Abstract
Background
With the properties of three-column fixation and anterior-approach-only procedure, anterior transpedicular screw (ATPS) is ideal for severe multilevel traumatic cervical instabilities. However, the accurate insertion of ATPS remains challenging. Here we constructed a patient-specific biocompatible drill template and evaluated its accuracy in assisting ATPS insertion.
Methods
After ethical approval, 24 formalin-preserved cervical vertebrae (C2–C7) were CT scanned. 3D reconstruction models of cervical vertebra were obtained with 2-mm-diameter virtual pin tracts at the central pedicles. The 3D models were used for rapid prototyping (RP) printing. A 2-mm-diameter Kirschner wire was then inserted into the pin tract of the RP model before polymethylmethacrylate was used to construct the patient-specific biocompatible drill template. After removal of the anterior soft tissue, a 2-mm-diameter Kirschner wire was inserted into the cervical pedicle with the assistance of drill template. Cadaveric cervical spines with pin tracts were subsequently scanned using the same CT scanner. A 3D reconstruction was performed of the scanned spines to get 3D models of the vertebrae containing the actual pin tracts. The deviations were calculated between 3D models with virtual and actual pin tracts at the middle point of the cervical pedicle. 3D models of 3.5 mm-diameter screws were used in simulated insertion to grade the screw positions.
Findings
The patient-specific biocompatible drill template was constructed to assist ATPS insertion successfully. There were no significant differences between medial/lateral deviations (P = 0.797) or between superior/inferior deviations (P = 0.741). The absolute deviation values were 0.82±0.75 mm and 1.10±0.96 mm in axial and sagittal planes, respectively. In the simulated insertion, the screws in non-critical position were 44/48 (91.7%).
Conclusions
The patient-specific drill template is biocompatible, easy-to-apply and accurate in assisting ATPS insertion. Its clinical applications should be further researched.
Introduction
Surgical interventions are common for degenerative cervical spine diseases [1], [2], [3]. Due to the three-column fixation property, transpedicular screw fixation via the posterior approach has been shown to have superior stabilization capabilities in several biomechanical and clinical surveys [4], [5], [6], [7]. However, due to the posterior musculature stripping, the posterior approach can cause significant myofascial pain and lead to significant postoperative axial symptoms and neck pain [8], [9], [10]. On the contrary, the anterior approach is less traumatic with no damage to the paravertebral muscles and allows for anterior instrumentation as far as T1 [11], [12]. However, since the screws in the anterior approach are anchored in the cancellous vertebral body, the biomechanical stability of anterior plate fixation is limited, leading to significant failure rates [13]. Thus, for a successful ≥2-level corpectomy or operation for severe traumatic three-column instabilities, a combined anterior and posterior approach was found to be desirable [14], [15], [16] but it would require a secondary posterior approach procedure that might lead to a significant increase in morbidity.
Anterior transpedicular screw (ATPS) in clinical application was first reported by Aramoni et al. [17]. After corpectomy at one to three levels in 9 patients, Aramoni et al. placed ATPS under visualization of the pedicles to affix fibular grafts to cervical pedicles [17]. Koller et al. demonstrated the anatomical feasibility of ATPS and found the pull-out strength of ATPS to be 2.5-fold that of vertebral body screws [18], [19]. The ATPS technique merges the biomechanical merits of posterior transpedicular fixation with the surgical benefits of anterior-approach-only procedures [19], because it can increase initial construct stability in an anterior surgery which is believed to be best beneficial for some severe multilevel cervical instabilities [20], [21], [22].
Accurate insertion is a key to successful application of ATPS in clinic. In fluoroscopy-guided manual insertion of ATPS, a percentage of 78.3% was reported for correctly placed screws and non-critical pedicle breaches in the axial plane [18]. Yukawa et al. reported successful insertion of anterior pedicle screws in 6 patients with the aid of fluoroscopic images of the pedicle axis [23]. However, the sample number was small and the surgery required much time and experienced physicians. Koller et al., using the electronic conductivity device (ECD), found a high accuracy rate of ATPS insertion with no critical screw positioned in the axial or sagittal plane [24]. However, the physical property of ECD prevents it from penetrating the dense cortical bone. Patient-specific drill templates were developed to assist screw insertion using 3D reconstruction, computer aided design (CAD) and rapid prototyping (RP) techniques and good accuracy of screw insertion was obtained [25], [26], [27], [28], [29], [30]. However, these techniques have been used just in the posterior pedicle approach but not in the anterior pedicle approach. Also, the materials used in them, such as photosensitive resin, possess significant cytotoxicity [31], [32]. In the process of surgical drilling, debris of the drill template can get in contact with the wounded area, a potential danger if the debris cannot be totally rinsed.
