Abstract
We recently have shown that selective growth of transplanted normal hepatocytes can be achieved in a setting of cell cycle block of endogenous parenchymal cells. Thus, massive proliferation of donor-derived normal hepatocytes was observed in the liver of rats previously given retrorsine (RS), a naturally occurring alkaloid that blocks proliferation of resident liver cells. In the present study, the fate of nodular hepatocytes transplanted into RS-treated or normal syngeneic recipients was followed. The dipeptidyl peptidase type IV-deficient (DPPIV−) rat model for hepatocyte transplantation was used to distinguish donor-derived cells from recipient cells. Hepatocyte nodules were chemically induced in Fischer 344, DPPIV+ rats; livers were then perfused and larger (>5 mm) nodules were separated from surrounding tissue. Cells isolated from either tissue were then injected into normal or RS-treated DPPIV− recipients. One month after transplantation, grossly visible nodules (2–3 mm) were seen in RS-treated recipients transplanted with nodular cells. They grew rapidly, occupying 80–90% of the host liver at 2 months, and progressed to hepatocellular carcinoma within 4 months. By contrast, no liver nodules developed within 6 months when nodular hepatocytes were injected into the liver of recipients not exposed to RS, although small clusters of donor-derived cells were present in these animals. Taken together, these results directly point to a fundamental role played by the host environment in modulating the growth and the progression rate of altered cells during carcinogenesis. In particular, they indicate that conditions associated with growth constraint of the host tissue can drive tumor progression in vivo.
Current cancer research focuses mainly on genetic abnormalities to explain the acquisition of malignant phenotypic properties by a target cell population. However, increasing evidence points to a relevant role played by an altered host environment during cancer development at various stages and in different systems (1–11). For example, primary alterations in the stroma, leading to disruption of the normal epithelial-stromal interactions, have been implicated in the pathogenesis of some epithelial cancers, including bladder (12, 13) and mammary cancer (14, 15). More recently, host-derived factors have also been proposed to contribute to the acquisition of an invasive and metastatic phenotype (16). Furthermore, the importance of field cancerization, defined as the pathological and genetic changes that are found in the tissue peripheral to a tumor (17), is slowly emerging in clinical oncology (18–20). It has also been proposed that an evaluation of this parameter, when feasible, would be relevant to the staging of tumors, at least in some organs (17). This in turn highlights the need to study and to better define any specific type(s) of alteration(s) in the host environment that can be directly related to the pathogenesis of cancer in any system.
Over the years, experimental models involving cell transplantation (Tx) have unequivocally demonstrated a role of the local environment in tumor development. For example, a few decades ago preirradiation of lung was shown to enhance artificial pulmonary metastasis in mice (2, 3). More recently, McCullough et al. (6) have reported that aging can affect cancer development via modifications induced in the microenvironment outside the tumor. A liver-derived transformed cell line was reported to induce tumors when injected into the liver of aged animals, whereas the liver of young recipients did not support the neoplastic growth of the same cell population (6). Similarly, Barcellos-Hoff and Ravani (15) have provided evidence to indicate that ionizing radiation, a known carcinogen able to both initiate and promote neoplastic development, can act, at least in part, by affecting the tissue environment in the host. When a p53-mutated cell line was transplanted into either preirradiated or nonirradiated epithelial-free mammary stroma of rats, tumors developed more rapidly and at higher incidence in the irradiated side (15).
We have recently developed a model for hepatocyte Tx in the rat wherein selective proliferation of transplanted cells takes place in a setting of persistent growth inhibition of the endogenous liver (21–23). Rats are exposed to retrorsine (RS), a pyrrolizidine alkaloid which blocks the hepatocyte cell cycle (22), and then transplanted with hepatocytes isolated from a normal donor. Under these conditions, donor-derived cells were able to replace >90% of the host liver within a few months (21, 23). However, virtually no growth of transplanted normal hepatocytes occurs in the liver of syngeneic untreated recipients (21).
Based on the above, the present study was undertaken to investigate whether such a growth-constrained environment induced by RS, which allows proliferation of transplanted normal cells, would also affect the rate of growth and/or progression of transplanted altered hepatocytes isolated from chemically induced liver nodules. We found that isolated nodular hepatocytes can rapidly grow and progress to hepatocellular carcinoma when transplanted into animals exposed to RS. By contrast, no significant growth of those cells was seen after Tx into untreated syngeneic recipients.
Materials and Methods
Animals.
All animals were maintained on daily cycles of alternating 12-h light/darkness with food and water available ad libitum. They were fed Purina Rodent Lab Chow diet throughout the experiment and received humane care according to the criteria outlined in the National Institutes of Health Publication 86-23, revised 1985.
