Abstract
Context
Because Tai Chi (TC) is beneficial to elders without cognitive impairment (CI), it also may benefit elders with CI. But elders with CI have generally been excluded from TC studies because many measurement tools require verbal reports and some elders with CI are unable to provide.
Objectives
To tested the efficacy of a TC program in improving pain and other health outcomes in community-dwelling elders with knee osteoarthritis (OA) and CI.
Methods
This pilot cluster-randomized trial was conducted between January 2008 and June 2010 (ClinicalTrials.gov Identifier: NCT01528566). The TC group attended Sun style TC classes, three sessions a week for 20 weeks; the control group attended classes providing health and cultural information for the same length of time. Measures included the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain, physical function and stiffness subscales, the Get Up and Go test, the Sit-to-Stand test and the Mini-Mental State Examination (MMSE), administered at baseline, every four weeks during the intervention and at the end of the study (post-test).
Results
Eight sites participated in either the TC group (four sites, 28 participants) or the control group (four sites, 27 participants). The WOMAC pain (P=0.006) and stiffness scores (P=0.010) differed significantly between the two groups at post-test, whereas differences between the two groups in the WOMAC physical function score (P=0.071) and the MMSE (P=0.096) showed borderline significance at the post-test. WOMAC pain (P=0.001), physical function (P=0.021) and stiffness (P≤0.001) scores improved significantly more over time in the TC group than in controls. No adverse events were found in either group.
Conclusion
Practicing TC can be efficacious in reducing pain and stiffness in elders with knee OA and CI.
Keywords: Tai Chi, osteoarthritis, knee, pain, physical function, cognitive function
Introduction
Osteoarthritis (OA) affects 27 million people in the U.S. (1) and costs $185.5 billion a year (2). About 12.1% of those age 60 and older have symptomatic knee OA, and up to 37% have radiographic knee OA (1). The prevalence of symptomatic knee OA among those aged 70 and over has doubled in women and tripled in men over the past 20 years (3). Chronic knee pain is a major characteristic of knee OA. Currently, there is no cure for knee OA pain, only pharmacological interventions for alleviating pain and inflammation. However, fewer than 40% of chronic pain sufferers, including those with knee OA, obtain satisfactory pain relief from medications (4). Without proper treatment, elders with OA knee pain experience difficulty in performing activities of daily living (ADLs), and limiting ADLs results in further loss of muscle strength, range of motion, and mobility, leading to physical deconditioning and increased pain (5).
Elders with both knee OA and cognitive impairment (CI) face a double jeopardy in regard to functioning. Because proper functioning requires proper cognitive capacity, functioning declines more rapidly in elders with CI than in elders without CI (6-8). Knee OA further limits functioning in elders with CI (9). Thus, effective interventions to reduce knee OA pain and improve other health outcomes in elders with CI are greatly needed. Given the high prevalence of knee OA in elders and the inadequacy of medication in treating their pain, the use of nonpharmacological adjunct interventions should be considered to reduce pain and improve functioning.
Tai Chi (TC) is a gentle aerobic exercise derived from ancient Chinese martial arts (10). Many studies have shown beneficial effects of TC on knee OA pain (11-15) and cognitive and physical function in elders without CI (11, 13-20). Because TC is beneficial to elders without CI, it also may benefit elders with CI. Yet elders with CI have generally been excluded from TC studies because many measurement tools require verbal reports and some elders with CI are unable to provide these (16, 21, 22). However, if elders with CI are not included in trials, we cannot know whether TC is beneficial to them. We also cannot know how to prescribe the dosing of TC, such as numbers of sessions per week, and numbers of weeks of intervention needed to relieve their pain and improve their functioning. Our previous feasibility studies indicated that TC might relieve knee OA pain and improve functioning in elders with CI (23, 24). Building on those studies, the pilot cluster-randomized trial reported here was designed to test the efficacy of a TC program in improving pain and other health outcomes in community-dwelling elders with CI and knee OA.
Methods
Study Design
This 20-week cluster-randomized clinical trial had two arms, a TC group and an attention control group. Cluster randomization was carried out by the statistician after screening was completed at each site. A random number table was used to randomly assign each site to the TC or attention control arm (four sites each) according to the sequence of even/odd numbers from a random starting point in the table. The assessor was not involved in the intervention and the interventionists were not involved in the outcome assessment.
Participants
Inclusion criteria for the study were 1) age ≥ 60 years; 2) moderate, mild or subtle CI, defined as a Mini-Mental State Examination (MMSE) score of 18-28; 3) a diagnosis of knee OA based on medical history reviewed with elders or family members/staff and confirmed by a health care provider; 4) self-report of knee OA pain ≥ 2 on the Verbal Descriptor Scale (VDS), or a pain score ≥ 3 on the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale; 5) ability to speak English; 6) physician's/nurse practitioner's permission to participate; 7) no participation in a regular exercise program in the past month; 8) ambulation without assistance from staff or a walking device for 50 meters; and 9) ability to stand and maintain balance for one minute without a walking device. We included elders with moderate, mild or subtle CI, with or without dementia, i.e., MMSE scores of 18 or above, because studies have found that these elders are able to provide valid answers to inquiries about their pain (25, 26) and could learn TC. Although published studies have tended to use 27/28 as the cutoff MMSE score for normal cognition, recent studies have shown that some elders with MMSE = 28 may have pre-symptom or subtle CI (27). Thus, we included elders with MMSE scores up to 28.
