Abstract
Botulinum toxin A (BT) is used therapeutically for the treatment of primary focal hyperhidrosis, a chronic debilitating condition characterised by over-activity of the eccrine sweat glands. Systemic toxicity concerns require BT to be administered by local injection, which in the case of hyperhidrosis means multiple painful intradermal injections by a skilled clinician at 6-monthly intervals. This study investigates the potential of a liquid-loaded pocketed microneedle device to deliver botulinum toxin A into the human dermis with the aim of reducing patient pain, improving therapeutic targeting and simplifying the administration procedure. Initially, β-galactosidase was employed as a detectable model for BT to (i) visualise liquid loading of the microneedles, (ii) determine residence time of a liquid formulation on the device and (iii) quantify loaded doses. An array of five stainless steel pocketed microneedles was shown to possess sufficient capacity to deliver therapeutic doses of the potent BT protein. Microneedle-mediated intradermal delivery of β-galactosidase and formaldehyde-inactivated botulinum toxoid revealed effective deposition and subsequent diffusion within the dermis. This study is the first to characterise pocketed microneedle delivery of a liquid formulation into human skin and illustrates the potential of such systems for the cutaneous administration of potent proteins such as BT. A clinically appropriate microneedle delivery system for BT could have a significant impact in both the medical and cosmetic industries.
Keywords: Microneedle, Intradermal, Transdermal, Botulinum Toxin, Botox, Primary Focal Hyperhidrosis
Introduction
Botulinum toxin A (BT) is a potent neurotoxin with an expanding list of therapeutic and cosmetic indications. Its primary therapeutic uses relate to the treatment of hypersecretory and muscular defects in peripheral tissues. These include primary focal hyperhidrosis (PFHH), a chronic, debilitating condition characterised by over-activity of the eccrine sweat gland, most commonly on the palms, soles and the axillae. PFHH typically impacts significantly on a patient’s quality of life [1, 2], with effects that are comparable to better-known clinical conditions such as acne vulgaris and psoriasis [3]. It affects up to 1% of the population, with over 1 million US citizens suffering from a severe form of the condition [4]. Traditional medical approaches to PFHH treatment include topical application of aluminium chloride salts, or glycopyrronium bromide iontophoresis; therapeutic effects of these therapies are short-lived and ineffective for more severe forms of the condition. The traditional surgical approach involves sweat gland denervation or endoscopic transthoracic sympathectomy; both treatments are associated with potential for serious complications. In recent years localised administration of BT has proven to be a highly effective alternative therapy [5] and is increasingly used in the clinical setting due to its prolonged therapeutic effects, typically 6-12 months, and the absence of systemic side effects. However, effective delivery of BT to the eccrine sweat gland requires multiple intradermal injections into the hyperhidrotic site. The severity of the condition and the area of the anatomical site dictate the number of injections required; treatment typically involves up to 50 intradermal injections of 0.05-0.2ml of a botulinum toxin solution, administered by a skilled clinician, at 1-2cm intervals in a grid-like pattern. Administration of BT is often extremely painful, sometimes requiring patient anaesthesia in palmar and plantar regions. Furthermore, it is laborious and relies on high levels of administrator skill to achieve targeted deposition of BT in the dermis. A simple, less painful, yet effective alternative administration method for the targeted delivery of BT could therefore have a positive impact for both the patient and clinician.
In the previous decade there has been a considerable effort to develop minimally invasive delivery systems, such as the microneedle (MN) device [6], for intradermal administration of molecules and macromolecular biologics such as peptides [7], proteins [8] and nucleic acids [9, 10]. MNs consist of one or more miniaturised needles, between 100 and 1000μm in length, which are used to facilitate localised delivery of a therapeutic across the stratum corneum without significantly impinging on blood vessels and nerve fibres that occupy deeper regions of the stratified tissue. Numerous MN designs and compositions have been manufactured and developed to deliver pharmaceutical formulations using a diversity of approaches including (i) a dry coating on the MN shaft [11], (ii) topical application in combination with MN skin puncture [12, 13], (iii) liquid delivery via hollow MNs [14] and (iv) biodegradation / dissolving of a polymer / sugar MN [15, 16]
A further, less-characterised method is the use of pocketed MNs; devices containing cavities that function as integrated reservoirs in the MN shaft. Pocketed MNs have been used primarily for the intradermal delivery of dried formulations [17, 18]; however commercial formulations of macromolecular therapeutics, such as BT, are most often delivered as a solution. In this study, we therefore investigate the pocketed MN as a means to facilitate intradermal delivery of a liquid formulation of BT. In addition to reduced pain and increased convenience, further proposed advantages of such a delivery system include the ability to deliver an existing commercial BT formulation without the need to reformulate, and to provide visual feedback to the user regarding the successful delivery of a formulation following application of the device.
2 Materials and methods
Materials
General laboratory reagents were used as received and were primarily purchased from Sigma-Aldrich Ltd (Poole UK) and Fisher Scientific (Loughborough, UK). Foetal Bovine Serum (FBS), Penicillin-streptomycin solution, Dulbecco’s Modified Eagle’s Medium (DMEM) and 25mM HEPES were purchased from Invitrogen Corporation, Paisley, UK. Optimal Cutting Temperature (OCT) embedding media was purchased from RA Lamb Limited, (Eastbourne UK). Potassium ferrocyanide trihydrate (A.C.S. reagent grade) was purchased from ICN Biomedicals Inc. (Aurora, Ohio). Harris’ Haematoxylin and Gurrs’ Eosin were purchased from Lab 3 (Bristol, UK). Micronised salbutamol sulphate (mean diameter of 50%; particle population ≤ 3.07 μm) was purchased from Micron Technologies Ltd (Dartford, UK). Botulinum Neurotoxin Type A Toxoid and Anti Botulinum toxin type A chicken IgY were purchased from List Biological Laboratories (Campbell, California, USA). DAB+ chromogen (3,3 diaminobenzidine chromogen solution) and Dual Endogenous Peroxidase Block was purchased from Dako UK Ltd. (Cambridgeshire, UK). EasyLink PE/Cy7® (3 × 10 μg PE/Cy7®) conjugation kit was purchased from AbCam (Cambridge, UK).
