Abstract
Study Objectives:
Describe the prevalence of sleep disorders in military personnel referred for polysomnography and identify relationships between demographic characteristics, comorbid diagnoses, and specific sleep disorders.
Design:
Retrospective cross-sectional study.
Setting:
Military medical treatment facility.
Participants:
Active duty military personnel with diagnostic polysomnogram in 2010.
Measurements:
Primary sleep disorder rendered by review of polysomnogram and medical record by a board certified sleep medicine physician. Demographic characteristics and conditions of posttraumatic stress disorder (PTSD), mild traumatic brain injury (mTBI), anxiety, depression, and pain syndromes determined by medical record review.
Results:
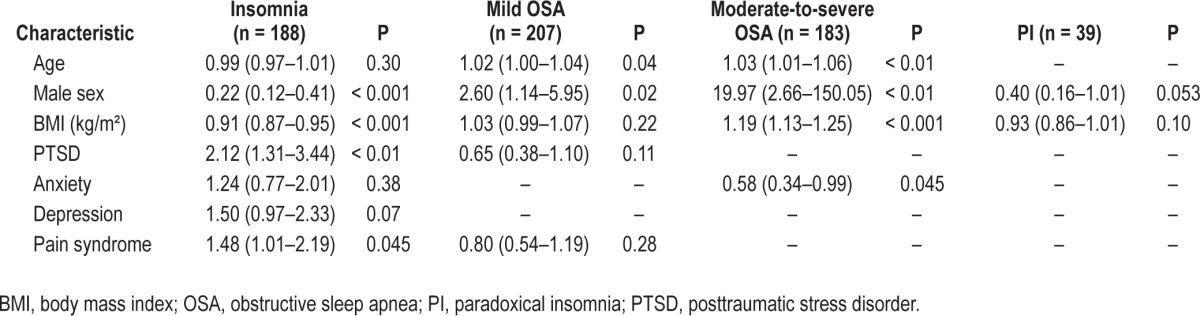
Primary sleep diagnoses (n = 725) included: mild obstructive sleep apnea (OSA), 207 (27.2%); insomnia, 188 (24.7%); moderate-to-severe OSA, 183 (24.0 %); and paradoxical insomnia,39 (5.1%); behaviorally induced insufficient sleep syndrome, 68 (8.9%) and snoring, 40 (5.3%) comprised our control group. Short sleep duration (< 5 h) was reported by 41.8%. Overall 85.2% had deployed, with 58.1% having one or more comorbid diagnoses. Characteristics associated with moderate-to-severe OSA were age (adjusted odds ratio [OR], 1.03 [95% confidence interval {CI}, 1.0–1.05], sex (male) (adjusted OR, 19.97 [95% CI, 2.66–150.05], anxiety (adjusted OR, 0.58 [95% CI, 0.34–0.99]), and body mass index, BMI (adjusted OR 1.19 [95% CI, 1.13–1.25]; for insomnia, characteristics included PTSD (adjusted OR, 2.12 [95% CI, 1.31–3.44]), pain syndromes (adjusted OR, 1.48 [95%CI, 1.01–2.12]), sex (female) (adjusted OR, 0.22 [95% CI, 0.12–0.41]) and lower BMI (adjusted OR, 0.91 [95% CI, 0.87, 0.95]).
Conclusions:
Service-related illnesses are prevalent in military personnel who undergo polysomnography with significant associations between PTSD, pain syndromes, and insomnia. Despite having sleep disorders, almost half reported short sleep duration. Multidisciplinary assessment and treatment of military personnel with sleep disorders and service-related illnesses are required.
Citation:
Mysliwiec V; McGraw L; Pierce R; Smith P; Trapp B; Roth BJ. Sleep disorders and associated medical comorbidities in active duty military personnel. SLEEP 2013;36(2):167-174.
Keywords: Deployment, insomnia, mild traumatic brain injury (mTBI), military, obstructive sleep apnea (OSA), posttraumatic stress disorder (PTSD), short sleep duration (SSD)
INTRODUCTION
More than two million military personnel have deployed to Iraq and Afghanistan in support of Overseas Contingency Operations.1 Both combat and noncombat experiences, as well as exposure to harsh environments and living conditions, contribute to the physical and psychosocial demands of deployment. The toll on the overall health of military personnel cannot be ignored. Musculoskeletal injuries are the most frequently reported physical injuries in military personnel; posttraumatic stress disorder (PTSD), depression, anxiety, and mild traumatic brain injury (mTBI) are the most common psychologic and neurologic injuries identified.2–4 Sleep disturbances, however, are increasing in frequency and are commonly diagnosed during deployment and when military personnel return from deployment (redeployment).5–7 Recent evidence suggests the increased incidence of sleep disturbances in redeployed military personnel is potentially related to PTSD, depression, anxiety, or mTBI.8–10 To date, no large cohort studies of redeployed military personnel with a definitive sleep disorder diagnosis exist; thus, it remains unclear if their sleep complaints are solely an epiphenomenon of comorbid illnesses, persistent maladaptive sleep practices that occur during deployment, or an independent diagnosis.11
The preponderance of research on sleep disorders in military personnel is limited by the use of data from subjective assessment tools or examination of specific diagnoses. Irrespective of deployment status, self-reported sleep duration ranges from 5.8 to 6.5 h nightly, consistent with short sleep duration (SSD).5–7,12 Those with prior deployments, significant combat exposures, or positive screening for PTSD, anxiety, and depression reported significantly less sleep.6,7 No specific cause of SSD was rendered in these studies, and it is conceivable that comorbid illnesses or insomnia contributed to these findings. Recent reports from Department of Defense medical data illustrate a marked increase in the International Classification of Diseases (ICD)-9 coded incident diagnoses of insomnia and obstructive sleep apnea (OSA) across all services.13,14 The incident rate of insomnia from 2000 to 2009 increased from 7.2 to 135.8 cases per 10,000 person-y whereas the rate of OSA increased from 25.6 to 145.3 cases per 10,000 person-y. One study evaluated polysomnographic (PSG) data in 69 redeployed soldiers with PTSD, TBI, and other mental health disorders; a diagnosis of OSA was made in 76.8%. This study was limited in that OSA was the only sleep diagnosis reported.15
The importance of sleep in military personnel working in technical occupations and operating in high-risk environments that require mental clarity and alertness cannot be overstated. Sleep deprivation and untreated sleep disorders are known to result in cognitive impairment, decreased performance, and increased accidents.16–18 For military personnel, performance without sufficient sleep may have devastating consequences, affecting both the individual and the unit's overall mission. Long-term sequelae of SSD include associations with increased mortality and medical disorders such as cardiovascular disease, obesity, and diabetes.19–22 SSD is also implicated as a potential basis for anxiety and PTSD.23,24 Identification of relationships between sleep disorders and comorbid illnesses may facilitate timely diagnosis and treatment, providing for improved sleep and duty performance as well as long-term health outcomes.