Induction of Liver Nodules in Donor Rats and Isolation of Hepatocytes.
Hepatocyte nodules were induced according to a well characterized experimental model in the rat (24). Two-month-old male Fischer 344 rats (Charles River Breeding Laboratories) were injected with a single initiating dose of diethylnitrosamine (200 mg/kg body weight i.p.; Sigma) followed, 3 weeks later, by exposure to a modified version of the Solt and Farber protocol (24) to stimulate the growth of hepatocyte foci and nodules. Such protocol consisted of three consecutive daily doses of 2-acetylaminofluorene (20 mg/kg body weight, given by gavage tube; Sigma) followed, on the fourth day, by a single administration of CCl4 (0.2 ml/kg body weight, by gavage, mixed in corn oil, 1:1 vol/vol). Six months after the initial treatment, livers were perfused according to a standard two-step collagenase perfusion technique (25). Typically, 3–5 large (5–10 mm) persistent nodules are present in the liver at this time point using the above experimental protocol. They express increased levels of the marker enzyme glutathione S-transferase (GST) 7-7 (26), and this was confirmed in a parallel set of experiments (data not reported). When left in situ, a subgroup of these nodules (an average of one or two per animal), will progress to cancer within 1 year (27). Large (>5 mm) nodules were physically separated from surrounding tissue and cells isolated from either tissue were suspended in Williams E culture medium (Sigma catalog no. W-4125) and prepared for Tx experiments. Cell viability, determined by trypan blue dye exclusion, was ≈75% in the nodular cell preparation, whereas it was slightly higher (≈80%) in hepatocytes isolated from surrounding tissue.
Treatment of Recipient Rats and Tx of Hepatocytes.
To follow the fate of donor hepatocytes into the recipient liver, the dipeptidyl peptidase type IV-deficient (DPPIV−) rat model was used (28). In this system, cells isolated from a Fischer 344 rat expressing DPPIV (DPPIV+) are transplanted into a syngeneic DPPIV− recipient, such that donor-derived cells can be detected in the host liver through a simple histochemical technique. A colony of DPPIV− F344 rats has been established in our laboratory at the Department of Medical Sciences and Biotechnology, University of Cagliari (23). DPPIV− recipient rats were treated according to a RS-based protocol recently developed by our group (22). Briefly, a group of 18 F344 DPPIV− rats, weighing 80–100 g, were given two injections of RS (Sigma), 30 mg/kg each, i.p., 2 weeks apart (group I). Such protocol is able to impose a persistent inhibition on hepatocyte proliferation, both in response to partial hepatectomy (PH) (22) and under conditions of normal tissue growth and turnover (23). For example, liver size and liver DNA content were significantly reduced in animals treated with RS and killed as long as 8 months after exposure (23). A second group of 18 DPPIV− rats was given injections of an equal volume of 0.9% NaCl solution instead of RS (group II). Two weeks after the last injection, each group was divided into two subgroups (A and B, of 10 and eight animals each, respectively) and received 3 × 105 cells freshly isolated from hepatocyte nodules (groups IA and IIA) or 5 × 105 cells isolated from surrounding liver (groups IB and IIB). Cells were isolated as described above and were delivered via portal vein infusion, suspended in 0.3 ml of Williams E medium. Animals from various groups were killed at different intervals after Tx, as indicated in Results. Livers were excised, cut into 1–2-mm-thick slices, and grossly examined for the presence of hepatic nodules and/or any other apparent lesions. Liver samples with nodules and/or random samples taken from each liver were fixed in 10% buffered formaldehyde for standard histological analysis [hematoxylin/eosin (H&E) staining] or snap-frozen. Histochemical determination of DPPIV enzyme activity and quantitation of DPPIV+ areas in the liver were performed as described (19, 21). GST 7-7 was detected by an immunohistochemical method (23).
Results
Rapid Growth and Progression to Cancer of Isolated Nodular Hepatocytes Transplanted into the Liver of Rats Pretreated with RS.
Grossly visible nodules (3–5 per liver) were already present in the liver of three rats treated with RS followed by Tx of nodular hepatocytes (group IA) and killed 1 month later. Nodules were generally round and measured 2–3 mm. Histochemical analysis for DPPIV revealed the presence of numerous clusters of donor-derived DPPIV+ hepatocytes (15–20 per cm2), comprising 10–30 cells per cluster per cross section; however, a few larger clusters contained up to 300 hepatocytes per cross section and corresponded to the grossly visible nodules described above (data not shown). Histologically (H&E) the liver was mostly (>90%) composed of enlarged parenchymal cells (megalocytes), as described in previous reports, whereas the remaining parenchyma (<10% of total section) consisted of scattered foci of small hepatocytes.
