Abstract
Medication adherence is a substantial problem in the elderly. It may be even more important among elderly persons with memory problems, since other factors that lead to non-adherence may be compounded with the memory problems themselves. The objective was to determine whether a model that integrates research on medication adherence from several research domains is useful in understanding adherence in elderly patients. The methodology involved a cross-sectional observational study using a convenience sample of 63 patients drawn from a university-affiliated outpatient memory disorders clinic. The primary measure of medication adherence was caregivers’ reports of patients’ medication adherence. Patients and their caregivers were asked questions assessing their beliefs about the seriousness of each condition for which a medication was prescribed and the likely outcome of that condition without treatment. Additional data collected included presence of side effects, total number of medications taken, and patients’ mood and cognitive status. Multilevel path analysis confirmed several model-based predictions. Caregivers’ reports of adherence were predicted by estimates of disease outcome, the presence of side effects, and patients’ relying on themselves to remember to take medications. Results partially confirm the integrative model in understanding medication adherence in these patients. Patients’ beliefs about the likely effect of medication treatment for their condition and the presence of side effects influence reported medication adherence. Results thus suggest that efforts to educate patients about the likely response of their medical condition to treatment and to assess and deal with medication side effects might improve patient adherence.
Introduction
The report on medical errors of the Institute of Medicine (Kohn, Corrigan & Donaldson, 2000) identified medication non-adherence as an important source of medical errors. Low levels of adherence may decrease the effects of prescribed medications or other treatments and increase the likelihood of poor outcomes (McDonald, Garg & Haynes, 2002). Close relations between adherence and intermediate clinical outcomes have been demonstrated for a number of diseases, and a significant number of adverse events have been linked to non-adherence among the elderly (Gurwitz, Field & Harrold, 2003).
Low levels of adherence to prescribed medications have been documented in older adults with a number of chronic diseases, including hypertension (Bobb-Liverpool, Duff & Bailey, 2002), congestive heart failure (Evangelista et al., 2003), statin treatment in patients with cardiovascular disease (Applegate, 2002) and asthma (Barr, Somers, Speizer & Camargo, Jr., 2002). Evidence has shown that cognitive and memory problems may play an important role in medication adherence (Ganguli et al., 2004; Salas et al., 2001), but few readily-identifiable studies have explicitly examined the role of cognitive factors in adherence among patients with known memory problems that do not preclude self care, such as mild cognitive impairment (MCI) or early Alzheimer’s disease (AD).
Medication adherence is a complex behavior that can be influenced by patient beliefs and knowledge, patient characteristics such as socioeconomic status, depression, and age, and the methods by which patients try to remember to take their medications. The Health Belief Model (Janz & Becker, 1984), for example, implies that medication adherence will be related to patients’ beliefs about the seriousness of their disease, the likelihood that the medication will affect the disease and obstacles they encounter in taking their medication. Other social cognitive theories similarly specify that patient beliefs about the nature of the disease and its treatment are likely to influence health behaviors such as medication adherence (Leventhal, Leventhal, Robitaille & Brownlee, 1999). Patient characteristics that may influence levels of medication adherence include age, education, and socioeconomic status (Dunbar-Jacob & Schlenk, 2001). Depression may also be a particularly important factor in medication adherence (DiMatteo, Lepper & Croghan, 2000), and patients’ memory functioning is also important. Finally, it is likely that medication adherence can be affected by the means by which patients remember to take their medications (Park, Morrell, Frieske & Kincaid, 1992). Survey data (Gould, 1999) show that older adults’ strategies for remembering can be grouped into internal (for example, trying hard to learn about medication instructions) and external (leaving the pills in a prominent place) groups.
In attempt to integrate these different areas of research, Park and Jones (1997) suggest that there are three general approaches to understanding adherence: (a) a focus on patient beliefs about their illness; (b) a focus on how patient characteristics affect medication adherence; and (c) a focus on mnemonic strategies, such as pillboxes or reminders to assist patients in adherence. Park and Jones (1997) organize observations about each area’s contribution to understanding adherence into an integrative theory of medication adherence. This theory is appealing because it strives to reconcile different approaches to understanding medication adherence.