The objectives of this study were to describe the prevalence of sleep disorders in a sample of military personnel referred for PSG and identify relationships between demographic characteristics, comorbid diagnoses, and specific sleep disorders.
METHODS
Study Population
This was a retrospective cross-sectional cohort study of all diagnostic PSG performed on military personnel in calendar year 2010 at a major military medical treatment facility in the Pacific Northwest. Military personnel undergo a sleep medicine evaluation upon referral from their primary care or behavioral medicine provider, command directed when sleep difficulties hinder duty performance, or as part of a service-connected disability evaluation. It is our clinical practice to perform PSG on almost all military personnel who have a sleep medicine evaluation because they are in a high-risk profession. PSG performed for continuous positive airway pressure titration, postsurgical evaluation, or if the patient had previously undergone PSG were excluded. The institutional review board approved the research protocol and granted a waiver of informed consent. Medical record review was performed using the Armed Forces Health Longitudinal Technology Application system, the military electronic medical health record (EMR). Data elements were recorded in a de-identified database prior to statistical analysis. A total of 761 PSGs performed on active duty military personnel from the US Army, Air Force, and Navy at our institution in 2010 met inclusion criteria and were reviewed. For comparison of demographic and sleep characteristics, the control group consisted of military personnel receiving a diagnosis of either behaviorally induced insufficient sleep syndrome (BIISS) or snoring as their PSG variables were otherwise normal and comparable with those of individuals without an underlying sleep disorder.25
Study Variables
Baseline biometric parameters of age, height, weight, BMI, sex, and deployment history were obtained. Self-reported measures including home sleep duration (h), perceived sleep duration (h) during the overnight PSG and Epworth Sleepiness Scale (ESS) were recorded. Diagnoses of PTSD, mTBI, anxiety, and depression were obtained from the EMR problem list. Military personnel were classified with pain syndromes if traditional pain medications (e.g., opioids, muscle relaxants, antiepileptic agents) were on their self-reported medication list on the night of the PSG. Other active medications were categorized by drug class for data analysis: antidepressants, benzodiazepines, nonbenzodiazepine receptor agonist (NBDRAs), and prazosin, a sympatholytic drug originally used to treat high blood pressure, now used in the treatment of PTSD.
Diagnosis of Primary Sleep Disorder
The PSGs were performed using standardized techniques (Polysmith 5.0, Neurotronics, Gainesville, FL), with a subset of patients who met criteria for severe OSA undergoing a split- night PSG in accordance with laboratory policy. Polysomnography was performed with 16 channels, including: electrooculogram, electroencephalogram, electrocardiogram, electromyogram (submental, bilateral tibial), airflow measurements using both oronasal-thermal sensors and nasal air pressure transducers, tracheal sounds via microphone, rib cage and abdominal movement by inductance plethysmography using thoracoabdominal belts, and continuous pulse oximetry. The patient's sleep period was approximately 8 h in duration with recording time starting at 21:30 and ending at 05:30. All PSGs were scored by a registered polysomnography technician. Our laboratory uses the American Academy of Sleep Medicine alternative scoring method for hypopneas requiring a ≥ 50% decrease in the nasal pressure signal excursion from baseline lasting 10 sec or more with either a ≥ 3% desaturation or an arousal.26 The PSG variables we analyzed included sleep onset latency (SOL), rapid eye movement (REM) onset latency, total sleep time (TST), wakefulness after sleep onset (WASO), sleep efficiency (SE), arousal index (AI), sleep stages (stage N1, stage N2, stage N3, stage R), apnea-hypopnea index (AHI), and maximal desaturation.
We used the International Classification of Sleep Disorders, 2nd edition27 to classify the primary sleep disorder in our patients integrating the PSG data, ESS, self-reported home sleep duration, self-reported PSG sleep duration, and clinical notes. All diagnoses were adjudicated by one of two Sleep Medicine Boarded physicians (VM or BJR). For analysis purposes we used the following categories: mild OSA (AHI 5–15), moderate-to-severe OSA (AHI > 15), insomnia, paradoxical insomnia (PI), BIISS, snoring and “other” which encompassed infrequent diagnoses in our cohort. Moderate and severe OSA were grouped together because military personnel with this severity of disease require definitive treatment for deployability clearance.28 Insomnia was classified as either insomnia or PI, also known as sleep state misperception. This distinction was made given the significant differences in PSG variables between other forms of insomnia and PI. Military personnel with PI were required to have symptoms of insomnia with self-reported sleep duration of less than 4 h/night both at home and at the night of the PSG, with an otherwise normal PSG to include sleep architecture, sleep efficiency, TST, and arousal index along with an absence of other sleep disorders on their PSG. Individuals diagnosed with snoring required an audible report of snoring on the overnight PSG without other findings to suggest sleep disordered breathing or hypersomnolence, except if it could be directly attributed to SSD.