Three more rats from this group were killed at 2 months after Tx. In all animals, the liver was almost entirely nodular in appearance, with 80–90% of its volume occupied by large tumors, up to 2.5 cm in size (Fig. 1 a and b). Histochemical staining for DPPIV confirmed that hepatocytes in nodules were from donor origin; however, the pattern of DPPIV enzyme distribution was different from that of normal liver (Fig. 2a), consistent with other reports (29). These nodules were also positive for the expression of the marker enzyme GST 7-7, as expected (see Fig. 1 a and b). Standard histological analysis (H&E) revealed alterations similar to those described in primary hepatocyte nodules induced by chemical carcinogens (Fig. 2b). Nodular lesions were mostly eosinophilic, with some areas of intense cytoplasmic basophilia. Mitotic figures in the nodules were common and were associated with high levels of cell death. Hepatocytes were arranged in many-cell thick plates, with reduced numbers of portal vein branches and bile duct structures; no evidence of lobular organization in the liver was observed. Residual surrounding parenchyma of recipient origin (DPPIV−) was confined mostly to the edges of the liver lobes and appeared to be compressed by the expanding nodules.
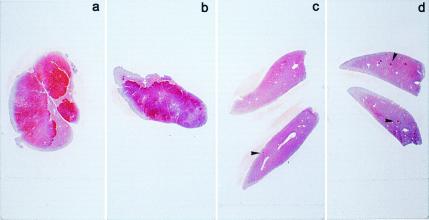
Figure 1.
Immunohistochemical staining for GST 7-7 (red) of liver sections from rats killed at 2 months after Tx. (a and b) Group IA: 80–90% of the liver was positive for GST 7-7. (c) Group IIA: Small positive foci are present (arrowhead). (d) group IB: A few GST 7-7-positive foci were detected (arrowheads); see text for details.
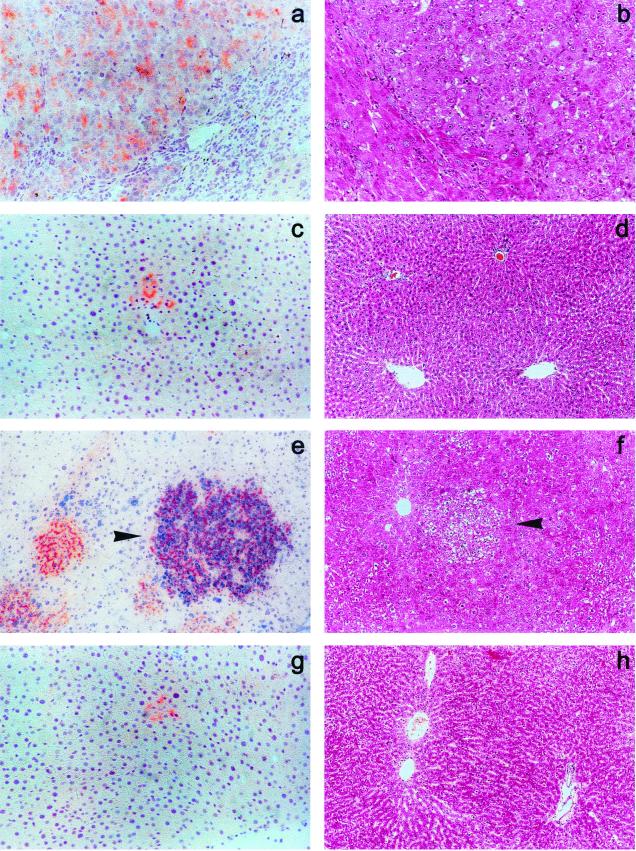
Figure 2.
All liver samples are from rats killed at 2 months after Tx. (a and b) Group IA. (a) Histochemical staining for DPPIV (orange) showing the edge of a large nodule expressing the enzyme activity; residual recipient liver is at the bottom right. (b) H&E-stained section representing a large nodule surrounded by residual megalocytic hepatocytes showing signs of compression (bottom left). (c and d) Group IIA. (c) Small cluster of DPPIV+ donor-derived hepatocytes. (d) H&E-stained section showing normal liver structure. (e and f) Group IB. (e) Dual histochemical/immunohistochemical staining for DPPIV (orange) and GST 7-7 (blue) demonstrating the presence of clusters of donor-derived hepatocytes (DPPIV+), some of which also expressed GST 7-7 (arrowhead). (f) Foci of altered hepatocytes (arrowhead) were easily discerned on H&E-stained sections. (g and h) Group IIB. (g) A small cluster of donor-derived (DPPIV+) hepatocytes is present. (h) H&E-stained section consistent with a normal liver architecture. (Original magnification ×100.)