No readily identifiable study has investigated medication adherence in patients with memory disorders. This group of persons may be especially at risk for non-adherence, given their memory deficits. A better understanding of adherence in this group may thus be desirable. Further, confirming the validity of the Park and Jones (1997) theory for understanding medication adherence in the elderly might provide a useful tool for investigations of medication adherence in this group. The purpose of this study was thus to investigate factors related to adherence in patients seen at a memory disorders clinic in the context of the Park and Jones model.
Method
Medication adherence was studied in a convenience sample of 75 patients evaluated at a universityaffiliated memory disorders clinic. Of these 75, 63 had caregivers who could provide sufficient data to be used in subsequent analyses of adherence. Patients with memory disorders who were willing to complete an additional questionnaire during routine evaluation or follow-up visits to the clinic participated in the study. Data collected were selected to represent the domains described by the Park and Jones (1997) model of medication adherence. In the area of disease representation, a questionnaire was developed that assessed patients’ views of their illnesses and the medication used in their treatment. This questionnaire asked patients what medications they took and for what purpose. For each medication, patients were asked to rate on a five-point Likert-type scale the seriousness of the condition for which the medication was taken and the likely outcome if medication were not taken as directed. Both patients and their caregivers were asked how often the patient took the medication on a five-point scale, ranging from ‘Almost never’ to ‘Almost always’. For each medication, patients were asked how they remembered to take their medication. Methods reported fell into three main groups: (a) remembering by oneself, usually by incorporating taking the medication into a daily routine such as having breakfast but not using any aid such as a calendar or pillbox; (b) reliance on another person, usually a spouse or other caregiver; and (c) reliance on a mechanical aid such as a pillbox with sections for each day’s doses.
Finally, patients were asked whether they experienced any side effects from each medication, and if so, what they were. Information obtained from the questionnaire thus also allowed assessment of the total number of medications taken by each patient. Information about how patients remembered to take medication allowed assessment of the portion of the Park and Jones model that focuses on the use of external memory supports. For data analyses, this item was collapsed into a single binary item reflecting whether or not the patient relied on him or herself or a caregiver or mechanical aid to remember to take his or her medication. The resulting questionnaire is available from the authors. It may be noted that although this questionnaire was specifically designed to assess aspects of the Park and Jones (1997) model, some questions were similar to those used in other questionnaires designed to assess the relation of medication beliefs and adherence (Horne, Weinman & Hankins, 1999).
Additional data were collected to assess patient characteristics, the third portion of the Park and Jones (1997) model. Patient cognitive status was assessed through scores on the Mini-mental Status Exam (MMSE) and patient mood was assessed through administration of the Hamilton Depression Rating Scale (HAM-D). Data on patient age, preferred language (i.e., Spanish or English), and educational attainment were obtained from patient records.
Data on patient diagnoses were grouped according to the first diagnosis listed in the patient’s medical chart. ‘Dementing illnesses’ included possible and probable Alzheimer’s disease, vascular dementia, and all other causes of dementia. ‘Psychiatric illnesses’ included diagnoses of mood and anxiety disorders, including major depression, dysthymic disorder, generalized anxiety disorder, and anxiety disorder not otherwise specified. Medications were categorized on the basis of the medication type and the purpose for which it was prescribed. Psychiatric medications included antidepressants, anxiolytics, antipsychotics, anticonvulsants prescribed for behavior problems, and medications prescribed for insomnia. Memory-related medications included cholinesterase inhibitors and memantine. General medical medications included medications prescribed for all other causes, including hypertension, dyslipidemias, diabetes mellitus, arthritis, hypothyroidism, and all similar conditions.