Statistical Analyses
Data were analyzed using PASW software (version 18.0, Chicago, IL). Differences between sleep diagnoses and a control group were assessed using chi square analyses with post hoc standardized residuals test for categorical variables and one-way analysis of variance with post hoc analyses using the Bonferroni correction for continuous variables. Although differences in patient characteristics and PSG variables existed between sleep disorders, the intent was to identify only differences between the control group (military personnel diagnosed with BIISS [n = 68] and snoring [n = 40]) and separate sleep disorders. Separate logistic regression models were examined to assess characteristics related to insomnia, PI, mild OSA, and moderate-to-severe OSA. Relevant variables of age, sex, PTSD, mTBI, anxiety, depression, and pain syndromes were entered in a univariate logistic regression model, with independent variables with P < 0.20 entered into a multivariate logistic regression model. For this portion of the analysis, military personnel who did not meet criteria for the specified diagnoses served as the outcome reference group. In the multivariate analyses, the significance was set at P < 0.05.
RESULTS
Seven hundred sixty-one PSGs and corresponding medical records were reviewed and adjudicated for a primary sleep disorder. We excluded 36 patients who had a PSG and met criteria for “other” diagnoses (Figure 1). Although relevant to identify these diagnoses in our population, the small numbers limit our ability to identify any substantive relationships with the independent variables of interest. Seven hundred twenty-five records were used in the analysis, comprised mostly of men (93.2%) and combat veterans (85.2%). The mean (SD) age of the group was 35.5 (8.6) y with a BMI of 29.8 (4.1) kg/m2. Their self-reported home sleep duration was 5.74 (1.54) h with an elevated ESS of 13.1 (5.0). The most frequently diagnosed primary sleep disorder was mild OSA (27.2%; n = 207), followed by insomnia (24.7%; n = 188), moderate to severe OSA (24.0%; n = 183), and PI (5.1%; n = 39) (Figure 2). Overall and group characteristics by sleep disorders are presented in Table 1. Insomnia and PI were more likely diagnosed in females than males; females were less likely to be diagnosed with moderate-to-severe OSA (χ24 = 45.58, P < 0.001). Those with insomnia were more often on prazosin (χ24 = 18.04, P = 0.001), pain medications (χ24 = 12.43, P = 0.014), antidepressants (χ24 = 22.39, P ≤ 0.001), and NBDRA (χ24 = 15.67, P = 0.003). Military personnel with insomnia were more likely to have a diagnosis in the EMR of anxiety (χ24 = 10.93, P = 0.03), depression (χ24 = 12.7, P = 0.013), PTSD (χ24 = 12.90, P = 0.012), and not surprisingly, two or more comorbid diagnoses (χ24 = 16.45, P = 0.002). The control group was composed of more military personnel with normal sleep duration and less with SSD than those with sleep disorders (both χ24 = 64.81, P < 0.001). As expected, SSD was universal in military personnel with PI (χ24 = 64.81, P < 0.001).
Figure 1.
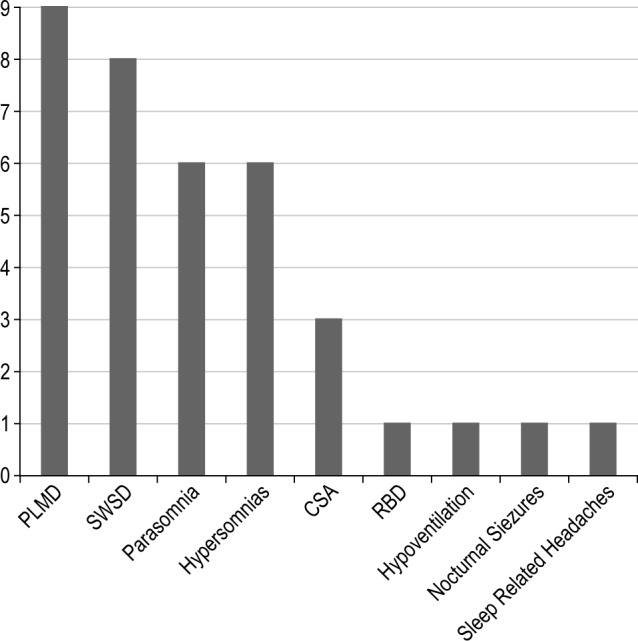
Other sleep disorders in military personnel. Parasomnia: three military personnel with somnambulism, two with nightmare disorder, one with sleep sex disorder. Hypersomnias: three military personnel with posttraumatic hypersomnia, two with idiopathic hypersomnia, one with narcolepsy without cataplexy. PLMD, periodic limb movement disorder; SWSD, shift work sleep disorder; CSA, central sleep apnea; RBD, rapid eye movement behavior disorder.
Figure 2.