By 4 months after Tx, progression to overt neoplasia was observed in three of four rats treated with RS followed by injection of nodular cells. Relative liver weight was up to 10% of body weight (normal range, 3–3.5%) and the diagnosis of hepatocellular carcinoma was histologically confirmed (Fig. 3a). Furthermore, cancer cells were positive for the expression of DPPIV enzyme (Fig. 3b), indicating their origin from transplanted nodular hepatocytes.
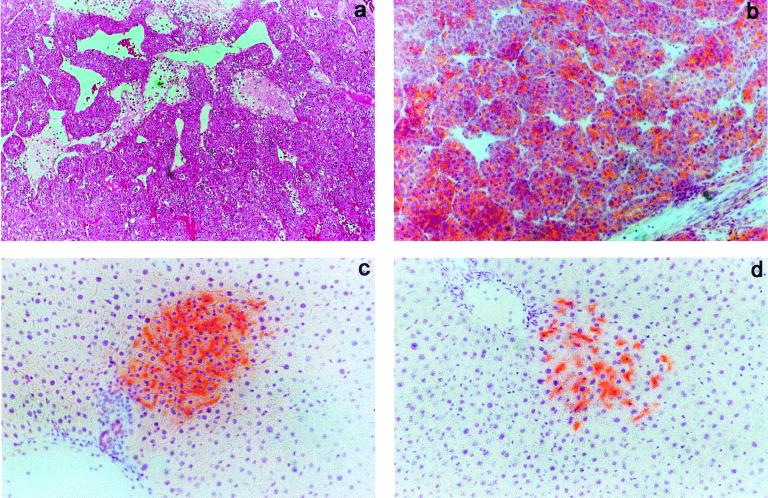
Figure 3.
(a and b) Liver samples from a rat in group IA killed 4 months after Tx. (a) H&E-stained section showing a well differentiated hepatocellular carcinoma with areas of necrosis. (b) Histochemical staining for DPPIV (orange) documenting that the cancer cell population was positive for the enzyme, i.e., it was from donor origin. (c) Liver sample from a rat in group IIA killed 6 months after Tx; the animal underwent two-thirds PH 2 months before killing. Histochemical staining for DPPIV (orange) revealed that donor-derived hepatocyte clusters were still present in these animals; however, their growth was very limited. (d) Liver sample from a rat in group IIB killed 6 months after Tx; the animal underwent two-thirds PH 2 months before killing. Staining for DPPIV enzyme activity documented the persistence of donor-derived cell clusters. (Original magnification ×100.)
Lack of Growth of Isolated Nodular Hepatocytes Transplanted into the Liver of Syngeneic Rats Not Treated with RS.
The pattern of results was remarkably different when the same preparation of nodular hepatocytes was injected into the liver of syngeneic untreated hosts (group IIA). No grossly visible nodules were observed in the liver of animals killed at 2 or 4 months after Tx (three animals were considered at each time point, Fig. 1c). Histochemical analysis for DPPIV confirmed and extended the above findings. Rare (1–2 per cm2) DPPIV-expressing cells were found isolated or in small clusters (up to five cells per cluster per cross section) in the liver of animals killed at 2 months (Fig. 2c). In addition, no increase in number and/or size of clusters was evident in samples taken at 4 months after Tx. Standard histological analysis was also consistent with the presence of a normal liver architecture throughout the organ (Fig. 2d).
We further investigated whether an exogenous growth stimulus, such as two-thirds PH (30), would trigger proliferation of transplanted nodular cells in untreated recipients. To this end, PH was performed in four rats at 4 months after Tx and animals were killed 2 months later. However, no visible hepatocyte nodules developed in these animals, although a moderate increase in the size of DPPIV+ clusters (to a maximum of 40–50 cells per cluster per cross section, mean 20–25 cells per cluster) was seen on histochemical examination (Fig. 3c).
The Growth of Hepatocytes Isolated from Surrounding Tissue and Transplanted into Rats Pretreated with RS.
In a parallel study, rats pretreated with RS were transplanted with hepatocytes isolated from the liver-surrounding nodules (group IB). Cell suspension of surrounding hepatocytes was prepared as described in Materials and Methods. Two animals were killed at 1 month, while three animals each were killed at 2 and 4 months after cell Tx, respectively.
