Abstract
Objectives:
The research determined (1) the information sources that family physicians (FPs) most commonly use to update their general medical knowledge and to make specific clinical decisions, and (2) the information sources FPs found to be most physically accessible, intellectually accessible (easy to understand), reliable (trustworthy), and relevant to their needs.
Methods:
A cross-sectional postal survey of 792 FPs and locum tenens, in full-time or part-time medical practice, currently practicing or on leave of absence in the Canadian province of Saskatchewan was conducted during the period of January to April 2008.
Results:
Of 666 eligible physicians, 331 completed and returned surveys, resulting in a response rate of 49.7% (331/666). Medical textbooks and colleagues in the main patient care setting were the top 2 sources for the purpose of making specific clinical decisions. Medical textbooks were most frequently considered by FPs to be reliable (trustworthy), and colleagues in the main patient care setting were most physically accessible (easy to access).
Conclusions:
When making specific clinical decisions, FPs were most likely to use information from sources that they considered to be reliable and generally physically accessible, suggesting that FPs can best be supported by facilitating easy and convenient access to high-quality information.
Highlights.
Medical textbooks were the most popular information source for family physicians' (FPs') clinical decision-making purposes, and medical journals were the most popular information source for the purpose of updating FPs' general medical knowledge.
FPs considered medical textbooks to be the most reliable (trustworthy) source, colleagues the most physically accessible, and continuing medical education the most relevant and intellectually accessible.
The lowest ranked information sources across all four attributes were personal digital assistants, mental health professionals, pharmaceutical sales representatives, and other decision aids.
Implications.
The most popular information sources for clinical decision-making purposes among FPs were sources characterized as reliable and generally physically accessible.
This study suggests the need for further research into interventions that target information access barriers in FPs' practice settings and the promotion of reliable evidence for FPs' clinical decision-making purposes.
INTRODUCTION
Clinical practice integrates tacit and explicit knowledge and requires expertise and judgment informed by patient values 1. Tacit knowledge “is the ‘knowing how’ which the clinician partners with the ‘knowing what’ of his explicit information. That is, it is the implicit knowledge which tells him how to use his explicitly known facts and rules” 2. Tacit, informal practice knowledge is based on experience and learned by observation 3, sources of which may include colleagues within the same practice, health professionals outside of the practice setting (e.g., specialists and pharmacists), and patients. Explicit knowledge is primarily gained by formal methods 3, such as rote learning 4, and may be drawn from sources that include medical texts, medical journals, clinical guidelines, drug manuals, and other forms of research-based media.
Information sources are equally important for the purposes of clinical decision making and continuing medical education 5 and contribute to physicians' tacit and explicit knowledgebases 6. However, physicians more often need information related to patient-specific decisions, such as questions about treatment 7,8 and diagnosis 7–9, than information to update their professional knowledge in general or further their understanding of a particular topic or disease 10.
Physicians' use of particular information sources for the purpose of clinical decision making may be associated with characteristics that physicians attribute to these sources. Studies suggest that physicians favor information that is concise 8; high quality 11; credible, trustworthy, and valid 8,12–14; presented attractively 8; convenient to access 11,12,14–16; clinically applicable and relevant 11,12,14–16; and easy to understand 12,15. A limited number of studies have directly investigated physicians' perceptions of particular information sources 8,12,13: two recent studies directly examined physicians' trust of sources 8,13, and an earlier 1990 study examined FPs' perceptions of credibility, availability, clinical applicability, and ease of understanding, among other information characteristics exhibited by common information sources 12.
Although it has been well established that colleagues and textbooks are the most popular information sources accessed by physicians to meet their clinical decision-making needs 9,11,14, there is a lack of current research investigating family physicians' (FPs') views on the accessibility, reliability, and relevance of these and other commonly used information sources. The main purposes of this study were to determine (1) the information sources most commonly used by FPs for the two separate purposes of updating their general medical knowledge and making specific clinical decisions, and (2) the information sources FPs found to be most physically accessible, intellectually accessible (easy to understand), reliable (trustworthy), and relevant to their needs.
