Abstract
Denosumab (Dmab) and zoledronic acid (ZOL) are antiresorptive agents, with different mechanisms of action, that are indicated for delaying the onset of skeletal-related events in patients with bone metastases from solid tumors. Clinical and preclinical data suggest that ZOL may have also anti-angiogenic activity; however, the effects of Dmab (a fully humanized antibody against the receptor activator of nuclear factor kappa B ligand) on angiogenesis are largely unknown. The objective of this study was to compare the potential anti-angiogenic activity of Dmab with that of ZOL in preclinical models. Dmab (0.31 to 160 μM) had no effect on the viability of human MDA-MB-436 and CG5 breast cancer cells or human umbilical vein endothelial cells (HUVECs) and no effect on tubule formation or invasion of HUVECs. In contrast, ZOL (0.31 to 160 μM) decreased the viability of breast cancer and HUVECs in a time- and concentration-dependent manner and also inhibited HUVEC tubule formation and invasion. In vivo, ZOL (20 μg/mouse for three times a week for three consecutive weeks) inhibited angiogenesis in Matrigel plugs and inhibited the growth and neo-angiogenesis of CG5 xenografts in athymic nude mice. In contrast, Dmab (10 mg/Kg twice a week for 4 consecutive weeks) had no effect on Matrigel vascularization or xenograft growth in this model. These findings support the potential antiangiogenic and anticancer activity of ZOL in vitro and in vivo and further suggest that Dmab does not have antiangiogenic activity. Additional studies are needed to elucidate the potential anticancer activity of Dmab.
Keywords: anticancer, angiogenesis, breast cancer, denosumab, HUVEC, RANKL, zoledronic acid
Introduction
Denosumab (Dmab) and zoledronic acid (ZOL) are antiresorptive agents with different mechanisms of action indicated for delaying the onset of skeletal-related events (SREs) in patients with bone metastases from solid tumors, including breast cancer.1,2 Moreover, these agents also have demonstrated efficacy for preserving bone health in patients in the adjuvant breast cancer setting.3-9 In addition to its antiresorptive effects, clinical and preclinical data suggest that ZOL also may have antiangiogenic effects.10-13 However, the effects of the newer antiresorptive agent Dmab on angiogenesis are largely unknown.
ZOL is among the most active nitrogen-containing bisphosphonates (N-BPs),14,15 and is the only bisphosphonate indicated for the treatment of patients with multiple myeloma or patients with bone metastases from solid tumors.1 All bisphosphonates accumulate in the mineral portion of the bone matrix and are released during bone resorption. After internalization by osteoclasts, N-BPs inhibit farnesyl pyrophosphate synthase, an enzyme in the mevalonate pathway required for the post-translational modification and function of small GTPases (e.g., Ras, Rho, Rac), which play a key role in cell proliferation and survival.14,16-18 Therefore, N-BPs such as ZOL interfere with multiple cellular functions required for the bone-resorbing activity and survival of osteoclasts.
In addition to its antiresorptive activity, studies have shown that ZOL (and other BPs) can inhibit several steps involved in angiogenesis,10,11,13 an important process involved in tumor growth and progression. For example, a preclinical study demonstrated that BPs (ie, ZOL, ibandronate, risedronate and clodronate) decreased proliferation and capillary-like tube formation and induced apoptosis in human umbilical vein endothelial cells (HUVECs).11 Moreover, ZOL has been shown to inhibit proliferation, adhesion and migration of HUVECs, reduce blood vessel sprouting in cultured aortic ring and chicken chorioallantoic membrane assays and inhibit basic fibroblast growth factor (bFGF)-induced angiogenesis in mice.13 Additionally, in a small clinical study (n = 26) of patients with bone metastases from solid tumors, repeated low doses of ZOL (1 mg q week × 4, 4 mg q 28 d × 3) produced significant (p < 0.01) decreases in vascular endothelial growth factor (VEGF) levels.12 Notably, these effects were observed early and were long-lasting. Taken together, these studies suggest that ZOL has antiangiogenic properties, which might translate to clinical anticancer activity.
Denosumab is a fully humanized monoclonal antibody that specifically targets the human receptor activator of nuclear factor kappa B (RANK) ligand (RANKL), a cytokine essential for osteoclast differentiation, activation and survival.2,19,20 In a recent phase III clinical trial, Dmab was more effective at delaying SREs than ZOL in women with bone metastases from breast cancer.21 Moreover, Dmab is indicated for the prevention of SREs in patients with bone metastases from solid tumors, but is not indicated for patients with multiple myeloma.2 Therefore, this antiresorptive agent represents an exciting new treatment option for patients with bone metastases from breast cancer.
In contrast with bisphosphonates, Dmab does not incorporate into the mineralized bone matrix.22,23 In addition, RANKL is expressed systemically; therefore, blocking RANKL with Dmab may interfere with important RANKL-mediated pathways outside of bone. Indeed, preclinical studies suggest that RANKL may be involved in angiogenesis, but data are conflicting.24-26 For example, proangiogenic factors such as VEGF have been shown to increase RANK expression,25 and RANKL has been shown to promote angiogenesis in vivo in an endothelial nitric oxide synthase-dependent manner.26 Intuitively, these data suggest that RANKL inhibition would also inhibit angiogenesis. However, another preclinical study showed that RANKL inhibits proliferation of HUVECs and VEGF-induced angiogenesis and induces apoptosis in these cells.24 Therefore, the effects of inhibiting RANKL on angiogenesis remain equivocal. The objective of this study was to examine the potential antiangiogenic effects of RANKL inhibition with Dmab.
Results
In vitro cytotoxicity and capillary tubule inhibition
The cytotoxicity of Dmab and ZOL was evaluated in human MDA-MB-436 (Fig. 1), CG5 (Fig. 2) cells and HUVECs (Fig. 3). Dmab (0.31 to 160 μM) did not significantly inhibit growth of MDA-MB-436, CG5 cells or HUVECs (p > 0.05), nor did inhibit HUVEC tubule formation in Matrigel compared with control (p > 0.05) (Fig. 4). In contrast with these findings, ZOL decreased the viability of MDA-MB-436, CG5 cells and HUVECs in a time- and concentration-dependent manner with an IC50 (concentration inhibiting 50% of growth) of 111.88 μM ZOL after 48 h and 34.75 μM ZOL after 72 h in MDA-MB-436 cells, 78.55 μM ZOL after 48 h and 14.54 μM ZOL after 72 h in MDA-MB-436 cells and 64.46 μM ZOL after 72 h in HUVECs (Table 1). As expected, ZOL caused considerable reduction in cell viability after 72 h of treatment, particularly for CG5 and MDA-MB-436 cells (p < 0.001). Moreover, HUVEC capillary tubule formation was inhibited after 24 h from ZOL addition in a dose-dependent manner (Fig. 5). Additionally, marked inhibition was observed at 10 μM ZOL and 160 μM ZOL caused almost complete capillary tubule disruption. Indeed, quantification of tubule networks in HUVECs illustrates the inhibitory effect of ZOL (already at 1 μM that is a concentration readily achievable in vivo) and the lack of any effect with Dmab even at high concentrations (Fig. 6).
