoong K, Lee SY, Moon TJ, Gustafson DH, et al. Empathic exchanges in online cancer support groups: Distinguishing message expression and reception effects. Health Communication. 2011;26(2):185–197. doi: 10.1080/10410236.2010.544283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood H. Report prepared by the Lewin Group for the National Institute on Alcohol Abuse and Alcoholism. Updating estimates of the economic costs of alcohol abuse in the United States: Estimates, update methods, and data. Rockville, MD: National Institutes of Health; 2000. [Google Scholar]
- Hoffman NG, DeHart SS, Fulkerson J. Medical care utilization as a function of recovery status following chemical addiction treatment. Journal of Addictive Diseases. 1993;12(1):97–108. doi: 10.1300/J069v12n01_08. [DOI] [PubMed] [Google Scholar]
- Hovland CI, Janis IL, Kelley HH. Communication and persuasion: Psychological studies of opinion change. New Haven, CT: Yale University Press; 1964. [Google Scholar]
- Larimer ME, Palmer RS, Marlatt GA. Relapse prevention: An overview of Marlatt’s cognitive-behavioral model. Alcohol Research & Health. 1999;23(2):151–160. [PMC free article] [PubMed] [Google Scholar]
- Lowman C, Allen J, Stout RL The Relapse Research Group. Replication and extension of Marlatt’s taxonomy of relapse precipitants: Overview of procedures and results. Addiction. 1996;91(12, Suppl. 1):51–72. doi: 10.1046/j.1360-0443.91.12s1.16.x. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, George WH. Relapse prevention: Introduction and overview of the model. British Journal of Addiction. 1984;79(3):261–273. doi: 10.1111/j.1360-0443.1984.tb00274.x. [DOI] [PubMed] [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100(11):1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McKay JR, Weiss RV. A review of temporal effects and outcome predictors in substance abuse treatment studies with long-term follow-ups: Preliminary results and methodological issues. Evaluation Review. 2001;25(2):113–161. doi: 10.1177/0193841X0102500202. [DOI] [PubMed] [Google Scholar]
- McLellan AT. The outcomes movement in substance abuse treatment: Comments, concerns and criticisms. In: Sorenson J, Rawson R, editors. Drug abuse treatment through collaboration: Practice and research partnerships that work. Washington, DC: American Psychological Association Press; 2002. pp. 119–134. [Google Scholar]
- McLellan AT, Carise D, Kleber HD. Can the national addiction treatment infrastructure support the public’s demand for quality care? Journal of Substance Abuse Treatment. 2003;25(2):117–121. doi: 10.1016/S0740-5472(03)00156-9. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic mental illness: Implications for treatment, insurance, and outcomes evaluation. JAMA: The Journal of American Medical Association. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: From retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100(4):447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York, NY: Guilford Press; 1991. [Google Scholar]
- Mueller SE, Petitjean S, Boening J, Wiesbeck GA. The impact of self-help group attendance on relapse rates after alcohol detoxification in a controlled study. Alcohol & Alcoholism. 2007;41(4):108–112. doi: 10.1093/alcalc/agl122. [DOI] [PubMed] [Google Scholar]
- Namkoong K, Shah DV, Han JY, Kim SC, Yoo W, Fan D, Gustafson DH, et al. Expression and reception of treatment information in breast cancer support groups: How health self-efficacy moderates effects on emotional well-being. Patient Education and Counseling. 2010;81(1):S41–S47. doi: 10.1016/j.pec.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA) Infofacts: Treatment statistics. 2011 Mar; Retrieved from http://www.drugabuse.gov/publications/infofacts/treatment-statistics.
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51(3):390–395. doi: 10.1037/0022-006X.51.3.390. [DOI] [PubMed] [Google Scholar]
- Rhodes F, Fishbein M, Reis J. Using behavioral theory in computer-based health promotion and appraisal. Health Education & Behavior. 1997;24(1):20–34. doi: 10.1177/109019819702400105. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist. 2000;55(1):68–78. doi: 10.1037/0003-66X.55.1.68. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Deci EL. Self-regulation and the problem of human autonomy: Does psychology need choice, self-determination, and will? Journal of Personality. 2006;74(6):1557–1586. doi: 10.1111/j.1467-6494.2006.00420.x. [DOI] [PubMed] [Google Scholar]
- Simpson DD. A conceptual framework for drug treatment process and outcomes. Journal of Substance Abuse Treatment. 2004;27(2):99–121. doi: 10.1016/j.jsat.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Slaymaker VJ, Owen PL. Employed men and women substance abusers: Job troubles and treatment outcomes. Journal of Substance Abuse Treatment. 2006;31(4):347–354. doi: 10.1016/j.jsat.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Smaglik P, Hawkins RP, Pingree S, Gustafson DH, Boberg EW, Bricker E. The quality of interactive computer use among HIV-infected individuals. Journal of Health Communication. 1998;3(1):53–68. doi: 10.1080/108107398127508. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The DASIS Report: Polydrug use among treatment admissions: 1998. (Office of Applied Studies) 2001 Retrieved from http://oas.samhsa.gov/2k1/polydrugTX/polydrugTX.htm.
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings (Office of Applied Studies, NSDUH Series H-36, HHS Publication No. SMA 09-4434) Rockville, MD: 2009. Retrieved from http://www.oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.pdf. [Google Scholar]
- White WL, Boyle M, Loveland D. Alcoholism/addiction as a chronic disease: From rhetoric to clinical reality. Alcoholism Treatment Quarterly. 2002;20(3/4):107–130. doi: 10.1300/J020v20n03_06. [DOI] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]