Data were collected in three waves by three interviewers who were psychiatrists completing specialized training in geriatric psychiatry under the supervision of a board-certified geriatric psychiatrist. Data for each wave were collected during consecutive academic years during which the psychiatrists completed fellowship training so that data were collected by different assessors over one of three years. Relations among variables in these data were thus potentially related to the individual characteristics of specific raters over the years during which data were collected. In addition, most patients reported taking more than one medication so that each patient-caregiver dyad provided ratings for a distinct group of medications. For example, a single patient might have provided ratings for a set of medications that included treatments for diabetes, hypertension, and dyslipidemias. Multiple ratings provided by patients were thus potentially intercorrelated as a result of each patient’s distinct viewpoint on his or her medications—any given patient, for example, might consistently over- or underrate the seriousness of his or her medical conditions or any other of the requested ratings.
Potential sources of variability in the data collected thus included the effects of the individual psychiatrists involved in data collection during different periods and the effects of individual patients who reported on groups of medications. Since data arose from several levels (clustered within patients and within the three samples), variables were potentially correlated within these levels. Traditional linear regression or path analysis would not take these intercorrelations into account in evaluating model parameters and thus might produce incorrect parameter estimates. These are usually incorrect estimates of parameters’ standard errors that in turn result in incorrect estimates of the statistical significance of the same parameter estimates (Singer, 1998). Relations among model variables were therefore analyzed in a multilevel path analytic model using PROC MIXED in SAS (Littell, Milliken, Stroup & Wolfinger, 1996). This approach allowed estimation of path relations among model variables and reported medication adherence while taking into account intercorrelations among variables resulting from the sample membership and from having obtained multiple rating from most patients.
It was recognized that patient and caregiver reports of adherence might differ, and further that differences might be related to the techniques patients reported they used to remember to take their medications. Differences between caregiver and patient reports of adherence were therefore evaluated across groups defined by reported techniques used to remember to take medications. A difference score was first calculated by subtracting patient report of adherence from the corresponding caregiver report, and then t-tests were used to evaluate between-group differences. Cases were weighted by the total number of medications taken by each patient to account for different number of medications reported by patients. The difference in magnitude of the patient-caregiver discrepancies for groups defined by reported mnemonic strategy was also tested via a t-test weighted for number of medications taken. In order to correct for the number of comparisons inherent in the use of several t-tests, the Bonferroni correction was used, resulting in the use of an alpha value of 0.01 (0.05 divided by the number of t-tests, five) in assessing results for statistical significance.
Since a large number of variables were thus collected, a multi-step data reduction procedure was employed in which two separate models of predictors were developed, and a final integrative model was formulated. First, a model of caregiver report of adherence was created that assessed the contributions of ratings of disease and treatment, patient, and environment variables to caregiver reports of medication adherence. Caregiver report was used as the dependent variable in these analyses since it was judged that caregiver report would more accurately reflect patients’ adherence. The hypothesized model specified that patient beliefs about disease (perceived outcome and seriousness) and treatment variables (regimen complexity as indexed by the total number of medications taken and presence of side effects) would predict caregivers’ reports of patient adherence.
A second model also assessed the relation of patient variables (age, HAM-D and MMSE scores, and education) to caregivers’ reports of adherence. The one environment variable available for analysis (medication reminder category) was also hypothesized to predict reported adherence. Finally, based on previous work, depression as measured by the HAM-D was hypothesized to predict the presence of side effects and to have a negative relation to MMSE score. Age was predicted to have an inverse relation with MMSE score, while educational attainment was predicted to have a positive relation to MMSE score.
The first multilevel regression analysis thus assessed the relation of disease representation variables to adherence, while the second evaluated the patient characteristic variables in combination with the single environment variable (memory strategy). Variables that predicted adherence at a statistical significance of p<0.10 in each of these analyses were retained for inclusion in a third overall model. Model-based predictions of the relations among HAM-D, age, and MMSE scores were evaluated in separate analyses.