Exclusion criteria were 1) uncorrectable moderate or severe hearing or vision deficits; 2) Parkinson's disease; 3) cancer pain; 4) chronic pain conditions, such as rheumatoid arthritis, fibromyalgia, or severe low back pain; 5) diabetic neuropathy; 6) arthroscopic surgery or total knee- or hip-replacement surgery in the past six months; 7) fractures in the past six months; 8) major psychiatric disorder or positive screen for depressive symptoms (Geriatric Depression Scale-15 score ≥ 5) without taking medication; 9) history of falls in the past three months; or 10) vertigo in the past month. The same study criteria were applied to the TC and the attention control groups.
Power Analysis
We intended to compare change in scores on pain measures between pre- and post-test in the TC and attention control groups. Based on a previous small pilot study (24), a sample size of 40 per group (80 total) was expected to provide 80% power to detect an effect size of 0.8 using a two-sided t-test with alpha=0.05, based on the assumption that the intracluster correlation (ICC) was 0.01 (28). No replacements for dropouts were considered. Instead of 80 participants, we were only able to recruit 55 participants over three years for the study.
As shown in Table 2, the ICC for the primary outcome, WOMAC pain, was 0.005 and ICCs for secondary outcomes were between 0.024 and 0.241. Based on these data, we had sufficient power to detect a large effect size for the outcomes of WOMAC pain and stiffness (0.90 and 1.21, respectively, at Week 21). However, with 55 participants, we only had a power of 65% to detect an effect size of 0.71 for WOMAC physical function at Week 21. Power to detect the effect sizes of other outcomes was below 50%.
Table 2.
Changes in Outcomes, Controlling for Site Effect
| Within Group Difference |
Between Group Difference |
Trendd |
ICC |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tai Chi (n=28) | Control (n=27) | |||||||||
| Outcome | Estimatesb | 95% confidence interval | Estimatesb | 95% confidence interval | Estimatesc | 95% confidence interval | P | P | r | |
| WOMAC Paina | 0.001 | 0.005 | ||||||||
| Week 1 | -0.70 | (-2.31, 0.92) | 0.395 | |||||||
| Week 5 | -1.11 | (-2.09, -0.12) | -0.86 | (-1.53, -0.20) | -0.94 | (-2.56, 0.67) | 0.252 | |||
| Week 9 | -1.90 | (-2.88, -0.91) | -0.76 | (-1.43, -0.09) | -1.84 | (-3.45, -0.22) | 0.026 | |||
| Week 13 | -2.30 | (-3.29, -1.32) | -0.79 | (-1.46, -0.12) | -2.21 | (-3.83, -0.60) | 0.007 | |||
| Week 17 | -2.49 | (-3.48, -1.51) | -0.93 | (-1.60, -0.26) | -2.27 | (-3.88, -0.65) | 0.006 | |||
| Week 21 | -2.60 | (-3.59, -1.62) | -1.02 | (-1.69, -0.36) | -2.28 | (-3.89, -0.66) | 0.006 | |||
| WOMAC Physicala | 0.021 | 0.061 | ||||||||
| Week 1 | -0.45 | (-6.94, 6.04) | 0.891 | |||||||
| Week 5 | -3.07 | (-6.51, 0.36) | -0.41 | (-2.80, 1.98) | -3.12 | (-9.60, 3.37) | 0.345 | |||
| Week 9 | -5.32 | (-8.76, -1.89) | 0.22 | (-2.17, 2.61) | -6.00 | (-12.48, 0.49) | 0.070 | |||
| Week 13 | -5.57 | (-9.01, -2.14) | -0.19 | (-2.58, 2.20) | -5.84 | (-12.33, 0.65) | 0.078 | |||
| Week 17 | -5.96 | (-9.40, -2.53) | -1.78 | (-4.17, 0.61) | -4.64 | (-11.13, 1.85) | 0.160 | |||
| Week 21 | -6.82 | (-10.26, -3.39) | -1.30 | (-3.69, 1.09) | -5.98 | (-12.47, 0.51) | 0.071 | |||
| WOMAC Stiffnessa | ≤0.001 | 0.089 | ||||||||
| Week 1 | 0.26 | (-0.72, 1.24) | 0.601 | |||||||
| Week 5 | -0.61 | (-1.13, -0.08) | -0.22 | (-0.67, 0.22) | -0.12 | (-1.11, 0.86) | 0.804 | |||
| Week 9 | -1.07 | (-1.60, -0.54) | -0.11 | (-0.56, 0.34) | -0.70 | (-1.68, 0.28) | 0.162 | |||
| Week 13 | -1.25 | (-1.78, -0.72) | -0.19 | (-0.63, 0.26) | -0.80 | (-1.79, 0.18) | 0.108 | |||
| Week 17 | -1.82 | (-2.35, -1.29) | -0.52 | (-0.97, -0.07) | -1.04 | (-2.02, -0.06) | 0.038 | |||
| Week 21 | -1.79 | (-2.31, -1.26) | -0.22 | (-0.67, 0.22) | -1.30 | (-2.28, -0.32) | 0.010 | |||
| GUGa | 0.776 | 0.112 | ||||||||
| Week 1 | -2.34 | (-6.82, 2.13) | 0.304 | |||||||
| Week 5 | -1.41 | (-2.10, -0.72) | -0.41 | (-1.42 0.60) | -3.34 | (-7.82, 1.13) | 0.143 | |||
| Week 9 | -1.64 | (-2.33, -0.95) | -0.10 | (-1.11, 0.91) | -3.88 | (-8.36, 0.59) | 0.089 | |||