METHODOLOGY
The results reported here were part of a larger survey of family physicians in Saskatchewan that received approval from the Behavioural Research Ethics Board of the University of Saskatchewan (BEH #07-41).
During June to October 2007, the authors conducted a pilot study survey of FPs and locum tenens practicing in the Canadian province of Saskatchewan (n = 100). An incentive to participate of $5 (Canadian) was included with the postal questionnaires. The sampling frame for the pilot study was drawn from the Canadian Medical Directory and the College of Physicians and Surgeons of Saskatchewan mailing list (n = 950). Surveys were completed by 30 of 78 eligible FPs (38% response rate). Ineligible persons were specialists, medical students, residents, retirees, and those employed primarily in nonclinical fields (i.e., administration, teaching, research). As in the triennial Canadian National Physician Survey, eligible physicians were FPs and locum tenens, in full-time or part-time medical practice, currently practicing or on leave of absence in Saskatchewan. Based on the results of the pilot study, questions were revised to improve readability and were eliminated to reduce questionnaire length. To improve the response rate, the incentive to participate was increased from $5 to $10 (Canadian), and data collection took place prior to summer holidays.
For the current study, the list of all locum tenens and FPs practicing in Saskatchewan was updated with the College of Physicians and Surgeons of Saskatchewan mailing list from December 2007 (n = 892). After removing the contact information for the FPs included in the pilot study, the sampling frame included 792 FPs and locum tenens.
Data were collected by mail questionnaire from January to April 2008. The questionnaire included a small ($10 [Canadian]) incentive to participate. Dillman's tailored design method 17, based on the principles of repeated and personalized contacts, informed data collection. Eligibility criteria for the present study followed the eligibility guidelines for the pilot study, with those individuals included in the pilot study sample ineligible for the present study.
Physicians received one of two similar eight-page questionnaires, one tailored to the care and treatment of depression (Appendix A, online only) and the other tailored to care and treatment of anxiety (Appendix B, online only). Both versions of the survey included questions concerning information use and perceptions of information sources addressed in the present study. Only data resulting from answers to questions on use of and evaluation of information sources are reported here.
To evaluate FPs' use of information sources, this study asked respondents to identify the sources that they regularly used (at least once per month) for two separate purposes: to update general medical knowledge and to make specific clinical decisions. Respondents indicated regular use by checking items from a list of fourteen sources. Checked items were classified as “use regularly,” and items not checked were coded as “do not use regularly.” This list was informed by previous studies that identified particular information sources preferred by physicians 4,9. This list included “psychiatrists” and “mental health professionals” as potential information sources in order to inform our larger project that investigated the care that FPs provided to patients with depression and anxiety 18,19. The information source “continuing medical education/continuing professional development/continuing professional learning (CME/CPD/CPL)” was not included in this list, because we determined that this information source was not applicable to making specific clinical decisions.
Given a similar list of fourteen information sources (with the addition of CME/CPD/CPL courses or programs and the removal of “other”), respondents were asked to indicate whether they found the information sources to exhibit, in general, four specific attributes identified in previous studies 9,11,12: reliability (trustworthiness), physical accessibility (easy to access), relevance (relevant to FPs' needs), and intellectual accessibility (easy to understand). To indicate that an information source exhibited these attributes, respondents checked boxes headed by the terms “reliable (you trust this source),” “easy to access,” “relevant (to your needs),” and “easy to understand.” Boxes that were not checked were taken to indicate that an information source was “not reliable,” “not easy to access,” “not relevant,” and “not easy to understand.”
RESULTS
Of the 792 FPs initially contacted to participate in the main study, 87 were ineligible, 30 had incorrect addresses on record, 8 were retired, and 1 physician was deceased. Of the remaining 666 eligible physicians, 331 completed and returned surveys, 129 (19.4%) refused to participate, and 206 (31.4%) did not respond. The response rate was 49.7% (331/666).