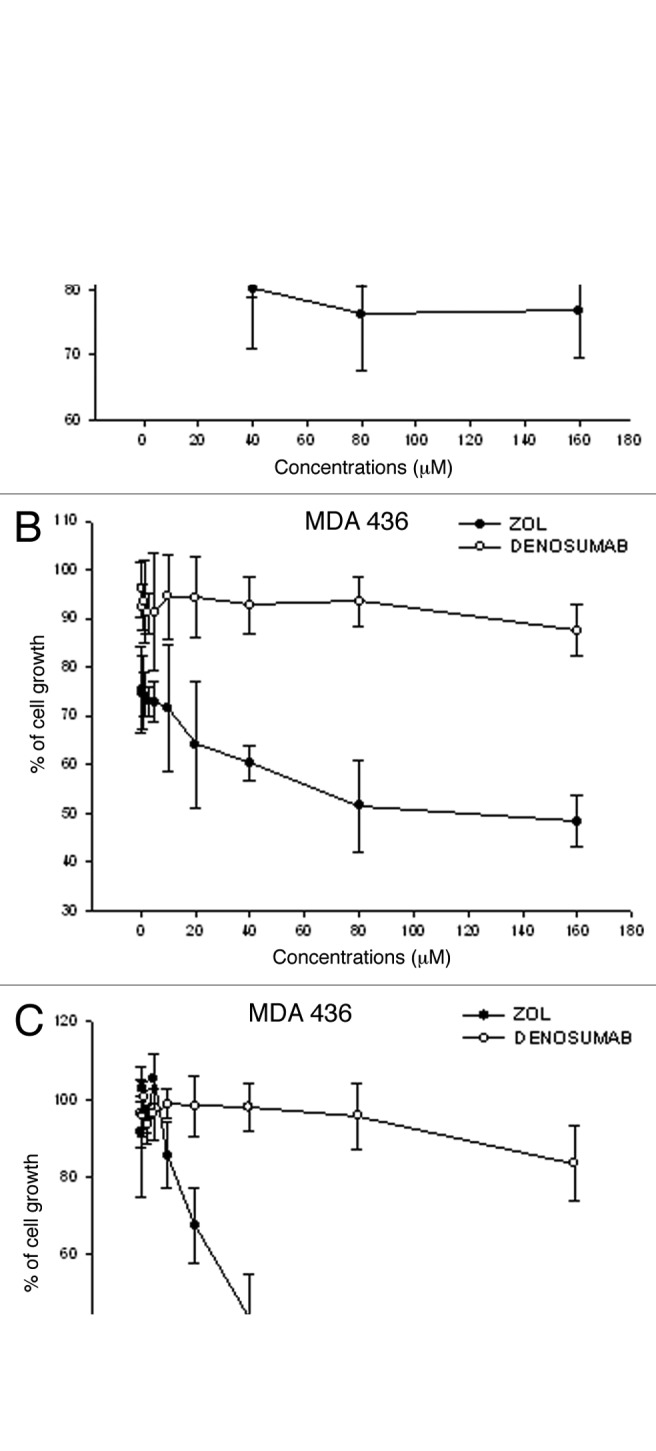
Figure 1. Cytotoxicity of Dmab and ZOL in human MDA-MB-436 cells. Cell viability of the human breast cancer cell line MDA-MB-436 after treatment with increasing concentrations (0.31 to 160 μM) of Dmab (○) or ZOL (•) for (A) 24 h, (B) 48 h and (C) 72 h was evaluated by MTT assay and expressed as percentage of untreated cells. Each point is the mean of at least four different replicate experiments (± S.D.). Statistical analysis: p < 0.01, untreated vs. 80 μM and 160 μM ZOL treated cells at 48 h; p < 0.001, untreated vs. 40 μM, 80 μM and 160 μM ZOL treated cells at 72 h.
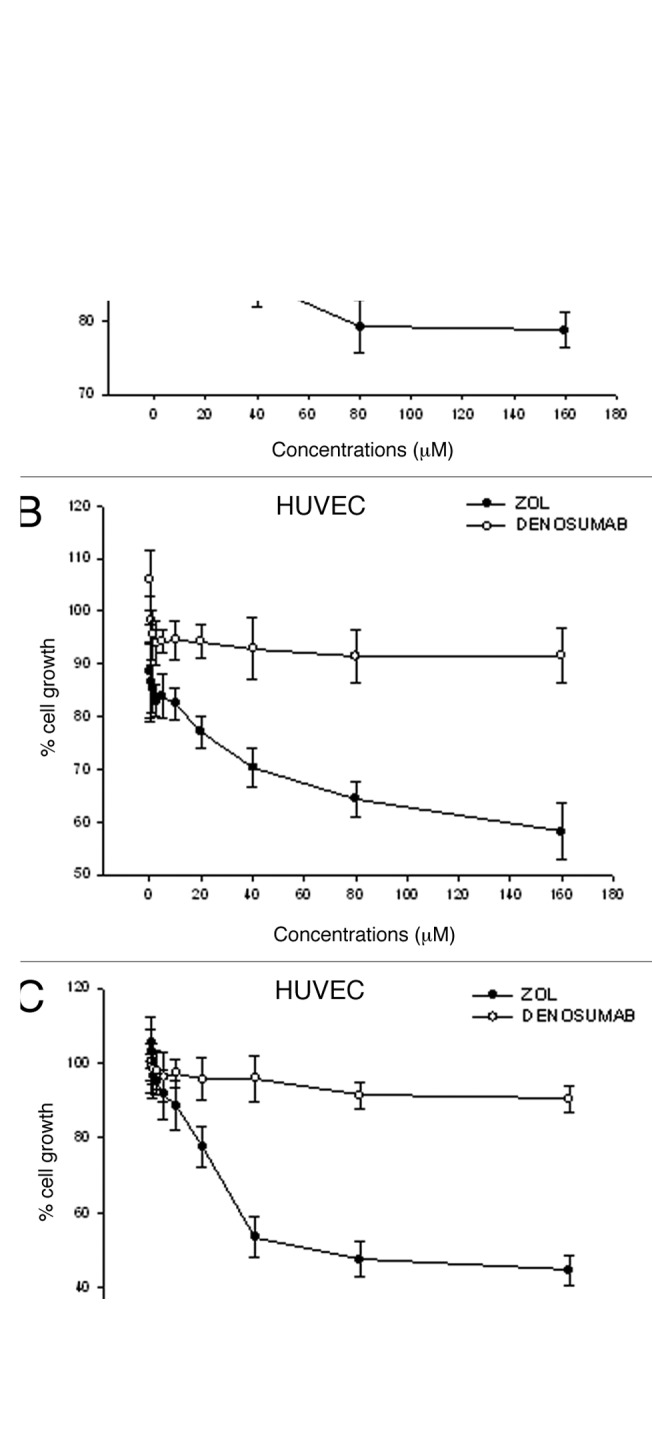
Figure 2. Cytotoxicity of Dmab and ZOL in human CG5 cells. Cell viability of the human breast cancer cell line CG5 after treatment with increasing concentrations (0.31 to 160 μM) of Dmab (○) or ZOL (•) for (A) 24 h, (B) 48 h and (C) 72 h was evaluated by MTT assay and expressed as percentage of untreated cells. Each point is the mean of at least four different replicate experiments (± S.D.). Statistical analysis: p < 0.01, untreated vs. 80 μM and 160 μM ZOL treated cells at 48 h; p < 0.001, untreated vs. 40 μM, 80 μM and 160 μM ZOL treated cells at 72 h.
