Abstract
Purpose
Depression and suicide are major public health concerns, and are often unrecognized among the elderly. This study investigated social inequalities in depressive symptoms and suicidal ideation among older adults.
Methods
Data come from 1,226 participants in PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial), a large primary care-based intervention trial for late-life depression. Linear and logistic regressions were used to analyze depressive symptoms and suicidal ideation over the two-year follow-up period.
Results
Mean Hamilton Depression Rating Scale (HDRS) scores were significantly higher among participants in financial strain (regression coefficient (b)=1.78, 95% confidence interval (CI)=0.67–2.89) and with annual incomes below $20,000 (b=1.67, CI=0.34–3.00). Financial strain was also associated with a higher risk of suicidal ideation (odds ratio=2.35, CI=1.38–3.98).
Conclusions
There exist marked social inequalities in depressive symptoms and suicidal ideation among older adults attending primary care practices, the setting in which depression is most commonly treated. Our results justify continued efforts to understand the mechanisms generating such inequalities, and to recognize and provide effective treatments for depression among high-risk populations.
Keywords: Depression, suicide, older adulthood, inequalities, primary care
INTRODUCTION
Social inequalities in major depression originate early in the life course and persist into adulthood [1–3]. In late-life, aspects of inequality that predict a markedly elevated risk of depression include low socioeconomic status and financial strain [4–9]. Defined as insufficient financial resources for meeting one’s basic needs, financial strain among older adults has been associated with higher levels of psychological distress, depressive symptoms [10–14], as well as diagnoses of major depression [15].
The inequalities observed primarily in epidemiologic samples have also been linked with worse depression outcomes in treated samples. For example, Cohen et al. have shown that older adults living in low-income neighborhoods: 1) have elevated levels of depressive symptoms and suicidal ideation; and 2) display, relative to older adults living in higher income neighborhoods, decreased response to antidepressant treatment [16–18]. Similarly, Friedman et al. reported that lower educational level predicted worse outcomes during antidepressant treatment [19].
The current study investigates social inequalities in late-life depression and suicidal ideation among primary care patients. This issue is of considerable public health importance given the likelihood that depression will be addressed in the first instance by a primary care provider, and the fact that the majority of depression treatment occurs in the context of primary care. The point prevalence of clinical depression among primary care patients approaches 10%, and has risen to become one of the ten leading conditions diagnosed and treated by primary care clinicians [20]. Sub-threshold depression is even more common in primary care settings, with a point prevalence approaching 20% in some samples [21]. The problem of depression in primary care is particularly relevant for older adults because of its impact on medical burden and disability, its relation with suicide and mortality, and because it is often untreated or inadequately treated [22–25]. Given generally universal access to health care among older adults in the United States, the primary care setting could be one avenue, albeit late in the life course, for reducing social inequalities in the burden of depression, and by implication the physical and mental health consequences of depression [26].
Determining the extent of depression inequalities among primary care patients would extend our knowledge of groups at heightened risk for psychiatric problems, and do so in a clinical settings where there is presumably ready access to psychiatric treatments. Accordingly, the objective of the current study is to expand our understanding of social inequalities in depression and suicidal ideation in the context of primary care. We hypothesize that the socioeconomic factors previously linked with risk for late-life depression in epidemiologic samples will also predict a heightened level of depression and suicidal ideation among older adult primary care patients—in particular, low educational attainment, low income, and financial strain. We also evaluate the roles of medical comorbidity and social support as potential explanatory factors in inequalities. Medical burden has been shown to exacerbate the course of depression [27–29], whereas social support may mitigate it [30–33]; and both of these are patterned by the socioeconomic factors which we examine.
We investigate the presence of social inequalities in the prevalence and course of depressive symptoms and suicidal ideation in the context of PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial), a large primary care-based intervention trial for late-life depression [34]. The PROSPECT trial presents a unique resource for investigating social inequalities because of a diverse study population ascertained from 20 primary care practices in three geographic locations, random selection of primary care patients for participation, systematic detection and assessment of depressive symptoms and suicidal ideation, longitudinal follow-up of participants over a two-year period, and the ability to exclude differential access to treatment as a potential confounding factor.
METHODS
Study cohort
The design of the PROSPECT trial, and the effectiveness of the PROSPECT intervention through the 24-month follow-up period, have been reported previously [35,36,34,37]. In practices randomized to the intervention arm, a depression care manager interfaced with patients and providers to ensure guideline-based provision of depression treatment (e.g., treatment with citalopram or interpersonal psychotherapy) and follow-up care throughout the study period. In practices randomized to the usual care arm, participants’ physicians received educational materials regarding geriatric depression, written notices of depression diagnoses, and contacts made by the investigators when the study personnel detected a significant suicide risk. All participants gave written informed consent prior to their enrollment in the study. The PROSPECT study was approved by the Institutional Review Boards of Cornell University, University of Pennsylvania, and University of Pittsburgh. Data analysis for the current study was approved by the Institutional Review Board of Harvard School of Public Health.
Whereas prior reports from PROSPECT have focused on participants who, at baseline, had clinically significant depressive symptoms, the current study includes all participants enrolled and followed over the course of the study, and investigates the naturalistic course of depression and suicidal ideation in relation to social factors. We therefore analyze the PROSPECT data as an observational study, and take advantage of the diverse sampling frame and the systematic detection and repeated assessments by mental health professionals of depression and suicidal ideation.
As described previously, the PROSPECT study was conducted in 20 primary care practices in the metropolitan areas of New York City, Philadelphia, and Pittsburgh [34]. Primary care patients ≥60 years old and with a Mini-Mental State Examination score ≥18 were eligible for enrollment into the study. Patients with scores >20 on the Center for Epidemiologic Studies Depression scale, or with a history of depression or depression treatment, were oversampled. Bruce et al. have described the recruitment procedures in detail [34]. The participation rate was 65.6% of all eligible patients, resulting in a sample size of 1,226. Individual participants were enrolled for a period of 2 years, with post-baseline assessments made at 4, 8, 12, 18, and 24 months. The current analyses assessed depressive symptoms and the presence of suicidal ideation at each follow-up assessment in relation to participants’ socioeconomic status (educational attainment, income, and financial strain), demographic characteristics (age, race, and marital status), overall medical burden, and availability of social supports.
