Abstract
The beneficial biologic effects attributed to vitamin D suggest a potential to influence overall mortality. Evidence addressing this hypothesis is limited, especially for African Americans who have a high prevalence of vitamin D insufficiency. The authors conducted a nested case-control study within the prospective Southern Community Cohort Study to relate baseline serum levels of 25-hydroxyvitamin D (25(OH)D) with subsequent mortality. Cases were 1,852 participants who enrolled from 2002 to 2009 and died >12 months postenrollment. Controls (n = 1,852) were matched on race, sex, age, enrollment site, and blood collection date. The odds ratios for quartile 1 (<10.18 ng/mL) versus quartile 4 (>21.64 ng/mL) levels of 25(OH)D were 1.60 (95% confidence interval (CI): 1.20, 2.14) for African Americans and 2.11 (95% CI: 1.39, 3.21) for non-African Americans. The effects were strongest for circulatory disease death, where quartile 1 versus quartile 4 odds ratios were 2.53 (95% CI: 1.44, 4.46) and 3.25 (95% CI: 1.33, 7.93) for African Americans and non-African Americans, respectively. The estimated odds of total mortality were minimized in the 25(OH)D range of 35–40 ng/mL. These findings provide support for the hypothesis that vitamin D status may have an important influence on mortality for both African Americans and non-African Americans.
Keywords: African Americans, biological markers, cardiovascular diseases, mortality, neoplasms, prospective studies, vitamin D, vitamin D deficiency
Vitamin D, in addition to its established role in maintaining bone health, has been cited as a potential protective factor for a number of diseases, including certain cancers, cardiovascular disease, diabetes, and autoimmune disease (1). A therapeutic role for vitamin D is being explored for many of these conditions (2–6). Among the wide-ranging biologic effects attributed to vitamin D are the regulation of inflammation, cellular proliferation, cellular differentiation, angiogenesis, and apoptosis, which are key cancer-related mechanisms (7). Vitamin D is also thought to play a role in regulating the immune and renin-angiotensin systems, insulin secretion, and thrombogenic activity (8–10). Thus, it is reasonable to assume that vitamin D status, given its broad ramifications, may have the potential to influence overall mortality. The existing body of work addressing this question is still limited, and observational studies of circulating 25-hydroxyvitamin D (25(OH)D), the clinical measure of vitamin D status, in relation to all-cause mortality have, with few exceptions (11–13), been relatively small, involving anywhere from 50 to 750 deaths (14–21). Furthermore, African Americans are recognized as being at high risk for vitamin D insufficiency (1) and have mortality rates higher than any other racial group in the United States (22). Yet the association between vitamin D status and overall mortality among African Americans is particularly understudied. The importance of vitamin D as a potential mediator of racial health disparities in the United States merits its exploration in relation to mortality in studies involving large numbers of African Americans.
Without randomized controlled trials designed to specifically address mortality endpoints, prospective cohort studies with baseline assessment of 25(OH)D can currently provide some of the most informative data to assess a potential link between vitamin D and mortality risk. Our objective was therefore to investigate the association between baseline serum 25(OH)D levels and subsequent mortality in a large, multiracial prospective cohort study.
MATERIALS AND METHODS
The Southern Community Cohort Study (SCCS) was approved by institutional review boards at Vanderbilt University and Meharry Medical College, and all participants provided written, informed consent.
Study population
The SCCS is a prospective cohort study designed to investigate racial disparities in cancer that enrolled over 85,000 men and women in 12 southeastern US states from 2002 to 2009. Comprehensive study details are provided elsewhere (23). In brief, individuals were eligible for enrollment if they were aged 40–79 years, English speaking, and had not been under treatment for cancer within the past year. Approximately two-thirds of SCCS participants self-reported their race as African American; the remainder were mostly non-Hispanic white. Recruitment took place primarily (86%) at community health centers, with a smaller proportion (14%) enrolling through the mail in the same geographic area. This analysis was restricted to community health center-enrolled participants, as blood samples were not collected from participants who enrolled through the mail.
At the community health centers, trained study interviewers administered a computer-assisted personal interview to collect baseline data on demographic characteristics, lifestyle factors, body size, and medical history. More than half (54%) of the participants provided a 20-mL nonfasting baseline blood sample, which was kept chilled until processing and freezing at −80°C the next day.
Case identification and control selection
The cohort was followed prospectively for mortality via linkage to the Social Security Administration's Death Master File and the National Death Index. Excluding deaths that occurred within 1 year of enrollment, we identified 3,953 deaths as of April 2010. Of these, 1,854 had a serum sample in frozen storage, and 25(OH)D measurement (described below) was successful for 1,852, forming the case group for this analysis with death dates ranging from May 2003 to February 2010. These deaths occurred an average of 3.6 (range: 1.0–7.8) years after study enrollment. Controls, who were alive on the death date of their corresponding case, were individually matched on sex, race (black/white/other), age at enrollment (±3 years), community health center enrollment site, and date of blood collection (±6 weeks). The latter 2 matching criteria provided tight control of the geographic location and season of blood collection. The mean absolute difference in the date of blood collection between the cases and their matched controls was 2.5 (standard deviation: 1.8) weeks. Matching on exact enrollment site could not be achieved for 10.6% of the cases, nor matching on exact race for 0.7% of the cases, but analyses restricted to the 89% with exact matching for all criteria provided the same overall results.
Of the 1,852 deaths studied, 1,798 occurred prior to January 1, 2010, the time period for which the National Death Index had cause of death data available. We obtained the underlying cause of death from the National Death Index for 1,774 (98.7%) of the deaths in this time period and created classifications based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) (version for 2007), as follows: cancer death (n = 477) (ICD-10 codes C00–C97); circulatory disease death (n = 537), which included hypertension (n = 86) (ICD-10 codes I10–I13), ischemic heart disease (n = 260) (ICD-10 codes I20–I25), pulmonary heart disease (n = 14) (ICD-10 codes I26–I28), cardiac arrest and arrhythmias (n = 43) (ICD-10 codes I44–I49), heart failure (n = 34) (ICD-10 code I50), cerebrovascular disease (n = 90) (ICD-10 codes I60–I69), atherosclerosis, and other diseases of the arteries, arterioles, and capillaries (n = 10) (ICD-10 codes I70–I78); and all other nonexternal causes (n = 621), which included all other deaths except those already classified as a cancer or circulatory disease death, or having ICD-10 codes beginning with S, T, V, W, X, or Y.
