Abstract
Used together, sitagliptin (Januvia) and metformin (Glucophage) help to improve glycemic levels in diabetic patients, suggesting a synergy between the agents. However, the cost of sitagliptin and the need for more data may restrict its use. More studies are needed to assess the effects of long-term sitagliptin and to determine its role in combination therapy.
INTRODUCTION
Of the 25.8 million Americans with type-2 diabetes mellitus, 7 million of these individuals are unaware that they have the disease. Medical costs are 2.3 times higher in patients with diabetes, with health care expenditures exceeding $174 billion annually.1 Complications include kidney failure, nontraumatic lower-extremity amputation, blindness, heart disease, and stroke. Type-2 diabetes is the seventh leading cause of death in the U.S.
Rather than recommending a specific hemoglobin A1c (HbA1c) goal for all patients, the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) recommend individualized treatment targets for each patient.2 Lifestyle changes, including weight loss and increased physical activity, can reduce blood glucose levels; however, the utility of such interventions is limited, and most patients need to begin pharmacotherapy.3
Metformin (Glucophage, Bristol-Myers Squibb) is recommended in all patients at diagnosis unless contraindications exist.2 Despite the proven efficacy of metformin, blood glucose often remains uncontrolled with monotherapy.2 Outcomes with additional agents are not consistent and depend on multiple factors, including adherence to therapy, cost, adverse effects, and comorbid conditions.
Combination therapy with a dipeptidyl peptidase-4 (DPP-4) inhibitor, such as sitagliptin (Januvia, Merck), may be considered, especially as evidence of its safety and efficacy has become available. In February 2012, Merck announced the approval of a once-daily formulation of a sitagliptin/metformin combination (Janumet XR).4 This dosage form allows for diabetes treatment with multiple modes of action while affording patients the convenience of once-daily administration.
PHARMACOLOGY AND MODE OF ACTION
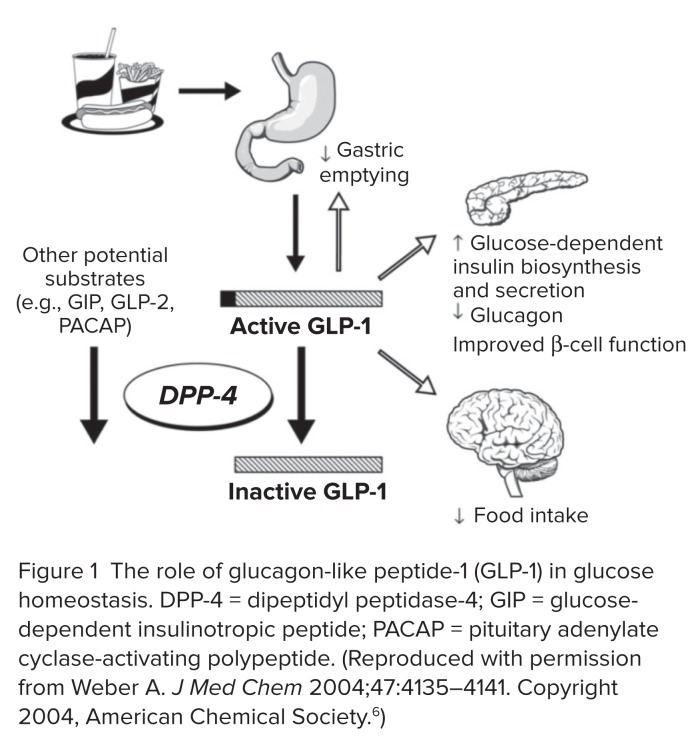
In order to appreciate the mechanism associated with the DPP-4 inhibitors, we must understand the normal function of incretin hormones. Creutzfeldt first described the incretins in 1979.5 Incretin hormones are released from the gut in response to nutrient consumption, and they cause insulin release in a glucose-dependent manner. Glucagon-like peptide-1 (GLP-1) is one hormone that meets these criteria. GLP-1 is involved in glucose homeostasis via stimulation of insulin biosynthesis and secretion as well as inhibition of glucagon release. GLP-1 also improves satiety, slows gastric emptying, and may be associated with improved beta-cell function (Figure 1).6 However, GLP-1 is quickly inactivated by DPP-4, which is present in the kidneys, intestines, and bone marrow. Lower concentrations of GLP-1 are also found in the liver, pancreas, placenta, thymus, spleen, epithelial cells, vascular endothelium, and lymphoid and myeloid cells.7
Figure 1.
The role of glucagon-like peptide-1 (GLP-1) in glucose homeostasis. DPP-4 = dipeptidyl peptidase-4; GIP = glucose-dependent insulinotropic peptide; PACAP = pituitary adenylate cyclase-activating polypeptide. (Reproduced with permission from Weber A. J Med Chem 2004;47:4135–4141. Copyright 2004, American Chemical Society.6)
A clinical trial was conducted to examine whether patients with type-2 diabetes had reduced concentrations of intact GLP-1.8 In a study of 12 diabetic subjects and 12 healthy patients, a postprandial blood sample was collected at 15, 30, 45, 60, 75, 90, 120, 150, and 180 minutes. After meal ingestion, GLP-1 concentrations were lower in the diabetic patients at 75, 90, and 120 minutes (P = 0.056, 0.017, and 0.017, respectively). Dramatic differences in intact GLP-1 levels were observed. Healthy patients had an enhanced, prolonged response, with a peak concentration observed at 90 to 120 minutes. Conversely, GLP-1 levels peaked at around 30 minutes in the diabetic group but decreased to preprandial levels between 75 and 120 minutes.
Therefore, in the late phase of meal response, diabetic patients may have impaired secretion of GLP-1. C-peptide levels and insulin levels were also reduced in the study group. On the basis of these results, the investigators concluded that patients with type-2 diabetes do not have intact GLP-1, which may play a role in the inadequate insulin response.
More recently, Nauck et al. reported that GLP-1 concentrations might not be reduced in patients with type-2 diabetes.9 Factors such as age, obesity, degree of insulin resistance, and fasting glucagon levels may be responsible for the varied response identified in clinical trials. In addition, metformin, by an unknown mechanism, may enhance GLP-1 response. Theoretically, numerous factors may determine GLP-1 secretion and response to DPP-4 inhibition.
Sitagliptin
Sitagliptin is a potent, highly selective oral DPP-4 inhibitor. Inhibition of similar enzymes, DPP-8 and DPP-9, have led to serious toxicities, which emphasizes the importance of prescribing a highly selective agent.10 Sitagliptin has an oral bioavailability of 87% and a terminal half-life of 10 to 12 hours. During clinical trials, the mean time to maximum concentration (Tmax) in plasma was 1 to 6 hours and varied across the dosing range. Half-life and Tmax were not significantly altered after administration of food.
Sitagliptin is excreted primarily by the urinary system as the unchanged parent molecule; therefore, a decreased dose is warranted in the presence of renal dysfunction.11 Sitagliptin is a minor substrate for the cytochrome P450 system, and drug interactions are limited to concomitant use with digoxin.12
Metformin
The primary mechanism by which metformin lowers glucose levels is the reduction of excessive rates of hepatic glucose production. Metformin increases hepatic sensitivity to insulin and decreases hepatic extraction of gluconeogenic substrates (lactate), thereby decreasing gluconeogenesis.13 In addition, glucose uptake in the skeletal muscle is increased, whereas glycogenolysis is reduced.