Macroscopic examination of the liver was negative for the presence of any hepatic nodule at any time point considered (Fig. 1d). However, histochemical analysis for DPPIV revealed that cells isolated from surrounding liver were also able to proliferate upon Tx into rats treated with RS. Significant growth of DPPIV+ cells was already evident at 1 month after Tx; clusters of donor-derived hepatocytes were present throughout the parenchyma (10–15 per cm2) and contained 5–15 cells per cross section. The size of clusters increased at 2 months to 30–70 cells per cluster per cross section (Fig. 2e) and by 4 months after Tx the largest collections of DPPIV+ hepatocytes comprised 100–150 cells per cross section. By this time, transplanted hepatocytes occupied 20–25% of the total area in the recipient liver (data not presented), compared with an initial level of about 0.1% (at the time of Tx). This pattern of results is consistent with our previous studies describing extensive replacement of the recipient liver when hepatocytes isolated from normal donors are transplanted into rats treated with RS (21, 23).
Dual histochemical/immunohistochemical staining for DPPIV and GST 7-7, performed at various intervals after Tx, indicated the presence of a subset of DPPIV+ clusters (about 1 in 10), which were also positive for the expression of GST 7-7 (Fig. 2e). Such observation was consistent throughout the experiment at 1, 2, and 4 months after Tx. Given that hepatocytes isolated from untreated donors were never found to express the GST 7-7 marker enzyme upon Tx and proliferation into RS-treated recipients (23), the finding reported above must reflect the presence of cells expressing GST 7-7 in the surrounding hepatocyte preparation. This is not surprising, because foci of GST 7-7-positive hepatocytes are invariably found in nodule-bearing livers, and such smaller lesions would go undetected during separation of surrounding tissue from larger nodules, before cell infusion.
Standard histological analysis on H&E-stained sections confirmed the presence of numerous islands of small hepatocytes in a background of megalocytosis, resulting from exposure to RS (Fig. 2f).
The Fate of Hepatocytes Isolated from Surrounding Tissue and Transplanted into the Liver of Untreated Rats.
An additional set of control experiments included Tx of hepatocytes isolated from surrounding liver into previously untreated syngeneic recipients (group IIB). Cells were infused via the portal vein (5 × 105 per rat) and groups of two and three animals were killed at 2 or 4 months after Tx, respectively.
On macroscopic examination, livers appeared to be normal at both time points considered. A few (1–2 per cm2) small clusters (2–4 cells per cluster per cross section) of DPPIV-expressing cells were found in liver samples taken at 1 month after Tx, with no appreciable differences at 2 months (Fig. 2g). Liver histology (H&E) was also normal (Fig. 2h).
Three animals in this group also underwent PH to determine whether the resulting proliferative stimulus would exert any effect on the growth of transplanted cells. Rats received PH at 4 months after Tx and were killed 2 months thereafter. However, the largest of DPPIV+ clusters reached a size of about 20–25 cells per cluster per cross section (Fig. 3d), while the mean size was of 10–15 cells per cluster. Taken together, these results are in agreement with previous findings, reported by us (21) and other groups (31), documenting the limited growth of normal adult hepatocytes upon Tx into the liver of normal untreated recipients.
Discussion
A pioneering experimental approach for the induction and the analysis of cancer development in the liver is described in this study. Hepatocyte nodules were first generated according to a well characterized protocol (24). Nodular cells were then isolated and transplanted into syngeneic hosts and their fate in the recipient liver was followed by using an enzyme marker, DPPIV (28), which was normally expressed in donor hepatocytes, although it was genetically defective in the hosts. This approach was specifically designed to investigate the possible role of any alteration(s) induced in the host environment before Tx on the fate of transplanted nodular hepatocytes isolated at various stages during carcinogenic process in vivo.
In this report, hepatocytes isolated from persistent liver nodules were transplanted into rats pretreated with RS, a naturally occurring alkaloid, which causes a persistent block on the hepatocyte cell cycle (22). This type of protocol was based on our previous studies indicating that hepatocytes isolated from a normal donor could selectively proliferate upon Tx into animals preexposed to RS, with massive (>90%) replacement of the host liver; however, virtually no growth of transplanted normal cells was seen in untreated recipients (21, 23). In light of these findings, we tested whether such treatment would also affect the rate of growth and/or progression of transplanted nodular hepatocytes. The results obtained were in line with the above prediction. Nodular hepatocytes grew rapidly in the liver of all animals pretreated with RS; they formed grossly visible nodules within 1 month after Tx and occupied 80–90% of the recipient organ by 2 months; furthermore, progression to hepatocellular carcinoma occurred within 4 months in three of four transplanted rats. All lesions originated from cells of donor origin, as documented by the positive staining for the DPPIV histochemical marker. By contrast, no significant growth of nodular cells was observed at 1, 2, and 4 months after Tx in untreated recipients injected with the same cell preparation; moreover, only a limited expansion of transplanted cells was seen in these animals in response to a growth stimulus such as PH.