Serum 25(OH)D measurement
Serum 25(OH)D levels were measured at Heartland Assays, Inc. (Ames, Iowa), by using a US Food and Drug Administration-approved direct, competitive, chemiluminescence immunoassay, the DiaSorin LIAISON 25 OH Vitamin D TOTAL assay (DiaSorin, Stillwater, Minnesota), which is co-specific for 25-hydroxyvitamin D2 and D3 (24, 25). Among 10 (blinded) triplicate sets of identical serum samples included for quality control, the average intraassay coefficient of variation was 4.2%.
Statistical analysis
Serum 25(OH)D quartiles were determined on the basis of the distribution among the controls, with 25%, 50%, and 75% cutoffs of 10.18, 15.15, and 21.64 ng/mL. Although the distributions of 25(OH)D measurements varied by race, there were sufficient overlap and adequate numbers of African Americans and non-African Americans across each quartile to avoid the need for race-specific quartiles. Mean 25(OH)D levels within each quartile were nearly identical by sex (quartile 1: 7.5, 7.2; quartile 2: 12.6, 12.4; quartile 3: 18.2, 18.3; quartile 4: 29.6, 28.9 ng/mL for males and females, respectively) and by race (quartile 1: 7.3, 7.5; quartile 2: 12.5, 12.5; quartile 3: 18.1, 18.5; quartile 4: 29.3, 29.5 ng/mL for African Americans and non-African Americans, respectively).
Mean 25(OH)D levels were compared across participant characteristics by using 1-way analysis of variance or t tests. Participant characteristics were also compared by case-control status by Pearson's χ2 test. Conditional logistic regression was used to estimate odds ratios and 95% confidence intervals for all-cause and cause-specific mortality in relation to quartiles of serum 25(OH)D. Matching factors were accounted for in the conditional analysis, and additional covariates included body mass index (using a continuous and quadratic term), smoking status (never, former smoker of below-median pack-years, former smoker of above-median pack-years, current smoker of below-median pack-years, current smoker of above-median pack-years), annual household income (<$15,000, $15,000–$24,999, $25,000–$49,999, ≥$50,000), and total work and leisure time physical activity (in quartiles of metabolic equivalent-hours/day). Other potential confounders that were examined but not retained in the final models included education, total energy intake, height, alcohol intake, health insurance status, marital status, and (for women) use of hormone replacement therapy. Time participating in sports, because of its potential for a stronger relation with outdoor exposure, was tested as a replacement for total physical activity in the models, but the results did not change. To examine the shape of the continuous relation between 25(OH)D and mortality risk, we also utilized fully adjusted restricted cubic spline models.
Interaction by race, sex, and body mass index was assessed by using the likelihood ratio test to compare models with and without the relevant interactions terms. We found no significant interaction by sex or by body mass index. Where we found significant interaction by race, race-specific results are presented. African-American versus white results were nearly identical to African-American versus non-African-American results, so only the latter are presented.
All analyses were performed by using SAS, version 9.2, statistical software (SAS Institute, Inc., Cary, North Carolina). All P values are 2 sided.
RESULTS
Mean serum 25(OH)D levels varied significantly across strata of age, race, sex, season of blood collection, body mass index, smoking status, and household income (Table 1). The 2 major determinants of 25(OH)D levels, race and season of blood collection, showed expected patterns, with African Americans having levels an average of 5.1 ng/mL lower than whites and blood collected in winter having levels 5.6 ng/mL lower than those collected in summer (a seasonal pattern seen for both African Americans and non-African Americans).
Table 1.
Distribution of Baseline Characteristics and Mean Serum 25(OH)D Levels, by Strata of Baseline Characteristics, for 3,704 US Participants in the Southern Community Cohort Study, 2002–2010
| Baseline Characteristic | Mean 25(OH)D Levels (SD) | P Valuea | Cases (n = 1,852) |
Controls (n = 1,852) |
P Valueb | ||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | ||||
| Age at study enrollment, years | |||||||
| 40–49 | 15.8 (9.5) | 607 | 32.8 | 624 | 33.7 | ||
| 50–59 | 15.5 (8.4) | 679 | 36.7 | 660 | 35.6 | ||
| ≥60 | 17.3 (10.0) | <0.001 | 566 | 30.6 | 568 | 30.7 | 0.78 |
| Race | |||||||
| African American | 14.7 (8.4) | 1,275 | 68.8 | 1,286 | 69.4 | ||
| White | 19.8 (10.3) | 504 | 27.2 | 502 | 27.1 | ||
| Other | 17.1 (9.0) | <0.001 | 73 | 3.9 | 64 | 3.5 | 0.73 |
| Sex | |||||||
| Female | 14.7 (9.0) | 777 | 42.0 | 777 | 42.0 | ||
| Male | 17.2 (9.3) | <0.001 | 1,075 | 58.0 | 1,075 | 58.0 | 1.0 |