| Week 13 | -1.34 | (-2.03, -0.65) | -1.30 | (-2.31, -0.29) | -2.38 | (-6.86, 2.09) | 0.296 | |||
| Week 17 | -1.62 | (-2.30, -0.93) | -0.94 | (-1.95, 0.07) | -3.02 | (-7.49, 1.46) | 0.186 | |||
| Week 21 | -1.41 | (-2.09, -0.72) | -0.26 | (-1.26, 0.75) | -3.49 | (-7.97, 0.99) | 0.126 | |||
| STSa | 0.238 | 0.241 | ||||||||
| Week 1 | 0.20 | (-5.31, 5.70) | 0.944 | |||||||
| Week 5 | -1.46 | (-2.48, -0.44) | -0.65 | (-1.79, 0.49) | -0.62 | (-6.12, 4.89) | 0.825 | |||
| Week 9 | -2.18 | (-3.20, -1.16) | -0.80 | (-1.94, 0.34) | -1.17 | (-6.68, 4.33) | 0.675 | |||
| Week 13 | -2.00 | (-3.02, -0.97) | -1.46 | (-2.60, -0.32) | -0.34 | (-5.85, 5.17) | 0.903 | |||
| Week 17 | -2.31 | (-3.33, -1.29) | -1.15 | (-2.29, -0.01) | -0.96 | (-6.47, 4.54) | 0.731 | |||
| Week 21 | -2.18 | (-3.20, -1.16) | -1.01 | (-2.15, 0.13) | -0.98 | (-6.48, 4.53) | 0.728 | |||
| MMSE | 0.223 | 0.024 | ||||||||
| Week 1 | 1.11 | (-0.46, 2.68) | 0.165 | |||||||
| Week 5 | 0.86 | (0.17, 1.54) | 0.22 | (-0.52, 0.96) | 1.75 | (0.17, 3.32) | 0.030 | |||
| Week 9 | 1.29 | (0.60, 1.97) | 1.00 | (0.26, 1.74) | 1.40 | (-0.17, 2.97) | 0.081 | |||
| Week 13 | 0.86 | (0.17, 1.54) | 0.30 | (-0.44, 1.03) | 1.67 | (0.10, 3.24) | 0.037 | |||
| Week 17 | 1.29 | (0.60, 1.97) | 0.56 | (-0.18, 1.29) | 1.84 | (0.27, 3.41) | 0.022 | |||
| Week 21 | 1.00 | (0.32, 1.68) | 0.78 | (0.04, 1.52) | 1.33 | (-0.24, 2.90) | 0.096 | |||
ICC = intracluster correlation.
Lower scores indicate improvement.
Mean difference between each follow-up time point and baseline based on model estimation, controlling for site effect.
Mean difference between Tai Chi and control groups at each time point based on model estimation, controlling for site effect.
Test linearly increasing trend on group difference over time by linear contrast.
Intervention
TC Intervention
The 12-form Sun TC for arthritis (29) was adapted for elders with knee OA and CI based on our previous pilot work (23, 24, 30). The TC group received three sessions a week of TC exercise for 20 weeks. TC exercise started at 20 minutes per session and gradually increased to 40 minutes per session, as described in our previous report (31). A standardized treatment manual was developed to ensure that the TC forms were taught consistently.
The TC intervention was led by a senior certified TC instructor who had six years’ experience in teaching Sun TC for arthritis. Two other certified TC instructors (with three or more years’ experience in teaching TC) assisted in teaching at various times during the three-year study period. All instructors were certified by the same organization under the same Master Instructor (32). Individual instructors’ performance of TC forms, which are TC movements that work together in a continuous motion, was taped and analyzed. When any deviation in TC instruction was observed, the senior TC instructor practiced with the individual instructor to ensure the consistency of the forms and teaching methods based on the treatment manual. Details of the method for conducting a TC class have been published previously (31).
Attention Control Intervention
The attention control group participated in health education, culture-related activities and other social activities (e.g., sharing travel experiences, hobbies and collections) for a total of 20 weeks. The attention control protocol implemented at each study site was standardized in terms of content, materials and duration. The length and frequency of the activities for this group closely matched those in the TC group. The senior TC instructor, a medical school faculty member, discussed various health-related topics (e.g., Alzheimer's disease, Parkinson's disease, macular degeneration) and led various culture-related activities (e.g., Chinese painting, cooking and writing) in this group. Two other instructors were trained by the senior TC instructor to conduct other related activities. The senior TC instructor routinely visited the sites to monitor the fidelity of the instructors in teaching method, materials used and duration of activities. Any deviations from the protocol were discussed and corrected as appropriate.