A general conclusion from these results is that the surrounding environment can exert a profound effect on the fate of altered cell populations emerging during carcinogenesis to the point that it can be a rate-limiting component in the pathway toward neoplastic progression. This conclusion is in line with previous data in the literature documenting the plasticity of the neoplastic phenotype in vivo (6, 15, 32, 33).
More specifically, our present findings indicate that the persistent cell cycle block imposed by RS on resident hepatocytes is permissive for the rapid growth and progression toward cancer of transplanted nodular cells, although no such rapid growth and progression occurs in untreated recipients. Different lines of evidence suggest a role for impaired growth conditions as a selective force during neoplastic development (34–39). Most carcinogenic agents or exposures exert a growth-suppressive effect on their target organs, as pointed out by Haddow (34) more than 70 years ago. In the mid-1970s, Farber and coworkers (1, 35) introduced a model for cancer induction with chemicals whereby the selective expansion of initiated resistant cells is achieved through inhibition of the normal surrounding counterpart. This concept was later extended to other models of experimental carcinogenesis and might also apply to cancer development in humans, at least in some systems (ref. 36 and references therein). For example, human hepatocellular carcinoma is frequently found in a background of liver cirrhosis, which impairs the regenerative capacity of this organ (37). Furthermore, elegant studies conducted in vitro by Rubin and coworkers (1, 38, 39) have repeatedly associated conditions of growth constraint to an increased frequency in the emergence of transformed cell clones. Our present data provide direct support to the concept above. Isolated nodular hepatocytes were unable to significantly expand and/or progress when transplanted into the liver of a syngeneic untreated recipient; however, they grew very efficiently and developed into cancer upon Tx into a growth-inhibited host liver, such as induced by preexposure to RS.
Any possible involvement of the host immune system in mediating the effect(s) of RS on the fate of transplanted cells was not directly ruled out in these studies. However, we think it unlikely based on the following evidence. (i) Transplanted nodular cells were able to survive and grow to a limited extent in the liver of untreated animals also, indicating that they were not efficiently rejected by the immune system. (ii) The pattern of results described in the present studies using nodular cell Tx is similar to our previous findings obtained with normal hepatocyte Tx. Normal cells were able to grow and to repopulate the liver of recipient animals treated with RS, although they grow very little when transplanted into a normal host (21, 23). This pattern was further confirmed in this report when hepatocytes surrounding liver nodules were injected into either RS-treated or untreated recipients. Taken together, these data suggest that similar biological forces sustain the growth of normal and nodular hepatocytes in RS-treated hosts, making it unlikely that any alteration of immune-mediated mechanisms is critically involved in this process.
The above-referenced similarities in the biological response of normal and nodular hepatocytes are intriguing (40). However, at least two main differences were evident in the phenotypic behavior of the two cell populations. First, the growth pattern of normal hepatocytes transplanted into a liver exposed to RS is very typical. They do not form grossly visible or histologically detectable nodules, but rather migrate and integrate into the recipient parenchyma, forming hybrid canaliculi with adjacent endogenous cells; at no time in the process of liver repopulation is there any evidence of compression of surrounding tissue (21, 23). This is in sharp contrast with the findings described in this study. The growth pattern of nodular cells transplanted into RS-treated recipients was in fact very similar to that observed in the original host. They formed discrete lesions, which were sharply demarcated from surrounding tissue; the latter was compressed as the size of these lesions increased and invasion was not observed until overt neoplasia developed. This suggests that the inability to integrate into the host environment is a critical property which differentiates nodular hepatocytes from their normal counterpart. More studies are warranted to explore this aspect.
Second, total liver mass was never found to exceed normal values during liver repopulation by transplanted normal hepatocytes in rats treated with RS (23). This observation strongly supports the conclusion that the entire process is under normal homeostatic control: in fact, the growth of transplanted cells appears to be driven and limited by a physiologic response of the animal to the proliferative block imposed by RS on resident hepatocytes (21, 23). Furthermore, no evidence of neoplastic transformation has been observed so far in donor-derived cells in this model after >2 years of follow-up (E.L., unpublished observation). Conversely, very large livers (up to 10% of the body weight, >20 g of absolute weight) were present in RS-treated animals transplanted with nodular cells, and this was associated with the rapid development of large hepatic nodules and cancer. Thus, although it is reasonable to conceive that similar permissive forces are sustaining the initial growth of transplanted normal and nodular hepatocytes in this model, nodular cells soon become independent of these mechanisms and continue to grow indefinitely. The formation of a biological niche, composed of a sufficient number of interacting nodular cells, could represent a critical step toward escaping growth control mechanisms imposed by the surrounding environment, which still seem to operate on normal cells transplanted into RS-treated hosts.