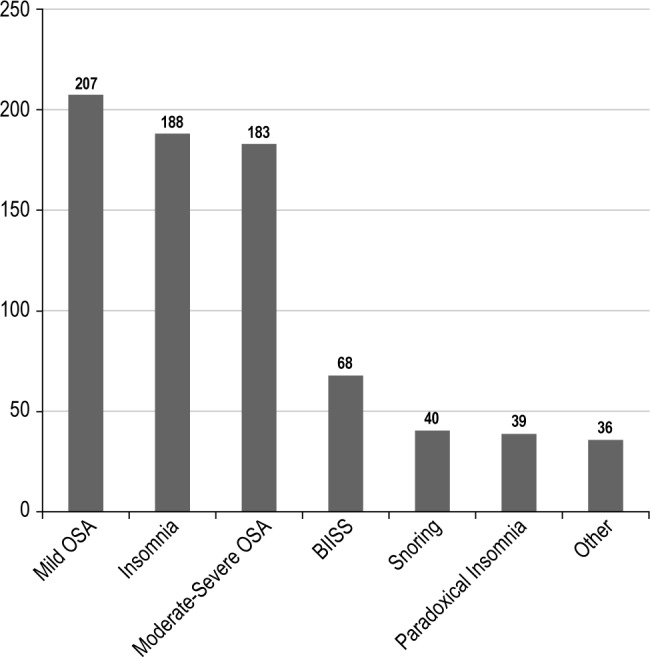
Primary sleep disorders in military personnel. Mild OSA (obstructive sleep apnea): apnea-hypopnea index (AHI) = 5–15/h. Moderate-to-severe OSA: AHI > 15/h. BIISS, behaviorally induced insufficient sleep syndrome. Other diagnoses presented in Figure 1.
Table 1.
Comparison of characteristics of military personnel by sleep diagnoses
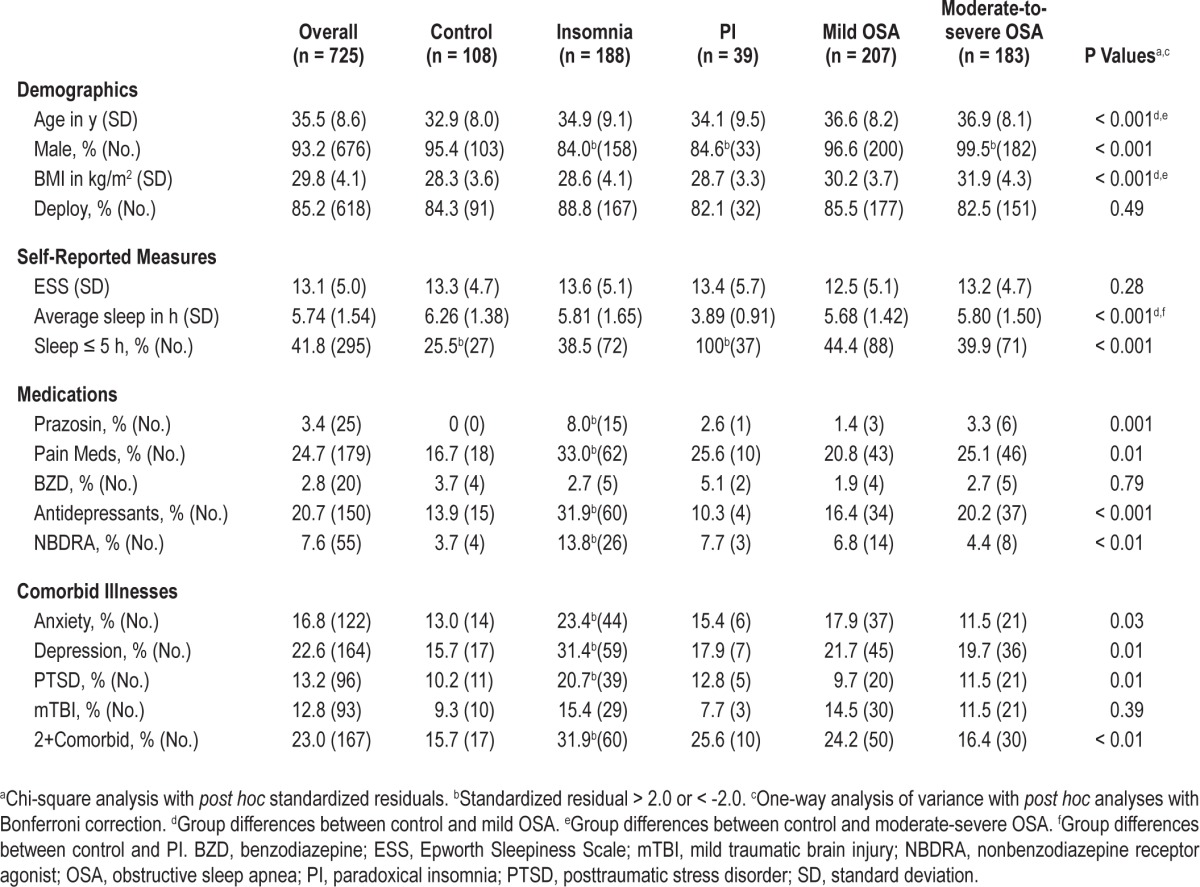
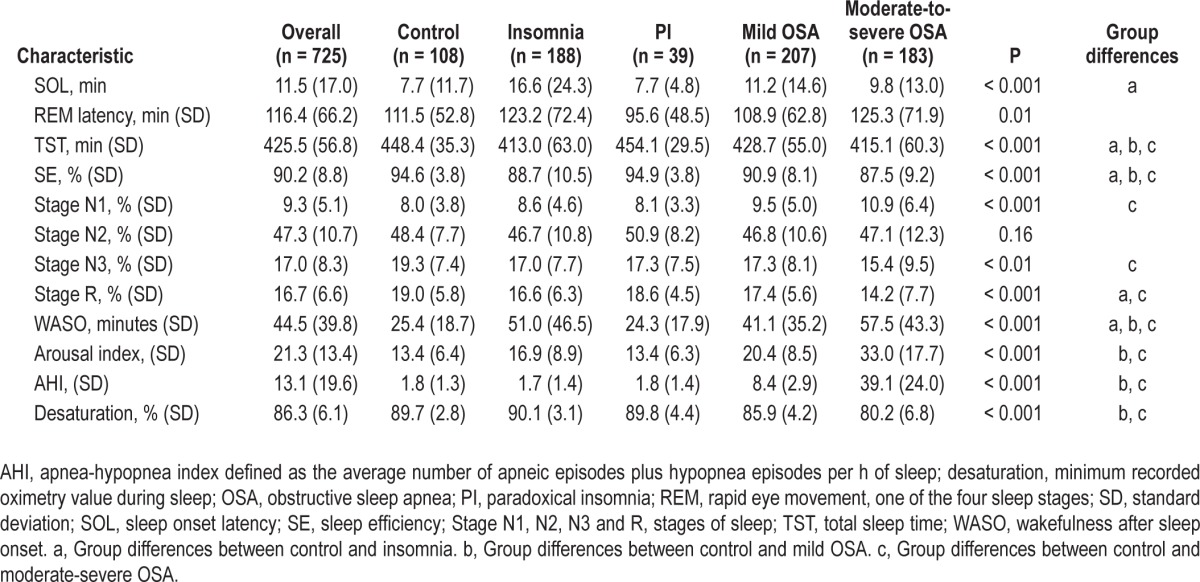
In comparison with the control group, significant differences were identified between groups on PSG variables clinically consistent with the respective sleep disorder and are presented in Table 2. Individuals with insomnia had increased SOL, WASO, and decreased SE and TST. Those with PI had normal PSG variables and were otherwise similar to the control group. Military personnel with mild and moderate-to-severe OSA had an elevated AHI and desaturation profile corresponding with their severity of disease with notable sleep architectural changes including an elevated AI, decreased SE, and decreased N3 and REM sleep.