| Season of blood collectionc | |||||||
| Winter | 12.7 (7.5) | 345 | 18.6 | 333 | 18.0 | ||
| Spring | 14.8 (9.5) | 525 | 28.4 | 514 | 27.8 | ||
| Summer | 18.3 (9.4) | 565 | 30.5 | 588 | 31.8 | ||
| Autumn | 17.6 (9.1) | <0.001 | 417 | 22.5 | 417 | 22.5 | 0.85 |
| Body mass indexd | |||||||
| <25 | 17.0 (10.1) | 608 | 32.8 | 523 | 28.2 | ||
| 25–29.9 | 17.0 (9.2) | 536 | 28.9 | 588 | 31.8 | ||
| 30–34.9 | 16.0 (8.7) | 329 | 17.8 | 390 | 21.1 | ||
| ≥35 | 13.6 (8.4) | <0.001 | 353 | 19.1 | 340 | 18.4 | 0.003 |
| Missing | 26 | 1.4 | 11 | 0.6 | |||
| Total activity, MET-hours/daye | |||||||
| Quartile 1 (<7.97) | 15.9 (8.7) | 619 | 33.4 | 459 | 24.8 | ||
| Quartile 2 (7.97–17.14) | 16.2 (10.1) | 529 | 28.6 | 460 | 24.8 | ||
| Quartile 3 (17.15–31.68) | 15.8 (8.9) | 368 | 19.9 | 458 | 24.7 | ||
| Quartile 4 (>31.68) | 16.8 (9.4) | 0.13 | 320 | 17.3 | 459 | 24.8 | <0.001 |
| Missing | 16 | 0.9 | 16 | 0.9 | |||
| Smoking status at enrollment | |||||||
| Current | 15.7 (8.8) | 1,021 | 55.1 | 841 | 45.4 | ||
| Former | 17.5 (10.1) | 438 | 23.7 | 441 | 23.8 | ||
| Never | 15.6 (9.2) | <0.001 | 391 | 21.1 | 566 | 30.6 | <0.001 |
| Missing | 2 | 0.1 | 4 | 0.2 | |||
| Annual household income, $ | |||||||
| <15,000 | 16.0 (9.1) | 1,333 | 72.0 | 1,190 | 64.3 | ||
| 15,000–24,999 | 15.9 (9.3) | 345 | 18.6 | 387 | 20.9 | ||
| 25,000–49,999 | 17.0 (10.0) | 124 | 6.7 | 201 | 10.9 | ||
| ≥50,000 | 18.3 (10.2) | 0.03 | 32 | 1.7 | 59 | 3.2 | <0.001 |
| Missing | 18 | 1.0 | 15 | 0.8 | |||
Abbreviations: 25(OH)D, 25-hydroxyvitamin D; MET, metabolic equivalent; SD, standard deviation.
a P value comparing the mean serum levels of 25(OH)D estimated by using 1-way analysis of variance (for variables with >2 levels) or 2-sample t tests (for variables with 2 levels).
b P value from a Pearson χ2 test of whether the distribution of the participant's characteristic differs between cases and controls, not including missing values.
c Winter: December–February; spring: March–May; summer: June–August; autumn: September–November.
d Body mass index: weight (kg)/height (m)2.
e Includes both leisure time- and work-related activity.
We observed a significant trend (Ptrend < 0.001) of increasing risk of all-cause mortality with decreasing quartiles of serum 25(OH)D (Table 2). Those in the lowest quartile had an 80% increased mortality risk (95% CI: 1.43, 2.27) compared with those in the highest quartile. To evaluate whether preexisting disease affected these results, we repeated the analyses among participants without a reported history of heart attack/bypass surgery (odds ratio for quartile 1 (ORQ1) = 1.84, 95% CI: 1.47, 2.31), diabetes (ORQ1 = 1.55, 95% CI: 1.21, 1.99), hypertension (ORQ1 = 1.55, 95% CI: 1.08, 2.21), hypercholesterolemia (ORQ1 = 1.75, 95% CI: 1.34, 2.29), stroke/transient ischemic attack (ORQ1 = 1.68, 95% CI: 1.34, 2.10), emphysema/chronic bronchitis (ORQ1 = 1.67, 95% CI: 1.33, 2.09), or any of these 6 conditions (ORQ1 = 1.65, 95% CI: 1.05, 2.60) and found that the association persisted. Vitamin D was also a mortality risk factor for subjects who were nonsmokers at baseline (ORQ1 = 1.56, 95% CI: 1.02, 2.39) and who were of healthy weight (body mass index of 18.5–<25 kg/m2) at baseline (ORQ1 = 2.29, 95% CI: 1.55, 3.38).
Table 2.
Association Between Baseline Serum Levels of 25(OH)D and Subsequent All-Cause Mortality, Southern Community Cohort Study, 2002–2010
| Serum 25(OH)D, ng/mL | Cases, no. (n = 1,852) | Controls, no. (n = 1,852) | Multivariate ORa | 95% CI |
|---|---|---|---|---|
| All participants (n = 3,704) | ||||
| Quartile 4 (>21.64) | 364 | 463 | 1.00 | Referent |
| Quartile 3 (15.16–21.64) | 405 | 463 | 1.17 | 0.95, 1.45 |
| Quartile 2 (10.18–15.15) | 482 | 463 | 1.41 | 1.14, 1.74 |
| Quartile 1 (<10.18) | 601 | 463 | 1.80 | 1.43, 2.27 |
| Ptrend | <0.001 | |||
| African Americans (n = 2,550)b | ||||
| Quartile 4 (>21.64) | 181 | 219 | 1.00 | Referent |
| Quartile 3 (15.16–21.64) | 266 | 299 | 1.15 | 0.87, 1.53 |
| Quartile 2 (10.18–15.15) | 353 | 377 | 1.19 | 0.91, 1.57 |
| Quartile 1 (<10.18) | 475 | 380 | 1.60 | 1.20, 2.14 |
| Ptrend | 0.003 | |||
| Non-African Americans (n = 1,132)b,c | ||||
| Quartile 4 (>21.64) | 179 | 240 | 1.00 | Referent |
| Quartile 3 (15.16–21.64) | 136 | 160 | 1.09 | 0.78, 1.52 |
| Quartile 2 (10.18–15.15) | 129 | 85 | 1.99 | 1.37, 2.90 |
| Quartile 1 (<10.18) | 122 | 81 | 2.11 | 1.39, 3.21 |
| Ptrend | <0.001 | |||
Abbreviations: CI, confidence interval; 25(OH)D, 25-hydroxyvitamin D; OR, odds ratio.
a Odds ratio and 95% confidence interval from a conditional logistic regression model accounting for the matching factors and adjusted for body mass index, smoking, physical activity, and household income.
b Analysis restricted to case-control pairs with exact matching on race.
c Non-African-American group composed of 89% non-Hispanic whites and 11% other race/ethnicity.