In summary, these studies highlight the relevant role of the host environment in the pathogenesis of neoplasia to the point that it can be a rate-limiting factor for the entire process of cancer development. More specifically, conditions of growth constraint in the host tissue were found to represent an optimum soil for the growth and progression of altered cells.
Acknowledgments
We thank M. Boi and T. Puxeddu for their excellent technical and secretarial assistance. This work was supported in part by the Roche Organ Transplantation Research Foundation Grant ROTRF 759159119 (to E.L.) and the Ministero dell'Universitá e della Ricerca Scientifica e Tecnologica, Italy (to P.P.).
Abbreviations
- RS
retrorsine
- DPPIV−
dipeptidyl peptidase type IV deficient
- DPPIV+
DPPIV positive
- Tx
transplantation
- H&E
hematoxylin/eosin
- GST
glutathione S-transferase
- PH
partial hepatectomy
References
- 1.Farber E, Rubin H. Cancer Res. 1991;51:2751–2761. [PubMed] [Google Scholar]
- 2.Withers H R, Milas L. Cancer Res. 1973;33:1931–1936. [PubMed] [Google Scholar]
- 3.Brown J M, Marsa G W. Br J Cancer. 1978;37:1020–1025. doi: 10.1038/bjc.1978.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark W H, Tucker M A, Goldstein A M. Acta Oncol. 1995;34:749–757. doi: 10.3109/02841869509127182. [DOI] [PubMed] [Google Scholar]
- 5.Rinehart C A, Torti V R. Mol Carcinog. 1997;18:181–192. [PubMed] [Google Scholar]
- 6.McCullough K D, Coleman W B, Smith G J, Grisham J W. Cancer Res. 1997;57:1807–1813. [PubMed] [Google Scholar]
- 7.Petersen O W, Ronnov-Jessen L, Weaver V M, Bissell M J. Adv Cancer Res. 1998;75:135–161. doi: 10.1016/s0065-230x(08)60741-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barcellos-Hoff M H. J Mammary Gland Biol Neoplasia. 1998;3:165–175. doi: 10.1023/a:1018794806635. [DOI] [PubMed] [Google Scholar]
- 9.Gin-Wen C, Terzaghi-Howe M. Cancer Res. 1998;58:4445–4452. [PubMed] [Google Scholar]
- 10.Vaccariello M, Javaherian A, Wang Y, Fusenig N E, Garlick J A. J Invest Dermatol. 1999;113:384–391. doi: 10.1046/j.1523-1747.1999.00701.x. [DOI] [PubMed] [Google Scholar]
- 11.Park C C, Bissell M J, Barcellos-Hoff M H. Mol Med Today. 2000;6:324–329. doi: 10.1016/s1357-4310(00)01756-1. [DOI] [PubMed] [Google Scholar]
- 12.Hodges G M, Hicks R M, Spacey G D. Cancer Res. 1977;37:3720–3730. [PubMed] [Google Scholar]
- 13.Uchida K, Samma S, Momose H, Kashihara N, Rademaker A, Oyasu R. J Urol. 1990;143:618–622. doi: 10.1016/s0022-5347(17)40041-3. [DOI] [PubMed] [Google Scholar]
- 14.Haggie J A, Schor S L, Howell A, Birch J M, Sellwood R A S. Lancet. 1987;1:1455–1457. doi: 10.1016/s0140-6736(87)92206-9. [DOI] [PubMed] [Google Scholar]
- 15.Barcellos-Hoff M H, Ravani S A. Cancer Res. 2000;60:1254–1260. [PubMed] [Google Scholar]
- 16.Detmar M, Velasco P, Richard L, Claffey K P, Streit M, Riccardi L, Skobe M, Brown L F. Am J Pathol. 2000;156:159–167. doi: 10.1016/S0002-9440(10)64715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vauthey J-N, Walsh G L, Vlastos G, Lauwers G Y. Lancet Oncol. 2000;1:15–16. doi: 10.1016/S1470-2045(00)00105-4. [DOI] [PubMed] [Google Scholar]
- 18.Nishiguchi S, Kuroki T, Nakatani S, Morimoto H, Nakajima S, Shiomi S, Seki S, Kobayashi K, Otani S. Lancet. 1995;346:1051–1055. doi: 10.1016/s0140-6736(95)91739-x. [DOI] [PubMed] [Google Scholar]