Methods
2.1 MN fabrication and characterisation
MNs, either with (pocketed microneedle devices; PMNs) or without (non pocketed microneedle devices; NPMNs) cavities in the microneedle shafts, were cut from stainless steel sheets (Trinity Brand Industries, SS 304; McMaster-Carr, Atlanta, GA, USA) using an infrared laser and electropolished as described previously [19]. PMNs consisted of five individual needles, four of which contained central cavities and one of which was the central MN, without a cavity, which served as a non-pocketed control. For imaging, PMNs and NPMNs were mounted on aluminium stubs and characterised by scanning electron microscopy (SEM) (Veeco FEI (Philips) XL30, Eindhoven, The Netherlands). Images of MNs were also captured using a bright field light microscope (Zeiss Stemi 2000C Stereomicroscope, Welwyn Garden City, UK) with an associated with digital image capture system (Olympus C3040-ADL digital camera, Watford, UK) and an external electronic light source (Schott KL150, Stafford, UK).
2.2 Liquid loading PMNs with a model formulation
Commercially available formulations of BT (Botox®, Vistabel® Dysport® and Xeomin®) contain BT protein complexes with different molecular weights, ranging from 150kDa (Xeomin®) to 900 kDa (Botox®). A vial of Botox® contains 5 ng of BT (100 Units), 0.5 mg of HSA (human serum albumin) and 0.9 mg of sodium chloride (NaCl) in a lyophilised form. At these low concentrations BT is notoriously difficult to detect and at higher concentrations there are significant safety concerns. Therefore, to characterise PMN loading BT was replaced by a well characterised and detectable model protein, β-galactosidase (β-gal) [20], and a blue dye (20%v/v) was included in the formulation. The Botox® formulation mimic therefore included 5 ng β-gal, 0.5 mg HSA, 0.9 mg NaCl and 20 %v/v blue dye in a final volume of 150 μl. PMNs (n=3) and NPMNs (n=3) were loaded by a single immersion in to a reservoir of the representative formulation and visualized by light microscopy. Residency of the BT mimic formulation within the PMN cavities was monitored using a digital camera (Olympus C3040-ADL).
2.3 Enhancing the retention of liquid-loaded drug formulations in MN pockets
A viscosity enhancer was investigated as a means to increase the residence time of the liquid film within MN pockets. Aqueous loading solutions containing brilliant blue as a visible indicator were prepared using increasing concentrations of glycerine BP; 0 %w/v, 20 %w/v, 50%w/v and 80%w/v glycerine BP. Each of these formulations was loaded into a PMN at room temperature and continuously observed, using light microscopy, for 2 min. Subsequent observations were made at 30 min, 1 h, 24 h, 48 h, 120 h, 5 days, 12 days, 17 days, 26 days and 32 days.
2.4. Quantification of PMN loading capacity
The loading capacity of PMNs and NPMNs, after a single immersion into a loading formulation, was evaluated using established detectable model compounds. A low molecular weight drug, salbutamol sulphate (SS), and a high molecular weight protein, β-gal, were both evaluated.
2.4.1 Quantification of salbutamol sulphate (SS) loading
PMNs (n=10) and NPMNs (n=10) were loaded by immersion into a SS solution (0.1 g/ml in deionised water). Loaded microneedles were rinsed in 8μg/ml bamethane in methanol. Samples were analysed using high performance liquid chromatography (HPLC) using a Genesis C18 (Grace Vydac, Bannockburn, Illinois, USA) reverse phase column, a p200 pump, an AS 3000 autosampler, a UV 2000 detector and Chem Quest® 4.1 software (Thermo Electron Corporation, Altrincham, UK). The mobile phase was 40 % methanol and 60 % 1-heptane sulphonic acid in deionised water. The UV detector was set at a 278 nm wavelength and the retention time of the analyte was 6 min. Bamethane was included as an internal standard.
2.4.2 Quantification of β-gal loading
PMNs (n=10) and NPMNs (n=10) were loaded by a single immersion into the model formulation described in section 2.2, containing a detectable concentration of the macromolecular analyte β-gal (1.3 μg/μl). Liquid-loaded MNs were then rinsed for 1 h in sodium phosphate buffer and analysed using an established spectrophotometric method [21]. Briefly, test solutions were added to a reagent containing MgCl2 (30 mM), 2-mercaptoethanol (2-ME) (3.36 M) and o-nitrophenyl-β-D-galactoside (ONPG) (68 mM) and were incubated at pH 7.3, 37 °C. Addition of the protein, β-gal, to the colourless o-nitrophenyl-β-D-galactoside (ONPG) substrate results in a hydrolytic reaction and creation of a coloured product, O-nitrophenol (ONP) (λ max= 420 nm) [22]. After 40 min the reaction was arrested using sodium carbonate (1M) to increase the pH to 11. This assay was repeated for matched blank solutions (not containing the protein) and also a range of standards (0.06 ng/μl - 6 ng/μl). Absorbance values were measured at λ = 410 nm using a Fluostar fluorometer (BMG Lab technologies, Ortenberg, Germany).
2.4.3. Statistical analysis
Statistical analysis of quantitative data was performed using a two-tailed Mann Whitney U test, with significant differences indicated by p < 0.05.
2.5 Insertion of liquid-loaded PMNs into skin
Full-thickness human breast skin, excised on the day of the experiment, was obtained from two donors under informed patient consent and full ethical approval. Subcutaneous fat was removed by blunt dissection and the tissue was mounted on an underlying support. PMNs (n=6) and NPMNs (n=6) were liquid-loaded by a single immersion into a β-gal loading solution (0.65 μg/μl), inserted into human skin, held in situ for 5 s and were then withdrawn. NPMNs (n=3) were also coated with a β-gal loading solution (0.65 μg/μl), using an established micro-scale dip coated device [19], and dried overnight. Dry-coated NPMNs were inserted into the skin and left in place for 5 min before withdrawal.
