Abstract
Dengue virus (DENV) causes dengue fever and dengue haemorrhagic fever/dengue shock syndrome, both considered major public-health problems worldwide. We generated a lethal DENV-2 strain (D220) by 10 additional cycles of subcutaneous inoculation of mice with supernatant from mosquito cells infected with the previously characterized strain D2S10, followed by harvesting of serum. D220 induces mortality at ten-fold lower doses than D2S10 in mice lacking only the alpha/beta interferon (IFN-α/β) receptor in C57BL/6 or 129 backgrounds under both non-enhanced and antibody-enhanced conditions. Sequence analysis of the complete viral genome revealed five amino acid changes between D220 and D2S10, of which two (K122I in envelope and V115A in NS4B) appear to account for the observed phenotypic differences between the viruses. By causing mortality at lower doses in C57BL/6 mice lacking only the IFN-α/β receptor, D220 constitutes an improved tool for study of DENV-induced pathogenesis, as well as for testing potential vaccines and antiviral drugs against DENV.
The four serotypes of dengue virus (DENV-1–4) are mosquito-borne and cause dengue fever (DF) and dengue haemorrhagic fever/dengue shock syndrome (DHF/DSS). Found in tropical and subtropical regions of the world, DENV causes an estimated 50–100 million infections annually and places over 3 billion people at risk of infection (WHO, 2009). Most primary DENV infections with any serotype are asymptomatic or lead to the self-limited febrile illness DF; however, secondary infection with a different DENV serotype leads to increased risk of developing severe dengue disease (Halstead, 2007). This increase in severity upon secondary infection is thought to be mediated in part via antibody-dependent enhancement (ADE), whereby interaction between antibodies generated during a prior infection and the current infecting serotype can lead to increased uptake of virus via Fc receptors expressed on susceptible myeloid cells (Halstead, 2003).
Establishing a small-animal model is an important step in understanding the mechanisms underlying dengue pathogenesis and immunity. The first mouse models used high doses of neurovirulent DENV strains delivered intracranially into immunocompetent mice; this caused neurotropic disease and paralysis in infected mice, which is typically not observed in human dengue (Raut et al., 1996; Schlesinger, 1977). One of the second-generation models used a neurotropic mouse-adapted DENV2 strain in mice of the 129/Sv mouse background deficient in alpha/beta interferon (IFN-α/β) and IFN-γ receptors (AG129 mice) (Johnson & Roehrig, 1999; Zompi & Harris, 2012). In more recent work, a peripherally adapted DENV-2 virus, designated D2S10, was generated by alternately passaging the Taiwanese DENV-2 isolate PL046 between Aedes albopictus C6/36 cells and AG129 mouse serum. The D2S10 virus was lethal in AG129 mice at 107 p.f.u. and induced a vascular leak phenotype mediated in part by tumour necrosis factor alpha (TNF-α) (Shresta et al., 2006), which is similar to observations in severe human dengue. D2S10 could also be lethally enhanced in AG129 mice by the passive transfer of sub-neutralizing levels of anti-DENV antibodies prior to infection with a sublethal dose (Balsitis et al., 2010; Zellweger et al., 2010). A triple-plaque-purified clone of the D2S10 strain, named S221, caused mortality in IFN-α/β receptor-deficient C57BL/6 (IFNAR−/−) mice at 1012 genome equivalents (approx. 3×107 p.f.u.) administered intravenously (i.v.) (Perry et al., 2009), and in IFN-α/β receptor-deficient 129/Sv (A129) mice at 1011 genome equivalents i.v. under antibody-enhanced conditions (Zellweger et al., 2010).
We wished to generate a DENV-2 strain capable of infecting and causing mortality at lower doses in less-immunocompromised mice under both non-enhanced and antibody-enhanced conditions. In order to generate a more lethal DENV-2 strain, we further passaged a tissue-culture-propagated derivative of D2S10 between A. albopictus C6/36 mosquito cells (obtained from the ATCC) and AG129 mice. In brief, serum from D2S10-infected AG129 mice was obtained 3.5 days post-infection (p.i.). Mouse-passaged virus from the serum was propagated in C6/36 cells for 7 days, concentrated via Amicon Centrifugal Filter units (100 kDa; Millipore) and injected subcutaneously into naïve AG129 mice. Ten such alternate passages were performed to derive strain D220. All experiments were performed according to the guidelines of the University of California Berkeley Animal Care and Use Committee to ensure humane treatment.