Of 331 respondents, 330 completed the “information use” section for the current study. This sample was fairly representative of Saskatchewan FPs in terms of age and gender and slightly over-representative of FPs in practice for a lengthier period of time 20. Thirty percent (29.6%, n = 98) of respondents were female, and the average age was 49.6 years (range 28–88, SD = 11.8). Respondents had been in practice an average of 19.2 years (range 1–50, SD = 11.6); 17.8% (n = 59) practiced solo; 66.5% (n = 220) were in private practice versus community clinics, hospitals, or health centres; and 82.5% (n = 273) had Internet access in their main patient care setting. Thirty-one percent (31.1%, n = 103) practiced in rural settings, defined as “Metropolitan Area and Census Agglomeration Influenced Zones” outside an urban core of 10,000 or more 21.
Information use for updating general medical knowledge and making clinical decisions
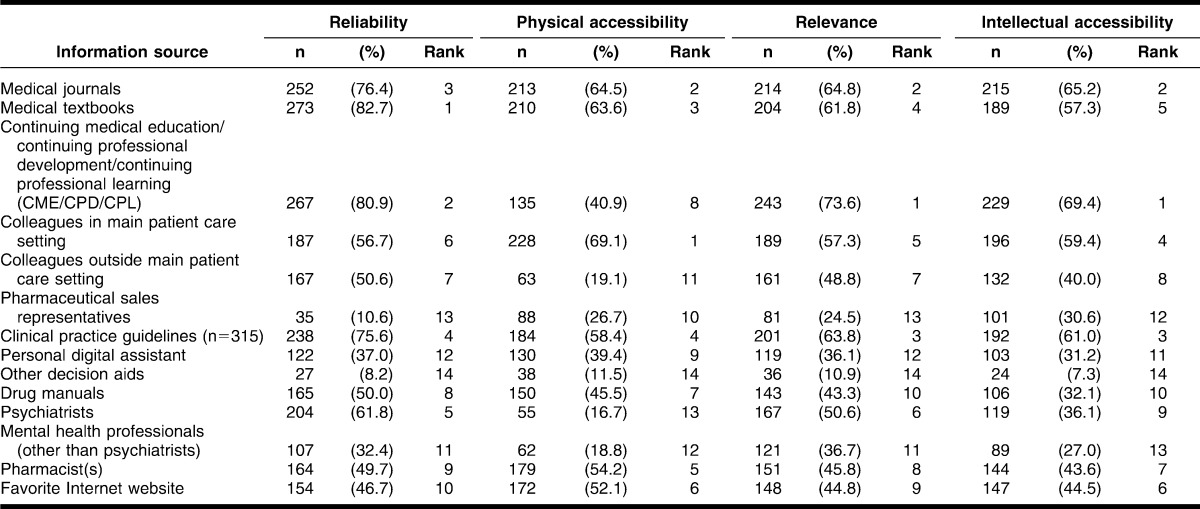
Medical journals (93.0%) were the most popular source of information for the purpose of updating respondents' general medical knowledge (Table 1). Clinical practice guidelines (70.0%) and favorite Internet website (49.4%) also ranked in the top 3 most frequently used sources. Among the 163 FPs (49.4%) who reported using a favorite Internet website to update their general medical knowledge, the top 5 websites included Canadian Medical Association (CMA) (27.6%), UpToDate (23.3%), eMedicine (14.7%), MD Consult (7.4%), and Google (6.7%). Respondents were least likely to update their general medical knowledge by using personal digital assistants (31.5%), pharmacists (29.1%), mental health professionals (21.8%), other decision aids (18.8%), and other information sources (9.3%)*.
Table 1.