- 19.Hittelman W N. J Natl Cancer Inst. 1999;91:1796–1799. doi: 10.1093/jnci/91.21.1796. [DOI] [PubMed] [Google Scholar]
- 20.Vlastos G, Rubio I T, Mirza N O, Newman L A, Aurora R, Alderfer J, Buzdar A U, Singletary S E. Ann Surg Oncol. 2000;7:581–587. doi: 10.1007/BF02725337. [DOI] [PubMed] [Google Scholar]
- 21.Laconi E, Oren R, Mukhopadhyay D K, Hurston E, Laconi S, Pani P, Dabeva M D, Shafritz D A. Am J Pathol. 1998;153:319–329. doi: 10.1016/S0002-9440(10)65574-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laconi S, Curreli F, Diana S, Pasciu D, De Filippo G, Sarma D S R, Pani P, Laconi E. J Hepatol. 1999;31:1069–1074. doi: 10.1016/s0168-8278(99)80320-1. [DOI] [PubMed] [Google Scholar]
- 23.Laconi S, Pillai S, Porcu P P, Shafritz D A, Pani P, Laconi E. Am J Pathol. 2001;158:771–777. doi: 10.1016/s0002-9440(10)64019-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Semple-Roberts E, Hayes A, Armstrong D, Becker R, Racz W, Farber E. Int J Cancer. 1987;40:643–645. doi: 10.1002/ijc.2910400512. [DOI] [PubMed] [Google Scholar]
- 25.Seglen P O. Methods Cell Biol. 1976;13:29–83. doi: 10.1016/s0091-679x(08)61797-5. [DOI] [PubMed] [Google Scholar]
- 26.Satoh K, Kitahara A, Soma Y, Inaba Y, Hatayama I, Sato K. Proc Natl Acad Sci USA. 1985;82:3964–3968. doi: 10.1073/pnas.82.12.3964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Solt D B, Cayama E, Tsuda H, Enomoto K, Lee G, Farber E. Cancer Res. 1983;43:188–191. [PubMed] [Google Scholar]
- 28.Thompson N L, Hixson D C, Callanan H, Panzica M, Flanagan D, Faris R A, Hong W J, Hartel-Schenk S, Doyle D. Biochem J. 1991;273:497–502. doi: 10.1042/bj2730497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stecca B A, Nardo B, Chieco P, Mazziotti A, Bolondi L, Cavallari A. J Hepatol. 1997;27:337–345. doi: 10.1016/s0168-8278(97)80180-8. [DOI] [PubMed] [Google Scholar]
- 30.Higgins G H, Anderson R M. Arch Pathol. 1931;12:186–202. [Google Scholar]
- 31.Gupta S, Rajvanshi P, Lee C D. Proc Natl Acad Sci USA. 1995;92:5860–5864. doi: 10.1073/pnas.92.13.5860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Illmensee K, Mintz B. Proc Natl Acad Sci USA. 1976;73:549–553. doi: 10.1073/pnas.73.2.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCullough K D, Coleman W B, Ricketts S L, Wilson J W, Smith G J, Grisham J W. Proc Natl Acad Sci USA. 1998;95:15333–15338. doi: 10.1073/pnas.95.26.15333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haddow A. Acta Unio Int Contra Cancrum. 1938;3:342–353. [Google Scholar]
- 35.Solt D B, Farber E. Nature (London) 1976;263:702–703. [Google Scholar]
- 36.Laconi E, Pani P, Farber E. Lancet Oncol. 2000;1:235–241. doi: 10.1016/s1470-2045(00)00154-6. [DOI] [PubMed] [Google Scholar]
- 37.Andiran F, Ayhan A, Tanyel C, Abbasoglu O, Sayek I. J Surg Res. 2000;89:184–188. doi: 10.1006/jsre.2000.5825. [DOI] [PubMed] [Google Scholar]
- 38.Chow M, Rubin H. Proc Natl Acad Sci USA. 1999;96:2093–2098. doi: 10.1073/pnas.96.5.2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rubin H. Cancer Res. 2001;61:799–807. [PubMed] [Google Scholar]
- 40.Laconi E. Am J Pathol. 2000;156:389–392. doi: 10.1016/S0002-9440(10)64741-4. [DOI] [PMC free article] [PubMed] [Google Scholar]