Metformin has the potential to induce mild anorexia, which may facilitate glycemic control. The drug is eliminated by renal tubular secretion, and it has a plasma elimination half-life of approximately 6.2 hours. Drug interactions with cimetidine (Tagamet, GlaxoSmithKline) have been observed in clinical trials. Theoretically, cationic drugs (e.g., morphine, digoxin, triamterene, and trimethoprim) have the potential to interact with metformin because they are eliminated renally via tubular secretion.14 Extensive clinical research, coupled with favorable results from the landmark United Kingdom Prospective Diabetes Study, has helped to make metformin a front-runner in the treatment of diabetes.2,15
CLINICAL TRIALS
Sitagliptin Plus Metformin Versus Monotherapies (Table 1)
Table 1.
Sitagliptin Plus Metformin vs. Monotherapies
| Findings | ||||||||
|---|---|---|---|---|---|---|---|---|
| Reference | No.a | Design | Specific Aim | Treatment | HbA1c | Hypoglycemia | Adverse Events | Other Findings |
| Brazg16 | 28 | DB, R, PC, 2-period CO | Efficacy | Both groups: Met Group 1: PBO (4 weeks), then Sit 100 mg q.d. (4 weeks) Group 2: Sit 100 mg q.d. (4 weeks), then PBO (4 weeks) |
NA | 0% | No significant differences between groups | (Periods 1 and 2 combined) Sit + Met WMG 130.5 FPG ⬇ 23.1 PBO + Met WMG 148.4 FPG ⬇ 7.7 |
| Williams-Herman17 | 517 | E, R, DB, F | Efficacy and Safety | Sit 50 mg b.i.d. + met 1,000 mg b.i.d. or Sit 50 mg b.i.d. + met 500 mg b.i.d. or Met 1,000 mg b.i.d. or Met 500 mg b.i.d. or Sit 100 mg q.d. |
⬇ 1.7% ⬇1.4% ⬇1.3% ⬇1.1% ⬇1.2% |
4.9% 2.6% 2.2% 1.6% 1.1% |
GI 33% GI 29.5% GI 33% GI 20.9% GI 20.7% |
|
| Reasner18 | 1250 | DB, R, PG | Efficacy and Safety | Sit 50 mg + met 500 mg b.i.d. → Sit 50 mg + met 1,000 mg b.i.d. or Met 500 mg b.i.d. → Met 1,000 mg b.i.d. |
⬇2.4% ⬇1.8% |
2.1% 1.8% |
AP 1.1% D 12% AP 3.9% (P < 0.05) D 16.6% (P < 0.05) |
FPG: ⬇ 68.4 FPG: ⬇ 54 |
| Goldstein19 | 1091 | R, DB, PC, PG | Efficacy and Safety | Sit 50 mg + met 1,000 mg b.i.d. or Sit 50 mg + met 500 mg b.i.d. or Met 1,000 mg b.i.d. or Met 500 mg b.i.d. or Sit 100 mg q.d. or PBO |
⬇1.90 ⬇1.40 ⬇1.13 ⬇0.66 ⬇0.82 ⬇0.17 |
2.2% 1.1% 1.1% 0.5% 0.6% 0.6% |
GI 24.7% GI 17.9% GI 25.3% GI 15.9% GI 15.1% GI 10.8% |
|
| Charbonnel20 | 701 | MN, R, PG, PC, DB | Efficacy and Safety | Ongoing Met ≥ 1,500 mg q.d. + PBO or Ongoing Met ≥ 1,500 mg q.d. + Sit 100 mg q.d. |
⬇0.02 ⬇0.67 |
2.1% 1.3% |
No significant differences between groups | FPG: ⬆ 9 mg/dL FPG: ⬇ 16.2 mg/dL |
| Perez-Monteverde21 | Phase A1 492 Phase B2 455 |
R, DB | Efficacy and Safety | Phase A Sit 100 mg q.d. Pio 15 mg q.d. Phase B Met 1,000 mg + Sit 50 mg b.i.d. Pio 45 mg q.d. |
Phase A Sit: ⬇ 1% Pio: ⬇ 0.9% Phase B Met/Sit: ⬇ 1.7% Pio: ⬇ 1.4% |
Sit/Met 2.3% Pio 2.2% |
Edema Sit/Met 0.9% Pio 6.1% ALT Sit/Met 2.7% Pio 0% |
Met/Sit: −1.1 kg in weight Pio: +3.4 kg in weight |
| Raz22 | 190 | MN, R, PC, PG, DB | Efficacy and Safety | Met > 1,500 mg q.d. + PBO or Met > 1,500 mg q.d. + Sit 100 mg q.d. |
0⬇1 (P < 0.001) | 0% 1% |
⬆ Pharyngitis in placebo arm ⬆ RTI in placebo arm ⬆ Hyperglycemia in placebo arm |
|
ALT = alanine aminotransferase; AP = abdominal pain; b.i.d. = twice daily; CO = crossover; D = diarrhea; DB = double-blind; E = extension; F = factorial; FPG = fasting plasma glucose; GI = gastrointestinal; HbA1c = glycosylated hemoglobin; Met = metformin; MN = multinational; NA = not available; PBO = placebo; PC = placebo-controlled; PG = parallel group; Pio = pioglitazone; q.d. = daily; R = randomized; RTI = respiratory tract infection; Sit = sitagliptin; WMG = weighted mean glucose.
Evaluable patients.
Two-phase study: phase A (12 weeks).
Two-phase study: phase B (28 weeks).
Brazg et al.16
A randomized, double-blind, placebo-controlled, two-period crossover study was one of the first to evaluate the combination of sitagliptin and metformin. A total of 28 type-2 diabetic patients with uncontrolled glucose levels who were currently receiving metformin monotherapy had baseline HbA1c levels of 6.5% to 9.6%. These patients were randomly assigned to one of two treatment groups: metformin plus placebo for 4 weeks, followed by sitagliptin 50 mg twice daily for 4 weeks or metformin plus sitagliptin for 4 weeks, followed by placebo for 4 weeks.
Patients receiving sitagliptin in either setting showed a significant reduction in 24-hour weighted mean glucose levels compared with those receiving placebo (–49.7 mg/dL vs. −16.0 mg/dL, respectively; P < 0.001) following each 4-week treatment period. Sitagliptin/metformin also resulted in a greater reduction in fasting plasma glucose (FPG) levels when compared with placebo (–31.1 mg/dL vs. −9.6 mg/dL, respectively; P < 0.001).
Patients reported no hypoglycemia, no significant weight fluctuations, and a similar incidence of gastrointestinal (GI)-related adverse effects. Overall, when added to metformin therapy, sitagliptin significantly lowered 24-hour weighted mean glucose, thereby improving 24-hour glycemic control. Therapy was generally well tolerated.