Treated skin was cultured at the air-liquid interface in a Trowel-type organ culture set-up [23] for 90 min at 37°C / 5% CO2. Following incubation samples were rinsed in PBS / MgCl2 (4 mM), fixed in glutaraldehyde 2 %v/v for 2 h at 4 °C and then rinsed again in PBS / MgCl2 (4mM). Fixed tissue was then incubated with X-gal staining solution (X-gal 40 mg/ml in N-N-dimethylformamide, 5% v/v; Potassium Ferricyanide 0.6 M, 0.84 % v/v; Potassium Ferrocyanide 0.6 M, 0.84 % v/v; Magnesium Chloride 1 M, 0.2 % v/v; Tris 200 mM-HCl 1M buffer pH 8.5, 50 % v/v; deionised water to 100 %) at 37°C / 5% CO2 for 24 h, rinsed in PBS and then stored overnight at 4°C [24, 25]. Samples were visualised en face using a Zeiss Stemi 2000C stereomicroscope attached to an Olympus C 3040-ADL digital camera and a fiber optic light source (Schott KL1500). Following en face analysis, samples were embedded in OCT medium, cryosectioned using a Leica CM3050s cryomicrotome and imaged using a Olympus® BX50 light/fluorescence microscope attached to an Olympus DP-10 digital camera. Selected slides were counterstained with Harris’ Haematoxylin and Gurrs’ Eosin.
2.6. Diffusion of the model macromolecule formulation within human skin
Excised skin, obtained from two human donors, was divided into eight 2cm2 areas (n=8) and subcutaneous fat was removed by blunt dissection. Each specimen was placed (epidermis side down) in a Trowel-type organ culture set up and 10 μl of β-gal solution (0.65 μg/μl) was topically applied to the centre of the dermal tissue. Samples were cultured for either 30 min (n=4) or 240 min (n=4) to evaluate dermal diffusion of the protein. Diffusion was arrested by fixation of the tissue and subsequent X-gal staining, as described previously (section 2.5). Skin samples were analysed en face and the diffusion area (cm2) calculated using ImageJ software (available at http://rsb.info.nih.gov/ij; developed by Wayne Rasband, National Institutes of Health, Bethesda, MD, USA). Data were presented as an average diffusion area +/- standard deviation.
2.7. Cutaneous delivery of botulinum toxoid A using liquid-loaded PMNs
PMNs (n=3) were liquid-loaded, as previously described, with a solution containing formaldehyde inactivated BT i.e. botulinum toxoid (BTD) (100ng/μl). Each PMN was inserted into excised human skin, held in situ for 5 s and subsequently withdrawn. The PMN-treated area was immediately excised, mounted in OCT and stored at -80°C prior to cryosection, as described previously (section 2.5). Slides were fixed in acetone at room temperature for 5 min, rinsed in PBS and incubated with dual endogenous peroxidase block for 5 min. Next, slides were washed with PBS and incubated for 1 h with a diluted primary polyclonal antibody (Anti-botulinum toxin/toxoid type A chichen IgY). The primary antibody was diluted with freshly prepared blocking buffer containing BSA 1%w/v in PBS/Tween20 0.05%v/v. Slides were then rinsed with PBS/Tween20 0.05%v/v and incubated for 1 h with anti-chicken IgY (IgG)-peroxidase secondary antibody at a dilution of 1/500 in blocking buffer. Finally, specimens were rinsed, incubated with DAB+ chromogen solution for 5-10 min and analysed under a light microscope (Olympus BX50; Olympus, Middlesex, UK) and digital camera (Olympus DP 10). Selected slides were counterstained with Harris’ Haematoxylin.
2.8 Cutaneous delivery of fluorescence-conjugated BTD using liquid-loaded PMNs
BTD was fluorescently labelled with PE/Cy7 using the EasyLink PE/Cy7® kit (AbCam, Cambridge, UK). Approximately 2μl of fluorescent compound was withdrawn by a pipette and loaded on to the PMN using a dip-coating technique. PMNs were observed using light and fluorescence microscopy (DM IRB, Leica Microsystems), subsequently inserted into excised human skin and held in situ for 1 min before withdrawal. The PMN was then re-imaged by fluorescence and light microscopy to evaluate release of the fluorescent BTD formulation from the pockets.
To evaluate deposition, PMNs were liquid-loaded, immediately inserted into the skin and held in position for 5 s before withdrawal. The treated skin areas were excised, mounted in OCT and stored at -80°C prior to cryosection, as described previously (section 2.5). Transverse sections were analysed by light and fluorescence microscopy. Representative sections were imaged by a QImaging Retiga, Exi digital camera.
3. Results and discussion
3.1. Device characterization
The laser-etched stainless steel NPMNs and PMNs used in this study are shown in Figure 1. The dimensions of PMNs are approximately 670×340×65μm (y, x and z plane respectively), with each integrated pocket measuring approximately 365×140×65 μm (y, x and z plane). Based upon these dimensions a single cavity can theoretically accommodate approximately 3nl of liquid. NPMN projections measured approximately 700×170×70 μm (y, x and z plane). Tip-to-tip distance between two adjacent microneedles is 1.5 mm for both PMNs and NPMNs. The greater width of PMNs permitted inclusion of the integrated pocket whilst maintaining the strength required to ensure needle integrity during the application procedure. A single non-pocketed MN was also included in each PMN array (Fig 1B), providing an integral control. This permitted comparison of the delivery characteristics between pocketed and non-pocketed MNs on the same array. The electropolishing stage of MN manufacture was minimal, thereby maintaining an irregular surface topography i.e. roughness (Fig 1C, D). It was anticipated that this surface roughness would promote retention of a liquid film within the pockets.
Figure 1. Characterisation of NPMNs and PMNs.
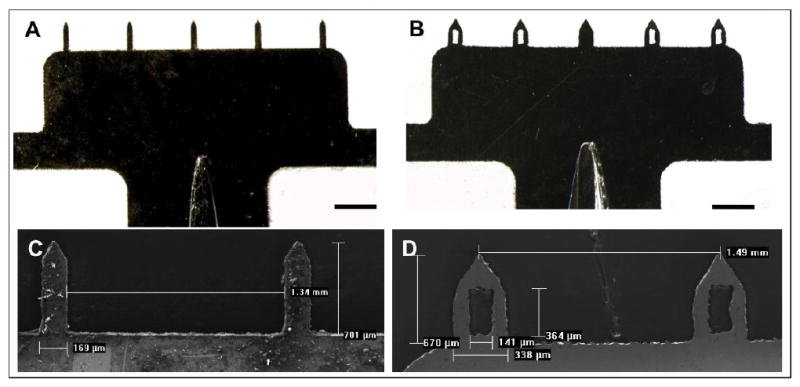
Brightfield micrographs of (A) a non-pocketed microneedle device (NPMN) and (B) a pocketed microneedle device (PMN); scale bar = 1mm. Scanning electron micrographs of two adjacent (C) non-pocketed and (D) pocketed microneedles.