Subsequent infections were performed in mice deficient in only the IFN-α/β receptor, as they are less immunocompromised than AG129 mice and hence are considered to be a more relevant mouse model for dengue. Six- to eight-week-old IFNAR−/− or A129 mice were infected i.v. with 105, 106 or 107 p.f.u. of the parental D2S10 or the derived D220 virus and monitored at least until day 14 p.i. Infections with 105 p.f.u. were mostly sublethal for both viral strains. IFNAR−/− mice that received 106 or 107 p.f.u. D2S10 demonstrated 15 and 60 % mortality, respectively (Fig. 1a), whereas 60 and 100 % mortality was observed in mice that received 106 or 107 p.f.u. D220, respectively (Fig. 1b). Similar results were obtained for D220 in A129 mice (Fig. S1a, available in JGV Online). These observations indicate that D220 causes significantly greater mortality than D2S10 in IFNAR−/− mice as determined by log-rank (Mantel–Cox) test, when administered at the same dose (P = 0.046 for 106 p.f.u.; P = 0.045 for 107 p.f.u).
Fig. 1.
D220 causes mortality at a 10-fold lower dose than D2S10 in IFNAR−/− mice. Kaplan–Meier curves illustrate the susceptibility of IFNAR−/− mice to DENV2 strains D2S10 or D220. Mice were inoculated i.v. with several doses of (a) D2S10 or (b) D220 in C57BL/6 mice lacking the IFN-α/β receptor. Mice were monitored daily until day 14 p.i. In (c) and (d), mice were administered 10 µg anti-E mAb 4G2 intraperitoneally 24 h prior to infection with (c) D2S10 or (d) D220. The mean morbidity of mice receiving sublethal doses of (e) D2S10 or (f) D220 is plotted on a scale of 1–5, where 1 represents healthy and 5 represents moribund mice (see Table S1). The data in (a–d) were tested for statistical differences by log-rank (Mantel–Cox) test, comparing both viruses at the same dose and experimental condition, or comparing non-enhanced with ADE conditions. For (e) and (f), analysis was performed using the Mann–Whitney test. The data are derived from two or three independent experiments, and a total of n mice were plotted for each condition as indicated.
We next compared the virulence of D220 and D2S10 under ADE conditions. Ten micrograms of the anti-E mAb 4G2 (obtained from the ATCC) was administered intraperitoneally 24 h prior to infection, followed by infection with 104–107 p.f.u. D2S10 or 104–106 p.f.u. D220. Under enhancing conditions, infections with 104 or 105 p.f.u. D2S10 caused 0 and 20 % mortality in IFNAR−/− mice, respectively, while animals receiving higher doses (106–107 p.f.u.) displayed 100 % mortality by 4.5 days p.i. (Fig. 1c). In contrast, animals receiving 105 p.f.u. D220 under ADE conditions exhibited >90 % mortality (Fig. 1d). Again, similar results were obtained in A129 mice (Fig. S1b). Comparing ADE conditions for both viruses at the same dose, D220 led to significantly higher mortality than D2S10 at 105 p.f.u. (P = 0.0095) and 106 p.f.u. (P = 0.0027). Hence, under ADE conditions, D220 is more virulent than D2S10 at a 10-fold lower dose. Compared with infection of IFNAR−/− mice in the absence of antibody, prior administration of mAb 4G2 induced a highly significant increase in mortality after infection with D220 at 105 p.f.u. (P = 0.0006) and 106 p.f.u. (P = 0.0005). It is noteworthy that only very few mice developed paralysis after infection with either virus (8.1 % for D2S10 and 9.3 % for D220), which occurred on average on day 6.4 and no later than day 7 p.i.