This study and subsequent data analyses were carried out under protocols approved by the Mt. Sinai Medical Center Institutional Review Board and the University of Miami Human Subjects Review Office.
Results
Descriptive data for the sample are presented in Tables I and II. It may be noted that the percentages reported in Table I for type of medication represent the percent of total medications rather than the percent of patients receiving a medication. Results of comparisons of differences between patient and caregiver reports of adherence compared for groups defined by method of remembering to take medications are reported in Table III. These results show that the discrepancy between patient and caregiver reports was greatest for the group of patients who reported relying on themselves or their daily routine to remember to take their medications. The difference was smaller, although still statistically significant, for the group that reported relying on a caregiver or spouse. The difference was smallest for patients who reported using a pillbox or other mechanical aid to remember to take medications. In this case, the average caregiver rating of adherence was actually higher than that reported by patients, although this difference was not statistically significant. The interpretation of this difference is limited by the small number of patients who reported using a pillbox or other device. The test for the size of the discrepancy between patient and caregiver reports for groups relying on themselves and on caregivers was also statistically significant. The size of the patient-caregiver reporting discrepancy was thus significantly larger in the group that relied on themselves to take their medication.
Table I.
Sample characteristics for categorical variables.
| Characteristic | Number | Percentage |
|---|---|---|
| Language/cultural background | ||
| Hispanic | 28 | 44.4 |
| Anglo | 35 | 55.6 |
| Gender | ||
| Male | 18 | 28.6 |
| Female | 45 | 71.4 |
| Memory strategy used | ||
| Self/routine | 89 | 34.5 |
| Caregiver/spouse | 129 | 54.9 |
| Pillbox/other aid | 11 | 4.7 |
| Presence of side effects | ||
| Yes | 24 | 10.2 |
| No | 211 | 89.8 |
| Sample | ||
| 1 | 26 | 41.3 |
| 2 | 21 | 33.3 |
| 3 | 16 | 25.4 |
| Medication category | ||
| Psychiatric | 81 | 34.5 |
| Memory-related | 38 | 16.2 |
| General medical | 116 | 49.4 |
| Primary diagnosis | ||
| Dementing illness | 49 | 77.8 |
| Psychiatric illness | 14 | 22.2 |
Table II.
Descriptive statistics for continuous study variables.
| Variable | Mean | SD | Range |
|---|---|---|---|
| Age | 76.3 | 7.9 | 34 |
| Educational level (years) | 11.5 | 3.8 | 16 |
| HAM-D | 8.3 | 6.0 | 28 |
| MMSE | 19.8 | 8.0 | 30 |
| Total number of medications taken | 3.7 | 1.5 | 6 |
Table III.
Comparisons of patient and caregiver report of adherence.
| Mean (SD) for caregivers |
Mean (SD) for patients |
n b | t | df | p | |
|---|---|---|---|---|---|---|
| Groupsa | ||||||
| Self or daily routine | 3.4 (4.0) | 4.3 (2.4) | 90 | 4.00 | 89 | <0.001 |
| Caregiver or spouse | 4.1 (3.3) | 4.5 (2.2) | 131 | 2.47 | 120 | 0.02 |
| Pillbox or other mechanical aid | 4.5 (1.2) | 4.2 (2.1) | 13 | 1.60 | 12 | 0.14 |
|
| ||||||
| Tests of differences between patient and caregiver reports of adherence for groups defined by use of mnemonic strategy | ||||||
| Mean (SD) Difference for Self-reliant Group |
Mean (SD) Difference for Caregiver Group |
Mean (SD) Difference for Mechanical Aid Group |
t | df | p | |
|
| ||||||
| Difference between self reliant and caregiver groupsc |
−0.10 (1.33) | −0.37 (1.81) | 4.80 | 219 | <0.001 | |
| Difference between caregiver and pillbox or mechanical aid groupsd |
−0.37 (1.81) | 0.38 (0.87) | −1.30 | 141 | 0.20 | |
Defined by mnemonic strategy. In self or daily routine group, patients reported, for example, that they relied of their own memory or their daily routine to remember to take their medication.