Information sources used by family physicians to update general medical knowledge at least once per month (n = 330)
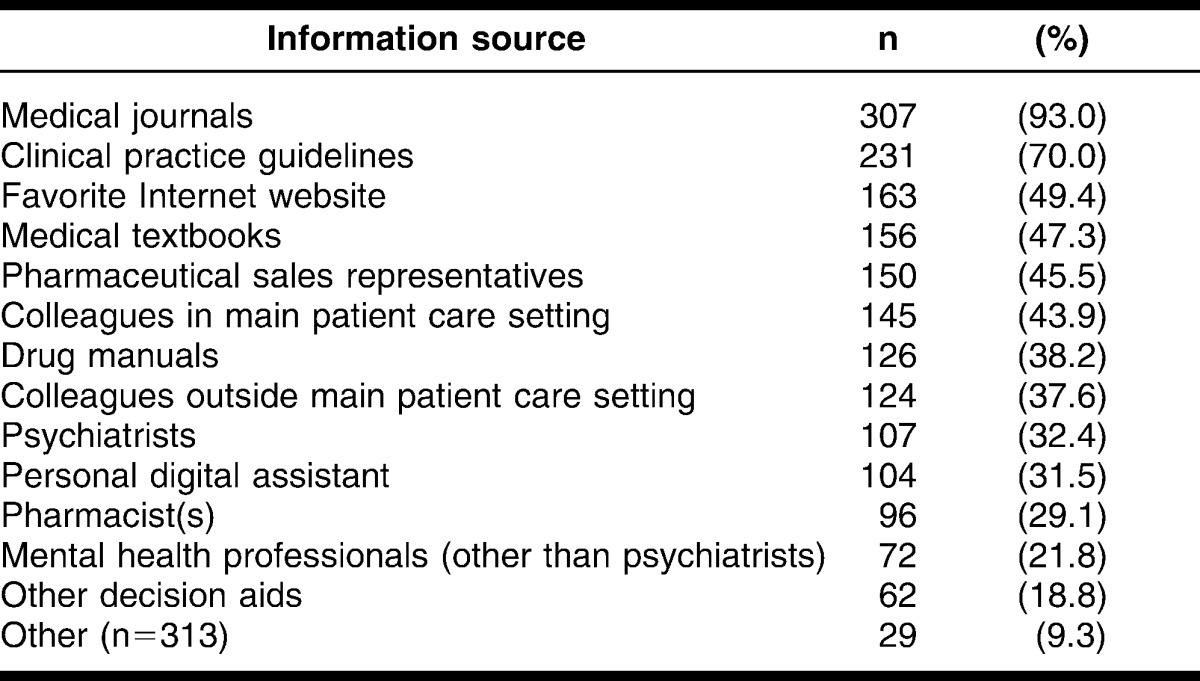
Medical textbooks (66.4%) were used most frequently to make specific clinical decisions, followed closely by colleagues in respondents' main patient care settings (62.4%) and psychiatrists (59.7%) (Table 2). The information sources used least often by respondents to make specific clinical decisions were personal digital assistants (34.5%), medical journals (25.2%), other decision aids (18.2%), other information sources (8.9%)*, and pharmaceutical sales representatives (4.2%).
Table 2.
Information sources used by family physicians to make specific clinical decisions at least once per month (n = 330)
Attributes of information sources
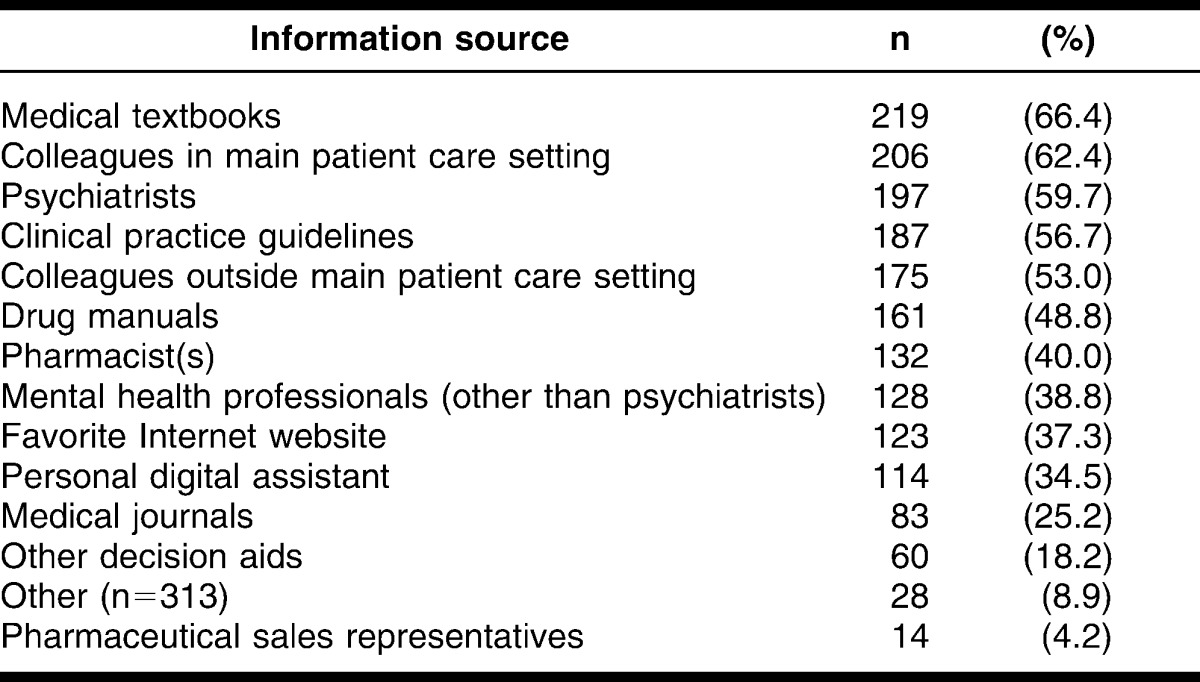
As shown in Table 3, medical journals ranked in the top 3 on all 4 attributes of information, as determined by the frequency of respondents who perceived each source to generally exhibit each of 4 attributes (Table 3). The 3 most popular information sources in terms of reliability (trustworthiness) were medical textbooks (82.7%), CME/CPD/CPL courses or programs (80.9%), and medical journals (76.4%). The top information source for physical accessibility was colleagues in the main patient care setting (69.1%), followed by medical journals (64.5%) and medical textbooks (63.6%). In terms of relevance, the top 3 information sources were CME/CPD/CPL courses or programs (73.6%), medical journals (64.8%), and clinical practice guidelines (63.8%)†. The 3 information sources that most respondents found intellectually accessible were CME/CPD/CPL courses or programs (69.4%), medical journals (65.2%), and clinical practice guidelines (61%). The lowest ranked information sources across all 4 attributes were personal digital assistant, mental health professionals, pharmaceutical sales representatives, and other decision aids.
Table 3.
Frequency of response and ranking on four attributes of information sources (by frequency of response) (n = 330)
Information use for clinical decision making and attributes of information sources
Medical textbooks and colleagues in the main patient setting were used by the greatest proportion of FPs for the purpose of making specific clinical decisions. Medical textbooks also ranked first on reliability (82.7%) and in the top 3 on physical accessibility (63.6%), whereas colleagues in the main patient care setting ranked first on physical accessibility (69.1%) and below the top 3 on all other attributes (56.7% to 59.4%).