Table 2.
Polysomnographic characteristics of military personnel by sleep diagnoses
In the multivariate model with insomnia as the outcome variable, males are less likely to have insomnia; the condition is more likely to be diagnosed in military personnel with PTSD, pain syndromes, and lower BMI. Older military personnel and males were more likely to have a diagnosis of mild and moderate-to-severe OSA; an elevated BMI and the absence of an anxiety diagnosis were also associated with moderate-to-severe OSA (Table 3).
Table 3.
Multivariate logistic regression analysis of biometric parameters and comorbidities associated with sleep diagnoses
DISCUSSION
This is the first study to systematically describe primary sleep disorders and associated comorbidities in a large cohort of military personnel referred with sleep complaints in accordance with standardized diagnostic criteria. OSA was the most frequent diagnosis in 51.2%, consistent with previous reports of primary sleep disorders at civilian sleep centers. However, our cohort otherwise differed as insomnia was diagnosed in 24.7% and BIISS was diagnosed in 8.9%, reported in 4.2% and 0.8% of patients, respectively, in civilian sleep centers.29 In the nonmilitary setting, individuals with insomnia and BIISS may not have obtained PSGs to arrive at a diagnosis.30 This highlights a potential difference in sleep evaluations because military service is a high-risk profession and ensuring the correct diagnosis is imperative. Notably, our results more closely reflect a recent report describing the prevalence of sleep disorders in North American police officers, where 40.4% screened positive for a sleep disorder with OSA and insomnia as the most common diagnoses.31
SSD is highly prevalent in our cohort, with a self-reported sleep duration average of 5.74 h of nightly sleep and 41.8% sleeping 5 h or less per night. This finding is consistent with prior studies of military personnel who habitually report SSD.6,7Compared with civilian reports, these findings are substantially higher than the 9.3% prevalence reported in the adult population in the United States32,33 (Figure 3). Although these data are not particularly surprising for military personnel, the unique aspect is that the prevalence of clinically relevant SSD (< 5 h) is not different across diagnostic groups. Further, the self-reported home sleep duration is not different between military personnel in the control group and those in whom insomnia or moderate-to-severe OSA is diagnosed. Military personnel face long work hours in both deployed and nondeployed settings and underlying this is a prevailing culture that “depriving oneself of sleep is a means of demonstrating mental and physical toughness.”34 The risk of accidents is likely increased in those with SSD and an associated sleep disorder.18 SSD is a significant health concern and potentially contributes to the growing number of military personnel with both sleep and comorbid medical disorders. A better understanding of the medical sequelae of SSD in military personnel is required.
Figure 3.
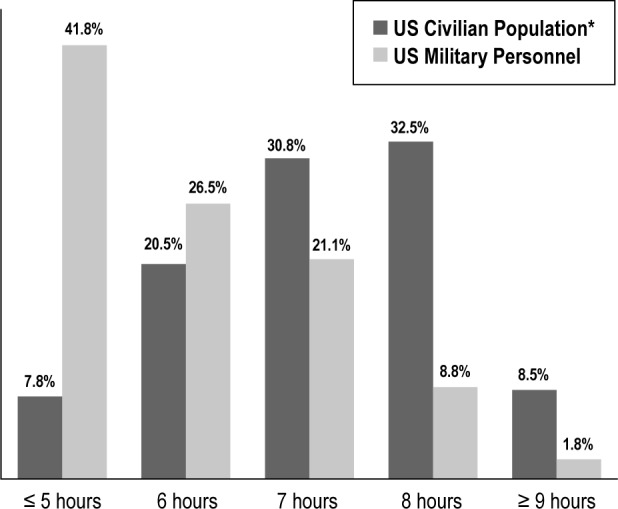
Comparison of self-reported home sleep duration per night between military personnel and US civilians. *Adapted from Krueger PM, Wallander JL: Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol 2009;169:1054.