Therefore, accurate and biocompatible insertion of ATPS remains a challenge. To address this challenge, we first adopted a new strategy to construct a biocompatible drill template for ATPS insertion using 3D reconstruction, RP production and reverse mold manufacture techniques. Secondly, we evaluated the accuracy of the drill template in assisting ATPS insertion.
Materials and Methods
Ethics Statement
Ethical approval was obtained from the Human Research Ethics Committee, Southern Medical University, Guangzhou, China. The subjects gave informed consent. And all consent was written in nature regarding body donation for research.
Specimens
Twenty four formalin-preserved cervical vertebrae (range C2–C7) from four human cadavers (3 males and 1 female, from 52 to 68 years of age, mean 61.5 years) were obtained. The entire specimens were imaged using a Brilliance CT 64-channel scanner (Philips, Eindhoven, The Netherlands). In-plane pixel size was 0.5 mm and slice thickness was 0.705 mm. All the 48 pedicles in the 24 cervical vertebrae were used after the CT scan images showed no significant bone defects.
Three-dimensional Reconstruction of Cervical Models with Virtual Pin Tracts
The datasets of cervical specimens were processed and edited with Mimics software v14.11 (Materialise Corp., Leuven, Belgium). 3D reconstructions were obtained from the 2D CT images. An interactive image processing strategy, such as “Threshold” and “Region growth”, was used to segment the contours of each vertebra to obtain the 3D-reconstructed models. The 2 cylinders, 2 mm in diameter and pre-designed in Unigraphics NX 6.0 (Siemens PLM Software, Plano, TX), were imported into Mimics software where it could be freely translated and rotated. It was made sure that the cylinders were located at the central cervical pedicle by visual observation. With the tool “subtraction” under “Boolean operation” in the Geomagic studio® software, 3D models of cervical vertebrae with bilateral pin tracts were obtained (Figure 1) and saved in group 1 in stereolithography file format (.stl) supported by many software packages and widely used for rapid prototyping and computer-aided manufacturing.
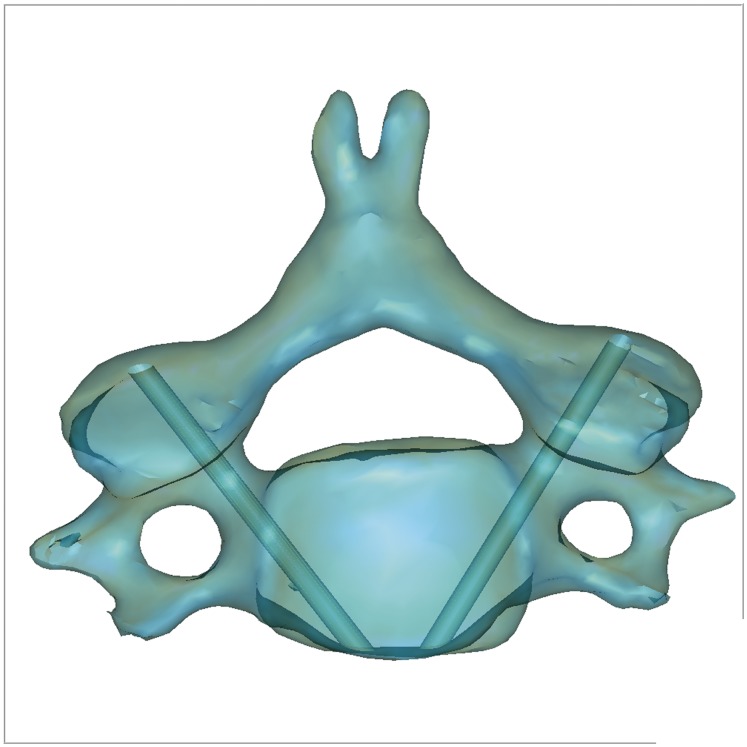
Figure 1. 3D model of cervical vertebra with virtual pin tracts.
3D model of each vertebra was reconstructed in Mimics software. The 2 cylinders with 2 mm-diameters were then imported and their locations were ensured at the central cervical pedicle by visual observation. With the tool “subtraction” under “Boolean operation” in the Geomagic studio® software, the 3D model of the cervical vertebrae with bilateral pin tracts was obtained and saved in group 1 in (.stl) file format.