Number of reports for each mnemonic strategy. Since patients reported on different numbers of medications, these numbers are greater than the total number of patients. T-tests were weighted to take into account different numbers of reports from various patients.
Between-group test of the magnitude of discrepancies between patient and caregiver reports for groups defined by reliance on self or caregiver to remember to take medication.
Between-group test of the magnitude of discrepancies between patient and caregiver reports for groups defined by reliance on caregiver or a pillbox or other mechanical aid to remember to take medication.
Results of the multilevel regression analysis of the disease representation model are presented in Table IV. Of the four disease representation variables, ratings of likely outcome without treatment and the presence of side effects were related to reported adherence. The analysis for patient characteristic variables is also reported in Table IV. Of this group of variables, age and memory strategy were related to adherence. Outcome (patients’ estimate of likely outcome if the medication were not to be taken) is included in this analysis because in preliminary analyses it was found to have a significant moderating effect on estimates of the relation between patient characteristic variables and caregiver estimates of medication adherence. As these analyses showed that outcome would be included in the final multilevel analysis and that it had a significant effect on other variables in the model, it was included in analyses of patient characteristic variables. Table V presents results of analyses of relations among depression, side effects, and cognitive status. Of the predicted relations, only the inverse relation between age and MMSE score was significant.
Table IV.
Multilevel regression analyses.
| Variable | Estimate | Standard error | t value | P |
|---|---|---|---|---|
| Disease representation model | ||||
| Intercept | 0.05 | 0.20 | 0.26 | 0.82 |
| Outcome | 0.28 | 0.08 | 3.37 | <0.001 |
| Seriousness | 0.03 | 0.09 | 0.33 | 0.74 |
| Total number of medications | 0.05 | 0.08 | 0.60 | 0.55 |
| Presence of side effects | −0.21 | 0.05 | −4.15 | <0.001 |
| Patient characteristics model | ||||
| Intercept | 0.25 | 0.25 | 0.98 | 0.43 |
| Outcome | 0.32 | 0.09 | 3.68 | <0.001 |
| Language | 0.09 | 0.05 | 1.68 | 0.09 |
| HAM-D | 0.09 | 0.05 | 1.78 | 0.08 |
| MMSE | 0.02 | 0.06 | 0.24 | 0.81 |
| Education | 0.12 | 0.05 | 2.23 | 0.03 |
| Gender | −0.02 | 0.12 | −0.14 | 0.89 |
| Age | 0.15 | 0.05 | 3.08 | 0.002 |
| Memory strategy: rely on self | −0.44 | 0.13 | −3.32 | <0.001 |
Table V.
Multilevel regression analyses for additional variables.
| Variable | Estimate | Standard error | t value | p |
|---|---|---|---|---|
| Model Predicting Side Effects | ||||
| Intercept | 0.01 | 0.07 | 0.16 | 0.88 |
| HAM-D | −0.11 | 0.07 | −1.51 | 0.13 |
| Model Predicting Cognitive Status (MMSE) | ||||
| Intercept | 0.01 | 0.21 | 0.03 | 0.98 |
| Age | −0.12 | 0.06 | −2.09 | 0.04 |
| HAM-D | −0.09 | 0.06 | −1.45 | 0.15 |
| Education | 0.004 | 0.06 | 0.07 | 0.95 |
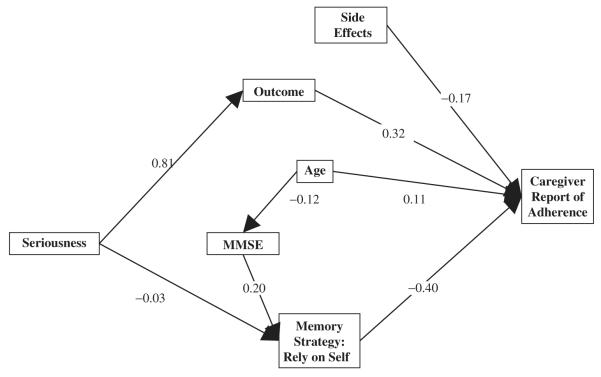
Follow-up analyses in this exploratory study investigated the relations of ratings of disease seriousness to other variables in the model. Ratings of condition seriousness were related to perceived outcome and reliance on self as a memory strategy but not directly to reported adherence. After the initial evaluations, we recomputed the model including only the significant coefficients from earlier models. This reduced model is presented as a path diagram in the Figure 1. The figure also illustrates results of the investigation of the relation of ratings of condition seriousness to other variables. Patients’ ratings of the seriousness of their condition did not directly predict adherence, but predicted perceived outcome without treatment and were inversely related to reliance on self as memory strategy.