Measures
Depressive symptoms were assessed at each study visit using the Hamilton Depression Rating Scale (HDRS) [38]. Suicidal ideation at each visit was assessed using both the HDRS and the Scale for Suicidal Ideation (SSI) [39]. Suicidal ideation was coded as present based on a score ≥1 on either the SSI or the suicide item of the HDRS (item #11).
Participant demographic factors were assessed at baseline and again at months 12 and 24. In the longitudinal analyses described below, demographic factors were updated to reflect any changes that were reported at these 2 time points. Age at baseline was categorized as ≥75 vs. 60–74. Race was categorized as White, Black, or Other. Educational attainment was categorized as <12 years, 12 years, 13–15 years, or ≥16 years. Annual income was coded in tertiles as follows: <$20,000, $20,001–$74,999, and ≥$75,000. In addition to income, our analyses included a measure of financial strain, which was coded positive if participants responded, “Can’t make ends meet” to a question asking about their current money situation. Financial strain reflects an individual’s income relative to his or her needs, and has been shown to predict depression independently from income among older adults [10]
Social support and medical comorbidity, assessed at baseline and reassessed at months 12 and 24, were included in the analyses due to their strong associations with depression [30,36]. Social support was based on the Duke Social Support Index (DSSI), which yielded scores on the following dimensions of support: social interaction, subjective social support, and instrumental support [40]. Overall medical burden was based on the Charlson Comorbidity Index [41].
Statistical analyses
We used random effects models to relate mean levels of depressive symptoms (using linear regression) and the likelihood of suicidal ideation (using logistic regression) at each study visit to participant demographic factors, socioeconomic status, social support, and medical comorbidity. The random effect that was included in the models was a subject-specific intercept, which accounted for within-subject variability in depressive symptoms or suicidal ideation over the course of the study. Random effects for primary care practices were not necessary given that the within-practice correlations of depression and suicidal ideation were negligible [34]. The linear random effects models were fitted using PROC MIXED, and the logistic random effects models were fitted using PROC GLIMMIX (using maximum likelihood estimation with adaptive quadrature), in SAS v9.2. For each dependent variable, we fitted a sequence of 5 models, adding successive blocks of covariates beginning with a demographics only model (age, race, sex, marital status, and educational attainment), and subsequently adding income (model 2), financial strain (model 3), medical comorbidity (model 4), and social support (model 5). With this sequence we assessed whether income, financial strain, medical comorbidity, and social support accounted for some of the association between the demographic factors and outcomes. All models included controls for site (New York, Philadelphia, or Pittsburgh) and intervention status.
We used multiple imputation to handle missing data that occurred either through item non-response or because of missed visits or attrition. This approach retains all observed data in the analyses, and to the extent that observed data are informative about the likelihood of missingness, yields results that are less biased than would be obtained from a complete-case analysis. The decision rule that we adopted for the PROSPECT trial was to impute all missing data up until a reported death [42]. The maximum number of theoretically observable person-visits was 7,356 (1,226 participants observed 6 times). However, 64 deaths were recorded over the study period, which reduced the total number of person-visits by 181, and yielded a final sample size of 7,175 person-visits in the longitudinal analyses. Of these, 5,658 person-visits were observed (78.9%), and the remainder was imputed. Imputations were done using the method of chained equations as implemented in IVEWare [43]. All analyses were conducted separately within each of 20 multiply imputed datasets, and the results were combined using the MIANALYZE procedure in SAS in order to account for sampling variability across the imputed datasets.
RESULTS
Participants in the PROSPECT study were predominantly female (69.9%) and <75 years of age (63.9%). The sample was diverse with respect to race/ethnicity (27.6% Black or African American) and educational attainment (24.7% with ≥16 years of education). The distribution of demographic factors and socioeconomic status in the sample is shown in the first column of Table 1. Mean HDRS scores, and the proportion of participants with suicidal ideation, across all study variables are shown in the second and third columns of Table 1, respectively. The general pattern that emerges at baseline is lower HDRS scores, and a lower risk of suicidal ideation, among PROSPECT participants in the highest educational category, highest income category, and not reporting financial strain.
Table 1.
Social and demographic characteristics of participants in the PROSPECT sample (n=1,226)
| Number of participants | Sample distribution, Percent (SE) | HDRS Score at Baseline, Mean (SE) | Suicidal Ideation at Baseline, Percent (SE) | |
|---|---|---|---|---|