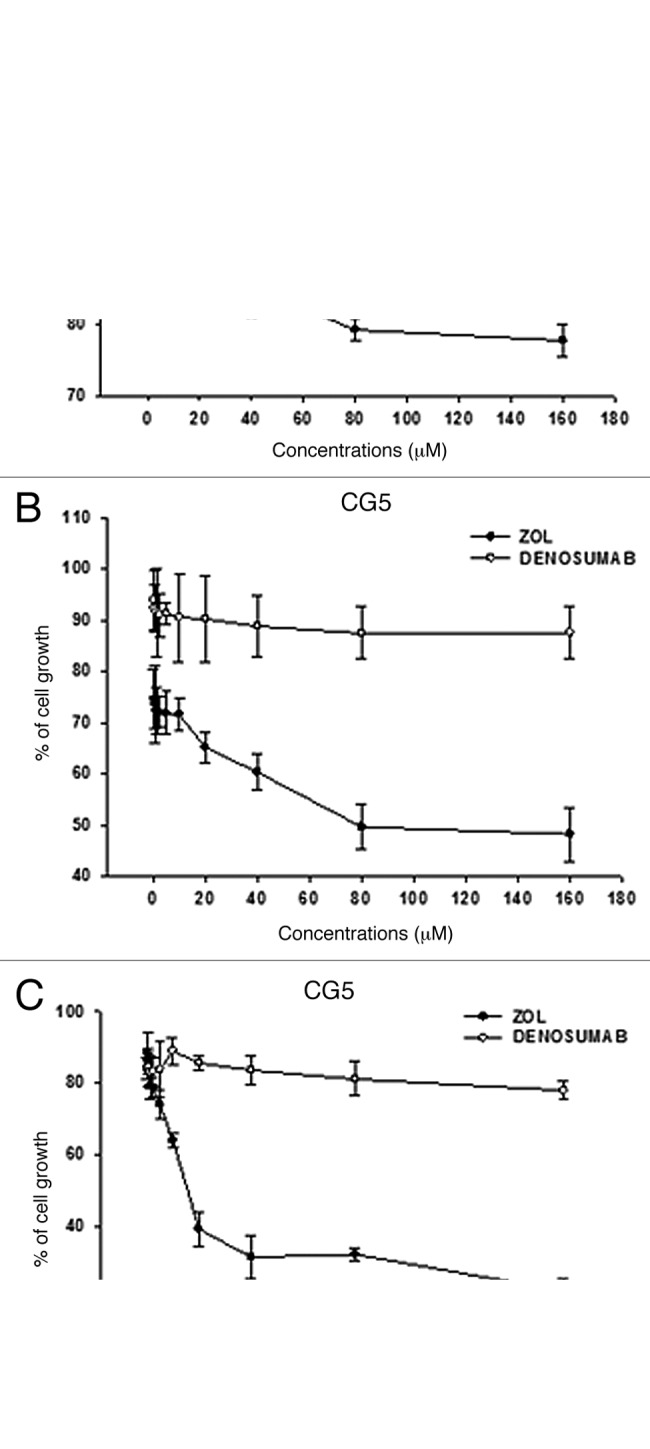
Figure 3. Cytotoxicity of Dmab and ZOL in HUVECs. Cell viability of HUVECs treated with increasing (0.31 to 160 μM) concentrations of Dmab (○) or ZOL (•) for (A) 24 h, (B) 48 h and (C) 72 h was evaluated by MTT assay and expressed as percentage of untreated cells. Each point is the mean of at least four different replicate experiments (± S.D.). Statistical analysis: p < 0.01, untreated vs. 160 μM ZOL treated cells at 48 h, untreated vs. 40 μM, 80 μM and 160 μM ZOL treated cells at 72h.
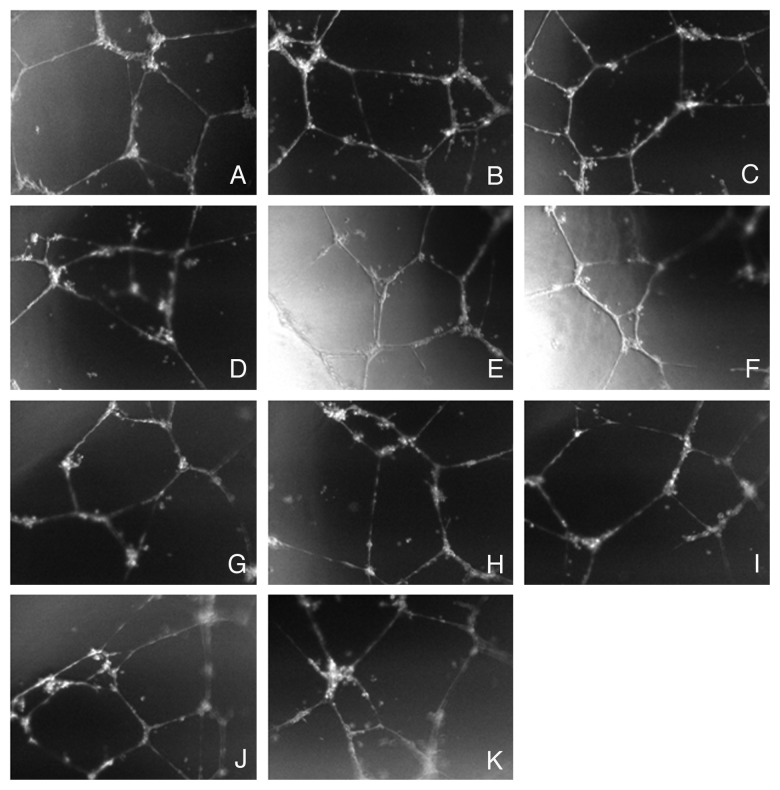
Figure 4. Effects of Dmab on HUVEC tubule formation. Representative photomicrographs of HUVECs plated onto Matrigel after 24 h of treatment with (A) vehicle control; (B) 0.31 μM Dmab; (C) 0.62 μM Dmab; (D) 1.25 μM Dmab; (E) 2.5 μM Dmab; (F) 5 μM Dmab; (G) 10 μM Dmab; (H) 20 μM Dmab; (I) 40 μM Dmab; (J) 80 μM Dmab; (K) 160 μM Dmab. Pictures were taken at magnification 10 × .
Table 1. IC50 Values (μM) of Dmab or ZOLa .
| |
IC50 |
||
|---|---|---|---|
| MDA 436 | CG5 | HUVEC | |
| 24h |
> 160 ± 0.02 |
> 160 ± 0.03 |
> 160 ± 0.04 |
| 48h |
> 160 ± 0.03 |
> 160 ± 0.04 |
> 160 ± 0.04 |
| 72h |
> 160 ± 0.07 |
> 160 ± 0.04 |
> 160 ± 0.06 |
| 24h |
> 160 ± 0.02 |
> 160 ± 0.02 |
> 160 ± 0.03 |
| 48h |
111.88 ± 0.03 |
78.55 ± 0.04 |
> 160 ± 0.02 |
| 72h | 34.75 ± 0.04 | 14.54 ± 0.05 | 64.46 ± 0.03 |
Data shown are mean ± standard deviation. Abbreviations: Dmab, denosumab; h = hours; ZOL, zoledronic acid.