We also assessed the mean morbidity observed in mice infected with different sublethal doses of D2S10 or D220, using a scoring system on a scale of 1–5 (Table S1). All infected animals, even at the lower sublethal doses of D2S10 and D220, exhibited some degree of morbidity (Fig. 1e, f). However, in mice that received equivalent doses of D220 or D2S10, D220 caused significantly greater morbidity than D2S10 under both non-enhanced (day 6, P = 0.0074) and antibody-enhanced (day 3, P = 0.0414; day 4, P = 0.0050; day 5, P = 0.0085; day 6, P = 0.0111; day 7, P = 0.0040) conditions, as determined via the Mann–Whitney test (Fig. 1e, f). The genome equivalent : p.f.u. ratios of D220 and D2S10 are very similar [6.8×103 for D2S10 and 5.7–6.8×103 for D220, as determined by quantitative (q)RT-PCR and plaquing on BHK-21 clone 15 cells]; thus, although mice were administered equivalent doses of virus in p.f.u., they received equivalent numbers of virions. In sum, our mortality and morbidity assays indicate that D220 is more virulent than D2S10 in mice lacking the IFN-α/β receptor.
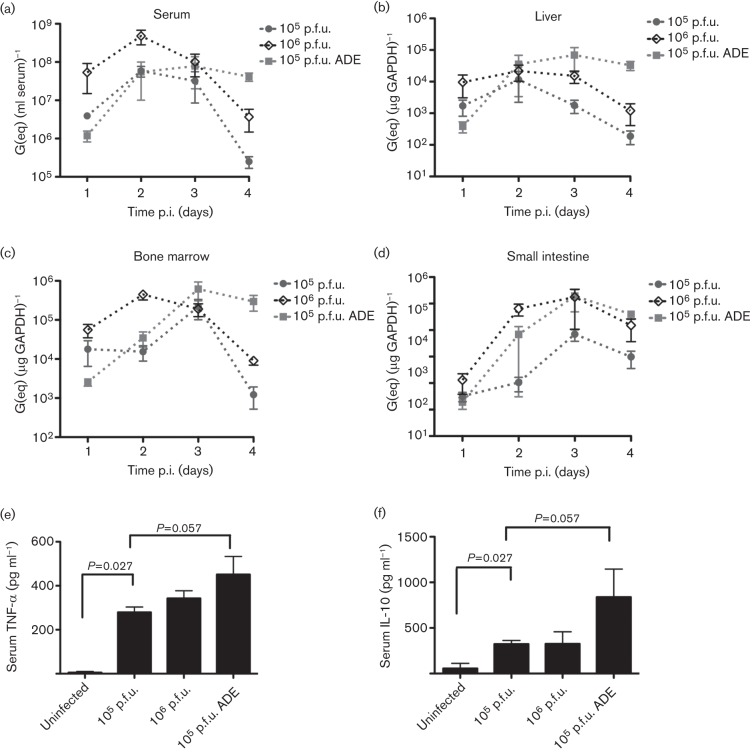
In order to characterize D220-induced DENV disease further, we measured the viral load in several tissues harvested from IFNAR−/− mice that were infected with 105 or 106 p.f.u. D220 alone, or 105 p.f.u. D220 under antibody-enhanced conditions. Animals infected with D220 were euthanized on days 1–4 p.i., and various organs were harvested and stored in RNAlater (Applied Biosystems) for quantification of virus. Bone marrow was flushed from the femur, and red blood cells were lysed. After washing twice with PBS, cells were counted, and a suspension of single cells was resuspended in RNAlater. Viral RNA was extracted with the RNEasy Mini kit (Qiagen) and measured by qRT-PCR as described previously (Houng et al., 2000). Viral load was assessed only until day 4 because substantial mortality was observed in mice beyond this time point, particularly at higher viral doses. Viral load in serum and liver was observed to peak at days 2–3 p.i. in all animals infected with D220 under both non-enhanced and antibody-enhanced conditions (Fig. 2a, b). However, by day 4 p.i., mice infected with D220 under ADE conditions had a significantly higher serum viraemia and viral load in the liver than mice infected with D220 in the absence of enhancing antibodies (P = 0.029) (Fig. 2a, b). Similar trends in viral load were also observed in the bone marrow, where D220-infected mice displayed higher viral loads at day 4 p.i. under ADE conditions compared with non-enhanced conditions (Fig. 2c). Viral load in the small intestine by day 4 p.i. was comparable between mice receiving 106 p.f.u. D220 and mice receiving 105 p.f.u. D220 under ADE conditions and lower in the mice receiving the sublethal 105 p.f.u. dose of D220 (Fig. 2d).