Williams-Herman et al.17
In a long-term randomized, double-blind, factorial trial, the efficacy and safety of sitagliptin/metformin were assessed in type-2 diabetes patients with inadequately controlled blood glucose levels. The objective was to compare this combination with metformin alone. HbA1c levels ranged from 7.5% to 11% with diet and exercise alone.
In this study, 788 patients completed the first 54 weeks and 517 patients continued through the 50-week extension study to complete a total of 104 weeks. The baseline HbA1c value was 8.7%. Patients received one of the following treatments:
sitagliptin 50 mg twice daily plus metformin 1,000 mg twice daily
sitagliptin 50 mg twice daily plus metformin 500 mg twice daily
metformin 1,000 mg twice daily
metformin 500 mg twice daily
sitagliptin 100 mg daily
placebo (from weeks 1 to 24)
Patients who had initially received placebo were switched to metformin 1,000 mg twice daily at week 24.
Throughout the study, significant reductions in HbA1c from baseline were observed for the treatment groups, with the greatest decreases occurring in patients with the higher baseline HbA1c levels. Average changes in HbA1c from baseline to week 104 were as follows: −1.7% with sitagliptin 50 mg twice daily plus metformin 1,000 mg twice daily; −1.4% with sitagliptin 50 mg twice daily plus metformin 500 mg twice daily; −1.3% with metformin 1,000 mg twice daily; −1.1% with metformin 500 mg twice daily; and −1.2% with sitagliptin 100 mg daily.
The reduction in HbA1c was greater with high-dose sitagliptin/metformin than with either drug alone. In addition, patients receiving the higher-dose combination were more likely to achieve an HbA1c of less than 7% by week 104. The adverse-effect profile was generally the same for metformin monotherapy and sitagliptin/metformin.
Reasner et al.18
A 44-week study was conducted to compare the efficacy and safety of sitagliptin/metformin with metformin monotherapy in treatment-naive patients with type-2 diabetes. HbA1c levels were 7.5% or higher (mean HbA1c, 9.9%) with diet and exercise. In this double-blind, randomized, parallel-group study, 1,250 drug-naive patients initially received either sitagliptin/metformin 50/500 mg twice daily or metformin 500 mg twice daily. Doses were titrated upward every 2 weeks to a goal of sitagliptin/metformin 50/1,000 mg twice daily or metformin 1,000 mg twice daily.
The primary endpoint was the change in HbA1c from baseline to week 18. The largest decrease in HbA1c was seen in the first 12 weeks of therapy, and a further decrease was seen in the subsequent 6 weeks. At the earliest measurement and at every examination thereafter, reductions in HbA1c were greatest with sitagliptin/metformin compared with metformin alone. The mean change in HbA1c from baseline to week 18 was −2.4% with sitagliptin/metformin and −1.8% with metformin alone (P < 0.001).
At week 18, reductions in HbA1c from baseline in both treatment groups were greater in patients with a higher baseline HbA1c. A greater proportion of patients receiving the sitagliptin/metformin combination had HbA1c levels below 7% or below 6.5% compared with those receiving metformin monotherapy (49.2% vs. 34.2% and 31.8% vs. 16%, respectively; P < 0.001). Improvements in FPG were significantly greater in the combination group (–68.5 mg/dL vs. −54 mg/dL, respectively; P < 0.001).
Reductions in body weight and lipid levels were similar among treatment groups. The potential risk for increased adverse effects with sitagliptin/metformin therapy is a concern; however, in this study, both the combination and metformin monotherapy groups experienced similar incidences of adverse effects, except for some GI intolerance. Significantly lower rates of abdominal pain and diarrhea were observed with sitagliptin/metformin than with metformin monotherapy. Both treatment arms received additional antihyperglycemic agents as indicated.
It was expected that the metformin monotherapy group would receive more antihyperglycemic agents; however, utilization of these agents was low despite elevated HbA1c levels. Overall, initial combination therapy with sitagliptin/metformin resulted in greater reductions of HbA1c and FPG levels, possibly aiding in attaining target HbA1c more quickly than metformin alone.
Goldstein et al.19
The safety and efficacy of initial sitagliptin/metformin therapy were explored in a 24-week study that enrolled patients who had inadequately controlled glucose levels and had been treated with diet and exercise only. In this double-blind, placebo-controlled, parallel-group study, 906 patients received one of the following regimens:
sitagliptin 100 mg daily
metformin 500 mg twice daily
metformin 1,000 mg twice daily
sitagliptin 50 mg twice daily plus metformin 500 mg twice daily
sitagliptin 50 mg twice daily plus metformin 1,000 mg twice daily
placebo
The mean HbA1c level was 8.8% (range, 6.3%–11.9%). All patients receiving active treatment experienced significant reductions in HbA1c and FPG levels from baseline to week 24. The placebo-subtracted HbA1c change from baseline was −0.83% with sitagliptin 100 mg daily; −0.99% with metformin 500 mg twice daily; −1.30% with metformin 1,000 mg twice daily; −1.57% with sitagliptin 50 mg twice daily plus metformin 500 mg twice daily; and −2.07% with sitagliptin 50 mg twice daily + metformin 1,000 mg twice daily (P < 0.01 for the comparison groups vs. placebo and for combination groups vs. monotherapy groups).
Patients receiving active treatment were also significantly more likely to achieve an HbA1c of below 7% (P < 0.001) and below 6.5% (P < 0.005) compared with patients receiving placebo.
While not statistically significant, the overall incidence of non-hypoglycemic adverse effects varied only slightly among study groups, with the lowest incidence in the placebo group (50.6%) and the highest incidence in the metformin 1,000-mg twice-daily group (62.1%).
The incidence of hypoglycemia was similar between the study groups (range, 0.5%–2.2%). The sitagliptin/metformin therapies provided additive glucose lowering with only a moderate change in adverse effects.
Charbonnel et al.20
A 24-week randomized, double-blind, parallel-group trial enrolled 701 patients to assess the safety and efficacy of adding sitagliptin to ongoing metformin therapy. Patients received either sitagliptin 100 mg daily or placebo in addition to metformin. Compared with placebo, sitagliptin significantly reduced HbA1c values by 0.65% (P < 0.001) and FPG levels by 25.4 mg/dL (P < 0.001).
Significantly more patients taking sitagliptin/metformin also achieved HbA1c levels below 7% compared with those receiving placebo (47% vs. 18.3%, respectively; P < 0.001). The incidence of GI adverse events, hypoglycemia, and changes in body weight were similar among the groups. Based on these results, the authors confirmed that the addition of sitagliptin 100 mg daily was safe and effective when added to metformin therapy.
Perez-Monteverde et al.21
A randomized study enrolling patients with an HbA1c of 7.5% to 12% (mean HbA1c, 9%) was conducted to compare sitagliptin monotherapy with sitagliptin/metformin versus pioglitazone (Actos, Eli Lilly) monotherapy. Following a 2-week run-in phase, patients received sitagliptin 100 mg daily or pioglitazone 15 mg daily (titrated upward to 30 mg daily after 6 weeks). Following the initial 12-week period, patients began a second phase of the trial for an additional 28 weeks. Patients who had originally received sitagliptin were switched to sitagliptin/metformin, with the dose titrated to 50/1,000 mg twice daily. The dose of pioglitazone was titrated to 45 mg daily. In the first phase of the trial, changes in HbA1c were similar between the sitagliptin groups (–1.0%) and the pioglitazone groups (–0.9%).