3.2. Liquid loading PMNs with a model formulation
PMNs and NPMNs were liquid-loaded by immersing the needles into a formulation containing β-gal as a detectable model of BT. Figures 2A and 2B depict PMN and NPMN arrays immediately after a single immersion into the model formulation. The cavities of the PMN were loaded, uniformly, with the blue-coloured model formulation and the integrity of the liquid film was maintained in the pockets of the device for approximately 90 s before evaporation resulted in a reduction in the surface tension and disappearance of the film (data not shown). Our results with the model formulation therefore indicate that the inherent viscosity of the Botox® formulation, predominantly provided by the inclusion of HSA, will permit liquid loading of the cavities in a PMN, without the need to reformulate. Development of a microneedle delivery system that can deliver a commercial therapeutic formulation to its target site without reformulation, in a comparable manner to current delivery methods, would significantly reduce the regulatory hurdles involved in translation to the clinic. Additionally, inclusion of a dye permitted visualisation of the formulation within the microneedle pockets. This visual signal provides an indicator of successful PMN loading and unloading, a desirable feature of future MN delivery systems [26].
Figure 2. Loading/coating of a Botox® like formulation on a PMN and NPMN.
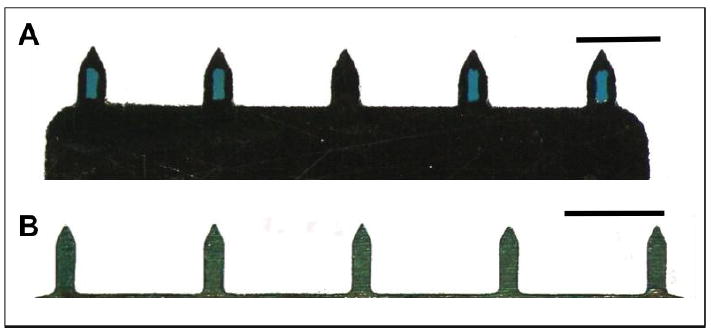
Brightfield micrographs of (A) a PMN and (B) a NPMN after immersion into a Botox®-like formulation containing blue dye; scale bar = 1mm.
3.3. Enhancing the retention of liquid-loaded drug formulations in MN pockets
Glycerine can reduce evaporation and therefore prolong the residency of a liquid within the PMN cavities. Figure 3 indicates that retention of a formulation within a PMN cavity can be dramatically increased by the inclusion of glycerine; the addition of 20-80% glycerine to the aqueous blue dye used in this component of the study extended the visible retention of the dye in the pockets from seconds (<70 s) to days. The addition of evaporation modifiers, such as glycerine, may therefore be used to tailor the retention times of aqueous solutions within the cavity of a PMN in order to suit the specific clinical application. However it should be noted that the formulations evaluated in Figure 3 consisted only of glycerine, water and a dye to enable visualisation i.e. they did not contain a protein component. The addition of protein to a simple aqueous solution will also increase the viscosity of the formulation, as exemplified in section 3.2 where inclusion of a high HSA concentration in the Botox® like formulation resulted in retention of the liquid in PMN cavities for up to 90 s. Future studies are therefore required to establish the duration of retention that would be required for BT delivery via a PMN and the formulation could then be modified, or not, accordingly.
Figure 3. The effect of a viscosity modifier on PMN loading and formulation retention.
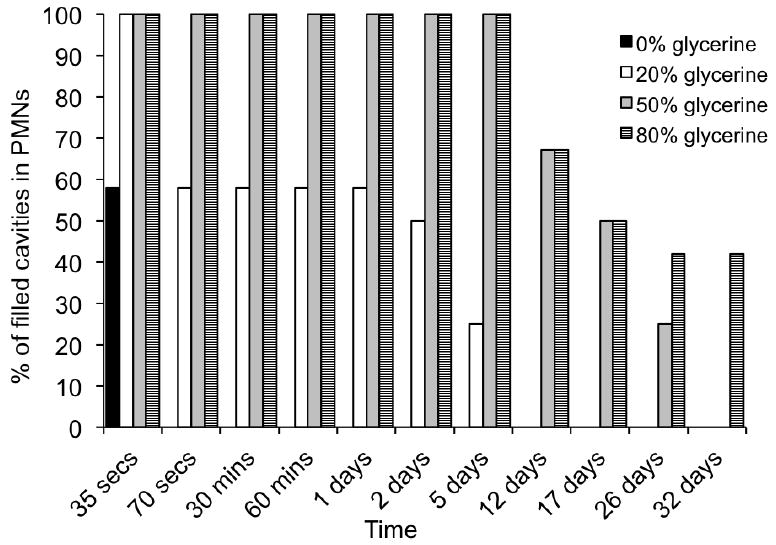
The percentage of PMN cavities that retained the glycerine formulation was calculated from the total number of cavities available in all PMNs tested for each of the formulations. The glycerine concentration in each of the aqueous formulations was 0% (N=4), 20% (N=3), 50% (N=3) or 80% (N=3). A blue dye was included in the formulation and the presence or absence of the formulation in the cavity was observed at regular time intervals up to 32 days.
3.4. MN loading capacity
The loading capacity of PMNs and NPMNs was determined using the β-gal model macromolecule (Fig 4A), included at greater concentrations than those previously used (section 3.2), in order to enable analytical detection of the protein. After a single immersion into a β-gal loading formulation (1.3 μg/μl), an average of 66.5 ng (+/- 52.3 ng) and 75.8ng (+/- 89.1 ng) of the BT model was loaded on the PMN and a NPMN, respectively (Fig 4A). Previous studies indicate that PFHH patients are effectively treated by approximately 28 intradermal injections, each of 100μl, of a Botox® solution (1.25 ng/ml), spaced at 1-1.5 cm intervals, into each palm [27]. This corresponds to a total dose of 3.5 ng per palm. BT is readily soluble in water, suggesting that a full dose of BT could be administered in nanolitre volumes of liquid formulation. This analysis indicates that both PMNs and NPMNs have the capacity to accommodate therapeutically relevant doses of BT for PFHH. However, the miniaturised nature of PMNs and the method of delivery means that these doses would have to be delivered in a significantly reduced volume compared to the 100 μl bolus doses that are delivered by hypodermic needles and syringes in current therapeutic practice.