Although psychiatrists (59.7%) and clinical practice guidelines (56.7%) were the third and fourth most frequently used information sources for the purpose of making specific clinical decisions, psychiatrists did not rank in the top 3 on any of the 4 examined attributes (16.7% to 61.8%), and clinical practice guidelines ranked in the top 3 on relevance and intellectual accessibility (61.0% to 63.8%).
CME/CPD/CPL, the top-ranked source on relevance (73.6%) and intellectual accessibility (69.4%), was not included in the list asking respondents to indicate those information sources that they used to update general medical knowledge and to make specific clinical decisions. Medical journals were the second-ranked source on these 2 attributes (relevance, 64.8%; intellectual accessibility, 65.2%). However, notably few respondents used medical journals for the purpose of making specific clinical decisions (25.2%).
Limitations
The response rate of 50% is comparable to response rates ranging from 36% to 75% 22–24 for other published survey studies of Canadian FPs. Generalizability of study results to Canadian FPs might be limited by overrepresentation of FPs who had been in practice for a longer time. Certain devices termed information sources in this study may be better understood as means to access information sources (e.g., personal digital assistant). FPs might have interpreted use of medical journals and textbooks to refer to both web-based and print formats, in which case FPs' actual Internet use and ratings (reliability, accessibility, and relevance) might be higher than indicated by FPs' reported use and ratings of “favorite Internet website.” Furthermore, measures created specifically for use in this study may have low reliability. For instance, information use was measured by self-report items that required a check mark to indicate “yes.” Respondents who did not check the items were assumed to have replied “no.” We employed this measure to minimize the bias of nonresponse. However, it is possible that respondents did not intend to answer “no” when they did not place a check mark next to an item. For this reason, this study might have underestimated nonresponse rates.