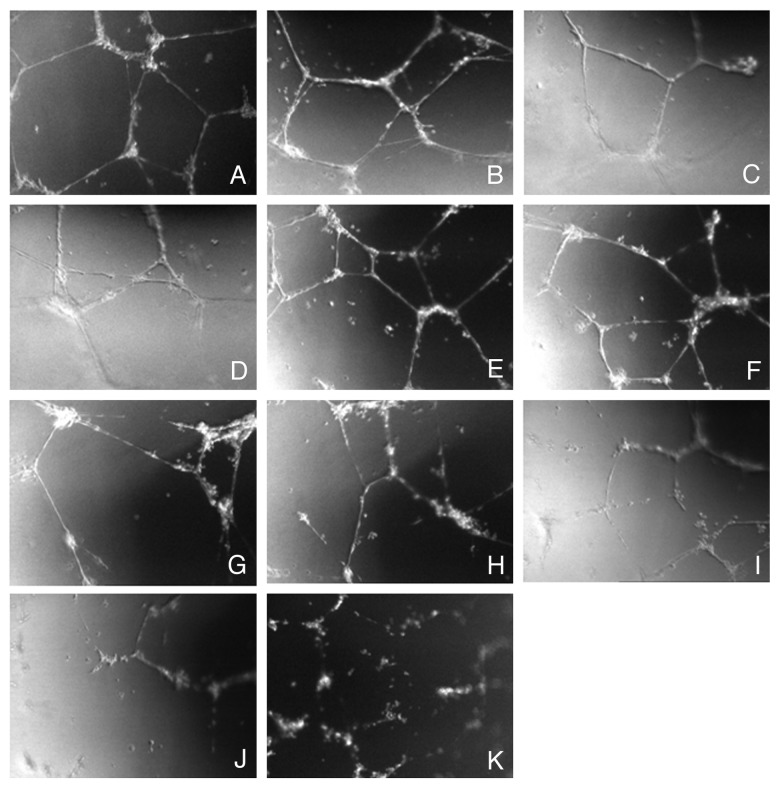
Figure 5. Effects of ZOL on HUVEC tubule formation. Representative photomicrographs of HUVECs plated on Matrigel after 24 h of treatment: with (A) vehicle control; (B) 0.31 μM ZOL; (C) 0.62 μM ZOL; (D) 1.25 μM ZOL; (E) 2.5 μM ZOL; (F) 5 μM ZOL; (G) 10 μM ZOL; (H) 20 μM ZOL; (I) 40 μM ZOL; (J) 80 μM ZOL; (K) 160 μM ZOL. Pictures were taken at magnification 10 × .
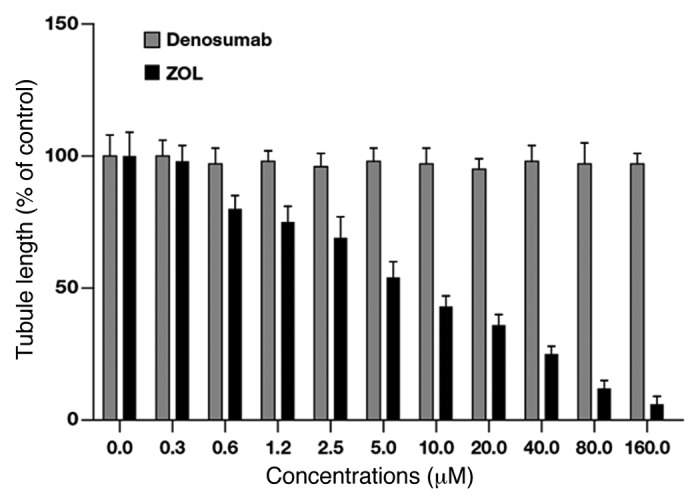
Figure 6. Quantification of the effects of Dmab and ZOL on HUVEC tubule formation. Capillary-like networks were quantified with ImageJ software. Each point is the mean of at least four different replicate experiments (± S.D.). Statistical analysis: p < 0.05, untreated vs. 0.6 μM, 1.2 μM and 2.5 μM ZOL treated cells; p < 0.01, untreated vs. 5.0 μM, 10.0 μM and 20.0 μM ZOL treated cells; p < 0.001, untreated vs. 40.0 μM, 80.0 μM and 160.0 μM ZOL treated cells.
In vitro invasion
In the presence of a chemoattractant (FBS), untreated HUVECs (positive control) strongly invaded the lower surface of the insert, whereas invasion in the absence of a chemoattractant (negative control) was limited. Dmab had no effect on chemoattractant-induced HUVEC invasion. However, treatment with ZOL for 24 h inhibited chemoattractant-induced HUVEC invasion in a dose-dependent manner (Fig. 7). The number of invading cells, compared with the positive control, was reduced by approximately 50%, 75% and 90% at 5 μM, 20 μM and 160 μM ZOL, respectively.
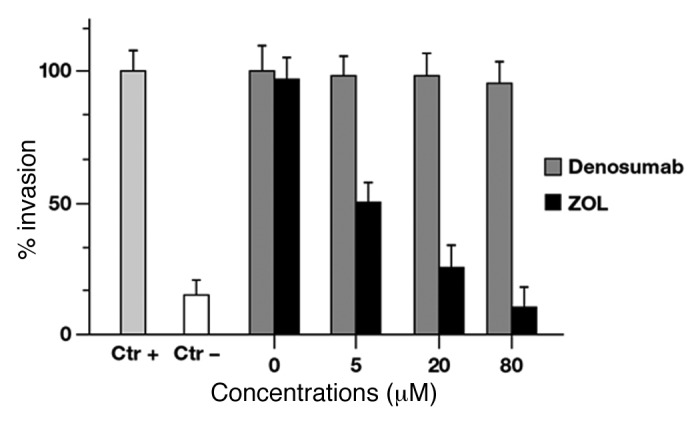
Figure 7. Effects of Dmab and ZOL on HUVEC invasion. Cultured HUVECs were harvested and suspended in DMEM and incubated for 24 h on filter coated with Matrigel in the absence or in presence of Dmab or ZOL; 3 mL of DMEM supplemented with 10% FBS (positive control) or not (negative control) was added to the well underneath the insert. Cells that crossed the Matrigel-coated filter were fixed, stained and counted. Six random microscope fields were counted for each group. Statistical analysis: p < 0.01 control vs. 5μM ZOL treated cells; p < 0.001 control vs. 20 μM and 80 μM ZOL treated cells.
In vivo angiogenesis
An in vivo vascularization assay was performed using Matrigel plug assay in mice to evaluate the effects of ZOL and Dmab on the angiogenic process. Any angiogenic response observed by macroscopic analysis (Fig. 8A,a and B,a) was found by quantitative evaluation obtained by measuring hemoglobin levels in the Matrigel of negative controls (without the addition of VEGF and TNFα). On the other hand, a potent angiogenic response was observed in positive controls (Fig. 8A,b and B,b) with an increase of about 5-fold of the recorded O.D.. Moreover, significant vascularization similar to the positive control was observed in Matrigel plugs containing untreated CG5 cells exposed in the presence of VEGF and TNFα (Fig. 8A,c and 8B,c) while a not significant reduction of angiogenesis was recorded in CG5 cells pre-treated with Dmab in presence of VEGF and TNFα (p = 0.08) (Fig. 8Ad and 8Bd). In contrast, hemoglobin content in the Matrigel plugs containing VEGF, TNFα and ZOL-pretreated CG5 cells was similar to the negative controls and about 5-fold lower than the positive controls (Fig. 8A,e and 8B,e), demonstrating a marked anti-angiogenic response with ZOL (p = 0.0008).