Figure 4. Evaluation of coating/loading capacity of PMNs and NPMNs.

The mass of (A) the BT macromolecular model, β-galactosidase (β-gal), and (B) a small molecular weight model, salbutamol sulphate (SS) recovered from PMNs (n=10) and NPMNs (n=10) following liquid loading. Horizontal lines depict the mean for each sample.
The loading doses recorded in this study (Fig 4A) indicate that comparable volumes of the model BT formulation is loaded on a MN, independent of whether the device possesses pocketed cavities, i.e. there is no significant difference between loading of the two needle types (p=0.79). Therefore, the PMN does not offer an advantage with respect to drug loading capacity. This is consistent with the use of a PMN to load dry-coated formulations [17]. It should also be noted that the calculated theoretical liquid loading capacity of the cavities in the PMN is 12 nl, which is a significantly smaller volume than the volumes we were generally able to accommodate in our loading studies. This difference exists, in part, because the pockets do not selectively retain the liquid-loaded formulation, i.e. the shaft of each MN is also coated. Previous studies examining dry-coating of PMNs [17] suggest that selective filling of the pockets may be achieved by the addition of excipients to the formulation.
Large standard deviation values indicate a lack of reproducibility in liquid loading (Fig 4A). To determine whether this irreproducibility was related to the macromolecular analyte or a limitation of the loading process MNs were also loaded with a well-characterised small drug molecule, SS. An average of 13.6 μg (+/- 8.84 μg) and 7.5 μg (+/- 5.2 μg) of SS was loaded on a PMN and NPMN, respectively, after a single immersion into a SS loading solution (0.1 g/ml) (Fig 4B). This equates to a mean volume of 136nl (PMN) and 75nl (NPMN) of SS solution. Therefore although SS data supports results with the β-gal model, indicating that there is no difference in the liquid-loading capacity of PMNs and NPMNs (p>0.05), reproducibility remains problematic and thus an accurate loading volume cannot be concluded from this data. The reason for the observed variability is likely due to the loading technique employed in this study. A simple manual loading technique without additional coating apparatus was envisaged to be convenient to clinicians in practice. However the micron scale of the device and small loading volumes mean that controlled immersion depths within a loading reservoir was practically challenging. A dip-coating device [19] is therefore required to achieve more reproducible liquid-loading on PMNs and, in combination with formulation strategies [17], could be used to selectively and reproducibly liquid load the cavities of a PMN.
Quantitative data suggests that liquid loading of MNs is most suited to very potent molecules (due to limited loading capacity). Less than nanogram quantities of BT need to be delivered into a 1 cm2 PFHH treatment site and the risk of toxicity from the pharmaceutical formulation of BT is low [28]. Therefore BT, in a liquid formulation, is an ideal candidate for MN-based delivery systems. However, to load a therapeutically relevant dose would require reconstitution of a commercial BT formulation using lower volumes than those currently used in clinical practice, i.e. the formulation would need to be reconstituted with a volume in the μl range instead of the ml range. Based upon excipient solubility and the nanogram quantity of BT included in the commercial Botox® formulation (5 ng BT; 0.5 mg of human serum albumin (HSA); 0.9 mg of NaCl) the formulation could be dissolved in saline solution using volumes as low as 50 μl and therefore liquid-loaded PMNs are a plausible means to deliver this therapeutic protein.
3.5. MN-mediated delivery into human skin
En face images of representative skin samples treated with β-gal from dry -coated NPMNs (Fig 5A) and liquid-loaded PMNs (Fig 5B) illustrate differences in the deposition and distribution of a protein delivered using these two types of systems. Confirmation of protein delivery is provided by evidence of blue staining at the site of MN penetration, arising from the enzymatic conversion of X-gal to an insoluble blue product. Diffusion of the protein proximal to the points of MN insertion is notably greater for the liquid-loaded PMNs (Fig 5B) compared to the dry-coated formulation, delivered from NPMNs (Fig 5A). Results therefore indicate that liquid-loaded protein formulations are able to diffuse more rapidly into the surrounding tissue than dry-coated formulations, which rely on dissolution and diffusion from the point of MN insertion. Proximal diffusion of the protein from the single, central NPMN (central position) within the liquid-loaded PMN array was also more restricted than its pocketed counterparts (Fig 5B). This suggests that diffusion of the formulation may be enhanced by the loading mechanism. Histological analysis (Fig 5D) confirms significant diffusion of the protein in all directions proximal to the point of PMN insertion, and successful delivery of this high molecular weight protein to the epidermal and dermal regions of the skin. Results therefore suggest that a MN with a central cavity may be advantageous for the delivery of liquid formulations that require rapid distribution within the skin.
Figure 5. Delivery of a BT model within human skin using PMNs and NPMNs.
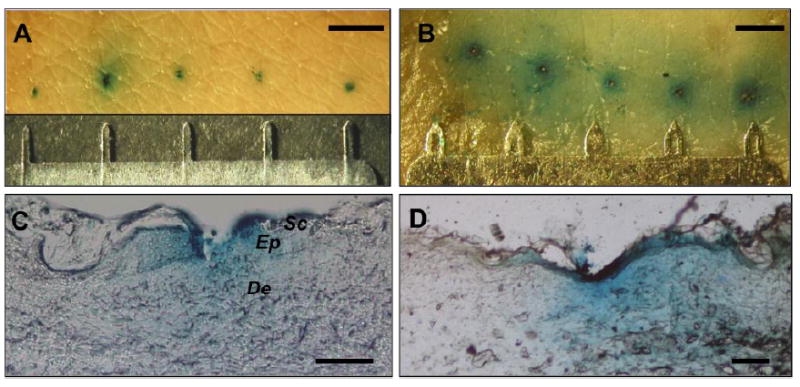
En face images (A, B) and histological sections (C, D) of human skin treated with the BT model drug, delivered using (A, C) a dry-coated NPMN (n=3) and (B, D) a liquid-loaded PMN (n=3). Blue pigmentation is an indicator for detection of the BT model (β-gal) in the skin. (A, B) scale bar = 1mm; (C, D) scale bar = 100 μm. Sc = Stratum Corneum, Ep = Epidermis, De = Dermis.