Fig. 2.
Mice receiving a sublethal dose of D220 under enhancing conditions have high tissue viral load and serum cytokines. (a–d) Viral titres of mice infected with D220 at days 1–4 p.i. IFNAR−/− mice in a C57BL/6 background were infected with 105 p.f.u. D220, 106 p.f.u. D220 or 105 p.f.u. D220 under enhancing conditions (10 µg 4G2 prior to infection). Mice were euthanized at the indicated time point, and viral load was determined by qRT-PCR as described in the text. Symbols indicate the mean value between individual mice (n = 3–5). (e, f) Serum TNF-α levels (e) and IL-10 levels (f) on day 4 p.i. as measured by ELISA.
We also measured serum levels of TNF-α and interleukin-10 (IL-10) in mice infected with D220. An increase in TNF-α levels during DENV infection has been linked to severe disease in humans (Hung et al., 2004; Pérez et al., 2004) and has also been observed in other relevant mouse models for dengue (Balsitis et al., 2010; Shresta et al., 2006; Wu-Hsieh et al., 2009; Zellweger et al., 2010). All mice infected with D220 showed a significant increase in serum TNF-α levels compared with uninfected animals (P = 0.027 for both 105 and 106 p.f.u. D220) on day 4 p.i., as detected using ELISA (eBioscience). Importantly, mice receiving 105 p.f.u. D220 under ADE conditions had the highest TNF-α levels, which is particularly evident in comparison with uninfected mice and mice that received 105 p.f.u. D220 (P = 0.047 and P = 0.057, respectively) (Fig. 2e). A similar pattern was also seen in serum IL-10 levels (Fig. 2f), where all infected mice had significantly higher IL-10 levels than uninfected mice, with the highest IL-10 levels observed in D220-infected mice under ADE conditions. Furthermore, all animals receiving lethal doses of D220 displayed fluid accumulation in organs within the abdominal cavity (data not shown), similar to AG129 mice infected with lethal doses of the parental strain D2S10 (Balsitis et al., 2010).
We next investigated whether genetic variations at the consensus level contributed to the observed differences in virulence between the D220 and D2S10 viruses. Viral RNA from D2S10 and D220 was reverse-transcribed, amplified in four overlapping segments (approx. 3.5 kb each) and sequenced using the 454/Roche pyrosequencing strategy at the Broad Institute using previously described methods (Lennon et al., 2010; Parameswaran et al., 2012) as part of the Genome Resources in Dengue Consortium project. Resulting sequence reads were assembled into a consensus using AV454 (Henn et al., 2012), and intra-host variants were called using the RV454 and V-Phaser (Macalalad et al., 2012) algorithms. All sequence changes were further confirmed using a targeted Sanger-based sequencing approach. The DENV genome encodes a polyprotein consisting of three structural (C, capsid; prM/M, pre-membrane; E, envelope) and seven non-structural (NS1, NS2A, NS2B, NS3, NS4A, NS4B, NS5) proteins. We identified differences between D2S10 and D220 in the consensus sequence at five distinct amino acid loci in the DENV2 genome: C-I106F, E-K122I, E-N124D, NS1-S228P and NS4B-V115A (Table 1). However, as mutations C-I106F, E-D124N and NS1-S228P were also present in other tissue-culture-propagated strains of D2S10 that behaved identically in vivo to the parental D2S10 (data not shown), we surmised that mutations E-K122I and/or NS4B-V115A are likely to be the genetic determinants of the observed increase in virulence.