| Total | 1226 | 100% | 11.4 (0.2) | 23.3 (1.2) |
| Age | ||||
| ≥75 | 443 | 36.1 (1.4) | 12.2 (0.3) | 24.3 (1.5) |
| 60–74 | 783 | 63.9 (1.4) | 9.9 (0.4) | 21.4 (2.0) |
| Race/ethnicity | ||||
| Non-Hispanic White | 852 | 69.5 (1.3) | 11.4 (0.3) | 24.2 (1.5) |
| Black or African American | 339 | 27.6 (1.3) | 11.5 (0.4) | 21.3 (2.2) |
| Other | 35 | 2.9 (0.5) | 11.3 (1.4) | 19.9 (6.7) |
| Sex | ||||
| Male | 368 | 30.1 (1.3) | 11.0 (0.5) | 23.3 (2.2) |
| Female | 858 | 70.0 (1.3) | 11.6 (0.3) | 23.2 (1.4) |
| Education | ||||
| <12 | 322 | 26.2 (1.3) | 12.2 (0.5) | 27.5 (2.5) |
| 12 | 367 | 29.9 (1.3) | 12.1 (0.4) | 22.4 (2.2) |
| 13–15 | 235 | 19.2 (1.1) | 11.4 (0.5) | 24.4 (2.8) |
| 16+ | 302 | 24.7 (1.2) | 9.7 (0.4) | 18.9 (2.3) |
| Marital status | ||||
| Married | 472 | 38.5 (1.4) | 11.1 (0.4) | 21.5 (1.9) |
| Widowed | 400 | 32.7 (1.3) | 10.9 (0.4) | 22.0 (2.1) |
| Separated | 63 | 5.2 (0.6) | 13.9 (1.1) | 31.8 (5.9) |
| Divorced | 173 | 14.1 (1.0) | 12.7 (0.7) | 25.0 (3.3) |
| Never married | 117 | 9.6 (0.8) | 11.2 (0.7) | 27.4 (4.1) |
| Financial strain (can’t make ends meat) | ||||
| Yes | 120 | 9.8 (1.2) | 15.1 (0.8) | 40.4 (4.6) |
| No | 1106 | 90.2 (1.2) | 11.0 (0.3) | 21.4 (1.3) |
| Income | ||||
| <20,000 | 569 | 46.4 (2.3) | 12.4 (0.4) | 27.4 (2.0) |
| 20,001–75,000 | 451 | 36.8 (2.3) | 10.9 (0.4) | 21.1 (2.1) |
| >75,000 | 206 | 16.8 (2.0) | 9.8 (0.8) | 16.2 (3.3) |
| Site | ||||
| New York | 467 | 38.1 (1.4) | 9.8 (0.4) | 18.4 (1.8) |
| Philadelphia | 426 | 34.8 (1.4) | 11.6 (0.4) | 23.7 (2.1) |
| Pittsburgh | 333 | 27.2 (1.3) | 13.4 (0.5) | 29.4 (2.5) |
| Intervention Status | ||||
| Intervention | 609 | 49.7 (1.4) | 12.0 (0.3) | 25.1 (1.8) |
| Control | 617 | 50.3 (1.4) | 10.8 (0.3) | 21.4 (1.7) |
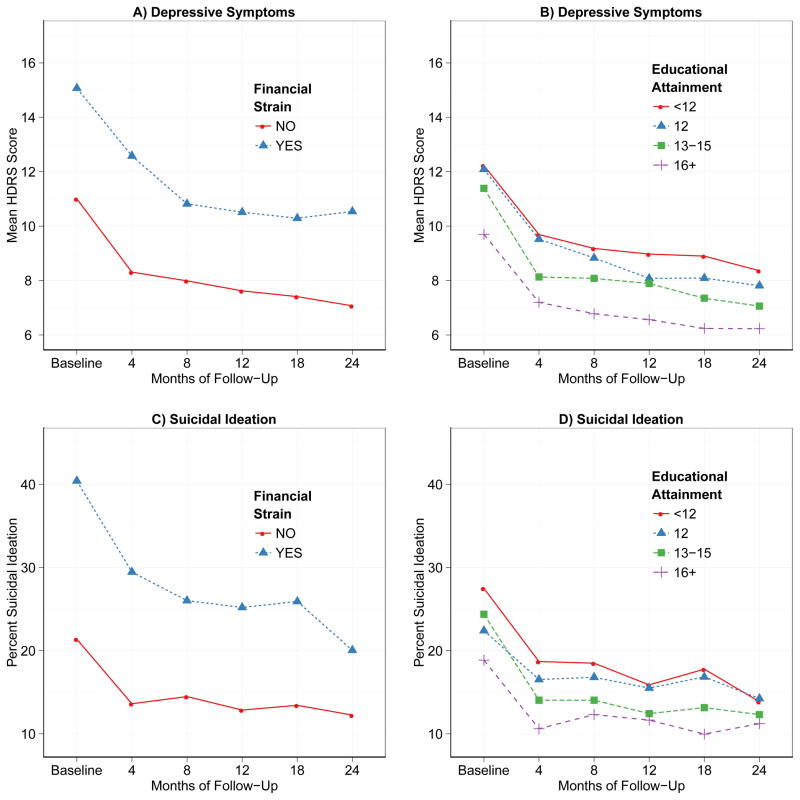
Trends in the relationship of socioeconomic indicators with HDRS scores and suicidal ideation over the course of the PROSPECT study are illustrated in Figure 1. The overall trends in depressive symptoms and suicidal ideation reflect higher levels at baseline and subsequent decreases in symptoms over the course of the follow-up period. This is expected given that participants with higher levels of depressive symptoms were preferentially selected for participation in the PROSPECT trial [35,36,34,37]. However, when stratified by socioeconomic status, both mean HDRS scores and the prevalence of suicidal ideation were significantly higher at baseline and throughout the follow-up period among individuals who reported financial strain (graphs A (t=6.0, p<0.001) and C (t=4.9, p<0.001)), or lower levels of education (graphs B (F=12.2, p<0.001) and D (F=4.1, p=0.006)). The magnitude of differences in depressive symptoms and in suicidal ideation was more pronounced when plotted by financial strain than education.
Figure 1.
Mean Hamilton Depression Rating Scale (HDRS) scores (panels A and B), and proportion of participants with suicidal ideation (panels C and D) over the two-year follow-up period in the PROSPECT trial (n=1,226). Means and proportions are presented separately according to financial strain (panels A and C) and educational attainment (panels B and D).
The mean (SE) HDRS at baseline in the sample is 11.4 (0.2). Results of longitudinal models for mean HDRS scores over the course of the PROSPECT study are presented in Table 2. Linear regression coefficients and corresponding 95% confidence intervals are presented from each of 5 models. Coefficients with a positive sign indicate factors associated with higher average HDRS scores over the course of the study. In the demographics only model (model 1), participants who were divorced or separated had significantly higher mean levels of depressive symptoms over the course of the trial, as did participants with less than high school or high school educations. However, when accounting for income, the magnitude of the regression coefficients for divorced or separated marital status were substantially reduced (model 2), suggesting that marital status differences in depressive symptoms are partly explained by differences in income. Financial strain, added in model 3, was also significantly associated with depressive symptoms. It is notable in model 3 that both financial strain and low income (<$20,000 annually) were independently associated with depressive symptoms, with regression coefficients of a similar magnitude. In model 4, higher levels of physical illness according to the Charlson Comorbidity Index were associated with higher mean HDRS scores. The final model (model 5) added the Duke Social Support Scales, two of which were significantly associated with depressive symptoms. Higher scores on the scales of social interaction and subjective social support were associated with lower mean HDRS scores over the course of the PROSPECT trial. Less than high school or high school education remained significant predictors of elevated HDRS scores in the final model, although the magnitude of the differences in HDRS between individuals in these two education categories relative to individuals with a college degree was substantially smaller in the final model (1.24 and 1.25, respectively) than in model 1 (2.88 and 2.13, respectively). In the final model, financial strain and annual incomes below $20,000 were associated with significantly higher mean HDRS scores over the course of the trial (coefficient for financial strain=1.78, CI=0.67, 2.89; for low income, coefficient=1.67, CI=0.34, 3.00).