At the end of the 40-week trial, patients receiving sitagliptin/metformin experienced significantly greater changes in HbA1c (–1.7%) compared with baseline than those receiving pioglitazone (–1.4%) (P < 0.05). A greater percentage of patients receiving sitagliptin/metformin were also likely to achieve HbA1c values below 7% and below 6.5% (55%) compared with those receiving pioglitazone (31.2%) (P < 0.05).
Although the incidence of adverse events was similar between groups, the number of drug-related adverse events was higher in the pioglitazone group. These patients were more likely to experience edema (6.1% vs. 0.9%, respectively; P < 0.05) and weight gain (1.6% vs. 0%, respectively) than those in the sitagliptin/metformin group. The frequency of hypoglycemia was low in both treatment groups.
In summary, both sitagliptin and pioglitazone monotherapies produced clinically significant reductions in HbA1c; however, combination sitagliptin/metformin therapy resulted in significantly greater HbA1c reductions than pioglitazone.
Raz et al.22
In a 30-week randomized trial, 159 patients were evaluated to determine the efficacy and safety of sitagliptin when added to metformin monotherapy. HbA1c values ranged from 8% to 11%. All patients received metformin for the first phase of the trial. Following the run-in period, patients who complied adequately with treatment and whose FPG levels were between 130 and 280 mg/dL received either sitagliptin 100 mg daily or placebo for 30 weeks in addition to their ongoing metformin dose. During the 30 weeks, glipizide (Glucotrol, Pfizer) was administered as rescue therapy as needed.
Primary and secondary endpoints were any changes in baseline HbA1c after 18 and 30 weeks of combination treatment, respectively. At the end of the initial metformin monotherapy period, mean HbA1c was 9.2% and FPG was 200 mg/dL. After the addition of sitagliptin or placebo to metformin therapy, sitagliptin patients at week 18 had significantly lower HbA1c values compared with patients receiving placebo (P < 0.001).
Patients receiving sitagliptin were more likely to achieve their HbA1c goal of less than 7% at both week 18 and week 30 (P = 0.012 and P < 0.001, respectively). Over the 30-week study period, the addition of sitagliptin to metformin therapy was generally well tolerated compared with placebo.
Adverse events were similar between groups, including hypoglycemia, which affected none of the patients in the placebo arm and one patient in the sitagliptin arm. There were no meaningful differences in body weight changes in either group. Overall, sitagliptin provided a significant reduction in HbA1c compared with placebo, and there were no major differences in the incidence of weight changes or hypoglycemic events.
Sitagliptin Plus Metformin vs. Other Agents Plus Metformin (Table 2)
Table 2.
Clinical Trials of Sitagliptin Plus Metformin vs. Other Agents Plus Metformin
| Findings | Findings | |||||||
|---|---|---|---|---|---|---|---|---|
| Reference | No.a | Design | Specific Aim | Treatment | HbA1c | Hypoglycemia | Adverse Events | Other Findings |
| ADA23 | 544 | R, DB, PC,1 AC2 | Efficacy and Safety | Phase A: Met + PBO Met + Sit 100 mg Phase B: Met + Sit or Met + Glip 5 mg/day (up to 15 mg/day) Both groups: Met ≥ 1,500 mg/day |
Sit: ⬇ 0.7% Glip: ⬇ 0.9% |
Sit: 1.7% Glip: 13% |
⬆ Incidence of GI complaints in Sit arm (N/V/D/abdominal pain) | Sit: −0.9 kg in weight Glip: +1.5 kg in weight |
| Nauck24 | 793 | R, PG, AC, DB, non-inferiority | Efficacy and Safety | Sit 100 mg q.d. Glip 5 mg/day (up to 20 mg/day) Both groups: Met ≥ 1,500 mg/day |
Sit: ⬇ 0.51% Glip: ⬇ 0.56% |
Sit: 5% Glip: 32% |
⬆Fatigue with Sit (3.1 vs. 0.9%)⬆ dizziness with Sit (3.7 vs. 2.1%) | Sit : −1.5 kg in weight Glip: +1.1 kg in weight |
| Scott25 | 273 | R, DB, PC, PG | Efficacy and Safety | Sit 100 mg q.d. or Rosi 8 mg or PBO Both groups: Met ≥ 1,500 mg/day |
Sit: ⬇ 0.51% Rosi: ⬇ 0.57% |
Sit: 1% Rosi: 1% PBO: 2% |
Edema Sit: 1% Rosi: 4% PBO: 1% |
Sit: −0.4 kg in weight Rosi: +1.5 kg in weight |
| Scheen26 | 739 | R, DB, non-inferiority | Efficacy and Safety | Sit 100 mg q.d. or Sax 5 mg Both groups: Met 1,500–3,000 mg/day |
Sit: ⬇ 0.62% Sax: ⬇ 0.52% |
— | — | Most common AE in both groups: influenza, UTI, nasopharyngitis |
| Bergenstal27 | 491 | R, DB | Efficacy and Safety | Exen 2 mg/week + PBO Sit 100 mg q.d. + PBO Pio 45 mg q.d. + PBO Both groups: Met 1,500–2,000 mg/day |
Exen: ⬇ 1.5% Sit: ⬇ 0.9% Pio: ⬇ 1.2% |
Exen: 1% Sit: 3% Pio: 1% |
N/D Exen 24%, 18% Sit 16%, 10% Edema/URI Pio 8%, 10% |
Exen: −2.3 kg in weight Sit: −0.8 kg in weight Pio: +2.8 kg in weight |
AC = active-controlled; AE = adverse events; D = diarrhea; DB = double-blind; Exen = exenatide; GI = gastrointestinal; Glip = glipizide; HbA1c = glycosylated hemoglobin; Met = metformin; N = nausea; PBO = placebo; PC = placebo-controlled; PG = parallel group; Pio = pioglitazone; q.d. = daily; R = randomized; Rosi = rosiglitazone; Sax = saxagliptin; Sit = sitagliptin; URI = upper respiratory infection; UTI = urinary tract infection; V = vomiting.
Evaluable patients.
Two-phase study: phase A (24 weeks).
Two-phase study: phase B (30 weeks).
American Diabetes Association23
A follow-up study to the trial by Charbonnel et al.20 was conducted to compare sitagliptin/metformin with glipizide/metformin. Of the 701 patients initially randomized, 544 completed the extension trial. Patients originally assigned to receive placebo were switched to glipizide 5 mg daily (titrated to 15 mg daily) for 30 weeks.
At the completion of the study, changes in HbA1c from baseline in the sitagliptin group were −0.7% and −0.9% in the glipizide group (P value not reported). Hypoglycemia was reported more often in the glipizide group (16% vs. 1%, respectively; P value not reported). Changes in body weight were −0.9 kg with sitagliptin and +1.5 kg with glipizide.