Production of Biocompatible Drill Templates
The “.stl” files of cervical vertebrae were processed using the software Zprint 7.10 (Z Corporation, Burlington, MA) and printed on the Z Corporation 3D printer Spectrum Z™510 (Z Corporation, Burlington, MA). The 3D models were virtually cut into thin layers of 0.0875 mm intervals with the Zprint 7.10 software and transferred into the Spectrum Z510 for rapid prototyping (Figure 2). A Kirschner wire was then inserted into the pin tract of the RP model. Polymethylmethacrylate (PMMA), which is usually used as bone cement and has good biocompatibility [33], [34], [35], was used to construct the drill templates (Figure 2). Also, to allow for convenience and easy handling, a grip was created at the top of the drill template. In addition, since the surgery field was narrow, the base of the drill template was not allowed to exceed the juncture of the vertebral body and the transverse process. After the PMMA was solidified, the Kirschner wire was pulled out to finalize the drill template.
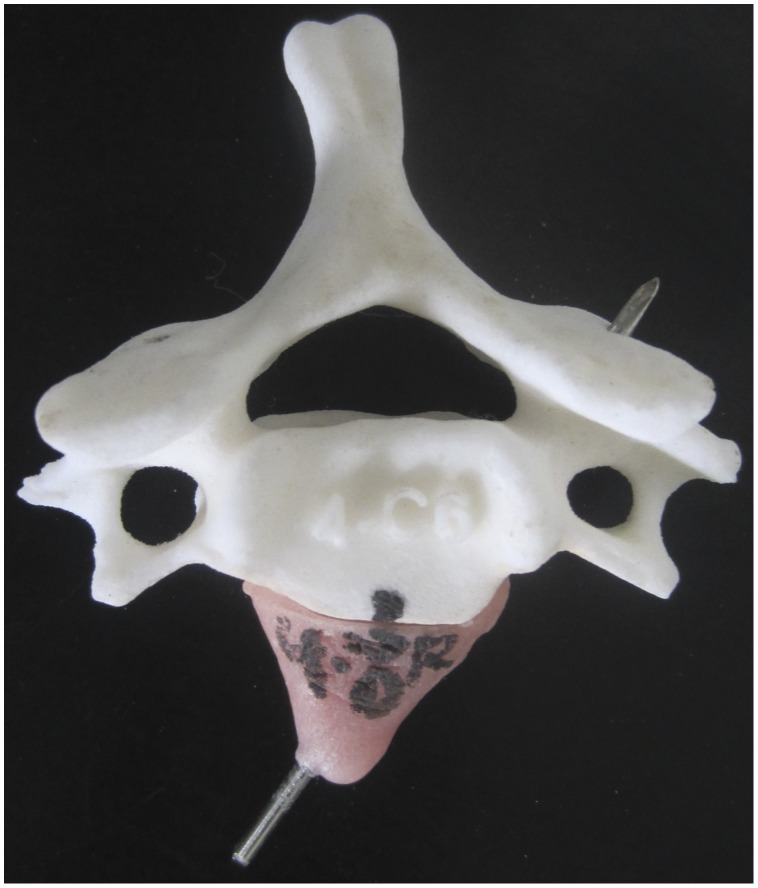
Figure 2. Production of biocompatible navigation template with RP model.
The 3D model of cervical vertebrae with virtual pin tracts was rapid-prototyped with Z Corporation 3D printer Spectrum Z™510. A Kirschner wire was then inserted into the pin tract of the RP model and polymethylmethacrylate (PMMA) was used to construct the drill template.
Cadaveric Kirschner Wire Insertion
Anterior soft tissue was removed from the vertebrae. The drill template was put in place by hand and compressed slightly to the anterior surface of cervical vertebrae. A 2-mm-diameter Kirschner wire was then drilled into the cervical pedicle with the assistance of the drill template (Figure 3).
Figure 3. Actual drill with navigation template in cadaveric cervical specimens.
Anterior soft tissue was removed from the vertebrae. The drill template was put in place by hand and compressed slightly to the anterior surface of cervical vertebrae. A 2 mm-diameter Kirschner wire was then drilled into the cervical pedicle with the assistance of the drill template.
Secondary 3D Reconstruction of Cervical Models with Pin Tracts
After all pin tracts were drilled, the cadaveric cervical specimens were scanned with the same CT scanner using the same parameters. Since the Kirschner wires produced image artifacts, they were pulled out before the image acquisition. 3D models of each vertebra with pin tracts were obtained with same segmentation and reconstruction strategy, and saved in group 2 in “.stl” file format.
Assessment of Accuracy of Screw Insertion
Accuracy of ATPS insertion with the assistance of the drill templates was evaluated by a reverse engineering process using the software Geomagic studio®, version 11 (Geomagic, Inc., Morrisville, NC). The 3D models of groups 1 and 2 were imported into the Geomagic software, and the deviations at the middle point of the pedicle in the axial and sagittal planes were calculated. The axial plane’s deviations towards the lateral side were recorded as positive values and the deviations towards the medial side as negative values. The sagittal plane’s deviations towards the superior and inferior sides were recorded as positive and negative values, respectively.