Although trends of increasing risk with decreasing 25(OH)D levels were significant for both racial groups, the effect was somewhat stronger for non-African Americans than for African Americans (Pinteraction < 0.001) (Table 2). By use of classifications recently issued by the Institute of Medicine (26) (with >20 ng/mL as the referent “adequate” level), African Americans with “inadequate” (12–20 ng/mL) and “deficient” (<12 ng/mL) levels had odds ratios of 0.95 (95% CI: 0.75, 1.21) and 1.35 (95% CI: 1.05, 1.74), and non-African Americans had odds ratios of 1.30 (95% CI: 0.96, 1.78) and 2.20 (95% CI: 1.51, 3.19), respectively. Using an alternate referent value suggested by others (1, 27) to represent vitamin D adequacy (>30 ng/mL), we found that African Americans with levels of 12–30 ng/mL and <12 ng/mL had odds ratios of 1.18 (95% CI: 0.79, 1.75) and 1.63 (95% CI: 1.08, 2.45), and non-African Americans had odds ratios of 1.27 (95% CI: 0.82, 1.95) and 2.37 (95% CI: 1.41, 3.96), respectively.
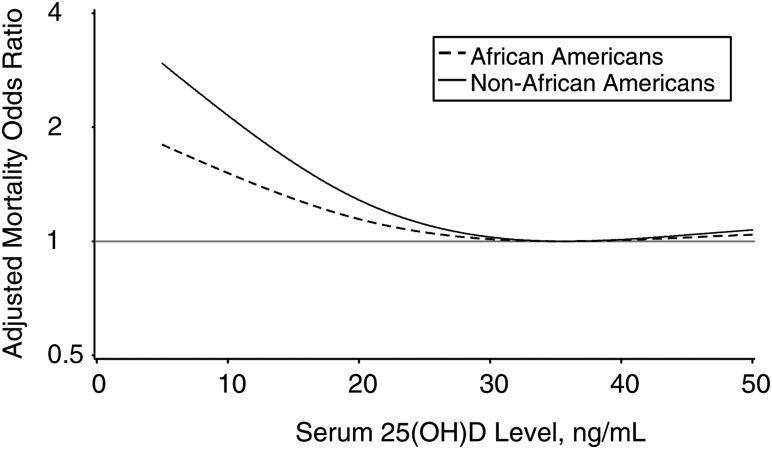
Figure 1 shows the estimated continuous association between serum 25(OH)D levels and mortality by using race-stratified restricted cubic spline models with knots at 5, 20, and 45 ng/mL. For African Americans, the odds of overall mortality reached its minimum at 35.4 ng/mL and, for non-African Americans, at 35.7 ng/mL. We applied 20 different variations for the placement of the 3 knots, and the odds of overall mortality reached its minimum in the 25(OH)D range of 35–40 ng/mL for the majority (34 of 40) of these models among African Americans and non-African Americans (not shown).
Figure 1.
Restricted cubic spline plots of the association between serum 25(OH)D and all-cause mortality, Southern Community Cohort Study, 2002–2010. Plots for African Americans (dashed line) and non-African Americans (solid line) depict predicted odds ratios from fully adjusted restricted cubic spline models with knots at 5, 20, and 45 ng/mL. 25(OH)D, 25-hydroxyvitamin D.
Serum 25(OH)D levels were not significantly associated with total cancer mortality, although there was a suggestion of an adverse effect for the lowest quartile (odds ratio = 1.28, 95% CI: 0.78, 2.11) (Table 3). In contrast, circulatory disease mortality was significantly elevated at below-median levels of 25(OH)D, with stronger effects seen for non-African Americans (Pinteraction = 0.004). Having quartile 1 levels of 25(OH)D was associated with an odds ratio of 2.53 (95% CI: 1.44, 4.46) among African Americans and 3.25 (95% CI: 1.33, 7.93) among non-African Americans. Our results also suggest an inverse association between 25(OH)D and mortality for an aggregate group of all other disease causes (Ptrend = 0.001), with an odds ratio for the lowest quartile of 1.72 (95% CI: 1.15, 2.58).
Table 3.
Association Between Baseline Serum Levels of 25(OH)D and Subsequent Cause-specific Mortality, Southern Community Cohort Study, 2002–2010
| Cause of Death | Pinteraction by Race | Cases, no. | Controls, no. | Multivariate ORa | 95% CI |
|---|---|---|---|---|---|
| Cancerb | 0.99 | ||||
| Quartile 4 (>21.64) | 115 | 113 | 1.00 | Referent | |
| Quartile 3 (15.16–21.64) | 102 | 126 | 0.79 | 0.52, 1.21 | |
| Quartile 2 (10.18–15.15) | 127 | 128 | 1.03 | 0.66, 1.59 | |
| Quartile 1 (<10.18) | 133 | 110 | 1.28 | 0.78, 2.11 | |
| Ptrend | 0.53 | ||||
| Circulatory disease | 0.004 | ||||
| African Americansb,c | |||||
| Quartile 4 (>21.64) | 41 | 68 | 1.00 | Referent | |
| Quartile 3 (15.16–21.64) | 76 | 86 | 1.67 | 0.95, 2.93 | |
| Quartile 2 (10.18–15.15) | 116 | 109 | 1.78 | 1.05, 3.01 | |
| Quartile 1 (<10.18) | 144 | 114 | 2.53 | 1.44, 4.46 | |
| Ptrend | 0.01 | ||||
| Non-African Americansb,c | |||||
| Quartile 4 (>21.64) | 40 | 67 | 1.00 | Referent | |
| Quartile 3 (15.16–21.64) | 38 | 46 | 1.09 | 0.51, 2.30 | |
| Quartile 2 (10.18–15.15) | 37 | 19 | 3.66 | 1.50, 8.95 | |
| Quartile 1 (<10.18) | 39 | 22 | 3.25 | 1.33, 7.93 | |
| Ptrend | 0.01 | ||||
| All other nonexternal causesb | 0.15 | ||||
| Quartile 4 (>21.64) | 114 | 153 | 1.00 | Referent | |
| Quartile 3 (15.16–21.64) | 141 | 147 | 1.40 | 0.94, 2.09 | |
| Quartile 2 (10.18–15.15) | 144 | 149 | 1.45 | 0.98, 2.14 | |
| Quartile 1 (<10.18) | 222 | 172 | 1.72 | 1.15, 2.58 | |
| Ptrend | 0.001 | ||||
Abbreviations: CI, confidence interval; 25(OH)D, 25-hydroxyvitamin D; OR, odds ratio.
a Odds ratio and 95% confidence interval from a conditional logistic regression model accounting for the matching factors and adjusted for body mass index, smoking, physical activity, and household income.
b The numbers of cases and controls were, respectively, for cancer: 477 and 477; circulatory disease, African American: 377 and 377; circulatory disease, non-African American: 154 and 154; and all other nonexternal causes: 621 and 621.
c Analysis restricted to case-control pairs with exact matching on race.