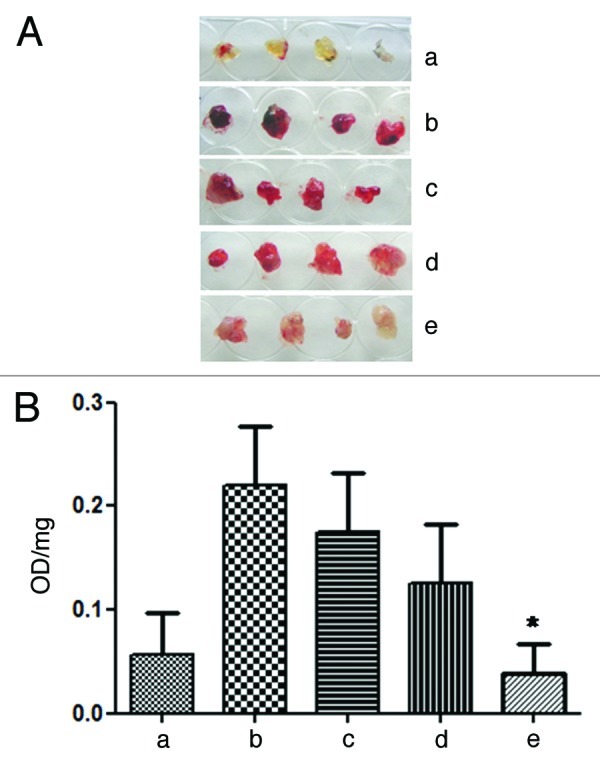
Figure 8. ZOL inhibits in vivo angiogenesis evaluated by matrigel plug assay. In vivo vessel formation was assessed after the injection of C57BL/6 mice with matrigel plugs containing heparin only (negative control) (a), containing heparin, VEGF and TNFα (positive control) (b), containing CG5 cells untreated (c) or previously treated with Denosumab at 100 μM (d) or ZOL at 100 μM (e) for 24 h in serum-free medium. After 5 d, animals were sacrificed and neovascularisation was evaluated by macroscopic analysis and by the measurement of Hb content of matrigel plugs. The macroscopic appearance of representative matrigel plugs from each experimental group is shown (A). Histograms represent the mean value (n = 10; data from two independent experiments) of the Hb content, expressed as absorbance (OD)/100 mg of matrigel plug. Bars: +SD values (B). Denosumab vs untreated: p = 0.08; ZOL vs. untreated p = 0.0008 (*).
In vivo antitumor effect
The in vivo potential anticancer activity of Dmab and ZOL was examined in athymic mice xenografted with the human breast cancer cell line CG5. The mean tumor weight was not significantly decreased in mice treated with Dmab for 42 d compared with untreated control vehicle-treated mice (p > 0.05) (Table 2, Figure 9). In contrast to Dmab, ZOL treatment caused a 44% reduction of the tumor weight if compared with untreated mice (p < 0.001). Interestingly, one out of 6 mice achieved a tumor stabilization and ZOL treatment induced also an increase of life survival (ILS) of 35% if compared with untreated mice (p = 0.002). On the other hand, Dmab did not induce any effect on tumor stabilization and caused an ILS of only 8% if compare with untreated mice (p > 0.05). The difference of the effects between ZOL and Dmab on ILS was statistically significant (p = 0.018). Maintenance of body weight across treatment arms suggests that both Dmab and ZOL did not have any adverse metabolic effects (data not shown).
Table 2. Therapeutic efficacy of Zoledronic Acid and Denosumab on CG5 breast cancer xenografts.
| Treatment groups# |
TWI* |
T-C § |
Stable disease∞/ |
ILS& |
Lethal |
|---|---|---|---|---|---|
| (%) | (days) | mice treated | (%) | toxicity° | |
|
ZOL |
44 |
7 |
6-Jan |
35 |
0/6 |
| Denosumab | - | 0 | 0/6 | 8 | 0/6 |
# CG5 tumor bearing-mice were treated starting from day 6 after tumor cells injection, as follows: a) ZOL at 20 μg/mouse i.v. three times a week for three consecutive weeks; b) Denosumab at 10 mg/Kg i.v. two times a week for three for four consecutive weeks. *Tumor weight inhibition was calculated at the nadir of the effect. Statistical significance of differences of tumor weight between each group are as follows: ZOL vs untreated, p = 0.013; ZOL vs Denosumab, p = 0.014. §Calculated as the median times for treated (T) and control (C) tumors to reach the same size (1000 mg). ∞Stable disease was defined as the maintenance of the same tumor weight for at least two weeks from the start of treatment. &Increase in lifespan. ILS of treated mice was calculated compared their median survival time (MST) with those of untreated mice. The animals were euthanized for ethical reasons when tumors reached a mean of 3.0 g in weight (the time of euthanization was recorded as the time of death). Statistical significance of differences of survival between each group are as follows: ZOL vs untreated, p = 0.002; ZOL vs Denosumab, p = 0.018. °Number of toxic deaths/total number of treated mice.
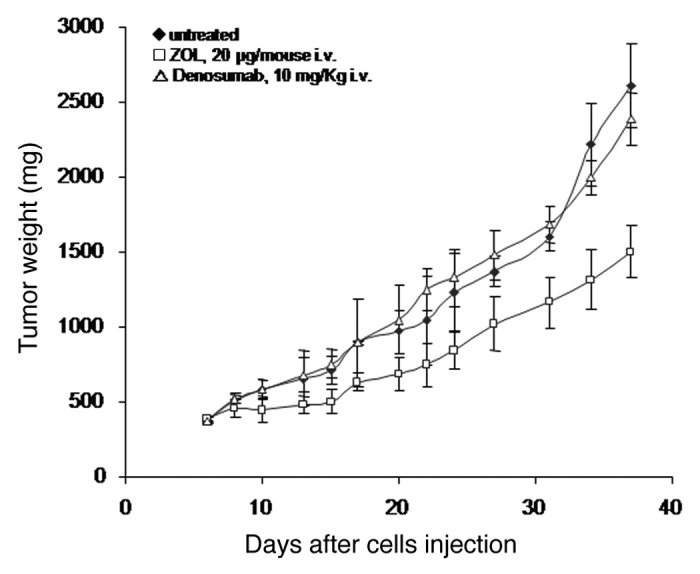
Figure 9. ZOL reduced the growth of CG5 xenografts. Nude mice were injected i.m. with 3x 106 CG5 cells/mouse and treatment started from day 6 after tumor cells injection. Groups: (♦) untreated; (□) ZOL, 20 μg/mouse i.v. (△) Denosumab, 10 mg/Kg i.v. Points are means with SD (bars).
Immunohistochemical determination of intratumor angiogenesis
The effect of Dmab and ZOL on the expression of CD34 as a marker of neo-vessel formation in the human xenografts was examined. The mean vessel counts in untreated tumors was 32 ± 3 and was almost unaltered in tumors treated with Dmab (30.3 ± 4, p = 0.526) (Table 3). On the other hand, treatment with ZOL caused a significant reduction of mean vessel count that reached the value of 16.8 ± 1 (p = 0.0001) providing biochemical support that ZOL, but not Dmab, inhibits tumor growth via an anti-angiogenic mechanism (Table 3). Some representative images of neo-vascularization are shown in Figure 10.
Table 3. Cd34 positive vessels.
| ZOL | Dmab | CTR | |
|---|---|---|---|
|
Mouse # 1 |
17 ± 3 |
31,6 ± 4 |
35,2 ± 4 |
|
Mouse # 2 |
16,3 ± 5 |
29,5 ± 5 |
31,7 ± 6 |
|
Mouse # 3 |
18,2 ± 7 |
34.4 ± 6 |
33,6 ± 5 |
|
Mouse # 4 |
15,8 ± 6 |
25,7 ± 5 |
27,4 ± 6 |
|
Mean SD |
16,8 ± 1 |
30,3 ± 4 |
32 ± 3 |
| p-value | 0,0001 | 0,526 |
Number vessels/hpf. Tumor sections were immunostained with anti-CD34 monoclonal antibody (mec 14.7 abnova). The number of vessels was evaluated over 10 sequential hpf (400× enlargement) chosen among the better vascularized areas of each tumor and reported as mean + sd/hpf.

Figure 10. Effect of ZOL on vascularization of breast cancer tumors xenografted in nude mice. Tumours were collected, fixed and paraffin embedded after 3 weeks of treatment of the animals with placebo (A) or Dmab (B) or ZOL (C). Thereafter, the expression of CD34 was evaluated and the vessel count was performed as described in the Materials and Methods section. Arrows indicate examples of vessels in the different treatment settings. The micrographs were obtained by observation with Zeiss microscope (400× magnification).