Nauck et al.24
The efficacy and safety of sitagliptin versus glipizide were studied in a year-long trial involving 793 patients with inadequate glucose control with metformin monotherapy. Mean HbA1c value was 7.7% (range, 6.5%–10%). Patients were randomly assigned to receive sitagliptin 100 mg daily or glipizide 5 mg daily. The dose was titrated upward to a maximum 20 mg daily.
The change in HbA1c from baseline to week 54 was similar between the two treatment groups (–0.51% with sitagliptin and −0.56% with glipizide). Of the randomized patients, 63% of those in the sitagliptin group and 59% of those in the glipizide group achieved an HbA1c of below 7%, whereas 29% of those in each group achieved an HbA1c of below 6.5%.
Patients receiving glipizide experienced more nonhypoglycemic adverse effects (30.3%) compared with the sitagliptin group (14.5%). Patients receiving sitagliptin were significantly less likely to experience hypoglycemia than those taking glipizide (5% vs. 32%, respectively; P < 0.001) and were more likely to lose weight (–1.5 kg vs. +1.1 kg, respectively; P < 0.001). The vast improvement in HbA1c and FPG levels with minimal hypoglycemia is consistent with the glucose-dependent mechanism of action of DPP-4 inhibitors.
Overall, the addition of sitagliptin to metformin therapy proved to be non-inferior when compared with glipizide/metformin combination therapy. However, when adverse effects such as hypoglycemia and weight gain were taken into account, sitagliptin was better tolerated.
Scott et al.25
Scott et al. enrolled 273 patients with a mean baseline HbA1c of 7.7% who were currently taking metformin. Patients were randomly assigned to receive sitagliptin 100 mg daily, rosiglitazone (Avandia, GlaxoSmithKline) 8 mg daily, or placebo for 18 weeks.
Changes in HbA1c were as follows: −0.73% (P < 0.001 vs. placebo) for sitagliptin, −0.79% (P < 0.001 vs. placebo) for rosiglitazone, and −0.22% for placebo. The percentage of patients achieving an HbA1c of below 7% was significantly higher for sitagliptin than for placebo (55% and 38%, respectively; P = 0.006) No significant differences were observed among the sitagliptin or rosiglitazone groups.
Rates of hypoglycemia and GI intolerance were similar among the active-treatment groups, but body weight decreased in patients taking sitagliptin (–0.4 kg) or placebo (–0.8 kg) and increased in those taking rosiglitazone (+1.5 kg).
In this study, sitagliptin was as efficacious as rosiglitazone in patients taking metformin and resulted in low rates of hypoglycemia, GI disturbances, and weight gain.
Scheen et al.26
Sitagliptin was compared with saxagliptin (Onglyza, Bristol-Myers Squibb/AstraZeneca) in an 18-week, double-blind, non-inferiority trial. Patients had inadequately controlled glucose levels with stable doses of metformin. Changes in baseline HbA1c were evaluated in patients who received either sitagliptin 100 mg (n = 398) or saxagliptin 5 mg (n = 403). Secondary endpoints included changes from baseline FPG levels, insulin, C-peptide, and pro-insulin.
Mean HbA1c decreased from 7.69% to 7.07% in the sitagliptin/metformin group (adjusted mean, −0.62%; 95% confidence interval [CI], −0.69% to −0.54%) and from 7.68% to 7.16% in the saxagliptin/metformin group (adjusted mean, −0.52%; 95% CI, −0.60 to −0.45%). The reduction in HbA1c was achieved after 8 weeks and was maintained throughout the entire study with both agents.
FPG levels decreased in both the sitagliptin and saxagliptin arms (by 16.2 mg/dL and 10.8 mg/dL, respectively). No differences in secondary endpoints (fasting insulin, pro-insulin, or C-peptide levels) were noted. Both drugs were well tolerated, and few serious adverse events were noted. Similar to other trials within this class, influenza, urinary tract infections, and nasopharyngitis were the most commonly reported adverse events. Both treatment arms experienced a 0.4-kg weight loss. The authors established non-inferiority in HbA1c reductions when saxagliptin was added to metformin compared to when sitagliptin was added to metformin.
Limitations of this study included the absence of a placebo group and the lack of reported P values.
Bergenstal et al.27
Investigators evaluated the safety, efficacy, and tolerability of three therapies when added to metformin: exenatide (Byetta, Amylin), sitagliptin, and pioglitazone. This double-blind, randomized, 26-week superiority trial compared 2 mg of exenatide injection once weekly plus oral placebo (n = 160), 100 mg of oral sitagliptin plus once-weekly injected placebo (n = 166), and 45 mg of oral pioglitazone once-daily plus once-weekly injected placebo (n = 165).
The primary endpoint analyzed was the change in HbA1c from baseline to the end of the study. Secondary endpoints included FPG, fasting insulin, and blood pressure. The exenatide group experienced the greatest HbA1c reductions from baseline to week 26 (1.5%). HbA1c was decreased with sitagliptin (by 0.9%) and with pioglitazone (by 1.2%).
Differences in treatment were −0.6% for exenatide (P < 0.0001) versus sitagliptin and −0.3% for exenatide, compared with pioglitazone (P = 0.0165). Improvements in FPG were significantly greater with exenatide (–1.8 mmol/L) than with sitagliptin (–0.9 mmol/L) but not significantly greater than with pioglitazone (–1.5 mmol/L).
At the end of the study, fasting insulin levels were significantly increased with once-daily exenatide (3.6 μIU/mL) compared with sitagliptin (0.4 μIU/mL), and pioglitazone (–3.9 μIU/mL). Weight loss was significantly greater with exenatide (–2.3 kg), compared with sitagliptin (–0.8 kg) and pioglitazone (2.8 kg).
All treatment arms experienced a reduction in blood pressure. High-density lipoprotein-cholesterol (HDL-C) levels were decreased in all treatment arms, with pioglitazone exerting the largest decrease. Pioglitazone was the only medication that significantly reduced triglyceride levels (by 0.16%; P = 0.062). No major episodes of hypoglycemia were reported.
The most commonly reported adverse events for exenatide and sitagliptin were nausea and diarrhea; however, the incidence of nausea (24% vs. 10%) as well as diarrhea (18% vs. 10%) was higher. The incidence of upper respiratory infections was higher with sitagliptin (9%) than with exenatide (4%). The most commonly reported side effects of pioglitazone included upper respiratory infections (10%), peripheral edema (8%), and diarrhea (7%). The overall safety profile appeared similar between the agents, and the reduction in HbA1c was greatest for exenatide.
Sitagliptin Plus Metformin Plus a Third Agent
VisbØll et al.28
A 24-week multinational, placebo-controlled, randomized, double-blind, parallel-group study was conducted to evaluate the efficacy and tolerability of sitagliptin when added to long-acting, intermediate-acting, or premixed insulin alone or in combination with metformin in patients with type-2 diabetes. Patients continued their home insulin regimens and were eligible for the study if they were taking at least 15 units of insulin per day. The study enrolled 641 patients with uncontrolled HbA1c (7.5%–11%), and 564 patients completed the study. Discontinuation and treatment compliance rates were similar between the study groups.
Throughout the study, patients’ metformin and insulin doses were expected to remain stable, except for a dose reduction if they experienced hypoglycemia. Patients were also eligible for rescue therapy if FPG levels remained above 280 mg/dL during weeks 1 to 12 and above 240 mg/dL during weeks 12 to 24.