DISCUSSION
We observed that low serum levels of 25(OH)D were associated with an increased risk of subsequent mortality among African Americans and non-African Americans. Many reports have shown low 25(OH)D levels to be predictive of poor prognosis among seriously ill patients (28–32), but if causal, an association between vitamin D and mortality among normal middle-aged adults would have far more serious public health implications. To our knowledge, the only previous study to report African-American–specific results regarding vitamin D and total mortality was that by Melamed et al. (11) within the Third National Health and Nutrition Examination Survey, which found no significant association with bottom quartile 25(OH)D levels (odds ratio = 1.05, 95% CI: 0.77, 1.44), although their analysis was based on only 401 African-American deaths and could not statistically distinguish these findings from the positive results among non-Hispanic whites. Nearly all previous epidemiologic studies of vitamin D and mortality have been conducted in populations entirely or largely of European descent (refer to reference 33 for review) (19, 20). Our study provides some of the first evidence that clinical vitamin D status may play an important role in mortality risk for African Americans, among whom vitamin D insufficiency is widespread (34).
To date, there are no published data from randomized controlled trials designed specifically to assess the effect of vitamin D supplementation on total mortality. However, Autier and Gandini (35) conducted a mortality outcome meta-analysis of 18 trials involving subjects randomized to vitamin D supplementation for other endpoints, mainly bone mineral density or bone fractures. Although this analysis was limited in some respects by the design orientation of the original trials (e.g., by and large, the studies were conducted among frail, elderly individuals of European descent taking ordinary doses of vitamin D supplements often with the addition of calcium), they did report a significant 7% reduction in total mortality risk among vitamin D supplement users with a mean daily dose of 528 IU and a mean follow-up time of 5.7 years (range: from 6 months to 7 years) (35). Among observational studies, several (including our own) are now in close accord in reporting an approximate doubling of mortality risk for 25(OH)D levels below ∼10 ng/mL (12, 14, 15, 17), and a recent meta-analysis of prospective observational studies with follow-up for overall mortality ranging from 1.3 to 13 years reported a summary relative risk for mortality of 0.77 (95% CI: 0.70, 0.84) associated with a 10-ng/mL increase in 25(OH)D over a median reference category of ∼11 ng/mL (33). With 25(OH)D levels slowly decreasing in the adult US population (36), and with 21% of non-Hispanic whites and 73% of blacks currently estimated to have levels <20 ng/mL (34), these accumulating findings highlight the need to focus clinical attention on attaining adequate vitamin D levels.
Our findings may help to inform the current debate about the scope of the public health impact of vitamin D insufficiency and delineating “goal” levels of circulating 25(OH)D. Although an Institute of Medicine report recently classified serum 25(OH)D levels above 20 ng/mL as adequate (26), others have suggested values of 30 ng/mL or higher (1, 27). Bischoff-Ferrari et al. (37) have proposed that 25(OH)D levels of 36–40 ng/mL would be optimal with regard to several health endpoints, which corresponds well with our spline model predictions that the odds of mortality would minimize at 25(OH)D levels in the range of 35–40 ng/mL.
We did not find a significant inverse association between serum 25(OH)D and subsequent total cancer mortality, in agreement with some (13, 17, 38) but not all (18, 39) observational studies. Randomized controlled trials of bone fractures have generally failed to detect significant benefits of vitamin D supplementation on total cancer mortality (40, 41), and some recent analyses even suggested adverse effects on cancer mortality at high (>40 ng/mL) blood levels (18, 38). Given the heterogeneous nature of cancer, grouping deaths across all cancer sites could obscure associations with specific cancers, but few studies have been sufficiently powered to examine cancer types individually for mortality. This may be resolved with ongoing follow-up of existing cohorts.
We found strong associations between baseline 25(OH)D and subsequent death from diseases of the circulatory system. This likely reflects contributions from multiple cardiovascular disease risk factors such as hypertension, atherosclerosis, inflammation, diabetes, and chronic kidney disease, all of which have been associated with vitamin D (8, 42). Cells of vascular system tissue, including the heart, express the vitamin D receptor, and experimental data suggest that vitamin D receptor activation positively influences cardiovascular function through effects on vascular smooth muscle cell growth, fibrinolysis, inflammation, thrombogenicity, and endothelial regeneration (43–48). Calcitriol downregulates the renin-angiotensin system (49), and vitamin D receptor knockout mice develop phenotypes of hypertension, left ventricular hypertrophy, and enhanced thrombogenic activity (44, 49). Similarly, human studies have shown that both ultraviolet B radiation and vitamin D supplementation may decrease blood pressure levels (50, 51). Overall, experimental data reinforce mounting epidemiologic evidence of a link between vitamin D and cardiovascular dysfunction, incident cardiovascular events, and cardiovascular disease mortality (52–56).