Table 1. Loci that exhibit intra-host diversity in D2S10 and D220.
| Gene | Gene-specificposition | Consensusaa change (D2S10→D220)* | D2S10 | D220 | PL046 | ||
| Primary aa(r.a.)† | Secondaryaa (r.a.)† | Secondaryaa (r.a.)† | Primary aa(r.a.)† | Consensusaa | |||
| C | 106 | I→F | I (100) | – | – | F (100) | I |
| E | 122 | K→I | K (96.4) | I (3.6) | K (41.2) | I (58.8) | K |
| E | 124 | N→D | N (80.5) | D (14.9)S (1.8)G (1.4)I (1.4) | G (2.5) | D (97.5) | N |
| NS1 | 228 | S→P | S (86.6) | P (13.4) | – | P (100) | S |
| NS4B | 115 | V→A | V (100) | – | V (3.6) | A (96.4) | V |
| E | 70 | na | T (94.7) | I (5.3) | – | T (100) | T |
| E | 83 | na | N (92.6) | D (7.4) | – | N (100) | N |
| E | 228 | na | G (88.9) | E (11.1) | – | G (100) | G |
| E | 203 | na | N (100) | – | D (19.1) | N (80.9) | N |
| E | 247 | na | K (100) | – | R (6.6) | K (93.4) | K |
| prM | 139 | na | I (100) | – | V (6.1) | I (93.9) | I |
| NS4A | 34 | na | A (100) | – | V (5.6) | A (94.4) | A |
na, Variants do not contribute to changes in consensus sequence.
r.a., Relative abundance (%) of the most prevalent amino acid (i.e. ‘primary’) and the minor amino acid (i.e. ‘secondary’) in D220 and D2S10 isolates.
We also compared patterns of genome-wide intra-host diversity between the D220 and D2S10 virus strains. The genetic composition of intra-host viral populations has been postulated to impact viral fitness and disease pathogenesis in many RNA viruses, e.g. poliovirus (Vignuzzi et al., 2006). We observed that, at three of the five loci associated with consensus-level variation, the newly dominant amino acid in D220 appeared to arise from a pre-existing minor variant in D2S10 (E-122, NS1-228 and NS4B-115; Table 1). There were only seven other loci in the genome that exhibited contributions from minor alleles (Table 1). Most of these loci exhibited low levels of diversity (<7.5 %), with the exception of E-203 (19.1 %) in D220 and E-228 (11.1 %) in D2S10 (Table 1); any of these low-abundance variants could conceivably contribute to differences in virulence between D2S10 and D220. Interestingly, five of seven loci mapped to E, which is known to be highly antigenic in mice and humans.
Our sequence data indicate that mutations K122I (E) and V115A (NS4B) may contribute to the increased virulence in mice observed in infections with D220. Residue 122 in E maps to an exposed surface of domain II and is thought to interact with heparan sulfate proteoglycans (Prestwood et al., 2008). Interestingly, the mutations responsible for the increased virulence of D2S10 compared with its parental strain, PL046, are also located in this region of E (N124D, K128E) (Shresta et al., 2006; Prestwood et al., 2008). These mutations consist of alterations that reduce positive charge and weaken the affinity with heparan sulfate, leading to reduced clearance and increased viraemia (Prestwood et al., 2008). The K122I mutation in D220 also reduces positive charge in this region and may further decrease the affinity for heparan sulfate and increase the serum half-life of the virus. The V115A mutation in NS4B has been linked to an increase in DENV titres in mammalian cells and has been postulated to facilitate readaptation of several DENV serotypes to growth in these cells following culture in C6/36 mosquito cells (Blaney et al., 2003, 2004). This mutation also lies in a hydrophobic part of the protein that contributes to inhibition of IFN type I signalling (Muñoz-Jordán et al., 2005). We hypothesize that this mutation may enhance virus growth in the mouse host, perhaps by inhibiting innate immune pathways, and thus contribute to the increased virulence observed in infections with D220.