Outcome Variables
Outcomes were measured at Week 1 (pre-test), Week 5, Week 9, Week 13, Week 17 and Week 21 (post-test). The WOMAC was used to measure subjective pain, physical functioning, and stiffness (33). A modified Get Up and Go (GUG) test was used to measure the elder's speed in getting up from an armchair, walking as fast as he or she could for 50 feet, returning to the chair, and sitting down (34, 35). The Sit-to-Stand (STS) test was modified for our elderly participants by asking participants, with arms across the chest, to rise five times from a chair as fast as possible (36). Cognitive functioning was measured by the MMSE (37).
Statistical Analyses
Intent-to-treat analysis was used for outcome variables. Bivariate statistics (t-tests and Chi-square) and general linear mixed models were used to analyze the data. To account for the cluster randomization, the random effects of sites and the random intercept of subject effects within a site were included in the mixed models. We analyzed changes in outcome variables within groups and the differences in outcome variables between groups. For within-group comparisons, change in outcome variables between baseline and each follow-up time point for participants in the TC group and control group were estimated from the mixed models, stratified by groups. For between-group comparisons, at each time point, the difference in outcome variables between the TC and control groups were estimated from the mixed model with the interaction between group and time. We further tested whether the differences between groups increased over time by building the linear contrast for trends in the mixed model. We report a 95% confidence interval for within-group comparisons and a 95% confidence interval and significance level for the difference and trend tests for between-group comparisons.
Results
Descriptive Results
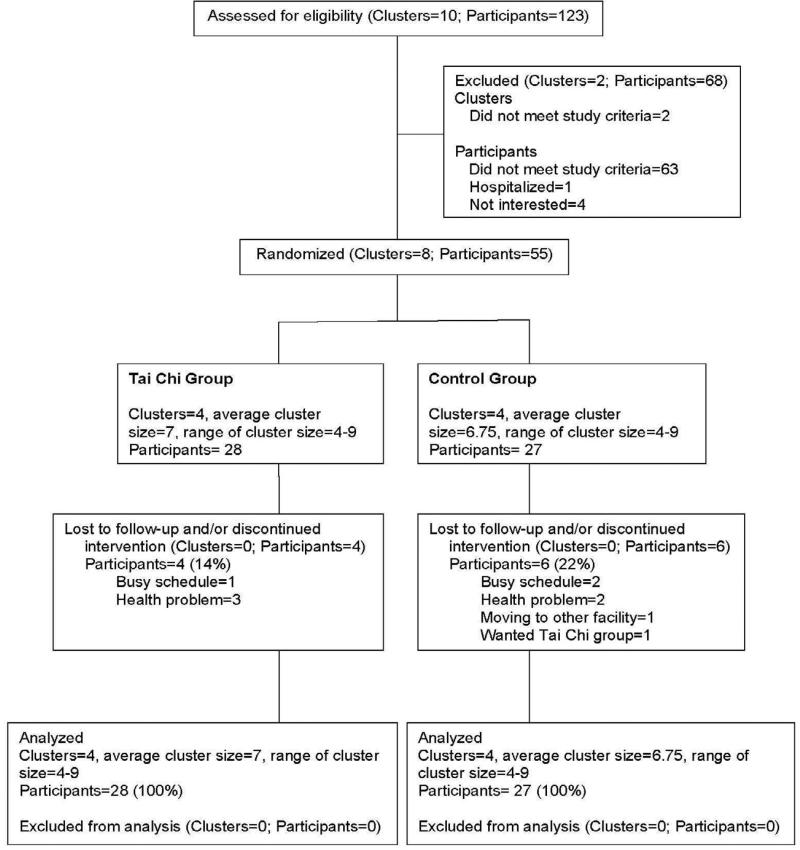
This study was conducted between January 2008 and June 2010. We approached 354 elders and screened 123. Among them, 60 were eligible (Fig. 1). Major reasons for exclusion were too high or too low MMSE scores (n=26); no knee OA (n=27); no or very mild knee pain (VDS <2 and WOMAC pain <3, n=12); recent fall (n=11); participation in another exercise program (n=10); major psychiatric problems (n=10) and other severe chronic pain (n=7). Five eligible elders dropped out before group assignment. Their reasons included hospitalization (n=1) and reduced interest in the project (n=4). The final sample size in the eight sites was 55 participants. Four sites (n=28) were assigned to the TC group and the other four (n=27) were assigned to the activity control group (Fig. 1).
Figure 1.
CONSORT Flowchart Clusters and participants flow through treatment
Baseline characteristics and group scores on study variables are summarized in Table 1. One site in each arm was a senior center, and the other three sites were senior residential complexes. Each arm had an average of seven elders per site. The average age of the 55 participants was 78.91 years; the majority were women (72.7%) and Caucasian (92.7%). Their average MMSE score was 25.45 ± 2.36.
Table 1.