DISCUSSION AND CONCLUSION
The present study found that medical journals were the most popular information source among FPs for the purpose of updating general medical knowledge. Far fewer FPs reported using clinical practice guidelines and their favorite Internet website, the second and third most popular information sources for this particular purpose.
Among FPs, medical textbooks were the most popular source for making specific clinical decisions, followed closely by colleagues in their main patient settings and psychiatrists. These findings lend support to the pattern noted in two separate reviews of pre-2006 9 and pre-2002 11 literature that medical textbooks, followed by colleagues, were the most popular information sources among physicians for clinical decision-making purposes. A third review of pre-2006 literature concluded that textbooks and colleagues were equally popular among primary care physicians 14. More recent studies (published since 2006) concluded that physicians were more likely to use colleagues than textbooks to answer clinical questions 10,13,16,25.
The present study indicates that the top two information sources for clinical decision making, medical textbooks and colleagues in the main patient care setting, rated high overall in terms of physical accessibility (#3 and #1) and rated high to mid-range in terms of reliability, in other words, trustworthiness (#1 and #6, respectively). The other information sources that ranked in the top four to make clinical decisions, psychiatrists and clinical practice guidelines (#3 and #4, respectively), ranked in the top five on reliability and varied in terms of physical accessibility (#13 and #4, respectively). In an early US study, Connelly et al. found that FPs perceived credibility to be highest among medical textbooks and colleagues from other specialties 12. In a New Zealand study, Dovey et al. found that hospital colleagues were the most trusted information source among primary care physicians 8. In their study of Mongolian hospital doctors, Callen et al. found that the top two trusted sources were medical textbooks and colleagues 13.
The proportion of FPs who reported using their favorite Internet website to make specific clinical decisions (37%) and update their general medical knowledge (49%) is in the low end of the range indicated in previous studies of physicians' use of the Internet to search for medical information prompted by a specific patient problem (34%) 10, “look for clinical information” (49%) 27, “find medical information” (80%) 26, and “seek information in clinical practice” (85%) 28. The present study indicates that FPs' favorite Internet website ranked 6th and lower on reliability, relevance, physical accessibility, and intellectual accessibility, while medical journals and textbooks ranked in the top 5 on all 4 attributes. These findings indicate websites lag behind several other information sources in terms of all 4 attributes and may further indicate that medical information derived from such sites does not yet satisfy the criteria necessary to appeal to the majority of FPs searching for evidence to answer specific clinical questions.
Given the widespread availability of web-based resources and the increasing amount of electronically available medical knowledge, it is apparent that the use of web-based information among physicians for the purposes of updating knowledge and clinical decision making will continue to increase 30. Indeed, recent research suggests that physicians' use of computer-based versions of traditionally text-based sources (e.g., online journals, databases such as MEDLINE, and evidence-based medicine resources such as UpToDate) is becoming more commonplace 5,9,29. Studies have identified more time 28,29,30, easy access to electronic resources 29,30, summarized and reliable information 28, simplified information-seeking capabilities 28, and websites with relevant information for clinical practice or useful links 28,30 as facilitators of online information use.
Findings from the present study suggest that to make specific clinical decisions, FPs report using information that they characterize to be reliable (trustworthy) and generally physically accessible. These findings suggest that FPs' clinical decisions can best be supported by facilitating easy and convenient access to high-quality information sources. Further research into interventions that target FPs' practice settings to decrease barriers to information access and strategies that promote the uptake of reliable evidence for FPs' clinical decision-making purposes is warranted.
Electronic Content
Footnotes
This research was supported by funding from Kelsey Trail Regional Health Authority and Ralston Brothers Medical Research Fund. Julie G. Kosteniuk was supported by a Canadian Institutes of Health Research (CIHR) doctoral research award in continuing health education and a fellowship from the CIHR Strategic Training Program in Public Health and the Agricultural Rural Ecosystem (PHARE).