Discussion
In this study we demonstrate that ZOL, but not Dmab, induces time- and dose-dependent growth inhibition of human MDA-MB-436, CG5 cells and HUVECs. Additionally, Dmab failed to inhibit HUVEC capillary tubule formation or HUVEC cell invasion. Although there are conflicting data on the role of RANKL in angiogenesis, our current data are not consistent with a preclinical study in which RANKL inhibited proliferation of HUVECs and VEGF-induced angiogenesis and induced apoptosis in these cells.24 Taken together, these data suggest that inhibiting RANKL with Dmab is not antiangiogenic. In contrast, ZOL markedly inhibited both HUVEC tubule formation and cell invasion and inhibited endothelial and breast cancer cell proliferation. These results are also in agreement with previous reports regarding the antiangiogenic activity of ZOL.10,11,13
In agreement with the in vitro assays, no antiangiogenic activity was observed with Dmab in vivo. However, this is to be expected as Dmab specifically binds human RANKL and does not bind murine RANKL.28 Furthermore, as the Matrigel used in this assay was derived from mouse sarcoma, extracellular matrix proteins were of mouse origin. As a result, in this experiment Dmab treatment acted as a second positive control. As expected, ZOL treatment inhibited angiogenesis in Matrigel vascularization assays in vivo while Dmab had again not significant effects. These data provide further support for the potential in vivo antiangiogenic effect of ZOL, which may translate into clinical anticancer activity.
Denosumab had no effect on the growth of human xenografts in athymic nude mice and no effect on the expression of CD34 as a marker of angiogenesis in these xenografts. In contrast, treatment with ZOL caused a substantial reduction in xenograft tumor volume and marker levels. Although it is unknown if mouse RANKL influenced growth of the xenograft tumor, the implanted breast cancer cells were of human origin and therefore expressed human RANKL. Thus, Dmab would be able to bind the RANKL expressed by the xenografts and potential anticancer activity should be observed by reduction in tumor size. Therefore, RANKL inhibition with Dmab does not appear to have anticancer activity against breast cancer tumors.
Overall, these data suggest that Dmab does not have antiangiogenic activity and provide additional support for the antiangiogenic activity of ZOL reported in other preclinical and clinical studies.29-31 However, a limitation of this study is the use of mice that do not express human RANKL. For example, a knock-in mouse model that expresses chimeric (murine/human) RANKL has been created.28 Moreover, this model was used to demonstrate that Dmab inhibits bone resorption and increases BMD, as has been shown in clinical trials with osteoporosis.7,28,32 Additional studies examining the effects of Dmab in such a mouse model will help clarify the role of RANKL inhibition in angiogenesis.
Materials and Methods
Materials
Dulbecco's Modified Eagle Medium (DMEM), bovine serum albumin (BSA) and fetal bovine serum (FBS) were purchased from Flow Laboratories. Tissue culture dishes were purchased from Becton Dickinson. Zoledronic acid1 was kindly provided as the hydrated disodium salt by Novartis Pharma AG. The neutralized sodium salt of ZOL was dissolved in sterile distilled deionized water (ddH2O) and aliquots of this stock solution were stored at ‑20°C. Denosumab was purchased from GlaxoSmithKline SpA (GSK).2
Cell culture
The experimental models consisted of the human breast cancer cell lines MDA-MB-436 and CG5 (both from American Type Tissue Culture Collection, Rockville, MD) and of human umbilical vein endothelial cells HUVECs (a kind gift from Dr. M. Festa). MDA-MB-436 and CG5 cells were grown in DMEM supplemented with 10% heat-inactivated FBS, 20 mM HEPES, 100 U/mL penicillin, 100 μg/mL streptomycin, 1% L-glutamine and 1% sodium pyruvate. The HUVECs were grown in endothelial cell growth medium-2 (EGM-2) with supplements and growth factors supplied by the vendor (Lonza). Both cell lines were grown in a humidified atmosphere at 37°C and 5% CO2.
Cell viability assay
Cells were seeded in serum-containing media in 96-well plates at 2.5 × 103 cells/well for MDA-MB-436 cells, 1.8 × 103 cells/well for CG5 and 4 × 103 cells/well for HUVECs. On the bases of preliminary experiments, after 24 h incubation at 37°C, the cells were treated with increasing concentrations of Dmab or ZOL (0.31 to 160 μM for both Dmab and ZOL) for 24, 48 and 72 h. Cell viability was assessed by adding MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide] solution in phosphate-buffered saline (PBS) to a final concentration of 5 mg/mL. The plates were then incubated at 37°C for an additional 4 h and the MTT-formazan crystals were solubilized in 1N isopropanol/hydrochloric acid 10% solution at 37°C on a shaking table for 20 min. The absorbance values of the solution in each well were measured at 570 nm using a Bio-Rad 550 microplate reader (Bio-Rad Laboratories, Milan, Italy). Percentage cell viability was calculated as 100% × (absorbance of the treated wells – absorbance of the blank control wells) / (absorbance of the negative control wells – absorbance of the blank control wells). All MTT experiments were performed in triplicate and repeated at least 3 times. Half maximum inhibitory concentration (IC50) values are presented as mean ± standard deviation (SD).
Tubule formation assay
To study the effect of Dmab and ZOL on angiogenesis in vitro, HUVECs were seeded on Matrigel (BD Biosciences). Briefly, 30 μL of Matrigel was pipetted into each well of a 96-well cell culture plate and incubated for 30 min at 37°C. Dissociated HUVECs were seeded on the Matrigel layer at a density of 8.5 × 103 cells/well. Next, Dmab or ZOL was added at increasing concentrations (0.31 to 160 μM). Then, Matrigel cultures were incubated at 37°C. After 24 h of incubation, tube formation was photographed (magnification 10 × ) under a phase-contrast microscope and the area covered by the tubule network was quantified using ImageJ (National Institutes of Health).
Animals
All procedures involving the animals were performed in accordance with the Institutional Guidelines and complied with the Italian D.L. no.116 of January 27, 1992 of Ministero della Salute and associated guidelines in the European Communities Council Directive of November 24, 1986 (86/609/ECC).
Invasion assay
For the invasion assay, 5 × 105 HUVEC cells were plated in the top chamber of uncoated polyethylene terephthalate (PET) membrane-covered dishes (6-well insert, pore size 8 μm; Becton Dickinson). Matrigel (100 μL of a 1 mg/mL dilution in serum-free DMEM medium) was placed on the lower side of each insert (6-well insert, pore size 8 μm; Becton Dickinson). The insert and the plate were incubated overnight at 4°C. The following day, cells were harvested and suspended in DMEM (containing 0.31 to 160 μM Dmab or ZOL) at a density of 1 × 106 cells/mL. The inserts were washed with serum-free DMEM, then 1 × 106 cells were added to each insert and 3 mL of DMEM containing 10% FBS was added to the well underneath the insert. After incubation at 37°C for up to 24 h, the inner side of the insert was wiped with a wet swab to remove the cells. The outer side of the insert was rinsed gently with PBS, stained with 0.25% crystal violet for 10 min, rinsed again and then allowed to dry. Next, the inserts were viewed under a CCD camera-equipped Nikon microscope. The inserts were processed and cell labeling was detected using a spectrophotometer. Crystal violet was extracted with 900 μL of 0.1 M sodium citrate in 50% ethanol and the absorbance was measured at 585 nm.
In vivo Angiogenesis assay
Eight week-old C57BL/6 (Charles River) mice were injected subcutaneously (s.c.) in the flank with 600 μl of matrigel (BD Biosciences). Positive control contained matrigel supplemented with VEGF (100 ng/ml) (R&D Systems), TNFα 2 ng/ml (R&D Systems) and heparin (19 U; Schwarz Pharma SpA). Negative controls contained heparin alone.