Figure 1.
Final multilevel path model. Numbers on lines are the standardized regression coefficients for the relation between variables.
In summary, perceived outcome and patient age were positively related to reported adherence, while the occurrence of side effects and reliance on self to remember were negatively related to adherence. Age was inversely related to cognitive status as measured by the MMSE but positively related to adherence. Scores on the MMSE in turn predicted reliance on one’s self to remember to take medications. Perceived seriousness of the condition for which the medication was taken was positively related to perceived outcome, and negatively related to the use of one’s self to remember to take medications.
Discussion
Results of this study thus partially confirm the notion that multiple influences affect medication adherence in older adults who are patients at a memory disorders clinic. Consistent with the contention implicit in the Park and Jones (1997) model, patients’ perceptions of their illness, the treatment they receive, their personal characteristics, and their use of memory strategies may be related to adherence. Patients’ beliefs about the how serious a medical condition were related to their understanding of the likely outcome of the condition without treatment. This understanding was in turn related to adherence. Motivational factors may thus play an important role in adherence in this population. Consistent with the model’s prediction, relying on a caregiver improved medication adherence.
It is noteworthy that increasing age was positively related to adherence. This is contrary to the stereotype that older individuals are less likely to be adherent, but consistent with finding reported by Park et al. (1999) in a study of adherence in patients with rheumatoid arthritis. In that study, older patients had higher levels of adherence when compared with younger patients, who reported being busy and having erratic schedules that interfered with remembering to take their medications. It may thus not be age by itself that has a negative impact on adherence, but rather other variables that include patients’ understanding and motivation as well as their cognitive and memory status. An alternative explanation might be that older adults who have mild to moderate cognitive impairment may have sufficient insight into the potential implications of not taking their medication to give them greater motivation to adhere to prescribed medication regimes. Perhaps as these patients age they become more aware of the impact of medications on their health status and are more strongly motivated to adhere to their medications. This finding thus highlights the complex nature of medication adherence in older adults and the elderly and suggests further needs for research. If these hypotheses are supported in future research, they might provide bases for designing new and more effective interventions to improve elders’ medication adherence.
Several predicted relations were not found. Contrary to expectations, regimen complexity as indexed by the total number of medications was not related to adherence. Depressed mood did not have a negative relation with general cognitive status, and education did not have a positive relation with it. These results may be the result of a small sample with limited power to detect these relations, and clarification of this issue will require a larger study.
The total number of medications per patient found in this study (3.7) is somewhat lower than that found in several other studies (van Dijk et al., 1998; Williams, Nichol, Yoon, McCombs & Margolies, 1999; Golden et al., 1998). For example, Golden et al. (1998) found that the average number of medications per person in a large sample of homebound elderly was 5.3, with a standard deviation of 2.9. These estimates are drawn from populations of persons who may have been more ill than the patients in the present study. It may be noted as well that in the study by Golden et al. (1998) there was substantial variability in number of medications, so that our current results are within the range that might be expected. Finally, since these data are based on self reports from patients and caregivers, it is possible that they failed to report all medications.