The most common primary sleep disorder was OSA, with most patients having mild OSA. Male sex, increasing age, and obesity (known risk factors for OSA) were significantly associated with moderate-to-severe OSA in our cohort,35 and stand in contrast to a previous study suggesting BMI was not related to OSA in military personnel.36 The high percentage of mild OSA in military personnel may be overestimated in our population as they are referred for symptoms of excessive sleepiness, which would be expected because this diagnostic group had the shortest self-reported home sleep duration. Whether the symptom of sleepiness is attributable to insufficient sleep, mild OSA, or both is unclear. It is possible that military personnel, who are subjected to chronic sleep deprivation, present at an earlier stage of disease than civilians. We only used a primary sleep diagnosis to characterize patients, so in the presence of an AHI > 5 the diagnosis we typically rendered was mild OSA. Insomnia frequently is comorbid with OSA.37 It is likely that some military personnel in whom mild OSA was diagnosed had insomnia symptoms, which were the reasons for their sleep evaluation.
Insomnia was the second most common primary sleep disorder and the only diagnosis associated with the presence of any medical comorbidities. Consistent with civilian data, females in our study were less likely than males to have OSA and more likely to have insomnia.38,39 The medications documented at the time of the PSG were appropriate for the underlying comorbidities, noting that individuals with insomnia were significantly more likely to take NBDRAs.
Medical comorbidities were frequently identified in military personnel undergoing PSG, with 58.1% having one or more service-related illnesses. The percentages of military personnel with PTSD (13.2%) and mTBI (12.8%) are similar to previous reports, whereas a larger percentage of those in our study had depression (22.6%) and anxiety (16.8%).4,40,41 A potential reason is that insomnia often precedes anxiety and depression, resulting in the referral for sleep evaluation.39,42 Sleep disturbances are a core feature of the hyperarousal criteria for PTSD; thus, our finding that military personnel in whom insomnia is diagnosed were more likely to have PSTD is not surprising.43 The relationship of insomnia to PTSD, however, may not be solely as a symptom or a comorbid disorder. Disturbed sleep prior to a traumatic event is a risk factor for the development of PTSD.44 Persistent insomnia 4 mo after deployment predicts changes in depression and PTSD symptoms.45 Further, the sleep disturbances of insomnia and nightmares can persist despite appropriate therapy for PTSD.46 Our finding of an association between PTSD and insomnia highlights the need for a multicomponent management plan for these two illnesses that are interrelated.47
Military personnel with the diagnosis of pain syndromes were more likely to have insomnia. Poor sleep is a recognized symptom in individuals who have medical disorders associated with pain. Previous studies using both questionnaires and PSGs have reported patients with pain have difficulties initiating and maintaining sleep, supporting the association of pain syndromes with insomnia.48,49 In our cohort, 24.7% were identified as taking medications for pain. This finding is consistent with a high rate of combat-related musculoskeletal injuries.50 The implications of pain management and sleep disorders are important; individuals with inadequately controlled pain may have fragmented sleep. Conversely, the side effects of medications such as opioids can result in oversedation and central sleep apnea, which was the case for two of the patients reviewed. Management of military personnel with pain, sleep disorders, and multiple medications may improve with a sleep medicine evaluation to ensure comorbid pain and sleep disorders are appropriately treated and side effects of medications are minimized.51
The diagnosis of PI in 17.2% of our cohort with insomnia was an unexpected finding because it is viewed as relatively rare, seen in fewer than 5% of individuals in whom insomnia is diagnosed.27 Paradoxical insomnia is a distinct form of insomnia in which affected individuals have normal sleep duration but perceive sleeping very little or not at all. Current understanding of this form of insomnia is limited, with the suggestion that depressive traits and excessive central nervous system activation during sleep act as predisposing factors.52 Deployed military personnel do not sleep in a safe environment and must maintain a high level of vigilance at all times. Military personnel's inability to reintegrate into a safe sleeping environment after maintaining hypervigilance during deployment may contribute to a perceived lack of sleep. Military personnel with insomnia warrant either actigraphy or PSG based on the substantial number in whom PI is diagnosed, as without objective findings they would likely not receive this diagnosis. Differentiating insomnia from PI has implications in terms of management and comorbid diagnoses. In the setting of normal sleep, medical management with sedative hypnotic agents is not warranted and education on determining sleep versus wakefulness could prove helpful.53 Recent evidence suggests that hypnotic prescriptions are associated with an increased risk of mortality with substantial implications for military personnel who may develop long-term dependence.54 In our study PI is not associated with any comorbid disorders. A previous study reported those patients with PI did not have underlying medical disorders but possessed anxious ruminative traits and poor coping resources for stress.55
ESS scores were not significantly different between those in our control group and those in whom insomnia or OSA was diagnosed. The fact that military personnel in our study report significant sleepiness is not surprising, but those with insomnia reporting the highest ESS is notable. Sleepiness, while a known symptom of insomnia, is usually not of the severity seen in our cohort of military personnel. Individuals with OSA usually present with higher ESS values (typically around 12), whereas those with insomnia have lower values (typically around 6), which are in the normal range (0–9).56,57 Given the prevalence of medical comorbidities in military personnel with insomnia, it is possible their sleepiness is not solely due to their insomnia. Comorbid medical disorders that may not have responded to medical or behavioral therapies or the increased usage of medications with sedative effects could act synergistically with SSD, resulting in their perceived sleepiness.58 The exact reason for this finding is unknown and warrants further study.