In summary, the mouse-adapted DENV-2 strain D220 is capable of causing morbidity and mortality in mice lacking only the IFN-α/β receptor under both non-enhanced and antibody-enhanced conditions at a ten-fold lower dose than its parental strain, D2S10. This is an improvement compared with previous models in which the D2S10 strain was used to infect AG129 mice, which lack IFN-α/β and -γ receptors. Also, as D220 can infect mice of the C57BL/6 background, infections in other immunologically relevant knockouts available in this background may be used to investigate the mechanisms of DENV disease pathogenesis and/or immunity. Thus, D220 is an improved tool for studying DENV infection and disease in vivo, and for testing potential vaccines and antiviral compounds against DENV under antibody-enhanced and non-enhanced conditions.
Acknowledgements
We would like to thank Kate Williams for technical advice and the Broad Institute’s Genome Sequencing and Biological Samples Platforms for their effort to generate genomic data. This project was funded with Federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under grant nos R01AI085607 (E. H.), U54AI065359 (E. H.) and U54AI065359 Career Development subaward (P. P.), and contract no. HHSN272200900018C (awarded to B. W. Birren).
Footnotes
A supplementary figure and table are available with the online version of this paper.
References
- Balsitis S. J., Williams K. L., Lachica R., Flores D., Kyle J. L., Mehlhop E., Johnson S., Diamond M. S., Beatty P. R., Harris E. (2010). Lethal antibody enhancement of dengue disease in mice is prevented by Fc modification. PLoS Pathog 6, e1000790 10.1371/journal.ppat.1000790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaney J. E., Jr, Manipon G. G., Firestone C. Y., Johnson D. H., Hanson C. T., Murphy B. R., Whitehead S. S. (2003). Mutations which enhance the replication of dengue virus type 4 and an antigenic chimeric dengue virus type 2/4 vaccine candidate in Vero cells. Vaccine 21, 4317–4327 10.1016/S0264-410X(03)00487-0 [DOI] [PubMed] [Google Scholar]
- Blaney J. E., Jr, Hanson C. T., Firestone C. Y., Hanley K. A., Murphy B. R., Whitehead S. S. (2004). Genetically modified, live attenuated dengue virus type 3 vaccine candidates. Am J Trop Med Hyg 71, 811–821 [PubMed] [Google Scholar]
- Halstead S. B. (2003). Neutralization and antibody-dependent enhancement of dengue viruses. Adv Virus Res 60, 421–467 10.1016/S0065-3527(03)60011-4 [DOI] [PubMed] [Google Scholar]
- Halstead S. B. (2007). Dengue. Lancet 370, 1644–1652 10.1016/S0140-6736(07)61687-0 [DOI] [PubMed] [Google Scholar]
- Henn M. R., Boutwell C. L., Charlebois P., Lennon N. J., Power K. A., Macalalad A. R., Berlin A. M., Malboeuf C. M., Ryan E. M. & other authors (2012). Whole genome deep sequencing of HIV-1 reveals the impact of early minor variants upon immune recognition during acute infection. PLoS Pathog 8, e1002529 10.1371/journal.ppat.1002529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houng H. H., Hritz D., Kanesa-thasan N. (2000). Quantitative detection of dengue 2 virus using fluorogenic RT-PCR based on 3′-noncoding sequence. J Virol Methods 86, 1–11 10.1016/S0166-0934(99)00166-4 [DOI] [PubMed] [Google Scholar]
- Hung N. T., Lei H.-Y., Lan N. T., Lin Y.-S., Huang K.-J., Lien L. B., Lin C.-F., Yeh T.-M., Ha D. Q. & other authors (2004). Dengue hemorrhagic fever in infants: a study of clinical and cytokine profiles. J Infect Dis 189, 221–232 10.1086/380762 [DOI] [PubMed] [Google Scholar]