Table 2.
Results of linear regression models of mean HDRS scores across the 2-year duration of the PROSPECT triala
| Model 1 Coefficient (CI)b | Model 2 Coefficient (CI)b | Model 3 Coefficient (CI)b | Model 4 Coefficient (CI)b | Model 5 Coefficient (CI)b | |
|---|---|---|---|---|---|
| Age | −0.15 (−0.19, −0.11) | −0.16 (−0.20, −0.11) | −0.15 (−0.19, −0.10) | −0.14 (−0.19, −0.10) | −0.13 (−0.17, −0.09) |
| Race/ethnicity | |||||
| Non-Hispanic White | Reference | Reference | Reference | Reference | Reference |
| Black or African American | −0.52 (−1.34, 0.30) | −0.72 (−1.54, 0.10) | −0.80 (−1.61, 0.01) | −0.94 (−1.74, −0.15) | −0.89 (−1.66, −0.13) |
| Other | −0.57 (−2.54, 1.40) | −0.66 (−2.63, 1.31) | −0.68 (−2.63, 1.28) | −0.82 (−2.73, 1.09) | −0.78 (−2.63, 1.06) |
| Sex | |||||
| Male | Reference | Reference | Reference | Reference | Reference |
| Female | 0.35 (−0.37, 1.08) | 0.25 (−0.48, 0.99) | 0.30 (−0.42, 1.02) | 0.38 (−0.33, 1.08) | 0.49 (−0.19, 1.17) |
| Marital status | |||||
| Married | Reference | Reference | Reference | Reference | Reference |
| Divorced | 1.53 (0.56, 2.50) | 0.85 (−0.19, 1.88) | 0.72 (−0.31, 1.75) | 0.78 (−0.23, 1.79) | 0.66 (−0.30, 1.62) |
| Separated | 1.76 (0.25, 3.28) | 1.11 (−0.42, 2.65) | 0.94 (−0.59, 2.48) | 0.79 (−0.73, 2.30) | 0.66 (−0.79, 2.12) |
| Widowed | 0.61 (−0.20, 1.43) | 0.09 (−0.78, 0.96) | 0.11 (−0.76, 0.99) | 0.16 (−0.69, 1.01) | 0.25 (−0.58, 1.08) |
| Never married | 1.08 (−0.06, 2.23) | 0.51 (−0.66, 1.69) | 0.40 (−0.77, 1.57) | 0.39 (−0.75, 1.53) | 0.17 (−0.94, 1.28) |
| Educational attainment | |||||
| Less than high school | 2.88 (1.95, 3.81) | 1.86 (0.75, 2.98) | 1.82 (0.71, 2.92) | 1.59 (0.52, 2.65) | 1.24 (0.23, 2.25) |
| High school | 2.13 (1.26, 3.00) | 1.48 (0.50, 2.47) | 1.52 (0.54, 2.50) | 1.42 (0.47, 2.36) | 1.25 (0.34, 2.15) |
| Some college | 1.10 (0.14, 2.06) | 0.77 (−0.21, 1.75) | 0.83 (−0.15, 1.81) | 0.79 (−0.16, 1.75) | 0.63 (−0.29, 1.54) |
| College degree | Reference | Reference | Reference | Reference | Reference |
| Income | |||||
| <20,000 | 2.33 (0.94, 3.72) | 2.05 (0.61, 3.50) | 1.88 (0.48, 3.27) | 1.67 (0.34, 3.00) | |
| 20,001–75,000 | 0.47 (−0.68, 1.62) | 0.42 (−0.74, 1.57) | 0.36 (−0.74, 1.45) | 0.28 (−0.77, 1.32) | |
| >75,000 | Reference | Reference | Reference | Reference | |
| Financial strain (can’t make ends meet) | |||||
| Yes | 2.16 (0.99, 3.33) | 1.96 (0.82, 3.10) | 1.78 (0.67, 2.89) | ||
| No | Reference | Reference | Reference | ||
| Charlson Comorbidity Index | 0.36 (0.25, 0.47) | 0.34 (0.23, 0.45) | |||
| Duke Social Interaction Score | −0.24 (−0.32, −0.16) | ||||
| Duke Subjective Support Score | −0.24 (−0.30, −0.18) | ||||
| Duke Instrumental Support Score | 0.03 (−0.05, 0.11) |
Regression models include data from 1,226 individuals observed across 6 waves of the PROSPECT trial. Site and intervention status also included in each model, along with random intercepts for each subject.
95% confidence interval.
We then fitted a similar sequence of regression models for suicidal ideation during the PROSPECT trial. The odds ratios from these mixed-effects logistic regression models are presented in Table 3. The pattern of results of the analyses of suicidal ideation was similar to the results obtained in the models of mean HDRS scores. In the model for demographic factors, lower levels of education, and divorced, widowed, and never married marital statuses, were associated with a higher odds of suicidal symptoms; yet these associations were attenuated in subsequent models that added measures of economic resources (primarily income). In the final model (model 5), financial strain was associated with a significantly higher odds of suicidal symptoms (odds ratio=2.35, CI=1.38, 3.98); physical illness at baseline was associated with a higher odds of suicidal symptoms; and higher scores on the scales of social interaction and subjective support were associated with a lower odds of suicidal symptoms.
Table 3.