Limitations of our study should be discussed. First, this is an observational study and not a randomized controlled trial and, thus, is susceptible to confounding influences that hinder causal inference. Second, the SCCS population is by design not representative of the general US population. The cohort is composed heavily of individuals of low socioeconomic status, having enrolled the vast majority of cohort members at community health centers that provide health services in medically underserved, low-income areas (23). However, this should not interfere with the validity of our internal analyses. Moreover, the sample of participants from which the cases and controls arose (i.e., the subset who provided baseline blood samples) is very similar with respect to age, education, income, body size, health habits (e.g., smoking), and medical history to that which did not provide a baseline blood sample (data not shown), so we can infer that our study sample is representative of the SCCS cohort. Third, we used only one 25(OH)D measurement as a proxy of “typical” vitamin D status, although we observed an intraclass correlation coefficient of 0.87 (95% CI: 0.83, 0.90) for serial measurements of 25(OH)D taken 1–3 years apart in a sample of more than 200 SCCS participants (57). Other groups have also found a single 25(OH)D measurement to adequately represent vitamin D status (58, 59). Fourth, our data were too sparse at high levels of 25(OH)D to feasibly estimate an association with mortality at levels where adverse effects on disease and mortality have been reported (11, 18, 38). Finally, the available follow-up period was relatively short, and it will be of interest to determine whether our findings vary with extended follow-up. Of concern is the possibility that morbidity in the time period leading up to death would discourage outdoor (and thus sun) exposure, creating a reverse-causation bias. We took steps to mitigate this problem by restricting case selection to deaths that occurred after at least 1 year of follow-up. Subanalyses among deaths that occurred after 3.6 years (our average) of follow-up still showed a strong association with 25(OH)D: ORQ3 = 1.15 (95% CI: 0.84, 1.58), ORQ2 = 1.42 (95% CI: 1.04, 1.95), ORQ1 = 1.64 (95% CI: 1.16, 2.30), similar for African Americans and non-African Americans. We also calculated the association between vitamin D and mortality among participants reportedly free of several chronic diseases at baseline and saw little effect on our results.
This investigation also has several notable strengths. To our knowledge, this study included the largest number of deaths of any single previous investigation of 25(OH)D and all-cause mortality. Further, unlike clinical populations, this community-based cohort allowed us to relate vitamin D status to subsequent mortality with findings of greater generalizability. Finally, we believe this represents the first robust assessment of the vitamin D–mortality association among African Americans, for whom vitamin D status has been a longstanding concern.
In conclusion, this study provides evidence that vitamin D status may have an important influence on mortality risk for African Americans and non-African Americans.
ACKNOWLEDGMENTS
Author affiliations: International Epidemiology Institute, Rockville, Maryland (Lisa B. Signorello, Xijing Han, Sarah S. Cohen, Elizabeth L. Cope, William J. Blot); Division of Epidemiology, Department of Medicine, Vanderbilt University, Nashville, Tennessee (Lisa B. Signorello, Qiuyin Cai, Wei Zheng, William J. Blot); and the Vanderbilt-Ingram Cancer Center, Nashville, Tennessee (Lisa B. Signorello, Qiuyin Cai, Wei Zheng, William J. Blot).
This work was supported by a grant from the National Cancer Institute at the National Institutes of Health (R01 CA092447).
The authors gratefully acknowledge the work of Dr. Ronald Horst of Heartland Assays (Ames, Iowa) whose laboratory performed the serum 25(OH)D measurements, Heather Munro of the International Epidemiology Institute (Rockville, Maryland) for statistical review of this manuscript prior to submission, and Dr. Jie Wu and Regina Courtney of Vanderbilt University (Nashville, Tennessee) for their excellent assistance in the lab with sample handling, preparation, and quality control.
Conflict of interest: none declared.
REFERENCES
- 1.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 2.Chadha MK, Tian L, Mashtare T, et al. Phase 2 trial of weekly intravenous 1,25 dihydroxy cholecalciferol (calcitriol) in combination with dexamethasone for castration-resistant prostate cancer. Cancer. 2010;116(9):2132–2139. doi: 10.1002/cncr.24973. [DOI] [PubMed] [Google Scholar]
- 3.Laverny G, Penna G, Vetrano S, et al. Efficacy of a potent and safe vitamin D receptor agonist for the treatment of inflammatory bowel disease. Immunol Lett. 2010;131(1):49–58. doi: 10.1016/j.imlet.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 4.Penna G, Amuchastegui S, Laverny G, et al. Vitamin D receptor agonists in the treatment of autoimmune diseases: selective targeting of myeloid but not plasmacytoid dendritic cells. J Bone Miner Res. 2007;22(suppl 2):V69–V73. doi: 10.1359/jbmr.07s217. [DOI] [PubMed] [Google Scholar]
- 5.Wu-Wong JR. Potential for vitamin D receptor agonists in the treatment of cardiovascular disease. Br J Pharmacol. 2009;158(2):395–412. doi: 10.1111/j.1476-5381.2009.00171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walsh JE, Clark AM, Day TA, et al. Use of α,25-dihydroxyvitamin D3 treatment to stimulate immune infiltration into head and neck squamous cell carcinoma. Hum Immunol. 2010;71(7):659–665. doi: 10.1016/j.humimm.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garland CF, Garland FC, Gorham ED, et al. The role of vitamin D in cancer prevention. Am J Public Health. 2006;96(2):252–261. doi: 10.2105/AJPH.2004.045260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu-Wong JR. Potential for vitamin D receptor agonists in the treatment of cardiovascular disease. Br J Pharmacol. 2009;158(2):395–412. doi: 10.1111/j.1476-5381.2009.00171.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boucher BJ. Vitamin D insufficiency and diabetes risks. Curr Drug Targets. 2011;12(1):61–87. doi: 10.2174/138945011793591653. [DOI] [PubMed] [Google Scholar]