Baseline Characteristics and Group Scores on Study Variables
| Variable | Total | Tai Chi | Activity | P-value |
|---|---|---|---|---|
| Site characteristics | ||||
| Number of sites | 8 | 4 | 4 | 1.000 |
| Number of sites that were senior centers | 2 | 1 | 1 | 1.000 |
| Number of participants per site | 6.88 | 7 | 6.75 | 0.888 |
| Participant characteristics | ||||
| Number of participants | 55 | 28 | 27 | |
| Demographics | ||||
| Female | 72.7% | 78.6% | 66.7% | 0.375 |
| Caucasian | 92.7% | 92.9% | 92.6% | 1.000 |
| Age | 78.91 (7.55) | 78.89 (6.91) | 78.93 (8.30) | 0.987 |
| Education in years | 14.56 (3.03) | 14.82 (3.10) | 14.30 (2.99) | 0.525 |
| WOMAC-Pain | 7.30 (3.23) | 6.96 (3.26) | 7.65 (3.21) | 0.433 |
| WOMAC-Physical | 26.58 (10.03) | 26.43 (8.62) | 26.74 (11.47) | 0.909 |
| WOMAC-Stiffness | 3.05 (1.52) | 3.25 (1.46) | 2.85 (1.59) | 0.336 |
| GUG | 20.43 (6.76) | 19.22 (5.69) | 21.68 (7.63) | 0.179 |
| STS | 18.36 (6.82) | 18.50 (8.09) | 18.20 (5.36) | 0.873 |
| MMSE-Cognition | 25.45 (2.36) | 26.04 (1.92) | 24.85 (2.64) | 0.062 |
Brackets indicate standard deviation.
WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index; GUG= Get Up and Go Test; STS= Sit-to-Stand Test; MMSE = Mini-Mental State Examination.
There were no significant differences between study sites on any of the outcome variables at Week 1 (baseline). There also were no significant differences between groups on any of the demographics and outcome variables at Week 1. MMSE scores differed most between the two groups, although the difference was only borderline significant (P=0.062). Because a borderline difference in MMSE scores favored better cognitive function in the treatment group, we also did a set of analyses controlling for this additional variable. These analyses indicated that results were identical whether or not we controlled for MMSE (not shown). We thus report the analyses without controlling for MMSE in this paper. Dropout rates were similar between the two groups (TC 14.3% vs. control 22.2%, P=0.503). No differences in demographics and pre-intervention outcome variables were found between participants who completed the study and those who dropped out. No adverse events were found in either group.
Major Study Results
Primary Outcome (WOMAC Pain)
Both groups improved their WOMAC pain score over the 20-week intervention period (P<0.001 [TC] vs. P=0.042 [control]). However, the TC group's score was 2.28 points (95% confidence interval -3.89, -0.66; P=0.006) lower than the control group's score by Week 21 (Table 2). The difference between the two groups increased significantly over time (P=0.001, see “Trend” in Table 2). The differences started at Week 9 (P=0.026) and continued throughout the remaining intervention period (Week 13, P=0.007; Week 17, P=0.006; Week 21, P=0.006). These results suggest that it took approximately eight weeks for TC to exhibit beneficial effects on pain relief.
Secondary Outcomes
WOMAC Physical Function. There was improvement in WOMAC physical function in the TC group (P=0.001), but this was not seen in the control group (P=0.515). By Week 21, the TC group score was 5.98 points (95% confidence interval -12.47, 0.51; P=0.071) lower than the control group (Table 2). The difference between the two groups increased significantly over time (P=0.021, see “Trend” in Table 2).
WOMAC Stiffness. Only the TC group improved their WOMAC stiffness score over the 20-week intervention period (P<0.001 [TC] vs. P=0.324 [control]). The TC group score was 1.30 points (95% confidence interval -2.28, -0.32; P=0.010) lower than the control group score by Week 21. The difference between the two groups increased significantly over time (P<0.001), starting at Week 17 (P=0.038) and continuing at Week 21 (P=0.010).
GUG and STS. There were some improvements in these outcomes in the TC group (GUG: P<0.001 [TC] vs. P=0.079 [control]; STS: P<0.001 [TC] vs. P=0.193 [control]). However, the differences in these outcomes between the two groups at Week 21 were not significant (P=0.126 for GUG; P=0.728 for STS). There was no trend toward improvement over time on these two tests (P=0.776 for GUG; P=0.238 for STS).
MMSE. There was some improvement in the TC group only (P=0.003 [TC] vs. P=0.082 [control]). At Week 21, there was a difference of 1.33 points (95% confidence interval -0.24, 2.90; P=0.096) between the two groups. However, there was no significant change in the difference between the two groups over time (P=0.223).
Discussion
In this pilot study, we found that both the TC and attention control groups improved in the primary outcome, WOMAC pain score. The attention received by the elders in both groups could have moderated their pain. However, TC caused improvement above and beyond that caused by attention alone. A statistically significant difference between the two groups could be observed starting in Week 9 (i.e., after eight weeks of TC exercise) and continued to Week 21 (Table 2). Results obtained from the trend analysis (P= 0.001) clearly supported the conclusion that TC practice was better than attention. A beneficial effect of TC on OA pain also was found in Wang et al.'s study (11). Thus, the relief of pain resulting from practicing TC is not merely the result of attention, but the specific components of TC that elders practice. Although it is not clear why practicing TC can reduce OA knee pain, this finding is encouraging and should serve as the starting point to look for the mechanism(s) behind the beneficial effects of TC.