Results of logistic regression models of suicidal ideation across the 2-year duration of the PROSPECT triala
| Model 1 OR (CI)b | Model 2 OR (CI)b | Model 3 OR (CI)b | Model 4 OR (CI)b | Model 5 OR (CI)b | |
|---|---|---|---|---|---|
| Age | 0.99 (0.97, 1.01) | 0.98 (0.96, 1.01) | 0.99 (0.97, 1.01) | 0.99 (0.97, 1.01) | 0.99 (0.97, 1.01) |
| Race/ethnicity | |||||
| Non-Hispanic White | Reference | Reference | Reference | Reference | Reference |
| Black or African American | 0.71 (0.45, 1.12) | 0.67 (0.42, 1.04) | 0.64 (0.41, 0.99) | 0.60 (0.38, 0.93) | 0.61 (0.40, 0.94) |
| Other | 0.51 (0.18, 1.44) | 0.50 (0.18, 1.40) | 0.51 (0.18, 1.39) | 0.47 (0.17, 1.29) | 0.51 (0.19, 1.32) |
| Sex | |||||
| Malec | Reference | Reference | Reference | Reference | Reference |
| Female | 0.96 (0.65, 1.42) | 0.90 (0.60, 1.35) | 0.92 (0.62, 1.38) | 0.95 (0.64, 1.42) | 1.03 (0.70, 1.52) |
| Marital status | |||||
| Marriedc | Reference | Reference | Reference | Reference | Reference |
| Divorced | 1.67 (1.00, 2.81) | 1.18 (0.68, 2.06) | 1.11 (0.64, 1.93) | 1.14 (0.66, 1.98) | 1.01 (0.60, 1.70) |
| Separated | 1.98 (0.90, 4.34) | 1.47 (0.67, 3.26) | 1.33 (0.61, 2.91) | 1.25 (0.58, 2.71) | 1.12 (0.53, 2.35) |
| Widowed | 1.52 (1.01, 2.28) | 1.20 (0.77, 1.87) | 1.23 (0.79, 1.92) | 1.24 (0.80, 1.92) | 1.26 (0.83, 1.92) |
| Never married | 2.78 (1.47, 5.26) | 2.15 (1.14, 4.06) | 2.00 (1.07, 3.74) | 1.99 (1.07, 3.71) | 1.71 (0.93, 3.14) |
| Education | |||||
| Less than high school | 2.25 (1.37, 3.69) | 1.46 (0.81, 2.65) | 1.41 (0.78, 2.53) | 1.30 (0.73, 2.32) | 1.13 (0.65, 1.95) |
| High school | 1.66 (1.05, 2.63) | 1.25 (0.76, 2.06) | 1.25 (0.76, 2.05) | 1.21 (0.74, 1.97) | 1.12 (0.70, 1.79) |
| Some college | 1.31 (0.79, 2.19) | 1.15 (0.68, 1.95) | 1.18 (0.70, 1.97) | 1.16 (0.69, 1.94) | 1.06 (0.65, 1.73) |
| College degreec | Reference | Reference | Reference | Reference | Reference |
| Income | |||||
| <20,000 | 2.82 (1.27, 6.27) | 2.41 (1.06, 5.44) | 2.28 (1.02, 5.12) | 2.07 (0.94, 4.56) | |
| 20,001–75,000 | 1.28 (0.69, 2.38) | 1.26 (0.70, 2.28) | 1.22 (0.68, 2.18) | 1.17 (0.66, 2.06) | |
| >75,000c | Reference | Reference | Reference | Reference | |
| Financial strain (can’t make ends meet) | |||||
| Yes | 2.90 (1.68, 5.00) | 2.65 (1.55, 4.54) | 2.35 (1.38, 3.98) | ||
| Noc | Reference | Reference | Reference | ||
| Charlson Comorbidity Index | 1.13 (1.07, 1.21) | 1.12 (1.05, 1.19) | |||
| Duke Social Interaction Score | 0.90 (0.86, 0.95) | ||||
| Duke Subjective Support Score | 0.90 (0.86, 0.95) | ||||
| Duke Instrumental Support Score | 0.99 (0.94, 1.05) |
Logistic regression models include data from 1,226 individuals observed across 6 waves of the PROSPECT trial. Site and intervention status also included in each model, along with random intercepts for each subject.
Odds ratio, 95% confidence interval.
DISCUSSION
In a longitudinal sample of older primary care patients, there were significant social inequalities in the prevalence and course of depression and suicidal ideation over a two-year period. The most important finding of our study is that lower income and financial strain were associated with higher levels of depressive symptoms, as well as an increased risk of suicidal ideation. The impact of financial strain on depression was independent of other demographic factors, including participants’ actual income level. Among older adults, current income may not reflect economic resources that derive from an individual or family’s accumulated wealth and assets [44]. Financial strain reflects the balance between income and needs, and therefore is more indicative of current economic hardship. It has been shown to predict older adulthood depression in prior community and clinical samples [45,10], and is one likely explanatory factor for the associations of unemployment and widowhood with depression [14,46]. In this regard, marital status differences in depressive symptoms and suicidal ideation in PROSPECT were substantially attenuated when accounting for financial strain.
The measurement of financial strain in PROSPECT, and in most prior studies, incorporates an individual’s subjective valuation of their economic situation that may be partly driven by anxiety over finances. In PROSPECT, financial strain was assessed at baseline, and was predictive of depressive symptoms and suicidal ideation over a 2-year period. This design confirms and extends the results of prior cross-sectional studies that reported associations between financial strain and depression. However, self-reports of financial strain could be distorted by current symptomatology [47]. More objective assessments of financial strain are rare; one exception is a study by Zimmerman and Katon, in which the definition of financial strain used was the ratio of debt to assets; they also found financial strain to be associated with depression independently from income [12].
Overall medical burden was also associated with a higher level of depressive symptoms as well as an increased risk of suicidal ideation, as reported previously among a subset of participants in the current sample as well as in other studies [36,48]. The psychiatric consequences of medical conditions are well documented [49], and it has been suggested that treating medical conditions may lead to reductions in the risk of depression (e.g., treatment for cardiovascular risk factors); however, this remains to be shown in experimental studies. The relevance of this finding for the current investigation is that social inequalities in depressive symptoms and suicidal ideation were not accounted for by inequalities in general medical burden.
There is considerable evidence of the importance of social support for mental health, and on the association between low social support and both depression and suicidality [50,30]. The evidence is somewhat mixed as to whether differences in social support explain economic inequalities in depression [51,52]. In our study, they did not. Associations of financial strain, income, and education with depressive symptoms and suicidal ideation were largely unchanged after adding social support to the regression models. It is notable that the dimensions of social support that were significantly related to depression were the more cognitively oriented dimensions of support—social interaction and subjective support—rather than instrumental support, defined as receiving help in a wide range of areas from family or friends. Social support-based interventions might be beneficial for reducing depressive symptoms [53], though it is unlikely that improving social support will significantly mitigate the adverse mental health consequences of socioeconomic deprivation or other stressful life events.