Aligned with the pin tract of the 3D model of group 2, a pre-designed 3D screw model (3.5 mm in diameter) was imported into Mimics to simulate the screw insertion (Figure 4). A grading was used to distinguish non-critical and critical screw positions [18], [24], [36]. Briefly, the grading consists of the following (Figure 5):
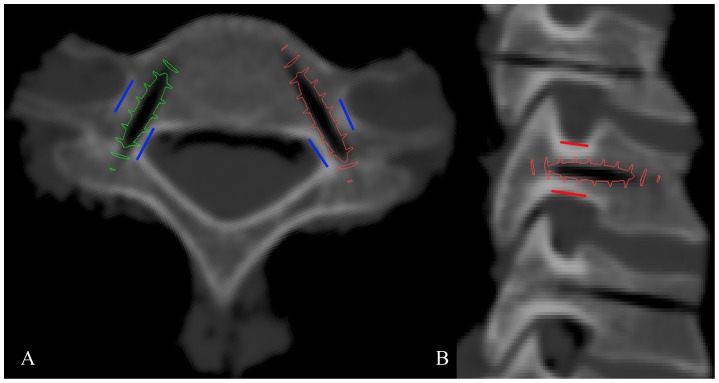
Figure 4. Accuracy evaluation with screw simulation insertion in the axial (A) and sagittal (B) planes.
The blue lines in Figure 4A are the border of cervical pedicle in axial plane. The structures inside and outside the blue lines are vertebral canal and vertebral artery, respectively. And the red lines in Figure 4B are the border of cervical pedicle in sagittal plane. The structures upper and lower the red lines are foramen intervertebrale. A pre-designed 3D screw model (3.5 mm in diameter), which aligned with the pin tract of the 3D model of group2, was imported into Mimics to simulate the screw insertion. The screw positions were graded according to the distance between the screw thread and the border of pedicle cortex.
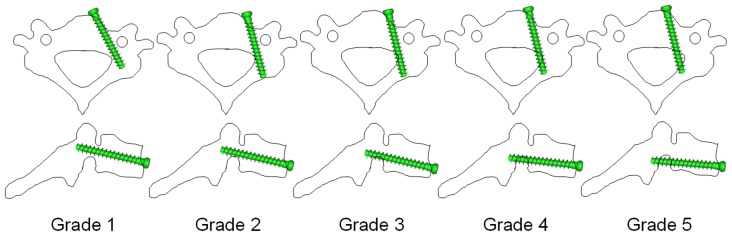
Figure 5. Illustration of grades of ATPS positions in cervical pedicle.
Grade 1: Screw positioned at the center of the pedicle. Grade 2: Less than one-third of the screw cross-section (≤1.2 mm with a 3.5-mm diameter screw) penetrating the cortex. Grade 3: Between one-third and one-half of the screw cross-section penetrating the cortex (or deviation <2 mm). Grade 4: More than one-half of the screw cross-section penetrating the cortex (or deviation ≥2 mm). Grade 5: Deviation equal or greater than the screw diameter.
Grade 1: Screw positioned at the center of the pedicle.
Grade 2: Less than one-third of the screw cross-section (≤1.2 mm with a 3.5-mm diameter screw) penetrating the cortex.
Grade 3: Between one-third and one-half of the screw cross-section penetrating the cortex (or deviation <2 mm).
Grade 4: More than one-half of the screw cross-section penetrating the cortex (or deviation ≥2 mm).
Grade 5: Deviation equal or greater than the screw diameter.
Non-critical pedicle breaches corresponded to grades 1 and 2. Critical pedicle breaches, with the potential of posing a risk to the vertebral artery (VA), nerve root or dural sac, corresponded to grades 3–5 [24].
Statistical Analysis
Independent-sample T test was used to analyze the screw direction differences between the deviations towards lateral and medial in the axial plane and towards superior and inferior in the sagittal plane. A P value <0.05 was considered as statistically significant. And, to show the real deviations, the absolute deviation values were calculated to get their means and standard deviations in the axial and sagittal planes, respectively.
With the scoring system [18], [24], assessment of pedicle screw position could be performed both in the axial and sagittal plane. Each point was assigned to each of the five grades of screw position. The accuracy score in the axial plane (range 1–5 points) and the accuracy score in the sagittal plane (range 1–5 points) was summed and described as the accuracy sum score with its maximum being 10 points and the minimum being 2, delineating most accurate screw placement.
Results
With the 3D reconstruction, rapid prototyping production and mold manufacture techniques, the patient-specific biocompatible drill templates were constructed successfully. During the operation, the drill template fit the position easily to allow no significant free motion between the drill template and the anterior cervical surface. The Kirschner wires were inserted into the cervical pedicle easily with the assistance of the patient-specific biocompatible drill template.