Although the BT model was successfully delivered to the dermal layer of human skin by both dry-coated and liquid-loaded MNs, lateral diffusion in the dermis was enhanced following liquid delivery via PMNs. The target skin structure in the treatment of PFHH is the pre-synaptic nerve terminals that innervate the eccrine sweat gland. These are located in the lower part of the dermis and therefore effective BT diffusion from the site of MN penetration will be an important factor if the device is to achieve therapeutic outcomes that are commensurate with current clinical practice, i.e. intradermal injections.
Little is understood about the diffusion of BT within the dermis following delivery of low volume liquid formulations. Figure 6 illustrates the diffusional area of a high molecular weight protein solution after topical application to the human dermis. Thirty minutes after application the diffusional area was approximately 0.4 cm2 (0.41 cm2 +/- 0.05 cm2) and after 240 min lateral diffusion of the protein extended to approximately 0.7 cm2 (0.67 cm2 +/- 0.07 cm2) (Fig 6). These results provide further evidence that large proteins in a liquid formulation can readily diffuse within the dermal layer of human skin. Importantly, this indicates that MN mediated delivery of BT to the upper regions of the dermis may be sufficient to enable interaction of the highly potent molecule with the eccrine sweet glands in the lower portion of the stratified tissue. However, when interpreting these results we must be cognisant of the differences in molecular weight, charge and structure of the model protein and BT. Predictive results indicate dermal diffusion of a high molecular weigh protein, delivered in a liquid formulation, would be relatively unhampered but diffusion studies in human volunteers [29] are required to confirm this.
Figure 6. Diffusion of the BT model, β-gal, in the dermal region of human skin.
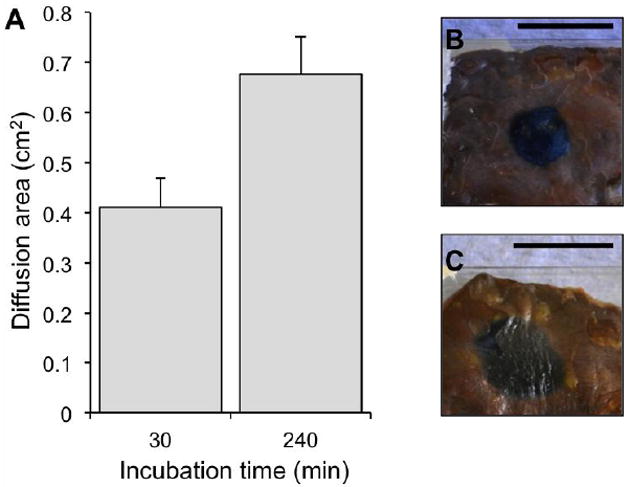
(A) The diffusion area (cm2) of β-gal after topical application of the enzymatic solution to human skin dermis. Β-gal diffusion area is shown as a function of incubation time in organ culture. Data are presented as mean+/-SD (n=4) from two skin donors. (B, C) En face images of treated dermis after (B) 30min and (C) 240 min; scale bar in inset images = 1cm.
3.6. Cutaneous delivery of botulinum toxoid (BTD) by liquid-loaded PMNs
Whilst the extreme potency of BT makes the toxin an ideal candidate for liquid-loaded MN delivery, detection of therapeutic (nanogram) levels of BT using standard laboratory methods is a significant challenge. To establish proof-of-concept we have used formaldehyde inactivated BTD as a readily-available, highly representative and detectable model of botulinum toxin. Negative controls, using a simple visible dye to detect areas of MN penetration, provide an indication of background staining (Fig 7C, D). Positive staining (dark brown) in the viable epidermis and the dermis proximal to individual MN penetrations suggests successful superficial delivery from liquid-loaded PMNs (Fig 7 A, B). However low levels of background staining in control samples (Fig 7D) make the results equivocal.
Fig 7. Delivery of botulinum toxoid A to human skin by liquid-loaded PMNs.
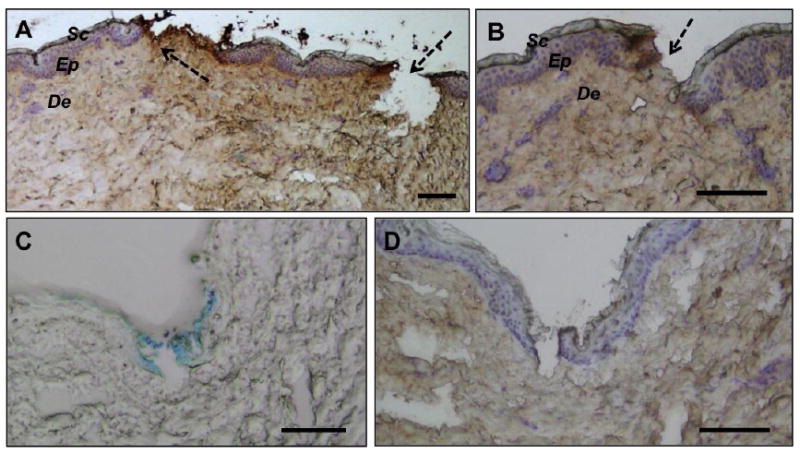
(A, B) Haematoxylin counterstained histological sections of human skin treated with PMNs loaded with a liquid BTD formulation. Arrows indicate MN disruption sites in the human skin. Brown stain is indicative of immunohistochemical detection of the toxoid. (C) Negative controls delivered methylene blue into the skin and were subsequently (D) processed alongside BTD-treated skin samples to evaluate background staining. Scale bar = 100 μm. Sc = Stratum Corneum, Ep = Epidermis, De = Dermis.
Fluorescently labelled botulinum toxoid was therefore used to corroborate IHC results and confirm delivery of the toxoid into human skin using PMNs. Fig 8 illustrates PMNs loaded with fluorescent BTD before (A) and after (B) insertion into human skin. The formulation was coated uniformly on both the surface of the PMN projection and within the integrated pocket following a single insertion into the formulation. Undetectable levels of fluorescence in the cavity following insertion into the skin confirmed that the majority of the BTD formulation was rapidly released from the PMN upon contact with the tissue. Figures 8C and 8D confirm this, clearly illustrating localised deposition of fluorescent BTD and also suggesting some lateral diffusion of the molecule from the point of deposition just minutes after treatment. Deposition from the PMN was localised to the epidermis and upper dermis. This proof-of-concept study confirms that a PMN can successfully deliver BTD, loaded onto a PMN as a liquid formulation, into human skin.