Since both patients and their caregivers or spouses reported estimates of the patients’ adherence to their medications, it was possible to examine differences between patient and caregiver reports of adherence. This was especially useful in light of the different mnemonic strategies used by patients. Under the assumption that caregivers’ reports were more likely to be accurate than patients’ it was thus possible to compare the two sets of reports in the context of reported mnemonic strategy. Results showed a larger discrepancy between patient and caregiver report of adherence for the group of patients who stated that they relied on themselves or their daily routine when compared to those who relied on caregivers’ reminders. This finding suggested that the size of the differences might be larger in the group that reported relying on themselves than in the group who relied on caregivers. This was true, as the size of the differences in the two groups was significantly different between two groups. This thus may imply that patient reports of adherence are less likely to be accurate than are the reports of their caregivers.
Several limitations of this study should be acknowledged. Reliance on caregiver report of medication adherence is potentially inaccurate. Other studies have shown that self-report measures of medication adherence consistently overestimate level of adherence, so that this reliance is a potential source of inaccuracy. Other, more accurate, measures of medication adherence such as electronic monitoring of medication use are available but were not used in this study due to its limited scope.
A second limitation of this study is the nature of the sample used. Patients were selected for evaluation in the study on the basis of their availability. Since patient selection was not random, it is difficult to assess the effects of potential selection biases on results. Patients in this study had been referred for psychiatric evaluation and treatment, so that the sample was less likely to include patients with memory problems but without concomitant or primary psychiatric diagnoses. Not all patients were judged to have a primary diagnosis of dementia, so that the sample was heterogeneous. Although from one perspective a limitation, this heterogeneity may more accurately reflect the general population served by a memory disorder clinic.
It should be noted that this sample included patients who were initially seen for evaluation of memory problems, although as a result of this evaluation some were judged to have primary psychiatric diagnoses and were therefore treated for psychiatric problems such as depression and agitation as well as memory problems. Sample size in this study is another issue. Given the exploratory nature of this study, a small sample was judged acceptable, but as noted above the path analytic model employed in data analysis may have had limited power to detect predicted relations among study variables.
This study thus suggests that Park and Jones’ (1997) central contention in creating their model may be correct in that information from several domains may be related to medication adherence in the elderly. This study shows that patient beliefs, treatment characteristics, patient characteristics, and memory strategies all may contribute to adherence. Results thus support the usefulness of this approach for understanding the complex behavior of taking specific medications in specific ways. Implications of these findings are that interventions that target patient beliefs about their medication and that minimize the occurrence of side effects may be useful in improving medication adherence.
References
- Applegate WB. Elderly patients’ adherence to statin therapy. Journal of the American Medical Association. 2002;288:495–497. doi: 10.1001/jama.288.4.495. [DOI] [PubMed] [Google Scholar]
- Barr RG, Somers SC, Speizer FE, Camargo CA., Jr. Patient factors and medication guideline adherence among older women with asthma. Archives of Internal Medicine. 2002;162:1761–1768. doi: 10.1001/archinte.162.15.1761. [DOI] [PubMed] [Google Scholar]
- Bobb-Liverpool B, Duff EM, Bailey EY. Compliance and blood pressure control in women with hypertension. West Indian Medical Journal. 2002;51:236–240. [PubMed] [Google Scholar]