This article has been approved for the Medical Library Association's Independent Reading Program <http://www.mlanet.org/education/irp/>.
Supplemental Appendix A and Appendix B are available with the online version of this journal.
The response rate for other information sources is 313 because 17 respondents who wrote a response did indicate whether they used this information source to “update their general medical knowledge” or “make specific clinical decisions.” The 2 variables for these 17 cases were coded as “missing,” reducing the n to 313 from 330.
The response rate is 315 for clinical practice guidelines due to an error in the anxiety questionnaire initially printed and mailed to respondents, which initially incorrectly read “Medical textbooks” rather than “Clinical practice guidelines” in question 2 of section B. By the time this error was caught and corrected, some questionnaires had already been mailed to respondents. As a result, 15 respondents returned an incorrect version of the questionnaire. The 4 variables for these 15 cases were coded as “missing,” reducing the n to 315 from 330.
REFERENCES
- 1.Thornton T. Tacit knowledge as the unifying factor in evidence based medicine and clinical judgement. Philos Ethics Humanit Med. 2006 Mar;1(2) doi: 10.1186/1747-5341-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldman G. The tacit dimension of clinical judgment. Yale J Biol Med. 1990 Jan–Feb;63:47–61. [PMC free article] [PubMed] [Google Scholar]
- 3.Epstein R. Mindful practice. JAMA. 1999 Sep;282(9):833–39. doi: 10.1001/jama.282.9.833. [DOI] [PubMed] [Google Scholar]
- 4.Sturmberg J, Martin C. Knowing—in medicine. J Eval Clin Pract. 2008 Oct;14:767–70. doi: 10.1111/j.1365-2753.2008.01011.x. [DOI] [PubMed] [Google Scholar]
- 5.Gravatt Z, Arroll B. What resources do Auckland general practitioners use for answering immediate clinical questions and for lifelong learning. J Prim Health Care. 2010 Jun;2(2):100–04. [PubMed] [Google Scholar]
- 6.Gabbay J, le May A. Evidence based guidelines or collectively constructed “mindlines?” ethnographic study of knowledge management in primary care. BMJ. 2004 Oct;329(7473):1013. doi: 10.1136/bmj.329.7473.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez-Gonzalez A, Dawes M, Sanchez-Mateos J, Riesgo-Fuertes R, Escortell-Mayor E, Sanz-Cuesta R, Hernandez-Fernandez R. Information needs and information behavior of primary care physicians. Ann Fam Med. 2007 Jul;5(4):345–52. doi: 10.1370/afm.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dovey S, Fraser T, Tilyard M, Ross S, Baldwin K, Kane D. ‘Really simple, summary, bang! That's what I need.’. N Z Fam Physician. 2006 Feb;33(1):18–24. [Google Scholar]
- 9.Davies K. The information-seeking behaviour of doctors: a review of the evidence. Health Info Lib J. 2007 Jun;24:78–94. doi: 10.1111/j.1471-1842.2007.00713.x. [DOI] [PubMed] [Google Scholar]
- 10.Bennett N, Casebeer L, Zheng S, Kristofco R. Information-seeking behaviors and reflective practice. J Contin Educ Health Prof. 2006 Spring;26(2):120–27. doi: 10.1002/chp.60. [DOI] [PubMed] [Google Scholar]
- 11.Dawes M, Sampson U. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inform. 2003 Aug;71:9–15. doi: 10.1016/s1386-5056(03)00023-6. [DOI] [PubMed] [Google Scholar]
- 12.Connelly D, Rich E, Curley S, Kelly J. Knowledge of resource preferences of family physicians. J Fam Pract. 1990 Mar;30(3):353–60. [PubMed] [Google Scholar]
- 13.Callen J, Buyankhishig B, McIntosh J. Clinical information sources used by hospital doctors in Mongolia. Int J Med Inform. 2008 Apr;77(2):249–55. doi: 10.1016/j.ijmedinf.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Coumou H, Meijman F. How do primary care physicians seek answers to clinical questions? a literature review. J Med Lib Assoc. 2006 Jan;94(1):55–60. [PMC free article] [PubMed] [Google Scholar]