After the placebo-controlled 2-week run-in period, patients received sitagliptin 100 mg daily or placebo. The primary end-point was the change in HbA1c levels from baseline to week 24. At baseline, HbA1c values ranged from 6.6% to 12.1% (mean, 8.7%) and the mean FPG level was 177 mg/dL. By week 24, a significant reduction in HbA1c was observed in the sitagliptin group (–0.6%) in contrast to a minimal reduction in the placebo group (–0.1%) (P < 0.001). At week 24, significantly more sitagliptin patients achieved HbA1c values below 7% compared with placebo patients (13% vs. 5%, respectively; P < 0.001); however, they experienced more drug-related adverse effects, including hypoglycemia (15.5% vs. 8.5%, respectively; P = 0.003).
Overall, the addition of sitagliptin to stable-dose insulin regimens, with or without metformin, improved glycemic control in patients with type-2 diabetes whose glucose levels had been inadequately controlled.
SAFETY AND TOLERABILITY
Adverse Effects
The most common adverse effects associated with sitagliptin include upper respiratory infections, nasopharyngitis, and headaches.12 Metformin is most often associated with diarrhea, nausea, vomiting, flatulence, abdominal discomfort, indigestion, asthenia, and headache.14 When sitagliptin and metformin are administered in combination, the most common adverse effects reported in 5% of patients or more include diarrhea, upper respiratory infection, and headache.
Hypoglycemia is not a particular concern with sitagliptin/metformin unless this combination is used with a sulfonylurea.29 In addition to hypoglycemia, weight gain remains a problem with the use of several antidiabetic therapies. Weight changes associated with sitagliptin/metformin have been equivalent to those with placebo in clinical trials.30
Warnings and Contraindications
A boxed warning regarding lactic acidosis can be found in the package insert for metformin as well as for Janumet (sitagliptin/metformin) and Janumet XR (extended-release sitagliptin/metformin).14,29,31 Lactic acidosis is a rare but serious metabolic complication that can be fatal in 50% of cases. The reported incidence in patients receiving metformin is 0.03 cases per 1,000 patient-years.14 Coexisting conditions such as sepsis, dehydration, excessive alcohol ingestion, hepatic insufficiency, renal impairment, and acute congestive heart failure can raise the risk of lactic acidosis as a result of metformin accumulation. Renal dysfunction (serum creatinine of 1.5 mg/dL or higher in men or 1.4 mg/dL or higher in women) is listed as a contraindication to metformin therapy.
Other contraindications to metformin include acute or chronic metabolic acidosis and radiological studies that involve the administration of intravascular iodinated contrast materials.29 Metformin should be used with caution or avoided in patients with hepatic disease or in patients 80 years of age and older.14,29
Sitagliptin has been associated with almost 90 postmarketing reports of acute pancreatitis, including two cases of hemorrhagic or necrotizing pancreatitis.32–34 Because of this effect, patients who are initiating treatment with sitagliptin (alone or in combination with metformin) or who are taking an increased dose should be monitored for the development of pancreatitis. If pancreatitis is suspected, sitagliptin should be discontinued immediately. Postmarketing reports of worsening renal function and hyper-sensitivity reactions, including anaphylaxis, angioedema, and Stevens–Johnson syndrome, have also been associated with sitagliptin.12
PLACE IN THERAPY
The cornerstone of therapy for patients with type-2 diabetes centers on lifestyle modifications and is associated with considerable beneficial effects. Weight loss that results from exercise and dietary modifications may significantly improve glucose levels, but long-term success is often limited.35 The initiation of pharmacotherapy is required for most patients and generally should not be delayed; lifestyle modifications are typically not adequate alone.
At least three core defects in diabetes are targeted by the available agents to decrease insulin resistance, improve insulin secretion, or impede glucagon production. More recent attention has focused on the abnormalities of the incretin system. Further research may be able to clarify whether this deviation represents a primary or secondary defect of type-2 diabetes.2
Despite the wide array of glucose-lowering interventions, choosing an appropriate treatment poses a challenge for health care practitioners. This task is compounded by an increase in newer distinct agents and by the realization that most patients will require more than one medication.
The ADA and the EASD have developed recommendations to aid clinicians in the decision-making process with the awareness that quality clinical trials comparing the available agents are limited.2 The approach to glycemic control in these recomendations is an emphasis on individualized treatment and patient involvement. Particular attention should be paid to the patient’s attitude and motivation, potential risk for falls, duration of disease, life expectancy, comorbidities, and support system.
The ADA and EASD continue to recommend lifestyle modifications for all patients upon diagnosis of type-2 diabetes. If there are no contraindications, metformin should be started for most patients. Patients whose HbA1c is close to goal (below 7.5%) may complete a 3- to 6-month trial of lifestyle modifications before metformin is initiated. In addition to its benefits in weight loss, metformin is inexpensive and is not associated with hypoglycemia when used as monotherapy. Benefits for cardiovascular disease were observed in the United Kingdom Prospective Diabetes Study and may be another reason for the strong recommendation of metformin.15
Choosing a subsequent agent requires a delicate balance between treating hyperglycemia and respecting the patients’ quality of life. Sulfonylureas, although effective and extensively studied, tend to cause hypoglycemia and weight gain. These economical agents are also associated with a secondary failure rate higher than that of other antidiabetic agents.2 The meglitinides have a mechanism of action similar to that of the sulfonylureas, and they are customarily given with meals. Increasing the frequency of administration must be weighed against the potential for higher rates of hypoglycemia.
At one time, the thiazolidinedione (TZD) class received significant media attention over the withdrawal of one its agents, rosiglitazone (Avandia). Another drug in this class, pioglitazone (Actos), is still available. Pioglitazone does not cause hypoglycemia. It is taken once daily; however, it has been associated with an increase in bladder cancer and a risk of bone fractures.36,37
The effect of TZDs on glucose lowering may be longer-lasting when compared with metformin or the sulfonylureas.38 Alphaglucosidase inhibitors, such as acarbose (Precose, Bayer), and bile acid sequestrants, such as coleselvam (Welchol, Sankyo Pharma), are used less frequently because of an elevated incidence of GI side effects. However, they do have the advantage of not causing hypoglycemia when used alone.
The incretin agents have received more attention in the recent ADA guidelines; however, these drugs are limited to specific populations because of a lack of evidence and cost. GLP-1 receptor agonists, a class within the incretins, cause varying degrees of weight loss among patients. GI adverse effects, the dosage form (injection), and the possible association with pancreatitis are concerns with these agents.
Sitagliptin, the prototype DPP-4 inhibitor, was approved in 2006 and has the distinct advantage of oral administration. The DPP-4 inhibitors are well tolerated and are considered weight-neutral. Neither GLP-1 agonists nor DPP-4 inhibitors cause hypoglycemia.