This study illustrates a pattern of associations that is consistent with the accumulation of socioeconomic disparities in depression over the life course. Lower educational attainment, a marker of socioeconomic status established in young adulthood, was strongly associated with depression—yet this association was reduced when controlling for current income and financial strain. This finding is consistent with theory and empirical evidence in the area of life course epidemiology arguing that the social determinants of health observed in older adulthood reflect not only the consequences of current social circumstances, but also the consequences of socioeconomic disadvantage experienced over many years [54,55]. This evidence would also argue that the mechanisms that generate inequalities in depression in older adulthood, as well as points of intervention for reducing such inequalities, may be identifiable early in the life course.
Strengths of the PROSPECT trial for investigating social inequalities in depression among older adult primary care patients include the diversity of participants enrolled, validated measures used to assess depression and suicidal symptoms, and the random selection of primary care patients for participation rather than selection by physician or self-referral. With few exceptions [56], prior studies of depression in primary care settings that were based on larger samples focused on diagnosed depression or depression based on screening instruments rather than clinician-administered measures of depression such as the HDRS, as was used in the current study.
While PROSPECT was an experimental study [37,34], our analysis of the social determinants of depression was observational, and therefore is subject to the usual limitations of observational research. Our results cannot be interpreted as estimates of causal associations, which means that we cannot establish solely from these results whether reducing financial strain will have the effect of ameliorating depressive symptoms. Another limitations is the potential confounding effects of unmeasured variables, including the effect of prior depression on lifetime earnings.
Conclusions
Social inequalities in the prevalence and course of depressive symptoms and suicidal ideation demonstrated in community samples exist among patients attending primary care practices, the clinical setting in which most depression is treated. These inequalities persisted over the two-year duration of the PROSPECT study (as illustrated in Figure 1). Depression among older adults is often chronic [57,58], and the results of the current study would suggest that this chronicity is exacerbated by economic disadvantage.
The results of this study could not be attributed to differential health care access, given that all study participants had access to primary care. However, future work is needed to determine the extent to which socioeconomic inequalities exist in antidepressant treatment outcomes [18]. Based on our findings, self-report of financial strain identifies such a population: in our study, those reporting strain continued to have, on average, clinically significant depressive symptoms as indicated by HDRS scores >10. Additional work is needed to determine whether targeting populations shown to be at elevated risk for depression on the basis of social and economic factors can mitigate disease onset or recurrence [59,60], as well as maximize the effectiveness of depression treatments [61].
Acknowledgments
This work was supported by the National Institutes of Health grants MH83335, MH085944, and MH059366. Forest Pharmaceuticals provided free citalopram for the PROSPECT study.
The authors sincerely appreciate the contributions of Ms. Kathleen McGaffigan for data management and statistical programming, and Ms. Rebecca Hawrusik for conducting literature reviews.
George S. Alexopoulos, M.D., receives research support from Forest; he serves on the speakers’ bureau for Forest, Lilly, Bristol Meyers Squibb, Astra Zeneca, Merck; and is a stockholder in Johnson & Johnson. Martha L. Bruce, Ph.D., M.P.H., has received financial compensation for consulting to Medispin, Inc., a medical education company. Benoit H. Mulsant, M.D., currently receives research support from the US National Institute of Mental Health, the Canadian Institutes for Health Research, Bristol-Myers Squibb, and Wyeth. During the past five years, he has also received research support or honoraria from Astra-Zeneca, Bristol-Myers Squibb, Eli Lilly, Forest Laboratories, GlaxoSmithKline, Janssen, Lundbeck, Pfizer and Wyeth; he previously directly held stocks (all less than $10,000) of Akzo-Nobel, Alkermes, AstraZeneca, Biogen, Celsion, Elan, Eli Lilly, Forest, Orchestra Therapeutics, and Pfizer. Charles F. Reynolds III, M.D., receives pharmaceutical supplies from Forest Laboratories, BMS, Pfizer, and Lilly for his NIH sponsored research.
References
- 1.Cairney J, Krause N. The social distribution of psychological distress and depression in older adults. J Aging Health. 2005;17(6):807–835. doi: 10.1177/0898264305280985. [DOI] [PubMed] [Google Scholar]
- 2.Lorant V, Deliege D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003;157 (2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- 3.Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Socioeconomic status in childhood and the lifetime risk of major depression. Int J Epidemiol. 2002;31:359–367. [PubMed] [Google Scholar]
- 4.Mulsant BH, Ganguli M. Epidemiology and diagnosis of depression in late life. J Clin Psychiatry. 1999;60(Suppl 20):9–15. [PubMed] [Google Scholar]
- 5.Alexopoulos GS. Depression in the elderly. The Lancet. 2005;365(9475):1961–1970. doi: 10.1016/s0140-6736(05)66665-2. [DOI] [PubMed] [Google Scholar]
- 6.Bruce ML. Psychosocial risk factors for depressive disorders in late life. Biol Psychiatry. 2002;52 (3):175–184. doi: 10.1016/s0006-3223(02)01410-5. [DOI] [PubMed] [Google Scholar]
- 7.Gilman SE, Carliner H, Cohen A. The social determinants of depression in older adulthood. In: Reynolds CF, HL, MS, editors. Late-Life Mood Disorders. Oxford University Press; (In Press) [Google Scholar]