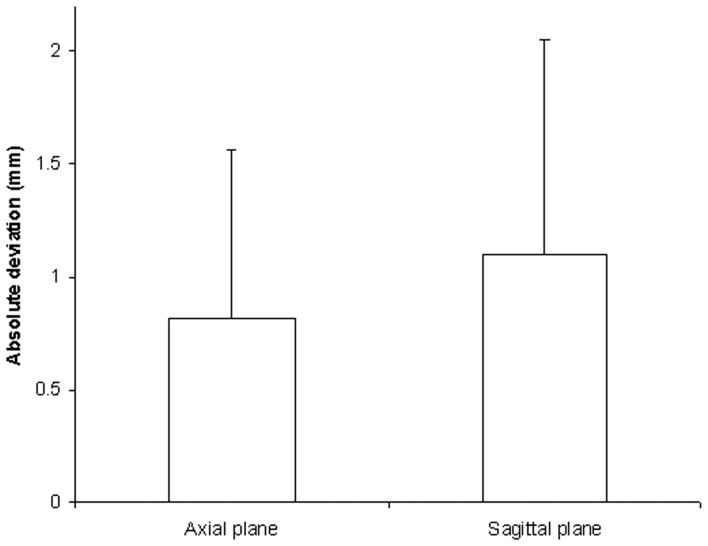
Calculation showed no significant difference between the deviations towards lateral and medial in the axial plane (t = −0.258, P = 0.797). The absolute deviation value in axial plane was 0.82±0.75 mm (Figure 6). There was no significant difference either between the deviations towards superior and inferior in the sagittal plane (t = 0.332, P = 0.741). The absolute deviation value in the sagittal plane was 1.10±0.96 mm (Figure 6).
Figure 6. Absolute deviation values in the axial and sagittal planes.
In the simulated insertion of 3.5 mm-diameter screw, one screw position was grade 3 (2.1%), one was grade 2 (2.1%) and the others were grade 1 (95.8%) in the axial plane. The mean accuracy score in the axial plane was 1.02. Three pedicle screw positions were grade 3 (6.25%), 4 were grade 2 (8.3%) and the others were grade 1 (85.4%) in the sagittal plane. The mean accuracy score in the sagittal plane was 1.22. The accuracy sum score showed a mean of 2.27 points with a possible total of 10 points. Summing up the screw positions in the axial and sagittal planes, the screws in a non-critical position were 44/48 (91.7%) and those in a critical position were 4/48 (8.3%).
Discussion
Pedicular screw insertion has generally been considered to be very risky because it can injure VA, the spinal cord or nerve roots seriously. Because of few landmarks on the anterior surface of cervical vertebra and also a relative long distance between the anterior surface and the pedicle, insertion of ATPS is more difficult and dangerous than posterior transpedicular fixation. Several methods have been explored for precise anterior cervical transpedicular screw placement, including the fluoroscopy-guided manual insertion [18], [19], fluoroscopic images of the pedicle axis [36] and ECD [24]. It is also possible to use CT-based and fluoroscopy-based computer assisted surgeries (CAS) to assist insertion of ATPS because they have been used to assist screw insertion in posterior transpedicular fixation and yielded high accuracy [37], [38], [39]. The rate of pedicle perforation in posterior cervical or cervical-thoracic fixation using pedicle screws was 8.6% in the conventional group and 3.0% in the CAS group [37]. Gelalis et al. [38] found the percentages of screws fully contained in the pedicle ranged from 89 to 100% using CT-based CAS and 81 to 92% using fluoroscopy-based CAS. However, several caveats should be considered: (1) the learning curve to master these complex techniques is relatively long; (2) errors may occur when adjacent segments of the spine shift intraoperatively or if the registration frame and optical array shift; (3) tracking of optical array devices can be obscured by the surgeon or surgical tools; (4) cost of equipment is high; and (5) surgical time is long [25].
The patient-specific drill templates eliminated the need for expensive equipment and a time-consuming procedure in an operating room [26]. They were initially used in hip and knee surgery [40] and so far have been developed to assist screw insertion in cervical surgery, yielding good accuracy of screw insertion [25], [26], [41], [42], [43]. In the present study we further improved the non-biocompatible drill templates into biocompatible ones. We first produced a non-biocompatible RP model of cervical vertebra with pin tracts. After inserting the Kirschner wire, we used PMMA, a biocompatible material [33], [34], [35], to produce the reverse mold of the RP model and construct a biocompatible drill template. Moreover, we improved the complex design of previous patient-specific drill templates which is beyond the ability of a surgeon because it requires not only medical knowledge but also knowledge of reverse engineering and CAD design [25]. First the drill template we constructed is easy to produce. It does not need surgeons to design the reverse surface modeling with complicated CAD technology. Since every step is programmed in certain software, an operator can just produce it step by step. Secondly, our drill template is easy to use. During a surgery, our drill template can find its position easily and fit the anterior cervical surface so well that the entry point and direction can be accurately determined. Next the Kirschner wire can be drilled into the cervical pedicle. Consequently it is possible for a surgeon to design customized surgical plan preoperatively. The technique we used can thus eliminate the need for complex equipment and markedly reduce the long duration of the surgery.