Metformin, the sulfonylureas, the TZDs, and the GLP-1 agonists confer the greatest reductions in HbA1c values (by 0–1.5%). The meglitinides and DPP-4 inhibitors also reduce HbA1c values (by 0.5% to 1%).2 If HbA1c values exceed 9%, patients usually require a combination of two oral agents or they may be started on insulin directly. If the HbA1c is between 10% and 12% or if FPG levels exceed 300 mg/dL, patients are strongly encouraged to start insulin at the onset of treatmentt.2
If metformin is not tolerated, a sulfonylurea, a meglitinide, pioglitazone, or a DPP-4 inhibitor is a possible choice. GLP-1 agonists may be considered when weight loss is desired, but therapy with these agents must be balanced against the cost and the inconvenience of an injection. If patients taking metformin do not achieve their HbA1c goal, any of the medications mentioned may be added.
The paucity of high-quality comparative clinical trials remains an obstacle to a strong recommendation of one class of agents over another. With no strong emphasis on any agent for add-on therapy, the risks and benefits of each agent should be discussed with the patient. In addition to the factors already discussed, health care practitioners should consider the patient’s age, weight, and comorbidities (e.g., heart failure, kidney or liver dysfunction, and risk of hypoglycemia).
PATIENT-FOCUSED PERSPECTIVES
Combination sitagliptin/metformin therapy appears to be well tolerated in patients with type-2 diabetes. When adjunctive therapy is being considered, several factors, including the route of administration, the adverse-effect profile, patient preference, and cost, should be evaluated. The fixed-dose combination of sitagliptin/metformin allows physicians to modify the regimens of patients with inadequately controlled glucose levels with metformin monotherapy without increasing pill burden.
Unlike other antihyperglycemic agents, sitagliptin/metformin is associated with little to no hypoglycemia or weight gain. This is an important factor to consider, especially in patients with coronary heart disease and the elderly. The tolerability profile of the combination is comparable to that of metformin monotherapy.39 The combination has also been well tolerated in 24-week clinical trials with insulin and glimepiride (Amaryl, Sanofi).28,40 The sitagliptin/metformin combination (Janumet) may be most appropriate in patients close to their HbA1c goal who are taking dual antihyperglycemic agents or in those experiencing hypoglycemia with their current regimen.
In addition to these benefits, combining sitagliptin and metformin may provide a neutral effect on body weight and HbA1c. Once-daily Janumet XR appears to be safe and effective for lowering glucose levels and minimizing the pill burden in patients with type-2 diabetes.
CONCLUSION
Diabetes mellitus is a chronic, progressive disease of epidemic proportions. Because lifestyle modifications alone are often inadequate, two or more agents are usually required to attain adequate glycemic control.
The prototype DPP-4 inhibitor, sitagliptin, emerged as the incretin effect became a focus of research. Current guidelines recommend metformin as a first-line therapy for type-2 diabetes. Sitagliptin and metformin provide additive glycemic improvements, suggesting a synergy between the agents. However, although sitagliptin is effective, its cost and limited long-term data may restrict its use. In addition, its effects on microvascular and macrovascular complications are not known.
Additional studies are necessary to fully evaluate the effects of long-term DPP-4 inhibition and to determine sitagliptin’s role in combination therapy.
Footnotes
Disclosure: The authors report that they have no financial or commercial relationships to disclose.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) National Diabetes Fact Sheet. 2011. Available at: www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed May 30, 2012.
- 2.Inzucci SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: A patient centered approach: Position Statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2012;35:1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Look AHEAD Research Group Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes. Diabetes Care. 2007;30:1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.FDA approves Janumet XR for type 2 diabetes, offering the powerful efficacy of Janumet now available with once-daily convenience. Available at: www.merck.com/newsroom/news-release-archive/prescription-medicine-news/2012_0202.html. Accessed May 31, 2012. [Google Scholar]
- 5.Creutzfeldt W. The [pre] history of the incretin concept. Regul Pept. 2005;128:87–91. doi: 10.1016/j.regpep.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Weber A. Dipeptidyl peptidase IV inhibitors for the treatment of diabetes. J Med Chem. 2004;47:4135–4141. doi: 10.1021/jm030628v. [DOI] [PubMed] [Google Scholar]
- 7.Miller SA, St. Onge E. Sitagliptin: A dipeptidyl peptidase inhibitor in the treatment of diabetes. Ann Pharmacother. 2006;40(7–8):1336–1343. doi: 10.1345/aph.1G665. [DOI] [PubMed] [Google Scholar]
- 8.VisbØll T, Krarup T, Deacon C, et al. Reduced postprandial concentrations of intact biologically active glucagon-like peptide 1 in type 2 diabetic patients. Diabetes. 2001;50:609–613. doi: 10.2337/diabetes.50.3.609. [DOI] [PubMed] [Google Scholar]
- 9.Nauck MA, Vardaril I, Deacon CF, et al. Secretion of glucagon-like peptide-1 (GLP-1) in type 2 diabetes: What is up, what is down? Diabetologia. 2011;54:10–18. doi: 10.1007/s00125-010-1896-4. [DOI] [PubMed] [Google Scholar]
- 10.Deacon CF. MK-431 (Merck) Curr Opin Investig Drugs. 2005;6:419–426. [PubMed] [Google Scholar]
- 11.Langely AK, Suffoletta TJ, Jennings HR, et al. Dipeptidyl peptidase IV inhibitors and the incretin system in type 2 diabetes mellitus. Pharmacotherapy. 2007;27(8):1163–1180. doi: 10.1592/phco.27.8.1163. [DOI] [PubMed] [Google Scholar]
- 12.Januvia (sitagliptin), package insert. Whitehouse Station, N.J.: Merck; 2011. Available at: www.januvia.com/sitagliptin/januvia/hcp/januvia/index.jsp?WT.svl=1. Accessed December 7, 2011. [Google Scholar]
- 13.Krentz AJ, Bailey CJ. Oral antidiabetic agents current role in type 2 diabetes mellitus. Drugs. 2005;65(3):385–411. doi: 10.2165/00003495-200565030-00005. [DOI] [PubMed] [Google Scholar]
- 14.Glucophage (metformin), package insert. Princeton, N.J: Bristol-Myers Squibb; 2009. Available at: http://packageinserts.bms.com/pi/pi_glucophage.pdf. Accessed December 7, 2011. [Google Scholar]
- 15.UK Prospective Diabetes Study (UKPDS) Group Effect of intensive blood glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS34) Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 16.Brazg R, Xu L, Dalla MC, Cobelli C, et al. Effect of adding sitagliptin, a dipeptidyl peptidase-4 inhibitor, to metformin on 24-hour glycemic control and β-cell function in patients with type 2 diabetes. Diabetes Obes Metab. 2007;9:186–193. doi: 10.1111/j.1463-1326.2006.00691.x. [DOI] [PubMed] [Google Scholar]