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: Meta-analysis of the effects of anxiety and depression on patient adherence. Archives of Internal Medicine. 2000;160:2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- Dunbar-Jacob J, Schlenk E. Patient adherence to treatment regimen. In: Baum A, Revenson TA, Singer JE, editors. Handbook of health psychology. Lawrence Erlbaum; Mahwah, NJ: 2001. pp. 371–380. [Google Scholar]
- Evangelista L, Doering LV, Dracup K, Westlake C, Hamilton M, Fonarow GC. Compliance behaviors of elderly patients with advanced heart failure. Journal of Cardiovascular Nursing. 2003;18:197–206. doi: 10.1097/00005082-200307000-00005. [DOI] [PubMed] [Google Scholar]
- Ganguli M, Rodriguez E, Mulsant B, Richards S, Pandav R, Bilt JV, et al. Detection and management of cognitive impairment in primary care: The Steel Valley Seniors Survey. Journal of the American Geriatrics Society. 2004;52:1688–1675. doi: 10.1111/j.1532-5415.2004.52459.x. [DOI] [PubMed] [Google Scholar]
- Golden AG, Preston RA, Barnett SD, Llorente M, Hamdan K, Silverman MA. Inappropriate medication prescribing in homebound older adults. Journal of the American Geriatrics Society. 1998;48:948–953. doi: 10.1111/j.1532-5415.1999.tb01289.x. [DOI] [PubMed] [Google Scholar]
- Gould ON. Cognition and affect in medication adherence. In: Park DC, Morrell RW, Shifren K, editors. Processing of medical information in aging patients. Lawrence Erlbaum; Mahwah, NJ: 1999. pp. 167–183. [Google Scholar]
- Gurwitz JH, Field TS, Harrold LR. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. Journal of the American Medical Association. 2003;289:1107–1116. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- Horne R, Weinman J, Hankins JM. The Beliefs About Medicines Questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medication. Psychology and Health. 1999;14:1–24. [Google Scholar]
- Janz NK, Becker MH. The health belief model: A decade later. Health Education Monographs. 1984;2:409–419. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS. To err is human: Building a safer health system. National Academies Press; Washington, DC: 2000. [PubMed] [Google Scholar]
- Leventhal EA, Leventhal H, Robitaille C, Brownlee S. Psychosocial factors in medication adherence: A model of the modeler. In: Park DC, Morrell RW, Shifren K, editors. Processing of medical information in aging patients. Lawrence Erlbaum; Mahway, NJ: 1999. pp. 145–165. [Google Scholar]
- Littell RC, Milliken GA, Stroup WW, Wolfinger RD. SAS system for mixed models. SAS Institute, Inc.; Cary, NC: 1996. [Google Scholar]
- McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions. Journal of the American Medical Association. 2002;288:2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- Park DC, Hertzog C, Leventhal H, Morrell RW, Leventhal E, Birchmore D, et al. Medication adherence in rheumatoid arthritis patients: Older is wiser. Journal of the American Geriatrics Society. 1999;47:172–183. doi: 10.1111/j.1532-5415.1999.tb04575.x. [DOI] [PubMed] [Google Scholar]
- Park DC, Jones TR. Medication adherence and aging. In: Fisk AD, Rogers WA, editors. Handbook of human factors and the older adult. Academic Press; New York: 1997. pp. 257–287. [Google Scholar]
- Park DC, Morrell RW, Frieske D, Kincaid D. Medication adherence behaviors in older adults: Effects of external cognitive supports. Psychology and Aging. 1992;7:252–256. doi: 10.1037//0882-7974.7.2.252. [DOI] [PubMed] [Google Scholar]
- Salas M, In’t Veld BA, van der Linden PD, Hofman A, Breteler M, Stricker BH. Impaired cognitive function and compliance with antihypertensive drugs in elderly: The Rotterdam Study. Clinical Pharmacology and Therapeutics. 2001;70:561–566. doi: 10.1067/mcp.2001.119812. [DOI] [PubMed] [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;24:323–355. [Google Scholar]
- Dijk KN, de Vries CS, van den Berg PB, Dijkema AM, Brouwers JRBJ, de Jong-van den Berg LTW. Constipation as an adverse effect of drug use in nursing home patients: An overestimated risk. British Journal of Clinical Pharmacology. 1998;46:255–261. doi: 10.1046/j.1365-2125.1998.00777.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams BR, Nichol MB, Yoon YS, McCombs JS, Margolies J. Medication use in residential care facilities for the elderly. The Annals of Pharmacotherapy. 1999;33:149–155. doi: 10.1345/aph.17424. [DOI] [PubMed] [Google Scholar]