There are strengths and limitations in our study that merit discussion. The inherent strength is that all the sleep diagnoses rendered included a review of their clinical record, self-reported symptoms, and PSG data. All previous reports of sleep disorders during Overseas Contingency Operations have relied on self-reported symptoms or focused on relatively specific diagnoses. Although this does not establish the overall prevalence of sleep disorders in military personnel, it does establish the prevalence of sleep disorders in those referred with sleep disturbances. Along with this, we provide a better understanding of sleep disorders and the common comorbidities military personnel have in relation to their deployments and combat experiences. The medical comorbidities were determined from diagnoses present in the EMR and may not accurately represent active illnesses. Only a primary sleep disorder was determined; a second sleep disorder was potentially present and was not considered. The increased use of PSG could have led to the overdiagnosis of mild OSA. The population of military personnel was selected from one military treatment facility that provides care for Army, Air Force, and Navy military personnel, but does not necessarily represent all Department of Defense facilities or veteran populations. Finally, the control population consisted of military personnel with the diagnoses of BIISS and primary snoring. These disorders, although not characterized by pathologic findings on PSG, are not necessarily healthy control conditions. This population was selected a priori because they are most likely to represent military personnel who do not have a significant sleep disorder except for SSD, and thus most closely represent a control for a military population. Despite the noted limitations, our study provides important findings regarding sleep disorders, as it is the first to assess a large cohort of military personnel during Overseas Contingency Operations and provide a reference regarding their diagnoses and associated medical conditions.
In conclusion, our study provides a unique insight into the growing body of evidence linking sleep disorders, and more specifically, insomnia and service-related illnesses that frequently occur in military personnel who have deployed in Overseas Contingency Operations. The dramatic self-report of SSD in our cohort is consistent with prior studies and suggests the need for a cultural change toward appropriate sleep practices throughout the military. Further research on specific performance and cognitive decrements associated with sleep deprivation as well as targeted interventions to address this accepted cultural paradigm in the armed forces must be conducted. Additionally, there is a gap in our understanding of the long-term health outcomes of military personnel with SSD and sleep disorders. Prospective studies examining the early assessment and treatment of those with sleep disorders would contribute to the understanding of this growing phenomenon in our military and veteran population.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the following for their contributions: Angela Mysliwiec, MD, Madigan Army Medical Center, for editing assistance and review of the manuscript; Tristin Baxter, AAS, Madigan Army Medical Center, for assistance with data collection and editing assistance; and Raywin Huang, PhD, Madigan Army Medical Center, for statistical consultation. None of these individuals received compensation for their contributions.
Vincent Mysliwiec, MD had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. This study was supported, in part, by grant #60855 from the Center for Neuroscience and Regenerative Medicine. The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript. The opinions and assertions in this manuscript are those of the authors and do not necessarily represent those of the Department of the Army, Department of Defense, US government, or the Center for Neuroscience and Regenerative Medicine.
Footnotes
A commentary on this article appears in this issue on page 159.
REFERENCES
- 1.Strengthening our military families: meeting America's commitment. 2012. [Accessed March 9]. http://www.defense.gov/home/features/2011/0111_initiative/strengthening_our_military_january_2011.pdf.
- 2.Associations between repeated deployments to OEF/OIF/OND, October 2001-December 2010, and post-deployment illnesses and injuries, active component, U.S. Armed Forces. MSMR. 2011;18:2–11. [PubMed] [Google Scholar]
- 3.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 4.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 2008;358:453–63. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 5.Peterson AL, Goodie JL, Satterfield WA, Brim WL. Sleep disturbance during military deployment. Mil Med. 2008;173:230–5. doi: 10.7205/milmed.173.3.230. [DOI] [PubMed] [Google Scholar]
- 6.Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–22. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34:1189–95. doi: 10.5665/SLEEP.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amin MM, Parisi JA, Gold MS, Gold AR. War-related illness symptoms among Operation Iraqi Freedom/ Operation Enduring Freedom returnees. Mil Med. 2010;175:155–7. doi: 10.7205/milmed-d-90-00153. [DOI] [PubMed] [Google Scholar]
- 9.McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175:759–62. doi: 10.7205/milmed-d-10-00193. [DOI] [PubMed] [Google Scholar]
- 10.Lewis V, Creamer M, Failla S. Is poor sleep in veterans a function of post-traumatic stress disorder? Mil Med. 2009;174:948–51. doi: 10.7205/milmed-d-04-0208. [DOI] [PubMed] [Google Scholar]
- 11.Gellis LA, Gehrman PR, Mavandadi S, Oslin DW. Predictors of sleep disturbances in Operation Iraqi Freedom/Operation Enduring Freedom veterans reporting a trauma. Mil Med. 2010;175:567–73. doi: 10.7205/milmed-d-09-00123. [DOI] [PubMed] [Google Scholar]
- 12.Mental Health Advisory Team (MHAT) V Operation Iraqi Freedom 06-08. 2011. [Accessed November 10]. http://www.armymedicine.army.mil/reports/mhat/mhat_v/mhat-v.cfm.
- 13.Insomnia, active component, U.S. Armed Forces, January 2000-December 2009. MSMR. 2010;17:12–15. [Google Scholar]
- 14.Obstructive sleep apnea, active component, U.S. Armed Forces, January 2000-December 2009. MSMR. 2010;17:8–11. [Google Scholar]
- 15.Capaldi VF, 2nd, Guerrero ML, Killgore WD. Sleep disruptions among returning combat veterans from Iraq and Afghanistan. Mil Med. 2011;176:879–88. doi: 10.7205/milmed-d-10-00440. [DOI] [PubMed] [Google Scholar]
- 16.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med. 2007;3:519–28. [PMC free article] [PubMed] [Google Scholar]
- 17.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 18.Drake C, Roehrs T, Breslau N, et al. The 10-year risk of verified motor vehicle crashes in relation to physiologic sleepiness. Sleep. 2010;33:745–52. doi: 10.1093/sleep/33.6.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30:1659–66. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 21.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep. 2007;30:1667–73. doi: 10.1093/sleep/30.12.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28:1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 23.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35:61–8. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pace-Schott EF, Milad MR, Orr SP, Rauch SL, Stickgold R, Pitman RK. Sleep promotes generalization of extinction of conditioned fear. Sleep. 2009;32:19–26. [PMC free article] [PubMed] [Google Scholar]
- 25.Pressman MR. Primer of polysomnogram interpretation. Waburn, MA: Butterworth-Heinemann; 2002. [Google Scholar]
- 26.Iber C, Ancoli-Israel S., Chesson AL, Jr, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 27.American Academy of Sleep Medicine. International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2nd ed. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 28.United States Central Command. PPG-TAB A: Amplification of the minimal standards of fitness for deployment to the CENTCOM AOR. 2012. [Accessed July 5, 2012]. http://pec.ha.osd.mil/files/MOD%2011%20Tab%20A%20%20Update%2027Mar12.pdf.