- 17.Williams-Herman D, Johnson J, Teng R, et al. Efficacy and safety of sitagliptin and metformin as initial combination therapy and as monotherapy over 2 years in patients with type 2 diabetes. Diabetes Obes Metab. 2010 May;12(5):442–451. doi: 10.1111/j.1463-1326.2010.01204.x. [DOI] [PubMed] [Google Scholar]
- 18.Reasner C, Olansky L, Seck TL, et al. The effect of initial therapy with the fixed-dose combination of sitagliptin and metformin compared with metformin monotherapy in patients with type 2 diabetes mellitus. Diabetes Obes Metab. 2011;13(7):644–652. doi: 10.1111/j.1463-1326.2011.01390.x. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein BJ, Feinglos MN, Johnson JJ, et al. Effect of initial combination therapy with sitagliptin, a dipeptidylpeptidase-4 inhibitor, and metformin on glycemic control in patients with type 2 diabetes. Diabetes Care. 2007;30:1979–1987. doi: 10.2337/dc07-0627. [DOI] [PubMed] [Google Scholar]
- 20.Charbonnel B, Karasik A, Liu J, et al. for the Sitagliptin Study 020 Group Efficacy and safety of the dipeptidyl peptidase-4 inhibitor sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes inadequately controlled with metformin alone. Diabetes Care. 2006;29(12):2638–2643. doi: 10.2337/dc06-0706. [DOI] [PubMed] [Google Scholar]
- 21.Perez-Montverde A, Seck T, Xu L, et al. Efficacy and safety of sitagliptin and the fixed-dose combination of sitagliptin and metformin vs. pioglitazone in drug-naive patients with type 2 diabetes. Int J Clin Pract. 2011;65(9):930–938. doi: 10.1111/j.1742-1241.2011.02749.x. [DOI] [PubMed] [Google Scholar]
- 22.Raz I, Chen Y, Wu M, et al. Efficacy and safety of sitagliptin added to ongoing metformin therapy in patients with type 2 diabetes. Curr Med Res Opin. 2008;24(2):537–550. doi: 10.1185/030079908x260925. [DOI] [PubMed] [Google Scholar]
- 23.Karasik A, Wu M, Williams-Herman D, Meininger G. Sitagliptin added to ongoing metformin therapy provides sustained glycemic control over 54 weeks, with a low incidence of hypoglycemia and with weight loss (Abstract 0523-P). American Diabetes Association, 67th Sessions; June 22–26, 2007; Chicago. Available at: http://professional.diabetes.org/Content/Posters/2007/p0523-P.pdf. Accessed June 6, 2012. [Google Scholar]
- 24.Nauck M, Meininger G, Sheng D, et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, compared with the sulfonylurea, glipizide, in patients with type 2 diabetes inadequately controlled on metformin alone: A randomized, double-blind, non-inferiority trial. Diabetes Obes Metab. 2007;9:194–205. doi: 10.1111/j.1463-1326.2006.00704.x. [DOI] [PubMed] [Google Scholar]
- 25.Scott R, Loeys T, Davies MJ, Engel SS, for the Sitagliptin Study 801 Group Efficacy and safety of sitagliptin when added to ongoing metformin therapy in patients with type 2 diabetes. Diabetes Obes Metab. 2008;10:959–969. doi: 10.1111/j.1463-1326.2007.00839.x. [DOI] [PubMed] [Google Scholar]
- 26.Scheen AJ, Charpentier G, Ostgren CJ, et al. Efficacy and safety of saxagliptin in combination with metformin compared with sitagliptin in combination with metformin in adults patients with type 2 diabetes mellitus. Diabetes Metab Res Rev. 2010;26:540–549. doi: 10.1002/dmrr.1114. [DOI] [PubMed] [Google Scholar]
- 27.Bergenstal RM, Wysham C, MacConell L, et al. Efficacy and safety of exenatide once weekly versus sitagliptin or pioglitazone as an adjunct to metformin for treatment of type 2 diabetes (DURATION-2): A randomised trial. Lancet. 2010;376:431–439. doi: 10.1016/S0140-6736(10)60590-9. [DOI] [PubMed] [Google Scholar]
- 28.VisbØll T, Rosenstock J, Yki-Jarvinen H, et al. Efficacy and safety of sitagliptin when added to insulin therapy in patients with type 2 diabetes. Diabetes Obes Metab. 2010;12(2):167–177. doi: 10.1111/j.1463-1326.2009.01173.x. [DOI] [PubMed] [Google Scholar]
- 29.Janumet, prescribing information. Whitehouse Station, N.J.: Merck; 2007. Available at: www.merck.com/product/usa/pi_circulars/j/janumet/janumet_pi.pdf. Accessed December 10, 2011. [Google Scholar]
- 30.Karasik A, Aschner P, Katzeff H, et al. Sitagliptin, a DPP-4 inhibitor for the treatment of patients with type 2 diabetes: A review of recent clinical trials. Curr Med Res Opin. 2008;24(2):489–496. doi: 10.1185/030079908x261069. [DOI] [PubMed] [Google Scholar]
- 31.Janumet XR, prescribing information. Whitehouse Station, N.J.: Merck; 2012. Available at: www.merck.com/product/usa/pi_circulars/j/janumet_xr/janumet_xr_pi.pdf. Accessed March 2, 2012. [Google Scholar]
- 32.FDA Drug Safety Communication: Information for healthcare professionals: Acute pancreatitis and sitagliptin (marketed as Januvia and Janumet) Available at: www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm183764.htm. Accessed October 20, 2011.
- 33.Garg R, Hussey C, Ibrahim S. Pancreatitis associated with the use of sitagliptin and orlistat combination: A case report. Diabet Med. 2010;27(4):485–486. doi: 10.1111/j.1464-5491.2010.02950.x. [DOI] [PubMed] [Google Scholar]
- 34.Iyer SN, Drake AJ, West RL, et al. Case report of acute necrotizing pancreatitis associated with combination treatment of sitagliptin and exenatide. Endocr Pract. 2012;18(1):e10–3. doi: 10.4158/EP11264.CR. [DOI] [PubMed] [Google Scholar]
- 35.Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy. A consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2006;29(8):1963–1971. doi: 10.2337/dc06-9912. [DOI] [PubMed] [Google Scholar]
- 36.Lewis JD, Ferrara A, Peng T, et al. Risks of bladder cancer among diabetic patients treated with pioglitazone: Interim report of a longitudinal cohort study. Diabetes Care. 2011;34:916–922. doi: 10.2337/dc10-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.FDA Actos (pioglitazone) Available at: www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm150451.htm?utm. Accessed June 5, 2012.
- 38.Kahn SE, Haffner SM, Heise MA, et al. for the ADOPT Study Group Glycemia durability of rosiglitazone, metformin, or glyburide monotherapy. N Eng J Med. 2006;355:2427–2443. doi: 10.1056/NEJMoa066224. [DOI] [PubMed] [Google Scholar]
- 39.Williams-Herman D, Johnson J, Teng R, et al. Efficacy and safety of initial combination therapy with sitagliptin and metformin in patients with type 2 diabetes: A 54-week study. Curr Med Res Opin. 2009;25(3):569–583. doi: 10.1185/03007990802705679. [DOI] [PubMed] [Google Scholar]
- 40.Hermansen K, Kipnes M, Luo E, et al. Efficacy and safety of the dipeptidyl peptidase-4 inhibitor, sitagliptin, in patients with type 2 diabetes mellitus inadequately controlled on glimepiride alone or on glimepiride and metformin. Diabetes Obes Metab. 2007;9(5):733–745. doi: 10.1111/j.1463-1326.2007.00744.x. [DOI] [PubMed] [Google Scholar]