It is important to point out that Wang et al.'s study was conducted with younger participants without CI, and the duration of their intervention was 12 weeks (11). Our study results indicated that eight weeks of TC practice significantly reduced OA pain and this continued to Week 21 when the intervention period ended (Table 2). Thus, our participants, who were older and had CI, did not require more time to show improvement in pain scores. Presumably, if they continue to practice TC over time, their OA knee pain will continue to decrease. Because pain is the number one complaint among people with knee OA, the finding that TC helped to relieve knee pain in this frail population is important.
Both subjective (the self-report WOMAC physical function score) and objective (GUG, STS) measures of physical function were employed in this study. Previous randomized controlled trials (RCTs) have not been conclusive on the effects of TC on self-reported physical functioning. Wang et al. found significant positive effects of TC (11), but Lee et al. did not find any effect of TC on the WOMAC physical functioning score (12). As noted earlier, Wang et al.'s participants were younger; in addition, that study did not exclude people who regularly participated in other exercise (11). In contrast, Lee et al. had an older sample and included only elders with a sedentary life style (12). That population was similar to ours. It is possible that older, frail participants such as those in our study and Lee et al.'s study (12) require a longer time to show improvement. It is also possible that, with advanced age, improvements in physical function may never reach the level achieved by younger people. Finally, this study was powered only for the primary pain outcome and was underpowered for physical function. Nevertheless, our TC groups showed significantly greater improvement in self-reported physical function over time than the control groups (P= 0.021, Table 2). In addition, TC is joint safe and mild, demands minimum physical strength, and requires limited space to practice. It should be beneficial for elders as a regular exercise.
In addition to self-reported physical function, we included objective physical function measures. The effects of TC on objective physical function in elders with knee OA also were examined in two other RCTs (11, 12). There were mixed results for walking speed (11, 12), but positive results for the STS test (11). Other non-RCT studies on TC for knee OA found that TC had positive effects on muscle strength (13), range of motion (14, 15), gait (15), and the GUG test (14).
Our TC group did not show significantly greater improvements on the GUG and STS tests than the control group. It should be noted, however, that we used an armchair for the tests because the majority of our participants could not get up from a chair without pushing themselves up. Conducting the tests with an armchair might have decreased the sensitivity of the measures for detecting physical function and thus prevented us from identifying the effects of TC. Objective measures of physical function that are appropriate for people of advanced ages are needed. Further, this study was underpowered for detecting the effect of TC on these variables and this might have contributed to the lack of significant differences.
Our power analysis indicated that we had sufficient power to detect the effects of TC on the WOMAC stiffness score (see Methods). TC significantly improved stiffness scores starting from Week 17 and continuing to Week 21 (Table 2). Trend analysis strongly supported this conclusion (P≤ 0.001). Because TC involves continuous, slow, smooth movements of the upper and lower limbs in a particular choreographic sequence, it should improve range of motion (14, 15) and help to reduce the stiffness experienced with knee OA. However, in Wang et al.'s study (assessed in Week 12) and in Lee et al.'s study (assessed in Week 8), TC did not produce significant improvements in this measure (11, 12). It is possible that the beneficial effects of TC on stiffness could only be observed with a longer intervention, such as that employed in our study. Indeed, TC did not improve stiffness scores in Week 9 (P=0.162) or Week 13 (P= 0.108), but only at later time points (Table 2).
In our study, TC had positive effects on MMSE with a difference between groups that was borderline significant (Table 2). This finding is similar to the findings of a study that used TC as part of a multimodal intervention for improving cognition in elders with early stage CI (38). Also, our previous pilot study, using participants with lower MMSE scores than in the current study, found beneficial effects of TC on MMSE scores (23). It is possible that TC may benefit only elders with lower MMSE scores, or TC may benefit only some aspects of cognitive functioning. MMSE is a global measure that includes six aspects of cognitive functioning. When they are lumped together, we may not observe the benefit for particular aspects of cognition. Also, our power analysis indicated that we did not have sufficient power to detect effects of TC on cognition.
We found that the proportions of elders achieving a minimal clinically important difference (MCID) for improvement (39) were 60.7%, 57.1% and 67.9% in the TC group for WOMAC pain, physical function and stiffness scores, respectively. In contrast, only 40.7%, 25.9% and 33.3% of elders in the attention control group improved in these measures. Thus, even though we observed improvement in both groups, more participants in the TC group than in the control group showed practically meaningful improvements in pain, self-reported physical function and stiffness.
There were some limitations of the current study. We observed positive outcomes of TC in subjective measures only, i.e., WOMAC pain, physical and stiffness. Objective measures, such as GUG, and STS, did not show positive improvements. Interpretation of the results, therefore, requires caution. Further, we identified elders with CI using MMSE scores and identified OA of the knee using self-report with confirmation from medical providers. This might have included false-positive cases in the sample. In addition, as noted earlier, the power analysis was based on WOMAC pain only. Consequently, this study was not sufficiently powered to detect changes in some of the other outcomes. Further, we could not completely separate therapist allegiance effects from the effect of the intervention. Finally, the percentages of Caucasians and females in this pilot study were higher than those in the Arkansas or the U.S populations. This limits the generalization of the results to a broader elderly population.