- 29.Punjabi NM, Welch D, Strohl K. Sleep disorders in regional sleep centers: a national cooperative study. Coleman II Study Investigators. Sleep. 2000;23:471–80. doi: 10.1093/sleep/23.4.471. [DOI] [PubMed] [Google Scholar]
- 30.Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- 31.Rajaratnam SM, Barger LK, Lockley SW, et al. Sleep disorders, health, and safety in police officers. JAMA. 2011;306:2567–78. doi: 10.1001/jama.2011.1851. [DOI] [PubMed] [Google Scholar]
- 32.Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975-2006. Sleep. 2010;33:37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169:1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller NL, Shattuck LG. Sleep patterns of young men and women enrolled at the United States Military Academy: results from year 1 of a 4-year longitudinal study. Sleep. 2005;28:837–41. doi: 10.1093/sleep/28.7.837. [DOI] [PubMed] [Google Scholar]
- 35.Pack AI. Advances in sleep-disordered breathing. Am J Respir Crit Care Med. 2006;173:7–15. doi: 10.1164/rccm.200509-1478OE. [DOI] [PubMed] [Google Scholar]
- 36.Lettieri CJ, Eliasson AH, Andrada T, Khramtsov A, Raphaelson M, Kristo DA. Obstructive sleep apnea syndrome: are we missing an at-risk population? J Clin Sleep Med. 2005;1:381–5. [PubMed] [Google Scholar]
- 37.Luyster FS, Buysse DJ, Strollo PJ., Jr. Comorbid insomnia and obstructive sleep apnea: challenges for clinical practice and research. J Clin Sleep Med. 2010;6:196–204. [PMC free article] [PubMed] [Google Scholar]
- 38.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–35. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 39.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 40.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–32. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 41.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167:476–82. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 42.Picchioni D, Cabrera OA, McGurk D, et al. Sleep symptoms as a partial mediator between combat stressors and other mental health symptoms in Iraq war veterans. Mil Psychol. 2010;22:340–55. [Google Scholar]
- 43.Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989;146:697–707. doi: 10.1176/ajp.146.6.697. [DOI] [PubMed] [Google Scholar]
- 44.Bryant RA, Creamer M, O'Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69–74. doi: 10.1093/sleep/33.1.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wright KM, Britt TW, Bliese PD, Adler AB, Picchioni D, Moore D. Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. J Clin Psychol. 2011;67:1240–58. doi: 10.1002/jclp.20845. [DOI] [PubMed] [Google Scholar]
- 46.Zayfert C, DeViva JC. Residual insomnia following cognitive behavioral therapy for PTSD. J Trauma Stress. 2004;17:69–73. doi: 10.1023/B:JOTS.0000014679.31799.e7. [DOI] [PubMed] [Google Scholar]
- 47.Ulmer CS, Edinger JD, Calhoun PS. A multi-component cognitive-behavioral intervention for sleep disturbance in veterans with PTSD: a pilot study. J Clin Sleep Med. 2011;7:57–68. [PMC free article] [PubMed] [Google Scholar]
- 48.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 49.Staedt J, Windt H, Hajak G, et al. Cluster arousal analysis in chronic pain-disturbed sleep. J Sleep Res. 1993;2:134–7. doi: 10.1111/j.1365-2869.1993.tb00076.x. [DOI] [PubMed] [Google Scholar]
- 50.Belmont PJ, Schoenfeld AJ, Goodman G. Epidemiology of combat wounds in Operation Iraqi Freedom and Operation Enduring Freedom: orthopaedic burden of disease. J Surg Orthop Adv. 2010;19:2–7. [PubMed] [Google Scholar]
- 51.Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307:940–7. doi: 10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- 52.Vanable PA, Aikens JE, Tadimeti L, Caruana-Montaldo B, Mendelson WB. Sleep latency and duration estimates among sleep disorder patients: variability as a function of sleep disorder diagnosis, sleep history, and psychological characteristics. Sleep. 2000;23:71–9. [PubMed] [Google Scholar]
- 53.Harvey AG, Sharpley AL, Ree MJ, Stinson K, Clark DM. An open trial of cognitive therapy for chronic insomnia. Behav Res Ther. 2007;45:2491–501. doi: 10.1016/j.brat.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 54.Kripke DF, Langer RD, Kline LE. Hypnotics' association with mortality or cancer: a matched cohort study. BMJ Open. 2012;2:e000850. doi: 10.1136/bmjopen-2012-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fernandez-Mendoza J, Calhoun SL, Bixler EO, et al. Sleep misperception and chronic insomnia in the general population: role of objective sleep duration and psychological profiles. Psychosom Med. 2011;73:88–97. doi: 10.1097/PSY.0b013e3181fe365a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 57.Moul DE, Nofzinger EA, Pilkonis PA, Houck PR, Miewald JM, Buysse DJ. Symptom reports in severe chronic insomnia. Sleep. 2002;25:553–63. [PubMed] [Google Scholar]
- 58.Roth T, Roehrs T. Insomnia: epidemiology, characteristics, and consequences. Clin Cornerstone. 2003;5:5–15. doi: 10.1016/s1098-3597(03)90031-7. [DOI] [PubMed] [Google Scholar]