Cells CG5 (3 × 106/ samples) untreated and treated with either Denosumab or with Zoledronic Acid at a dose of 100 μM for 24 h in serum-free medium were added to matrigel. Each group consisted of five animals.
After 5 d mice were sacrificed and matrigel plugs were harvested. The angiogenic response was evaluated by macroscopic analysis of the plug at autopsy and by measurement of the Hemoglobin (Hb) content into the pellet of matrigel.
Hb was mechanically extracted from the pellets in water and measured using the Drabkin (Sigma-Aldrich) method by spectrophotometric analysis at 540 nm. Values were expressed as optical density (OD)/100 mg of matrigel.
Analysis of in vivo therapeutic efficacy
CD-1 male nude (nu/nu) mice, 6–8 weeks old and weighing 22–24 g were purchased from Charles River Laboratories. All procedures involving animals and their care were conducted in conformity with the institutional guidelines, which are in compliance with national and international laws.
Immunosuppressed mice were injected intramuscularly (i.m.) into the hind leg muscles of mice at 3 × 106 CG5 breast cancer cells /mouse. After 6 d (when a tumor mass of about 300 mg was evident) mice were randomized, divided in three groups and treatment started.
Mice were treated intravenously (i.v.) with ZOL at 20 μg/ mouse for three times a week for 3 consecutive weeks or with Dmab at 10 mg/Kg twice a week for 4 consecutive weeks.
Tumor sizes were measured three times a week in two dimensions by a caliper and tumor weight was calculated using the following formula: a × b2/2, where a and b are the long and short diameter of the tumor, respectively. Antitumor efficacy of treatments was assessed by the following end points: (a) %TWI, percent tumor weight inhibition; (b) tumor growth delay, evaluated as T-C, where T and C are the median times for treated and control tumors, respectively, to achieve equivalent size; (c) stable disease, defined as the maintenance of the same tumor weight for at least two weeks from the start of treatment ; (d) increase of mice survival. The animals were euthanized for ethical reasons when tumors reached a mean of 3.0 g in weight (the time of euthanization was recorded as the time of death).
Immunohistochemistry
Tumors were harvested, fixed in formaldehyde and embedded in paraffin for immunohistochemistry. Briefly, 3- to 5-μm sections from each specimen were mounted on glass and dried overnight at 37°C. Sections were then deparaffinized in xylene, rehydrated with a graded alcohol series and equilibrated in PBS (used for all subsequent washes and antibody dilutions). Antigen retrieval was performed by heating tissue sections in a microwave oven (700 W) for 2 × 5 min in citrate buffer (pH 6) and then processed using the standard streptavidin-biotin-immunoperoxidase method (DAKO Universal Kit, DAKO Corporation). Mouse monoclonal antibody raised against CD34, was used as primary antibody (CD34 monoclonal antibody, clone MEC 14.7, Abnova).
Diaminobenzidine was used as the final chromogen and hematoxylin as the nuclear counterstain. Negative controls lacked the primary antibody and were performed for each tissue section. The specificity of staining also was confirmed via competition of the primary antibody with the respective peptide against which they were generated. All samples were processed under the same conditions. Two pathologists (AS and FDC) independently evaluated the staining pattern of the vessels and the number of vessels was evaluated over 10 sequential hpf (400× enlargement) chosen among the better vascularized areas of each tumor and reported as mean + sd/hpf. All samples were processed as previously described.27
Statistical analysis
The Student’s t-test (unpaired, two-tailed) was used for comparing statistical differences. Survival curves of mice were generated by Kaplan–Maier product-limit estimate and statistical differences between the various groups were evaluated by log-rank analysis with Yates correction (software Primer of Biostatistics, McGraw-Hill). Differences were considered statistically significant when p < 0.05.
Conclusions
These findings support the potential antiangiogenic activity of ZOL in vitro and in vivo. ZOL has, in fact, shown promising clinical activity against both bone tumor control33 and improvement in the quality of life of patients with bone metastases.34 The in vitro data do not rule out an antiangiogenic role of RANKL, or that RANKL inhibition could promote angiogenesis. Therefore, additional studies need to be performed to clarify the effects of Dmab on angiogenesis.
Acknowledgments
We thank Duprane Pedaci Young, PhD, ProEd Communications, Inc., for her medical editorial assistance with this manuscript. M.C. received support by MIUR (PRIN 2009).
Footnotes
Previously published online: www.landesbioscience.com/journals/cbt/article/22274
References
- 1.Zometa (zoledronic acid) [package insert] (2011) Novartis Pharmaceuticals Corporation, East Hanover, NJ.
- 2.Xgeva (denosumab) [package insert] (2010) Amgen Inc., Thousand Oaks, CA.
- 3.Brufsky AM, Harker WG, Beck JT, Bosserman L, Vogel C, Seidler C, et al. Final 5-year results of Z-FAST trial: adjuvant zoledronic acid maintains bone mass in postmenopausal breast cancer patients receiving letrozole. Cancer. 2012;118:1192–201. doi: 10.1002/cncr.26313. [DOI] [PubMed] [Google Scholar]
- 4.Eidtmann H, de Boer R, Bundred N, Llombart-Cussac A, Davidson N, Neven P, et al. Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST Study. Ann Oncol. 2010;21:2188–94. doi: 10.1093/annonc/mdq217. [DOI] [PubMed] [Google Scholar]
- 5.Gnant M, Mlineritsch B, Luschin-Ebengreuth G, Kainberger F, Kässmann H, Piswanger-Sölkner JC, et al. Austrian Breast and Colorectal Cancer Study Group (ABCSG) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 5-year follow-up of the ABCSG-12 bone-mineral density substudy. Lancet Oncol. 2008;9:840–9. doi: 10.1016/S1470-2045(08)70204-3. [DOI] [PubMed] [Google Scholar]
- 6.Llombart A, Frassoldati A, Paija O, Sleeboom HP, Jerusalem G, Mebis J, et al. Immediate Administration of Zoledronic Acid Reduces Aromatase Inhibitor-Associated Bone Loss in Postmenopausal Women With Early Breast Cancer: 12-month analysis of the E-ZO-FAST trial. Clin Breast Cancer. 2012;12:40–8. doi: 10.1016/j.clbc.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Ellis GK, Bone HG, Chlebowski R, Paul D, Spadafora S, Smith J, et al. Randomized trial of denosumab in patients receiving adjuvant aromatase inhibitors for nonmetastatic breast cancer. J Clin Oncol. 2008;26:4875–82. doi: 10.1200/JCO.2008.16.3832. [DOI] [PubMed] [Google Scholar]