Fig 8. Liquid loading of PMNs with fluorescence-conjugated BTD and subsequent delivery to human skin.
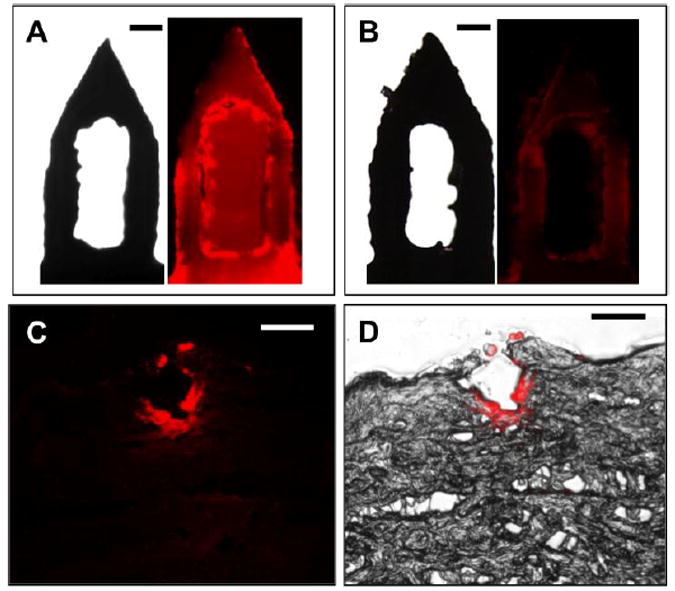
(A, B) Fluorescence and brightfield micrographs of a pocketed microneedle loaded with fluorescent BTD before (A) and after (B) insertion into human skin. (C, D) Histological sections of human skin, treated with a PMN that has been liquid-loaded with fluorescence-conjugated BTD. A fluorescence (C) and a fluorescence/brightfield overlay (D) are included. Scale bar = 100 μm.
Conclusions
BT is a very potent therapeutic with an expanding portfolio of clinical applications that is being used more frequently in clinical practice for both approved and unapproved indications in medicine and cosmetics. The most common administration method for BT, in conditions such as PFHH, is multiple painful intradermal injections by a skilled clinician. This study demonstrates that MNs provide a less invasive alternative that is suited to delivery of large proteins such as BT. Not only were MNs able to accommodate therapeutic doses of a model protein but they were also able to deliver an inactivated form of the toxin into human skin. Current approaches to MN-mediated delivery of biologics predominantly either reformulate therapeutic preparations to create dry-coated MNs or inject a liquid formulation, in relatively large volumes, using hollow MNs. This study is the first to systematically characterise an intermediate approach whereby PMNs are used to deliver nanolitre volumes of a therapeutically relevant liquid formulation into human skin. This novel approach is particularly suited to the intradermal delivery of potent therapeutics, such as BT. It also provides an opportunity to integrate a feature that would provide patients and clinicians with visible feedback of successful delivery, a feature that has been previously identified as being important in the translation of MN devices to clinical practice [26].
Acknowledgments
This work was supported in part by the National Institutes of Health. Mark Prausnitz is an inventor of patents that have been licensed to companies developing microneedle-based products, is a paid advisor to companies developing microneedle-based products and is a founder/shareholder of companies developing microneedle-based products.
Footnotes
This potential conflict of interest has been disclosed and is managed by Georgia Tech and Emory University.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weber A, Heger S, Sinkgraven R, Heckmann M, Elsener P, Rzanv B. Psychosocial aspects of patients with focal hyperhidrosis. Marked reduction of social phobia, anxiety and depression and increased quality of life after treatment with botulinum toxin A. Brit J Dermatol. 2005;152(2):342–345. doi: 10.1111/j.1365-2133.2004.06334.x. [DOI] [PubMed] [Google Scholar]
- 2.Hamm H, Naumann MK, Kowalski JW, Kütt S, Kozma C, Teale C. Primary focal hyperhidrosis: disease characteristics and functional impairment. Dermatology. 2006;212(4):343–353. doi: 10.1159/000092285. [DOI] [PubMed] [Google Scholar]
- 3.Swartling C, Naver H, Lindeberg C. Botulinum A toxin improves life quality in severe primary focal hyperhidrosis. Eur J Neurol. 2001;8(3):247–252. doi: 10.1046/j.1468-1331.2001.00207.x. [DOI] [PubMed] [Google Scholar]
- 4.Strutton DR, Kowalski JW, Glaser DA, Stang PE. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. J Am Acad Dermatol. 2004;51(2):241–248. doi: 10.1016/j.jaad.2003.12.040. [DOI] [PubMed] [Google Scholar]
- 5.Bhidayasiri R, Truong DD. Evidence for effectiveness of botulinum toxin for hyperhidrosis. J Neural Transm. 2008;115(4):641–645. doi: 10.1007/s00702-007-0812-7. [DOI] [PubMed] [Google Scholar]
- 6.Kim YC, Park JH, Prausnitz MR. Microneedles for drug and vaccine delivery. Adv Drug Deliv Rev. 2012 doi: 10.1016/j.addr.2012.04.005. In Press. Available online 01 May 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burton SA, Simmers R, Ng CY, Bradwein D, Gilbert T, Johnson N, Brown K, Alston T, Prochow G, Siebenaler K, Hansen K. Rapid intradermal delivery of liquid formulations using a hollow microstructured array. Pharm Res. 2011;28(1):31–40. doi: 10.1007/s11095-010-0177-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Widera G, Johnson J, Kim L, Libiran L, Nyam K, Daddona PE, Cormier M. Effect of delivery parameters on immunization to ovalbumin following intracutaneous administration by a coated microneedle array patch system. Vaccine. 2006;24(10):1653–1664. doi: 10.1016/j.vaccine.2005.09.049. [DOI] [PubMed] [Google Scholar]
- 9.Coulman SA, Barrow D, Anstey A, Gateley C, Morrissey A, Wilke N, Allender CJ, Brain KR, Birchall JC. Minimally invasive cutaneous delivery of macromolecules and plasmid DNA via microneedles. Curr Drug Deliv. 2006;3(1):65–75. doi: 10.2174/156720106775197510. [DOI] [PubMed] [Google Scholar]