- Johnson A. J., Roehrig J. T. (1999). New mouse model for dengue virus vaccine testing. J Virol 73, 783–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennon N. J., Lintner R. E., Anderson S., Alvarez P., Barry A., Brockman W., Daza R., Erlich R. L., Giannoukos G. & other authors (2010). A scalable, fully automated process for construction of sequence-ready barcoded libraries for 454. Genome Biol 11, R15 10.1186/gb-2010-11-2-r15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macalalad A. R., Zody M. C., Charlebois P., Lennon N. J., Newman R. M., Malboeuf C. M., Ryan E. M., Boutwell C. L., Power K. A. & other authors (2012). Highly sensitive and specific detection of rare variants in mixed viral populations from massively parallel sequence data. PLOS Comput Biol 8, e1002417 10.1371/journal.pcbi.1002417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz-Jordán J. L., Laurent-Rolle M., Ashour J., Martínez-Sobrido L., Ashok M., Lipkin W. I., García-Sastre A. (2005). Inhibition of alpha/beta interferon signaling by the NS4B protein of flaviviruses. J Virol 79, 8004–8013 10.1128/JVI.79.13.8004-8013.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parameswaran P., Charlebois P., Tellez Y., Nunez A., Ryan E. M., Malboeuf C. M., Levin J. Z., Lennon N. J., Balmaseda A. & other authors (2012). Genome-wide patterns of intra-human dengue virus diversity reveal associations with viral phylogenetic clade and inter-host diversity. J Virol. (In press) 10.1128/JVI.00736-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez A. B., García G., Sierra B., Alvarez M., Vázquez S., Cabrera M. V., Rodríguez R., Rosario D., Martínez E. & other authors (2004). IL-10 levels in Dengue patients: some findings from the exceptional epidemiological conditions in Cuba. J Med Virol 73, 230–234 10.1002/jmv.20080 [DOI] [PubMed] [Google Scholar]
- Perry S. T., Prestwood T. R., Lada S. M., Benedict C. A., Shresta S. (2009). Cardif-mediated signaling controls the initial innate response to dengue virus in vivo. J Virol 83, 8276–8281 10.1128/JVI.00365-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestwood T. R., Prigozhin D. M., Sharar K. L., Zellweger R. M., Shresta S. (2008). A mouse-passaged dengue virus strain with reduced affinity for heparan sulfate causes severe disease in mice by establishing increased systemic viral loads. J Virol 82, 8411–8421 10.1128/JVI.00611-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raut C. G., Deolankar R. P., Kolhapure R. M., Goverdhan M. K. (1996). Susceptibility of laboratory-bred rodents to the experimental infection with dengue virus type 2. Acta Virol 40, 143–146 [PubMed] [Google Scholar]
- Schlesinger R. W. (1977). Dengue viruses. Virol Monogr 16, 1–132 [DOI] [PubMed] [Google Scholar]
- Shresta S., Sharar K. L., Prigozhin D. M., Beatty P. R., Harris E. (2006). Murine model for dengue virus-induced lethal disease with increased vascular permeability. J Virol 80, 10208–10217 10.1128/JVI.00062-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vignuzzi M., Stone J. K., Arnold J. J., Cameron C. E., Andino R. (2006). Quasispecies diversity determines pathogenesis through cooperative interactions in a viral population. Nature 439, 344–348 10.1038/nature04388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2009). Dengue: Guidelines for Diagnosis, Treatment, Prevention, and Control. Geneva: World Health Organization; [PubMed] [Google Scholar]
- Wu-Hsieh B. A., Yen Y. T., Chen H. C. (2009). Dengue hemorrhage in a mouse model. Ann N Y Acad Sci 1171 (Suppl. 1), E42–E47 10.1111/j.1749-6632.2009.05053.x [DOI] [PubMed] [Google Scholar]
- Zellweger R. M., Prestwood T. R., Shresta S. (2010). Enhanced infection of liver sinusoidal endothelial cells in a mouse model of antibody-induced severe dengue disease. Cell Host Microbe 7, 128–139 10.1016/j.chom.2010.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zompi S., Harris E. (2012). Animal models of dengue virus infection. Viruses 4, 62–82 10.3390/v4010062 [DOI] [PMC free article] [PubMed] [Google Scholar]