- 8.Hershman DL, McMahon DJ, Crew KD, Shao T, Cremers S, Brafman L, et al. Prevention of bone loss by zoledronic acid in premenopausal women undergoing adjuvant chemotherapy persist up to one year following discontinuing treatment. J Clin Endocrinol Metab. 2010;95:559–66. doi: 10.1210/jc.2009-1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shapiro CL, Halabi S, Hars V, Archer L, Weckstein D, Kirshner J, et al. Zoledronic acid preserves bone mineral density in premenopausal women who develop ovarian failure due to adjuvant chemotherapy: final results from CALGB trial 79809. Eur J Cancer. 2011;47:683–9. doi: 10.1016/j.ejca.2010.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coxon JP, Oades GM, Kirby RS, Colston KW. Zoledronic acid induces apoptosis and inhibits adhesion to mineralized matrix in prostate cancer cells via inhibition of protein prenylation. BJU Int. 2004;94:164–70. doi: 10.1111/j.1464-4096.2004.04831.x. [DOI] [PubMed] [Google Scholar]
- 11.Fournier P, Boissier S, Filleur S, Guglielmi J, Cabon F, Colombel M, et al. Bisphosphonates inhibit angiogenesis in vitro and testosterone-stimulated vascular regrowth in the ventral prostate in castrated rats. Cancer Res. 2002;62:6538–44. [PubMed] [Google Scholar]
- 12.Santini D, Vincenzi B, Galluzzo S, Battistoni F, Rocci L, Venditti O, et al. Repeated intermittent low-dose therapy with zoledronic acid induces an early, sustained and long-lasting decrease of peripheral vascular endothelial growth factor levels in cancer patients. Clin Cancer Res. 2007;13:4482–6. doi: 10.1158/1078-0432.CCR-07-0551. [DOI] [PubMed] [Google Scholar]
- 13.Wood J, Bonjean K, Ruetz S, Bellahcène A, Devy L, Foidart JM, et al. Novel antiangiogenic effects of the bisphosphonate compound zoledronic acid. J Pharmacol Exp Ther. 2002;302:1055–61. doi: 10.1124/jpet.102.035295. [DOI] [PubMed] [Google Scholar]
- 14.Marra M, Abbruzzese A, Addeo R, Del Prete S, Tassone P, Tonini G, et al. Cutting the limits of aminobisphosphonates: new strategies for the potentiation of their anti-tumour effects. Curr Cancer Drug Targets. 2009;9:791–800. doi: 10.2174/156800909789760285. [DOI] [PubMed] [Google Scholar]
- 15.Caraglia M, Marra M, Naviglio S, Botti G, Addeo R, Abbruzzese A. Zoledronic acid: an unending tale for an antiresorptive agent. Expert Opin Pharmacother. 2010;11:141–54. doi: 10.1517/14656560903485664. [DOI] [PubMed] [Google Scholar]
- 16.Green JR. Bisphosphonates: preclinical review. Oncologist. 2004;9(Suppl 4):3–13. doi: 10.1634/theoncologist.9-90004-3. [DOI] [PubMed] [Google Scholar]
- 17.Mundy GR. Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer. 2002;2:584–93. doi: 10.1038/nrc867. [DOI] [PubMed] [Google Scholar]
- 18.Fritz G. Targeting the mevalonate pathway for improved anticancer therapy. Curr Cancer Drug Targets. 2009;9:626–38. doi: 10.2174/156800909789057033. [DOI] [PubMed] [Google Scholar]
- 19.Fizazi K, Bosserman L, Gao G, Skacel T, Markus R. Denosumab treatment of prostate cancer with bone metastases and increased urine N-telopeptide levels after therapy with intravenous bisphosphonates: results of a randomized phase II trial. J Urol. 2009;182:509–15, discussion 515-6. doi: 10.1016/j.juro.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 20.Fizazi K, Lipton A, Mariette X, Body JJ, Rahim Y, Gralow JR, et al. Randomized phase II trial of denosumab in patients with bone metastases from prostate cancer, breast cancer, or other neoplasms after intravenous bisphosphonates. J Clin Oncol. 2009;27:1564–71. doi: 10.1200/JCO.2008.19.2146. [DOI] [PubMed] [Google Scholar]
- 21.Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol. 2010;28:5132–9. doi: 10.1200/JCO.2010.29.7101. [DOI] [PubMed] [Google Scholar]
- 22.Boyle WJ, Simonet WS, Lacey DL. Osteoclast differentiation and activation. Nature. 2003;423:337–42. doi: 10.1038/nature01658. [DOI] [PubMed] [Google Scholar]
- 23.Rogers MJ, Gordon S, Benford HL, Coxon FP, Luckman SP, Monkkonen J, et al. Cellular and molecular mechanisms of action of bisphosphonates. Cancer. 2000;88(Suppl):2961–78. doi: 10.1002/1097-0142(20000615)88:12+<2961::AID-CNCR12>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 24.McGonigle JS, Giachelli CM, Scatena M. Osteoprotegerin and RANKL differentially regulate angiogenesis and endothelial cell function. Angiogenesis. 2009;12:35–46. doi: 10.1007/s10456-008-9127-z. [DOI] [PubMed] [Google Scholar]
- 25.Min JK, Cho YL, Choi JH, Kim Y, Kim JH, Yu YS, et al. Receptor activator of nuclear factor (NF)-kappaB ligand (RANKL) increases vascular permeability: impaired permeability and angiogenesis in eNOS-deficient mice. Blood. 2007;109:1495–502. doi: 10.1182/blood-2006-06-029298. [DOI] [PubMed] [Google Scholar]
- 26.Min JK, Kim YM, Kim YM, Kim EC, Gho YS, Kang IJ, et al. Vascular endothelial growth factor up-regulates expression of receptor activator of NF-kappa B (RANK) in endothelial cells. Concomitant increase of angiogenic responses to RANK ligand. J Biol Chem. 2003;278:39548–57. doi: 10.1074/jbc.M300539200. [DOI] [PubMed] [Google Scholar]
- 27.Caraglia M, Tagliaferri P, Marra M, Giuberti G, Budillon A, Gennaro ED, et al. EGF activates an inducible survival response via the RAS-> Erk-1/2 pathway to counteract interferon-alpha-mediated apoptosis in epidermoid cancer cells. Cell Death Differ. 2003;10:218–29. doi: 10.1038/sj.cdd.4401131. [DOI] [PubMed] [Google Scholar]
- 28.Kostenuik PJ, Nguyen HQ, McCabe J, Warmington KS, Kurahara C, Sun N, et al. Denosumab, a fully human monoclonal antibody to RANKL, inhibits bone resorption and increases BMD in knock-in mice that express chimeric (murine/human) RANKL. J Bone Miner Res. 2009;24:182–95. doi: 10.1359/jbmr.081112. [DOI] [PubMed] [Google Scholar]
- 29.Costa L, Harper P, Coleman RE, Lipton A. Anticancer evidence for zoledronic acid across the cancer continuum. Crit Rev Oncol Hematol. 2011;77(Suppl 1):S31–7. doi: 10.1016/S1040-8428(11)70006-3. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton E, Clay TM, Blackwell KL. New perspectives on zoledronic acid in breast cancer: potential augmentation of anticancer immune response. Cancer Invest. 2011;29:533–41. doi: 10.3109/07357907.2011.605413. [DOI] [PubMed] [Google Scholar]
- 31.Winter MC, Holen I, Coleman RE. Exploring the anti-tumour activity of bisphosphonates in early breast cancer. Cancer Treat Rev. 2008;34:453–75. doi: 10.1016/j.ctrv.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Anastasilakis AD, Toulis KA, Goulis DG, Polyzos SA, Delaroudis S, Giomisi A, et al. Efficacy and safety of denosumab in postmenopausal women with osteopenia or osteoporosis: a systematic review and a meta-analysis. Horm Metab Res. 2009;41:721–9. doi: 10.1055/s-0029-1224109. [DOI] [PubMed] [Google Scholar]
- 33.Addeo R, Nocera V, Faiola V, Vincenzi B, Ferraro G, Montella L, et al. Management of pain in elderly patients receiving infusion of zoledronic acid for bone metastasis: a single-institution report. Support Care Cancer. 2008;16:209–14. doi: 10.1007/s00520-007-0315-y. [DOI] [PubMed] [Google Scholar]
- 34.Vitale G, Fonderico F, Martignetti A, Caraglia M, Ciccarelli A, Nuzzo V, et al. Pamidronate improves the quality of life and induces clinical remission of bone metastases in patients with thyroid cancer. Br J Cancer. 2001;84:1586–90. doi: 10.1054/bjoc.2001.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]