- 10.Chen X, Kask AS, Crichton ML, McNeilly C, Yukiko S, Dong L, Marshak JO, Jarrahian C, Fernando GJ, Chen D, Koelle DM, Kendall MA. Improved DNA vaccination by skin-targeted delivery using dry-coated densely-packed microprojection arrays. J Control Release. 2010;148(3):327–333. doi: 10.1016/j.jconrel.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 11.Daddona PE, Matriano JA, Mandema J, Maa YF. Parathyroid Hormone (1-34) coated microneedle patch system: clinical pharmacokinetics and pharmacodynamics for treatment of osteoporosis. Pharm Res. 2010;28(1):159–165. doi: 10.1007/s11095-010-0192-9. [DOI] [PubMed] [Google Scholar]
- 12.McAllister DV, Wang PM, Davis SP, Park JH, Canatella PJ, Allen MG, Prausnitz MR. Microfabricated needles for transdermal delivery of macromolecules and nanoparticles: fabrication methods and transport studies. Proc Natl Acad Sci USA. 2003;100(24):13755–13760. doi: 10.1073/pnas.2331316100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birchall JC, Coulman SA, Pearton M, Allender CJ, Brian KR, Anstey A, Gateley C, Wilke N, Morrissey A. Cutaneous DNA delivery and gene expression in ex vivo human skin explants via wet-etch micro-fabricated micro-needles. J Drug Targ. 2005;13(7):415–421. doi: 10.1080/10611860500383705. [DOI] [PubMed] [Google Scholar]
- 14.Van Damme P, Oosterhuis-Kafeja F, Van der Wielen M, Almagor Y, Sharon O, Levin Y. Safety and efficacy of a novel microneedle device for dose sparing intradermal influenza vaccination in healthy adults. Vaccine. 2009;27(3):454–459. doi: 10.1016/j.vaccine.2008.10.077. [DOI] [PubMed] [Google Scholar]
- 15.Donnelly RF, Majithiya R, Singh TR, Morrow DI, Garland MJ, Demir YK, Migalska K, Ryan E, Gillen D, Scott CJ, Woolfson AD. Design, optimization and characterisation of polymeric microneedle arrays prepared by a novel laser-based micromoulding technique. Pharm Res. 2011;28(1):41–57. doi: 10.1007/s11095-010-0169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin CJ, Allender CJ, Brain KR, Morrissey A, Birchall JC. Low temperature fabrication of biodegradable sugar glass microneedles for transdermal drug delivery applications. J Control Release. 2012;158(1):93–101. doi: 10.1016/j.jconrel.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 17.Gill HS, Prausnitz MR. Pocketed microneedles for drug delivery to the skin. J Phys Chem Solids. 2008;69(5-6):1537–1541. doi: 10.1016/j.jpcs.2007.10.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gill HS, Prausnitz MR. Coating formulations for microneedles. Pharm Res. 2007;24(7):1369–1380. doi: 10.1007/s11095-007-9286-4. [DOI] [PubMed] [Google Scholar]
- 19.Gill HS, Prausnitz MR. Coated microneedles for transdermal delivery. J Control Release. 2007;117(2):227–237. doi: 10.1016/j.jconrel.2006.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fowler AV, Zabin I. Amino acid sequence of β-Galactosidase of Escherichia Coli. Proc Natl Acad Sci USA. 1997;74(4):1507–1510. doi: 10.1073/pnas.74.4.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Enzymatic assay of beta galactosidase. [12th August 2012];1999 http://www.sigmaaldrich.com Available at: http://www.sigmaaldrich.com/etc/medialib/docs/Sigma/Enzyme_Assay/g5635enz.Par.0001.File.tmp/g5635enz.pdf.
- 22.Griffith KL, Wolf RE., Jr Measuring beta-galactosidase activity in bacteria: cell growth permeabilization, and enzyme assays in 96-well arrays. Biochem Biophys Res Commun. 2002;290(1):397–402. doi: 10.1006/bbrc.2001.6152. [DOI] [PubMed] [Google Scholar]
- 23.Ng KW, Pearton M, Coulman SA, Anstey A, Gateley C, Morrissey A, Allender CJ, Birchall JC. Development of an ex vivo human skin model for intradermal vaccination: tissue viability and Langerhans cell behaviour. Vaccine. 2009;27(43):5948–5955. doi: 10.1016/j.vaccine.2009.07.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiss DJ, Liggitt D, Clark JG. In situ histochemical detection of beta-galactosidase activity in lung: assessment of X-Gal reagent in distinguishing lacZ gene expression and endogenous beta-galactosidase activity. Hum Gene Ther. 1997;8(13):1545–1554. doi: 10.1089/hum.1997.8.13-1545. [DOI] [PubMed] [Google Scholar]
- 25.Weiss DJ, Liggitt D, Clark JG. Histochemical discrimination of endogenous mammalian beta-galactosidase activity from that resulting from lac-Z gene expression. Histochem J. 1999;31(4):231–236. doi: 10.1023/a:1003642025421. [DOI] [PubMed] [Google Scholar]
- 26.Birchall JC, Clemo R, Anstey A, Jonh DN. Microneedles in clinical practice-an exploratory study into the opinions of healthcare professionals and the public. Pharm Res. 2011;28(1):95–106. doi: 10.1007/s11095-010-0101-2. [DOI] [PubMed] [Google Scholar]
- 27.Moreau MS, Cauiiepe C, Magues JP, Senard JM. A double-blind, randomized, comparative study of Dysport vs Botox in primary palmar hyperhidrosis. Br J Dermatol. 2003;149(5):1041–1045. doi: 10.1111/j.1365-2133.2003.05620.x. [DOI] [PubMed] [Google Scholar]
- 28.Solomon BA, Hayman R. Botulinum toxin type A therapy for palmarand digital hyperhidrosis. J Am Acad Dermatol. 2000;42(6):1026–1029. [PubMed] [Google Scholar]
- 29.Trindade de Almeida AR, Marques E, De Almeida J, Cunha T, Boraso R. Pilot study comparing the diffusion of two formulations of botulinum toxin type A in patients with forehead hyperhidrosis. Dermatol Surg. 2007;33(1):37–43. doi: 10.1111/j.1524-4725.2006.32330.x. [DOI] [PubMed] [Google Scholar]