- 10.Bikle DD. Vitamin D regulation of immune function. Vitam Horm. 2011;86:1–21. doi: 10.1016/B978-0-12-386960-9.00001-0. doi:10.1016/B978-0-12-386960-9.00001-0. [DOI] [PubMed] [Google Scholar]
- 11.Melamed ML, Michos ED, Post W, et al. 25-Hydroxyvitamin D levels and the risk of mortality in the general population. Arch Intern Med. 2008;168(15):1629–1637. doi: 10.1001/archinte.168.15.1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ginde AA, Scragg R, Schwartz RS, et al. Prospective study of serum 25-hydroxyvitamin D level, cardiovascular disease mortality, and all-cause mortality in older U.S. adults. J Am Geriatr Soc. 2009;57(9):1595–1603. doi: 10.1111/j.1532-5415.2009.02359.x. [DOI] [PubMed] [Google Scholar]
- 13.Hutchinson MS, Grimnes G, Joakimsen RM, et al. Low serum 25-hydroxyvitamin D levels are associated with increased all-cause mortality risk in a general population: the Tromso Study. Eur J Endocrinol. 2010;162(5):935–942. doi: 10.1530/EJE-09-1041. [DOI] [PubMed] [Google Scholar]
- 14.Dobnig H, Pilz S, Scharnagl H, et al. Independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Arch Intern Med. 2008;168(12):1340–1349. doi: 10.1001/archinte.168.12.1340. [DOI] [PubMed] [Google Scholar]
- 15.Pilz S, Dobnig H, Nijpels G, et al. Vitamin D and mortality in older men and women. Clin Endocrinol. 2009;71(5):666–672. doi: 10.1111/j.1365-2265.2009.03548.x. [DOI] [PubMed] [Google Scholar]
- 16.Kuroda T, Shiraki M, Tanaka S, et al. Contributions of 25-hydroxyvitamin D, co-morbidities and bone mass to mortality in Japanese postmenopausal women. Bone. 2009;44(1):168–172. doi: 10.1016/j.bone.2008.03.023. [DOI] [PubMed] [Google Scholar]
- 17.Semba RD, Houston DK, Bandinelli S, et al. Relationship of 25-hydroxyvitamin D with all-cause and cardiovascular disease mortality in older community-dwelling adults. Eur J Clin Nutr. 2010;64(2):203–209. doi: 10.1038/ejcn.2009.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michaelsson K, Baron JA, Snellman G, et al. Plasma vitamin D and mortality in older men: a community-based prospective cohort study. Am J Clin Nutr. 2010;92(4):841–848. doi: 10.3945/ajcn.2010.29749. [DOI] [PubMed] [Google Scholar]
- 19.Johansson H, Oden A, Kanis J, et al. Low serum vitamin D is associated with increased mortality in elderly men: MrOS Sweden. Osteoporos Int. 2012;23(3):991–999. doi: 10.1007/s00198-011-1809-5. [DOI] [PubMed] [Google Scholar]
- 20.Eaton CB, Young A, Allison MA, et al. Prospective association of vitamin D concentrations with mortality in postmenopausal women: results from the Women's Health Initiative (WHI) Am J Clin Nutr. 2011;94(6):1471–1478. doi: 10.3945/ajcn.111.017715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cawthon PM, Parimi N, Barrett-Connor E, et al. Serum 25-hydroxyvitamin D, parathyroid hormone, and mortality in older men. J Clin Endocrinol Metab. 2010;95(10):4625–4634. doi: 10.1210/jc.2010-0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Minino AM. Death in the United States, 2009. Hyattsville, MD: National Center for Health Statistics; 2011. NCHS data brief, no. 64. [Google Scholar]
- 23.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010;21(1 suppl):26S–37S. doi: 10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ersfeld DL, Rao DS, Body JJ, et al. Analytical and clinical validation of the 25 OH vitamin D assay for the LIAISON automated analyzer. Clin Biochem. 2004;37(10):867–874. doi: 10.1016/j.clinbiochem.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Wagner D, Hanwell HE, Vieth R. An evaluation of automated methods for measurement of serum 25-hydroxyvitamin D. Clin Biochem. 2009;42(15):1549–1556. doi: 10.1016/j.clinbiochem.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: National Academy Press; 2010. [Google Scholar]
- 27.Vieth R, Bischoff-Ferrari H, Boucher BJ, et al. The urgent need to recommend an intake of vitamin D that is effective. Am J Clin Nutr. 2007;85(3):649–650. doi: 10.1093/ajcn/85.3.649. [DOI] [PubMed] [Google Scholar]
- 28.Lee P, Eisman JA, Center JR. Vitamin D deficiency in critically ill patients. N Engl J Med. 2009;360(18):1912–1914. doi: 10.1056/NEJMc0809996. [DOI] [PubMed] [Google Scholar]
- 29.Ng K, Meyerhardt JA, Wu K, et al. Circulating 25-hydroxyvitamin D levels and survival in patients with colorectal cancer. J Clin Oncol. 2008;26(18):2984–2991. doi: 10.1200/JCO.2007.15.1027. [DOI] [PubMed] [Google Scholar]
- 30.Wolf M, Shah A, Gutierrez O, et al. Vitamin D levels and early mortality among incident hemodialysis patients. Kidney Int. 2007;72(8):1004–1013. doi: 10.1038/sj.ki.5002451. [DOI] [PubMed] [Google Scholar]
- 31.Matthews LR, Ahmed Y, Wilson KL, et al. Worsening severity of vitamin D deficiency is associated with increased length of stay, surgical intensive care unit cost, and mortality rate in surgical intensive care unit patients. Am J Surg. 2012;204(1):37–43. doi: 10.1016/j.amjsurg.2011.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Braun AB, Gibbons FK, Litonjua AA, et al. Low serum 25-hydroxyvitamin D at critical care initiation is associated with increased mortality. Crit Care Med. 2012;40(1):63–72. doi: 10.1097/CCM.0b013e31822d74f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zittermann A, Iodice S, Pilz S, et al. Vitamin D deficiency and mortality risk in the general population: a meta-analysis of prospective cohort studies. Am J Clin Nutr. 2012;95(1):91–100. doi: 10.3945/ajcn.111.014779. [DOI] [PubMed] [Google Scholar]
- 34.Looker AC, Johnson CL, Lacher DA, et al. Vitamin D Status: United States, 2001–2006. Hyattsville, MD: National Center for Health Statistics; 2011. NCHS data brief, no. 59. [Google Scholar]
- 35.Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167(16):1730–1737. doi: 10.1001/archinte.167.16.1730. [DOI] [PubMed] [Google Scholar]