- 8.Kraaij V, Arensman E, Spinhoven P. Negative life events and depression in elderly persons: a meta-analysis. The journals of gerontology Series B, Psychological sciences and social sciences. 2002;57 (1):87–94. doi: 10.1093/geronb/57.1.p87. [DOI] [PubMed] [Google Scholar]
- 9.Butterworth P, Rodgers B, Windsor TD. Financial hardship, socio-economic position and depression: results from the PATH Through Life Survey. Soc Sci Med. 2009;69(2):229–237. doi: 10.1016/j.socscimed.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Ferraro KF, Su Y. Financial strain, social relations, and psychological distress among older people: a cross-cultural analysis. J Gerontol B Psychol Sci Soc Sci. 1999;54 (1):S3–15. doi: 10.1093/geronb/54b.1.s3. [DOI] [PubMed] [Google Scholar]
- 11.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47 (1):17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 12.Zimmerman FJ, Katon W. Socioeconomic status, depression disparities, and financial strain: what lies behind the income-depression relationship? Health Econ. 2005;14(12):1197–1215. doi: 10.1002/hec.1011. [DOI] [PubMed] [Google Scholar]
- 13.Szanton SL, Thorpe RJ, Whitfield K. Life-course financial strain and health in African-Americans. Soc Sci Med. 2010;71(2):259–265. doi: 10.1016/j.socscimed.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Price RH, Choi JN, Vinokur AD. Links in the chain of adversity following job loss: how financial strain and loss of personal control lead to depression, impaired functioning, and poor health. J Occup Health Psychol. 2002;7 (4):302–312. doi: 10.1037//1076-8998.7.4.302. [DOI] [PubMed] [Google Scholar]
- 15.Friedman B, Conwell Y, Delavan RL. Correlates of late-life major depression: a comparison of urban and rural primary care patients. Am J Geriatr Psychiatry. 2007;15(1):28–41. doi: 10.1097/01.JGP.0000224732.74767.ad. [DOI] [PubMed] [Google Scholar]
- 16.Cohen A, Chapman BP, Gilman SE, Delmerico AM, Wieczorek W, Duberstein PR, Lyness JM. Social inequalities in the occurrence of suicidal ideation among older primary care patients. Am J Geriatr Psychiatry. 2010;18(12):1146–1154. doi: 10.1097/JGP.0b013e3181dd1e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cohen A, Gilman SE, Houck PR, Szanto K, Reynolds CF., 3rd Socioeconomic status and anxiety as predictors of antidepressant treatment response and suicidal ideation in older adults. Soc Psychiatry Psychiatr Epidemiol. 2009;44(4):272–277. doi: 10.1007/s00127-008-0436-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen A, Houck PR, Szanto K, Dew MA, Gilman SE, Reynolds CF., 3rd Social inequalities in response to antidepressant treatment in older adults. Arch Gen Psychiatry. 2006;63(1):50–56. doi: 10.1001/archpsyc.63.1.50. [DOI] [PubMed] [Google Scholar]
- 19.Friedman ES, Wisniewski SR, Gilmer W, Nierenberg AA, Rush AJ, Fava M, Zisook S, Balasubramani GK, Trivedi MH. Sociodemographic, clinical, and treatment characteristics associated with worsened depression during treatment with citalopram: results of the NIMH STAR(*)D trial. Depress Anxiety. 2009;26(7):612–621. doi: 10.1002/da.20568. [DOI] [PubMed] [Google Scholar]
- 20.Stafford RS, Ausiello JC, Misra B, Saglam D. National Patterns of Depression Treatment in Primary Care. Prim Care Companion. J Clin Psychiatry. 2000;2 (6):211–216. doi: 10.4088/pcc.v02n0603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zung WW, Broadhead WE, Roth ME. Prevalence of depressive symptoms in primary care. J Fam Pract. 1993;37 (4):337–344. [PubMed] [Google Scholar]
- 22.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72 (3):227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 23.Ryan J, Carriere I, Ritchie K, Stewart R, Toulemonde G, Dartigues JF, Tzourio C, Ancelin ML. Late-life depression and mortality: influence of gender and antidepressant use. Br J Psychiatry. 2008;192(1):12–18. doi: 10.1192/bjp.bp.107.039164. [DOI] [PubMed] [Google Scholar]
- 24.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289 (23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 25.Strothers HS, 3rd, Rust G, Minor P, Fresh E, Druss B, Satcher D. Disparities in antidepressant treatment in Medicaid elderly diagnosed with depression. J Am Geriatr Soc. 2005;53(3):456–461. doi: 10.1111/j.1532-5415.2005.53164.x. [DOI] [PubMed] [Google Scholar]
- 26.Park M, Unutzer J. Geriatric depression in primary care. The Psychiatric clinics of North America. 2011;34(2):469–487. doi: 10.1016/j.psc.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lyness JM, Heo M, Datto CJ, Ten Have TR, Katz IR, Drayer R, Reynolds CF, 3rd, Alexopoulos GS, Bruce ML. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Ann Intern Med. 2006;144 (7):496–504. doi: 10.7326/0003-4819-144-7-200604040-00008. [DOI] [PubMed] [Google Scholar]
- 28.Dew MA, Whyte EM, Lenze EJ, Houck PR, Mulsant BH, Pollock BG, Stack JA, Bensasi S, Reynolds CF., 3rd Recovery from major depression in older adults receiving augmentation of antidepressant pharmacotherapy. Am J Psychiatry. 2007;164 (6):892–899. doi: 10.1176/ajp.2007.164.6.892. [DOI] [PubMed] [Google Scholar]
- 29.Lyness JM, Niculescu A, Tu X, Reynolds CF, 3rd, Caine ED. The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics. 2006;47(5):435–439. doi: 10.1176/appi.psy.47.5.435. [DOI] [PubMed] [Google Scholar]
- 30.George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. Br J Psychiatry. 1989;154:478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- 31.Oxman TE, Berkman LF, Kasl S, Freeman DH, Jr, Barrett J. Social support and depressive symptoms in the elderly. Am J Epidemiol. 1992;135 (4):356–368. doi: 10.1093/oxfordjournals.aje.a116297. [DOI] [PubMed] [Google Scholar]
- 32.Rowe JL, Conwell Y, Schulberg HC, Bruce ML. Social support and suicidal ideation in older adults using home healthcare services. Am J Geriatr Psychiatry. 2006;14(9):758–766. doi: 10.1097/01.JGP.0000218324.78202.25. [DOI] [PubMed] [Google Scholar]
- 33.Taylor MG, Lynch SM. Trajectories of impairment, social support, and depressive symptoms in later life. J Gerontol B Psychol Sci Soc Sci. 2004;59 (4):S238–246. doi: 10.1093/geronb/59.4.s238. [DOI] [PubMed] [Google Scholar]