To ensure the accuracy of our drill template, we calculated the deviations at the central point of the cervical pedicles to get quantitative data. In this way we could evaluate the accuracy more directly. In the present study, we also calculated the absolute value of the deviations to show the real deviations because the deviations at different directions had positive and negative values, which resulted in a significantly smaller mean. Our study showed that the absolute value deviations in the axial plane (0.82±0.75 mm) and in the sagittal plane (1.10±0.96 mm) might be within an acceptable range in clinical application.
Gelalis et al. [38] found that the screws positioned with free-hand technique tended to perforate the cortex medially whereas the screws placed with CT navigation guidance seemed to perforate laterally more often. However, in our study, we found no significant differences between the medial and lateral deviations in the axial plane or between the superior and inferior deviations. Our finding means that there is no specific direction guidance resulting from our biocompatible drill templates.
The simulated insertion of 3.5 mm-diameter screw can show the real implant-pedicle anchorage. Our grade results are very close to the ECD results [24]. Unfortunately, we had 4 screw positions in grade 3. This means the screws penetrated the pedicle cortex from 1/3 to ½ of the screw cross-section. The deviations are relatively large although it is reported that surgeons judged the pedicle screw position of grade 3 as ‘indeterminate’ or ‘borderline’ because it would not cause injury to the VA or nerve root but rather would push the either one away [36]. We also found the virtual pin tracts had some deviations from the midline of the pedicle due to the error from our visual observation. This is one of the limitations of our research. In further research, optimal feature of the pin tract should be extracted from the irregular morphology of the cervical pedicle to make sure the pin tract at the midline of the cervical pedicle [25], [26]. Another limitation of ours is that the shape of drill templates was not optimized for clinical application. This is a primary study of ours on the biocompatible drill template. Future shape optimizing will follow the easy-to-apply and artistic principles. And pin tracts will be extended as long as possible to further improve the accuracy in assisting ATPS insertion.
Conclusion
In this in vitro study, the patient-specific drill template we constructed is compatible, easy-to-apply and accurate. Further research should be done to test its clinical applications.
Acknowledgments
The authors thank Zeyu Li, Chang Liu and Kuncheng Wu from the Department of Anatomy, Southern Medical University for assistance with specimen preparation; Weidong Wu from Department of Anatomy, Southern Medical University for assistance with constructing the 3D model of screw; Langyong Zeng from Department of Mold, Guangdong Electrical Vocational College, Guangzhou for assistance with technique support for software Geomagic, and Hugo Giambini from the Orthopedic Biomechanics Laboratory of Mayo Clinic, Rochester, Minnesota, for his assistance with manuscript review and modification.
Funding Statement
Projects 6110920, 6110922 and 6110923 were supported by National Natural Science Foundation of China (http://www.nsfc.gov.cn). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Yang B, Li H, Zhang T, He X, Xu S (2012) The incidence of adjacent segment degeneration after cervical disc arthroplasty (CDA): a meta analysis of randomized controlled trials. PLoS One 7(4): e35032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ponnusamy KE, Iyer S, Gupta G, Khanna AJ (2011) Instrumentation of the osteoporotic spine: biomechanical and clinical considerations. Spine J 11(1): 54–63. [DOI] [PubMed] [Google Scholar]
- 3. Fallah A, Akl EA, Ebrahim S, Ibrahim GM, Mansouri A, et al. (2012) Anterior Cervical Discectomy with Arthroplasty versus Arthrodesis for Single-Level Cervical Spondylosis: A Systematic Review and Meta-Analysis. PLoS One 7(8): e43407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, et al. (2005) Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976) 30(8): 915–922. [DOI] [PubMed] [Google Scholar]