- 15.Verhoeven A, Boerma E, Meyboom-de Jong B. Use of information sources by family physicians: a literature survey. Bull Med Lib Assoc. 1995 Jan;83(1):85–90. [PMC free article] [PubMed] [Google Scholar]
- 16.Dwairy M, Dowell A, Stahl J. The application of foraging theory to the information searching behaviour of general practitioners. BMC Family Practice. 2011 Aug;12:90. doi: 10.1186/1471-2296-12-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dillman D. Mail and Internet surveys: the tailored design method. New York, NY: Wiley & Sons; 2007. [Google Scholar]
- 18.Kosteniuk J, Morgan D, D'Arcy C. Diagnoses of anxiety and depression in clinical scenario patients: survey of Saskatchewan family physicians. Can Fam Physician. 2012 Mar;58(3):e144–51. [PMC free article] [PubMed] [Google Scholar]
- 19.Kosteniuk J, Morgan D, D'Arcy C. Treatment and follow-up of anxiety and depression in clinical scenario patients: survey of Saskatchewan family physicians. Can Fam Physician. 2012 Mar;58(3):e152–8. [PMC free article] [PubMed] [Google Scholar]
- 20.College of Family Physicians of Canada. National physician survey. Ottawa, ON, Canada: Canadian Medical Association; 2007. [Google Scholar]
- 21.Harris S, Alasia A, Bollman R. Rural commuting: its relevance to rural and urban labour markets. Rural and Small Town Canada Analysis Bulletin. Statistics Canada: catalogue no. 75-001-X, 2008.11. [Google Scholar]
- 22.Hillmer M, Krahn M, Pariser P, Naglie G. Prescribing patterns for Alzheimer's disease: survey of Canadian family physicians. Can Fam Physician. 2006 Feb;52:208–9. [PMC free article] [PubMed] [Google Scholar]
- 23.Clatney L, MacDonald H, Shah S. Mental health care in the primary care setting. Can Fam Physician. 2008 Jun;54:884–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrari R, Russell A. Survey of general practitioner, family physician, and chiropractor's beliefs regarding the management of acute whiplash patients. Spine. 2004 Oct;29:2173–7. doi: 10.1097/01.brs.0000141184.86744.37. [DOI] [PubMed] [Google Scholar]
- 25.Jones TH, Hanney S, Buxton MJ. The information sources and journals consulted or read by UK paediatricians to inform their clinical practice and those which they consider important: a questionnaire survey. BMC Pediatr. 2007 Jan;7(1) doi: 10.1186/1471-2431-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Casebeer L, Bennet N, Kristofco R, Carillo A, Centor R. Physician Internet medical information seeking and on-line continuing education use patterns. J Contin Educ Health Prof. 2002 Winter;22:33–42. doi: 10.1002/chp.1340220105. [DOI] [PubMed] [Google Scholar]
- 27.Cullen RJ. In search of evidence: family practitioners' use of the Internet for clinical information. J Med Lib Assoc. 2002 Oct;90(4):370–9. [PMC free article] [PubMed] [Google Scholar]
- 28.Bernard E, Arnould M, Saint-Lary O, Duhot D, Hebbrecht G. Internet use for information seeking in clinical practice: a cross-sectional survey among French general practitioners. Int J Med Inform. 2012 Jul;81(7):493–9. doi: 10.1016/j.ijmedinf.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Flynn M, McGuinness C. Hospital clinicians' information behaviour and attitudes towards the ‘Clinical Informationist’: an Irish survey. Health Info Lib J. 2011 Mar;28(1):23–32. doi: 10.1111/j.1471-1842.2010.00917.x. [DOI] [PubMed] [Google Scholar]
- 30.Davies KS. Physicians and their use of information: a survey comparison between the United States, Canada, and the United Kingdom. J Med Lib Assoc. 2011 Jan;99(1):88–91. doi: 10.3163/1536-5050.99.1.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.