- 34.Bruce ML, Ten Have TR, Reynolds CF, 3rd, Katz II, Schulberg HC, Mulsant BH, Brown GK, McAvay GJ, Pearson JL, Alexopoulos GS. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 35.Alexopoulos GS, Katz IR, Bruce ML, Heo M, Ten Have T, Raue P, Bogner HR, Schulberg HC, Mulsant BH, Reynolds CF., 3rd Remission in depressed geriatric primary care patients: a report from the PROSPECT study. Am J Psychiatry. 2005;162(4):718–724. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bogner HR, Cary MS, Bruce ML, Reynolds CF, 3rd, Mulsant B, Ten Have T, Alexopoulos GS. The role of medical comorbidity in outcome of major depression in primary care: the PROSPECT study. Am J Geriatr Psychiatry. 2005;13(10):861–868. doi: 10.1176/appi.ajgp.13.10.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alexopoulos GS, Reynolds CF, 3rd, Bruce ML, Katz IR, Raue PJ, Mulsant BH, Oslin DW, Ten Have T. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. Am J Psychiatry. 2009;166(8):882–890. doi: 10.1176/appi.ajp.2009.08121779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behav Res Ther. 1997;35 (11):1039–1046. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 40.Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. Med Care. 1988;26 (7):709–723. doi: 10.1097/00005650-198807000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40 (5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 42.Harel O, Hofer SM, Hoffman L, Pedersen NL, Johansson B. Population inference with mortality and attrition in longitudinal studies on aging: a two-stage multiple imputation method. Exp Aging Res. 2007;33(2):187–203. doi: 10.1080/03610730701239004. [DOI] [PubMed] [Google Scholar]
- 43.Raghunathan TE, Lepkowski JM, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27 (1):85–95. [Google Scholar]
- 44.Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294 (22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 45.Cohen CI, Goh KH, Gustave M. A prospective study of outcome and predictors of subclinical and clinical depression in an older biracial sample of psychiatric outpatients. J Affect Disord. 2010;121(3):204–211. doi: 10.1016/j.jad.2009.05.021. [DOI] [PubMed] [Google Scholar]
- 46.Umberson D, Wortman CB, Kessler RC. Widowhood and depression: explaining long-term gender differences in vulnerability. Journal of Health & Social Behavior. 1992;33 (1):10–24. [PubMed] [Google Scholar]
- 47.Cooper C, Bebbington PE, Meltzer H, Bhugra D, Brugha T, Jenkins R, Farrell M, King M. Depression and common mental disorders in lone parents: results of the 2000 National Psychiatric Morbidity Survey. Psychol Med. 2008;38(3):335–342. doi: 10.1017/S0033291707001493. [DOI] [PubMed] [Google Scholar]
- 48.von Ammon Cavanaugh S, Furlanetto LM, Creech SD, Powell LH. Medical illness, past depression, and present depression: a predictive triad for in-hospital mortality. Am J Psychiatry. 2001;158 (1):43–48. doi: 10.1176/appi.ajp.158.1.43. [DOI] [PubMed] [Google Scholar]
- 49.Callahan CM, Wolinsky FD, Stump TE, Nienaber NA, Hui SL, Tierney WM. Mortality, symptoms, and functional impairment in late-life depression. J Gen Intern Med. 1998;13 (11):746–752. doi: 10.1046/j.1525-1497.1998.00226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lynch TR, Mendelson T, Robins CJ, Krishnan KR, George LK, Johnson CS, Blazer DG. Perceived social support among depressed elderly, middle-aged, and young-adult samples: cross-sectional and longitudinal analyses. J Affect Disord. 1999;55 (2–3):159–170. doi: 10.1016/s0165-0327(99)00017-8. [DOI] [PubMed] [Google Scholar]
- 51.Huurre T, Eerola M, Rahkonen O, Aro H. Does social support affect the relationship between socioeconomic status and depression? A longitudinal study from adolescence to adulthood. J Affect Disord. 2007;100(1–3):55–64. doi: 10.1016/j.jad.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 52.Schulz AJ, Israel BA, Zenk SN, Parker EA, Lichtenstein R, Shellman-Weir S, ABL Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit’s eastside. Soc Sci Med. 2006;62(2):510–522. doi: 10.1016/j.socscimed.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 53.Harris T, Brown GW, Robinson R. Befriending as an intervention for chronic depression among women in an inner city. 1: Randomised controlled trial. Br J Psychiatry. 1999;174:219–224. doi: 10.1192/bjp.174.3.219. [DOI] [PubMed] [Google Scholar]
- 54.Hertzman C, Power C. Health and human development: understandings from life-course research. Developmental neuropsychology. 2003;24(2–3):719–744. doi: 10.1080/87565641.2003.9651917. [DOI] [PubMed] [Google Scholar]
- 55.Pearlin LI. The life course and the stress process: some conceptual comparisons. J Gerontol B Psychol Sci Soc Sci. 2010;65B(2):207–215. doi: 10.1093/geronb/gbp106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Leon AC, Olfson M, Broadhead WE, Barrett JE, Blacklow RS, Keller MB, Higgins ES, Weissman MM. Prevalence of mental disorders in primary care. Implications for screening. Arch Fam Med. 1995;4 (10):857–861. doi: 10.1001/archfami.4.10.857. [DOI] [PubMed] [Google Scholar]
- 57.Beekman AT, Geerlings SW, Deeg DJ, Smit JH, Schoevers RS, de Beurs E, Braam AW, Penninx BW, van Tilburg W. The natural history of late-life depression: a 6-year prospective study in the community. Arch Gen Psychiatry. 2002;59 (7):605–611. doi: 10.1001/archpsyc.59.7.605. [DOI] [PubMed] [Google Scholar]
- 58.Schoevers RA, Beekman AT, Deeg DJ, Hooijer C, Jonker C, van Tilburg W. The natural history of late-life depression: results from the Amsterdam Study of the Elderly (AMSTEL) J Affect Disord. 2003;76 (1–3):5–14. doi: 10.1016/s0165-0327(02)00060-5. [DOI] [PubMed] [Google Scholar]
- 59.Reynolds CF., 3rd Prevention of depressive disorders: a brave new world. Depress Anxiety. 2009;26(12):1062–1065. doi: 10.1002/da.20644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reynolds CF, 3rd, Dew MA, Lenze EJ, Whyte EM. Preventing depression in medical illness: a new lead? Arch Gen Psychiatry. 2007;64 (8):884–885. doi: 10.1001/archpsyc.64.8.884. [DOI] [PubMed] [Google Scholar]
- 61.Miranda J, Chung JY, Green BL, Krupnick J, Siddique J, Revicki DA, Belin T. Treating depression in predominantly low-income young minority women: a randomized controlled trial. JAMA. 2003;290 (1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]