Conclusion
This pilot study shows that, even in those with various levels of CI, TC can improve elders’ OA pain and stiffness over time if they practice it regularly. Even though the study was underpowered for outcomes other than pain and stiffness, our data suggest that TC may be useful in improving physical function and cognitive functioning. However, some important questions remain to be answered: 1) What strategies should be used to encourage elders to continue TC practice? 2) Is TC better than other exercises in reducing pain and stiffness and improving other health outcomes in this population? 3) Does TC save medical dollars over other exercise programs? 4) Are there other appropriate physical and cognitive functioning outcome measures for elders with CI? Further studies are necessary to answer these questions and provide more definitive data on TC's beneficial effects.
Acknowledgments
This pilot study was supported by grant R21NR010003 from the National Institute of Nursing Research, and also was supported in part by grant 1IL1RR029884 from the National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
The authors thank Elizabeth Tornquist for editorial assistance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors declare no conflicts of interest.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kotlarz H, Gunnarsson CL, Fang H, Rizzo JA. Insurer and out-of-pocket costs of osteoarthritis in the US: evidence from national survey data. Arthritis Rheum. 2009;60(12):3546–3553. doi: 10.1002/art.24984. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen US, Zhang Y, Zhu Y, et al. Increasing prevalence of knee pain and symptomatic knee osteoarthritis: survey and cohort data. Ann Intern Med. 2011;155(11):725–732. doi: 10.1059/0003-4819-155-11-201112060-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turk DC, Loeser JD, Monarch ES. Chronic pain: purposes and costs of interdisciplinary pain rehabilitation programs. Trend Evidence-Based Neuropsych. 2002;4(2):64–69. [Google Scholar]
- 5.Steultjens MP, Dekker J, Bijlsma JW. Avoidance of activity and disability in patients with osteoarthritis of the knee: the mediating role of muscle strength. Arthritis Rheum. 2002;46(7):1784–1788. doi: 10.1002/art.10383. [DOI] [PubMed] [Google Scholar]
- 6.Shah KR, Carr D, Roe CM, et al. Impaired physical performance and the assessment of dementia of the Alzheimer type. Alzheimer Dis Assoc Disord. 2004;18(3):112–119. doi: 10.1097/01.wad.0000127441.77570.f3. [DOI] [PubMed] [Google Scholar]
- 7.Dodge HH, Kadowaki T, Hayakawa T, et al. Cognitive impairment as a strong predictor of incident disability in specific ADL-IADL tasks among community-dwelling elders: the Azuchi Study. Gerontologist. 2005;45(2):222–230. doi: 10.1093/geront/45.2.222. [DOI] [PubMed] [Google Scholar]
- 8.Spiers NA, Matthews RJ, Jagger C, et al. Diseases and impairments as risk factors for onset of disability in the older population in England and Wales: findings from the Medical Research Council Cognitive Function and Ageing Study. J Gerontol A Biol Sci Med Sci. 2005;60(2):248–254. doi: 10.1093/gerona/60.2.248. [DOI] [PubMed] [Google Scholar]
- 9.Jinks C, Jordan K, Croft P. Measuring the population impact of knee pain and disability with the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Pain. 2002;100(1-2):55–64. doi: 10.1016/s0304-3959(02)00239-7. [DOI] [PubMed] [Google Scholar]
- 10.Taylor-Piliae RE. The effectiveness of Tai Chi exercise in improving aerobic capacity: an updated meta-analysis. Med Sport Sci. 2008;52:40–53. doi: 10.1159/000134283. [DOI] [PubMed] [Google Scholar]
- 11.Wang C, Schmid CH, Hibberd PL, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Rheum. 2009;61(11):1545–1553. doi: 10.1002/art.24832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HJ, Park HJ, Chae Y, et al. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: a pilot, randomized, waiting list controlled trial. Clin Rehabil. 2009;23(6):504–511. doi: 10.1177/0269215508101746. [DOI] [PubMed] [Google Scholar]
- 13.Lee HY. [Comparison of effects among Tai-Chi exercise, aquatic exercise, and a self-help program for patients with knee osteoarthritis]. [in Korean]. Taehan Kanho Hakhoe Chi. 2006;36(3):571–80. doi: 10.4040/jkan.2006.36.3.571. [DOI] [PubMed] [Google Scholar]
- 14.Lee HY, Lee KJ. [Effects of Tai Chi exercise in elderly with knee osteoarthritis]. [in Korean]. Taehan Kanho Hakhoe Chi. 2008;38(1):11–18. doi: 10.4040/jkan.2008.38.1.11. [DOI] [PubMed] [Google Scholar]
- 15.Shen CL, James CR, Chyu MC, et al. Effects of Tai Chi on gait kinematics, physical function, and pain in elderly with knee osteoarthritis--a pilot study. Am J Chin Med. 2008;36(2):219–232. doi: 10.1142/S0192415X08005734. [DOI] [PubMed] [Google Scholar]
- 16.Brismee JM, Paige RL, Chyu MC, et al. Group and home-based tai chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007 Feb;21(2):99–111. doi: 10.1177/0269215506070505. [DOI] [PubMed] [Google Scholar]