- 5. Schmidt R, Wilke HJ, Claes L, Puhl W, Richter M (2005) Effect of constrained posterior screw and rod systems for primary stability: biomechanical in vitro comparison of various instrumentations in a single-level corpectomy model. Eur Spine J 14(4): 372–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim SM, Lim TJ, Paterno J, Park J, Kim DH (2004) A biomechanical comparison of three surgical approaches in bilateral subaxial cervical facet dislocation. J Neurosurg Spine 1(1): 108–115. [DOI] [PubMed] [Google Scholar]
- 7. Jones EL, Heller JG, Silcox DH, Hutton WC (1997) Cervical pedicle screws versus lateral mass screws. Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976) 22(9): 977–982. [DOI] [PubMed] [Google Scholar]
- 8. Koller H, Hempfing A, Ferraris L, Maier O, Hitzl W, et al. (2007) 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J 16(12): 2055–2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ohnari H, Sasai K, Akagi S, Iida H, Takanori S, et al. (2006) Investigation of axial symptoms after cervical laminoplasty, using questionnaire survey. Spine J 6(3): 221–227. [DOI] [PubMed] [Google Scholar]
- 10. Rao RD, Gourab K, David KS (2006) Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am 88(7): 1619–1640. [DOI] [PubMed] [Google Scholar]
- 11. Henriques T, Olerud C, Bergman A, Jonsson HJ (2004) Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech 17(1): 1–7. [DOI] [PubMed] [Google Scholar]
- 12. Fraser JF, Diwan AD, Peterson M, O’Brien MF, Mintz DN, et al. (2002) Preoperative magnetic resonance imaging screening for a surgical decision regarding the approach for anterior spine fusion at the cervicothoracic junction. Spine (Phila Pa 1976) 27(7): 675–681. [DOI] [PubMed] [Google Scholar]
- 13. Brazenor GA (2007) Comparison of multisegment anterior cervical fixation using bone strut graft versus a titanium rod and buttress prosthesis: analysis of outcome with long-term follow-up and interview by independent physician. Spine (Phila Pa 1976) 32(1): 63–71. [DOI] [PubMed] [Google Scholar]
- 14. Wang CS, Liu MJ, Lin JH, Xu WH, Luo HB (2011) One stage anterior-posterior approach for traumatic atlantoaxial instability combined with subaxial cervical spinal cord injury. Chin J Traumatol 14(3): 137–142. [PubMed] [Google Scholar]
- 15. Lv GH, Wang B, Kang YJ, Lu C, Ma ZM, et al. (2009) Combined anterior and posterior surgery for treatment of cervical fracture-dislocation in patients with ankylosing spondylitis. Chin J Traumatol 12(3): 148–152. [PubMed] [Google Scholar]
- 16. Yu DK, Heo DH, Cho SM, Choi JH, Sheen SH, et al. (2008) Posterior cervical fixation with nitinol shape memory loop in the anterior-posterior combined approach for the patients with three column injury of the cervical spine : preliminary report. J Korean Neurosurg Soc 44(5): 303–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aramomi M, Masaki Y, Koshizuka S, Kadota R, Okawa A, et al.. (2008) Anterior pedicle screw fixation for multilevel cervical corpectomy and spinal fusion. Acta Neurochir (Wien) 150(6): 575–582, 582. [DOI] [PubMed]
- 18. Koller H, Acosta F, Tauber M, Fox M, Martin H, et al. (2008) Cervical anterior transpedicular screw fixation (ATPS)–Part II. Accuracy of manual insertion and pull-out strength of ATPS. Eur Spine J 17(4): 539–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Koller H, Hempfing A, Acosta F, Fox M, Scheiter A, et al. (2008) Cervical anterior transpedicular screw fixation. Part I: Study on morphological feasibility, indications, and technical prerequisites. Eur Spine J 17(4): 523–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Acosta FJ, Aryan HE, Chou D, Ames CP (2008) Long-term biomechanical stability and clinical improvement after extended multilevel corpectomy and circumferential reconstruction of the cervical spine using titanium mesh cages. J Spinal Disord Tech 21(3): 165–174. [DOI] [PubMed] [Google Scholar]
- 21. Brazenor GA (2007) Comparison of multisegment anterior cervical fixation using bone strut graft versus a titanium rod and buttress prosthesis: analysis of outcome with long-term follow-up and interview by independent physician. Spine (Phila Pa 1976) 32(1): 63–71. [DOI] [PubMed] [Google Scholar]