- 36.Looker AC, Pfeiffer CM, Lacher DA, et al. Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000–2004. Am J Clin Nutr. 2008;88(6):1519–1527. doi: 10.3945/ajcn.2008.26182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bischoff-Ferrari HA, Giovannucci E, Willett WC, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 38.Freedman DM, Looker AC, Abnet CC, et al. Serum 25-hydroxyvitamin D and cancer mortality in the NHANES III study (1988–2006) Cancer Res. 2010;70(21):8587–8597. doi: 10.1158/0008-5472.CAN-10-1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pilz S, Dobnig H, Winklhofer-Roob B, et al. Low serum levels of 25-hydroxyvitamin D predict fatal cancer in patients referred to coronary angiography. Cancer Epidemiol Biomarkers Prev. 2008;17(5):1228–1233. doi: 10.1158/1055-9965.EPI-08-0002. [DOI] [PubMed] [Google Scholar]
- 40.Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double-blind controlled trial. BMJ. 2003;326(7387):469. doi: 10.1136/bmj.326.7387.469. doi:10.1136/bmj.326.7387.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Brunner RL, Wactawski-Wende J, Caan BJ, et al. The effect of calcium plus vitamin D on risk for invasive cancer: results of the Women's Health Initiative (WHI) calcium plus vitamin D randomized clinical trial. Nutr Cancer. 2011;63(6):827–841. doi: 10.1080/01635581.2011.594208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Michos ED, Melamed ML. Vitamin D and cardiovascular disease risk. Curr Opin Clin Nutr Metab Care. 2008;11(1):7–12. doi: 10.1097/MCO.0b013e3282f2f4dd. [DOI] [PubMed] [Google Scholar]
- 43.Mitsuhashi T, Morris RC, Jr, Ives HE. 1,25-Dihydroxyvitamin D3 modulates growth of vascular smooth muscle cells. J Clin Invest. 1991;87(6):1889–1895. doi: 10.1172/JCI115213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Aihara K, Azuma H, Akaike M, et al. Disruption of nuclear vitamin D receptor gene causes enhanced thrombogenicity in mice. J Biol Chem. 2004;279(34):35798–35802. doi: 10.1074/jbc.M404865200. [DOI] [PubMed] [Google Scholar]
- 45.Wu-Wong JR, Nakane M, Ma J, et al. Effects of vitamin D analogs on gene expression profiling in human coronary artery smooth muscle cells. Atherosclerosis. 2006;186(1):20–28. doi: 10.1016/j.atherosclerosis.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 46.Wu-Wong JR, Nakane M, Ma J. Vitamin D analogs modulate the expression of plasminogen activator inhibitor-1, thrombospondin-1 and thrombomodulin in human aortic smooth muscle cells. J Vasc Res. 2007;44(1):11–18. doi: 10.1159/000097812. [DOI] [PubMed] [Google Scholar]
- 47.Bucharles S, Barberato SH, Stinghen AE, et al. Hypovitaminosis D is associated with systemic inflammation and concentric myocardial geometric pattern in hemodialysis patients with low iPTH levels. Nephron Clin Pract. 2011;118(4):c384–c391. doi: 10.1159/000323664. [DOI] [PubMed] [Google Scholar]
- 48.Jablonski KL, Chonchol M, Pierce GL, et al. 25-Hydroxyvitamin D deficiency is associated with inflammation-linked vascular endothelial dysfunction in middle-aged and older adults. Hypertension. 2011;57(1):63–69. doi: 10.1161/HYPERTENSIONAHA.110.160929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li YC, Qiao G, Uskokovic M, et al. Vitamin D: a negative endocrine regulator of the renin-angiotensin system and blood pressure. J Steroid Biochem Mol Biol. 2004;89-90:387–392. doi: 10.1016/j.jsbmb.2004.03.004. doi.org/10.1016/j.jsbmb.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 50.Krause R, Buhring M, Hopfenmuller W, et al. Ultraviolet B and blood pressure. Lancet. 1998;352(9):709–710. doi: 10.1016/S0140-6736(05)60827-6. [DOI] [PubMed] [Google Scholar]
- 51.Judd SE, Raiser SN, Kumari M, et al. 1,25 Dihydroxyvitamin D3 reduces systolic blood pressure in hypertensive adults: a pilot feasibility study. J Steroid Biochem Mol Biol. 2010;121(1-2):445–447. doi: 10.1016/j.jsbmb.2010.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Al Mheid I, Patel R, Murrow J, et al. Vitamin D status is associated with arterial stiffness and vascular dysfunction in healthy humans. J Am Coll Cardiol. 2011;58(6):186–192. doi: 10.1016/j.jacc.2011.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Giovannucci E, Liu Y, Hollis BW, et al. 25-Hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med. 2008;168(11):1174–1180. doi: 10.1001/archinte.168.11.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kilkkinen A, Knekt P, Aro A, et al. Vitamin D status and the risk of cardiovascular disease death. Am J Epidemiol. 2009;170(8):1032–1039. doi: 10.1093/aje/kwp227. [DOI] [PubMed] [Google Scholar]
- 55.Anderson JL, May HT, Horne BD, et al. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am J Cardiol. 2010;106(7):963–968. doi: 10.1016/j.amjcard.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 56.Wang L, Manson JE, Song Y, et al. Systematic review: vitamin D and calcium supplementation in prevention of cardiovascular events. Ann Intern Med. 2010;152(5):315–323. doi: 10.7326/0003-4819-152-5-201003020-00010. [DOI] [PubMed] [Google Scholar]
- 57.Sonderman JS, Munro HM, Blot WJ, et al. Reproducibility of serum 25-hydroxyvitamin D and vitamin D-binding protein levels over time in a prospective cohort study of black and white adults. Am J Epidemiol. doi: 10.1093/aje/kws141. 2012;176(7):615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hofmann JN, Yu K, Horst RL, et al. Long-term variation in serum 25-hydroxyvitamin D concentration among participants in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. Cancer Epidemiol Biomarkers Prev. 2010;19(4):927–931. doi: 10.1158/1055-9965.EPI-09-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kotsopoulos J, Tworoger SS, Campos H, et al. Reproducibility of plasma and urine biomarkers among premenopausal and postmenopausal women from the Nurses’ Health Studies. Cancer Epidemiol Biomarkers Prev. 2010;19(4):938–946. doi: 10.1158/1055-9965.EPI-09-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]