- 17.Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57(3):407–414. doi: 10.1002/art.22621. [DOI] [PubMed] [Google Scholar]
- 18.Song R, Lee EO, Lam P, Bae SC. Effects of a Sun-style Tai Chi exercise on arthritic symptoms, motivation and the performance of health behaviors in women with osteoarthritis. Taehan Kanho Hakhoe Chi. 2007;37(2):249–256. doi: 10.4040/jkan.2007.37.2.249. [DOI] [PubMed] [Google Scholar]
- 19.Matthews MM, Williams HG. Can Tai chi enhance cognitive vitality? A preliminary study of cognitive executive control in older adults after A Tai chi intervention. J S C Med Assoc. 2008;104(8):255–257. [PubMed] [Google Scholar]
- 20.Taylor-Piliae RE, Newell KA, Cherin R, et al. Effects of Tai Chi and Western exercise on physical and cognitive functioning in healthy community-dwelling older adults. J Aging Phys Act. 2010;18(3):261–279. doi: 10.1123/japa.18.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolf SL, Barnhart HX, Kutner NG, et al. Selected as the best paper in the 1990s: Reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. J Am Geriatr Soc. 2003;51(12):1794–1803. doi: 10.1046/j.1532-5415.2003.51566.x. [DOI] [PubMed] [Google Scholar]
- 22.Li F, Harmer P, McAuley E, et al. An evaluation of the effects of Tai Chi exercise on physical function among older persons: a randomized controlled trial. Ann Behav Med. 2001;23(2):139–146. doi: 10.1207/S15324796ABM2302_9. [DOI] [PubMed] [Google Scholar]
- 23.Chang JY, Tsai PF, Beck C, et al. The effect of tai chi on cognition in elders with cognitive impairment. Medsurg Nurs. 2011;20(2):63–69. quiz 70. [PMC free article] [PubMed] [Google Scholar]
- 24.Tsai PF, Beck C, Chang JY, et al. The effect of tai chi on knee osteoarthritis pain in cognitively impaired elders: pilot study. Geriatr Nurs. 2009;30(2):132–139. doi: 10.1016/j.gerinurse.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chibnall JT, Tait RC. Pain assessment in cognitively impaired and unimpaired older adults: a comparison of four scales. Pain. 2001;92(1-2):173–186. doi: 10.1016/s0304-3959(00)00485-1. [DOI] [PubMed] [Google Scholar]
- 26.Weiner D, Peterson B, Ladd K, McConnell E, Keefe F. Pain in nursing home residents: an exploration of prevalence, staff perspectives, and practical aspects of measurement. Clin J Pain. 1999;15(2):92–101. doi: 10.1097/00002508-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Friedman TW, Yelland GW, Robinson SR. Subtle cognitive impairment in elders with Mini-Mental State Examination scores within the ‘normal’ range. Int J Geriatr Psychiatry. 2012;27(5):463–471. doi: 10.1002/gps.2736. [DOI] [PubMed] [Google Scholar]
- 28.Adams G, Gulliford MC, Ukoumunne OC, et al. Patterns of intra-cluster correlation from primary care research to inform study design and analysis. J Clin Epidemiol. 2004;57:785–794. doi: 10.1016/j.jclinepi.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 29.Arthritis Foundation [December 9, 2010];Tai Chi program. 2010 Available from http://www.arthritis.org/events/getinvolved/ProgramsServices/TaiChi.asp.
- 30.Tsai P, Beck C, Chang JY, et al. The feasibility of implementing Tai Chi for nursing home residents with knee osteoarthritis and cognitive impairment. Activities Directors’ Quarterly for Alzheimer's & Other Dementia Patients. 2009;10(1):9–17. [PMC free article] [PubMed] [Google Scholar]
- 31.Chang JY, Tsai P, Woods S, et al. Teaching Tai Chi to elders with osteoarthritis pain and mild cognitive impairment. Activities Directors’ Quarterly for Alzheimer's & Other Dementia Patients. 2010;11(4):8–17. [PMC free article] [PubMed] [Google Scholar]
- 32.Tai Chi for Health Institute Certified instructor. 2011 Available from http://www.taichiforhealthinstitute.org/instructors/certified_instructors/
- 33.Bellamy N. Pain assessment in osteoarthritis: experience with the WOMAC osteoarthritis index. Semin Arthritis Rheum. 1989;18(4 Suppl 2):14–17. doi: 10.1016/0049-0172(89)90010-3. [DOI] [PubMed] [Google Scholar]
- 34.Hurley MV, Scott DL, Rees J, Newham DJ. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis. 1997;56(11):641–648. doi: 10.1136/ard.56.11.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piva SR, Fitzgerald GK, Irrgang JJ, Bouzubar F, Starz TW. Get up and go test in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2004;85(2):284–289. doi: 10.1016/j.apmr.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 36.Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills. 1995;80(1):163–166. doi: 10.2466/pms.1995.80.1.163. [DOI] [PubMed] [Google Scholar]
- 37.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 38.Burgener SC, Yang Y, Gilbert R, Marsh-Yant S. The effects of a multimodal intervention on outcomes of persons with early-stage dementia. Am J Alzheimers Dis Other Demen. 2008;23(4):382–394. doi: 10.1177/1533317508317527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002;29(1):131–138. [PubMed] [Google Scholar]