- 22. Koller H, Hempfing A, Ferraris L, Maier O, Hitzl W, et al. (2007) 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J 16(12): 2055–2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yukawa Y, Kato F, Ito K, Nakashima H, Machino M (2009) Anterior cervical pedicle screw and plate fixation using fluoroscope-assisted pedicle axis view imaging: a preliminary report of a new cervical reconstruction technique. Eur Spine J 18(6): 911–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Koller H, Hitzl W, Acosta F, Tauber M, Zenner J, et al. (2009) In vitro study of accuracy of cervical pedicle screw insertion using an electronic conductivity device (ATPS part III). Eur Spine J 18(9): 1300–1313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lu S, Xu YQ, Chen GP, Zhang YZ, Lu D, et al. (2011) Efficacy and accuracy of a novel rapid prototyping drill template for cervical pedicle screw placement. Comput Aided Surg 16(5): 240–248. [DOI] [PubMed] [Google Scholar]
- 26. Lu S, Xu YQ, Lu WW, Ni GX, Li YB, et al. (2009) A novel patient-specific navigational template for cervical pedicle screw placement. Spine (Phila Pa 1976) 34(26): E959–E966. [DOI] [PubMed] [Google Scholar]
- 27. Lu S, Zhang YZ, Wang Z, Shi JH, Chen YB, et al. (2012) Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med Biol Eng Comput 50(7): 751–758. [DOI] [PubMed] [Google Scholar]
- 28. Lu S, Xu YQ, Zhang YZ, Li YB, Xie L, et al. (2009) A novel computer-assisted drill guide template for lumbar pedicle screw placement: a cadaveric and clinical study. Int J Med Robot 5(2): 184–191. [DOI] [PubMed] [Google Scholar]
- 29. Lu S, Xu YQ, Zhang YZ, Xie L, Guo H, et al. (2009) A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J 18(9): 1379–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lu S, Xu YQ, Zhang YZ, Li YB, Shi JH, et al. (2009) Rapid prototyping drill guide template for lumbar pedicle screw placement. Chin J Traumatol 12(3): 177–180. [PubMed] [Google Scholar]
- 31. Nicholson JW, Czarnecka B (2008) The biocompatibility of resin-modified glass-ionomer cements for dentistry. Dent Mater 24(12): 1702–1708. [DOI] [PubMed] [Google Scholar]
- 32. Souza PP, Aranha AM, Hebling J, Giro EM, Costa CA (2006) In vitro cytotoxicity and in vivo biocompatibility of contemporary resin-modified glass-ionomer cements. Dent Mater 22(9): 838–844. [DOI] [PubMed] [Google Scholar]
- 33.Lye KW, Tideman H, Wolke JC, Merkx MA, Chin FK, et al.. (2011) Biocompatibility and bone formation with porous modified PMMA in normal and irradiated mandibular tissue. Clin Oral Implants Res. [DOI] [PubMed]
- 34. Ormsby R, McNally T, O’Hare P, Burke G, Mitchell C, et al. (2012) Fatigue and biocompatibility properties of a poly(methyl methacrylate) bone cement with multi-walled carbon nanotubes. Acta Biomater 8(3): 1201–1212. [DOI] [PubMed] [Google Scholar]
- 35. Gerhart TN, Roux RD, Horowitz G, Miller RL, Hanff P, et al. (1988) Antibiotic release from an experimental biodegradable bone cement. J Orthop Res 6(4): 585–592. [DOI] [PubMed] [Google Scholar]
- 36. Tomasino A, Parikh K, Koller H, Zink W, Tsiouris AJ, et al. (2010) The vertebral artery and the cervical pedicle: morphometric analysis of a critical neighborhood. J Neurosurg Spine 13(1): 52–60. [DOI] [PubMed] [Google Scholar]
- 37. Richter M, Cakir B, Schmidt R (2005) Cervical pedicle screws: conventional versus computer-assisted placement of cannulated screws. Spine (Phila Pa 1976) 30(20): 2280–2287. [DOI] [PubMed] [Google Scholar]
- 38. Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, et al. (2012) Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J 21(2): 247–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ishikawa Y, Kanemura T, Yoshida G, Ito Z, Muramoto A, et al. (2010) Clinical accuracy of three-dimensional fluoroscopy-based computer-assisted cervical pedicle screw placement: a retrospective comparative study of conventional versus computer-assisted cervical pedicle screw placement. J Neurosurg Spine 13(5): 606–611. [DOI] [PubMed] [Google Scholar]
- 40. Radermacher K, Portheine F, Anton M, Zimolong A, Kaspers G, et al. (1998) Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop Relat Res(354): 28–38. [DOI] [PubMed] [Google Scholar]
- 41. Berry E, Cuppone M, Porada S, Millner PA, Rao A, et al. (2005) Personalised image-based templates for intra-operative guidance. Proc Inst Mech Eng H 219(2): 111–118. [DOI] [PubMed] [Google Scholar]
- 42. Mac-Thiong JM, Labelle H, Rooze M, Feipel V, Aubin CE (2003) Evaluation of a transpedicular drill guide for pedicle screw placement in the thoracic spine. Eur Spine J 12(5): 542–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Owen BD, Christensen GE, Reinhardt JM, Ryken TC (2007) Rapid prototype patient-specific drill template for cervical pedicle screw placement. Comput Aided Surg 12(5): 303–308. [DOI] [PubMed] [Google Scholar]